Older women have lower levels of physical functioning and higher associated health care costs than men after coronary artery bypass surgery (CABS) (Vaccarino et al., 2003a&b). Clinical trials have demonstrated that interventions to increase physical activity levels can reduce the risk of recurrent cardiac events, reduce health care expenditures, prolong life, improve functional capacity, and increase quality of life in the elderly cardiac population (Angevaren, Aufdemkampe, Verhaar, Aleman, & Vanhees, 2008; Church, Earnest, Skinner, & Blair, 2007; Corrà et al., 2010; Gu & Conn, 2008; Johnson, Lim, & Bowe, 2009; Liu-Ambrose et al., 2005). Despite the compelling evidence of their benefits, few studies have evaluated the cost effectiveness of these interventions (Mller-Riemenschneider, 2009), and as a result, they are not being translated into practice. More women are expected to have CABS because of their longer lifespan and the diminished cardiac protective factors after menopause (Bypass Surgery in Women, 2010). Given that women tend to have suboptimal outcomes and higher health care costs following CABS (Ahmed, Tully, Knight, & Baker, 2011; Cartier, Bouchot, & El-Hamamsy, 2008; Czech et al., 2007; Duvernoy et al., 2010; Katircibasi et al., 2007; Maganti, Rao, & Cusimano, 2009; Patel, Smith, & Engel, 2006; Siegrist et al., 2008; Williams, Trivedi, Doughtie, & Slaughter, 2011), it is important for the patients, providers, health care payers, and policymakers to identify a cost-effective recovery intervention that has the potential to increase women’s physical activity and functioning during their early recovery from CABS, especially in this time of limited health care resources.
The overall purpose of this secondary analysis study was to evaluate the cost effectiveness of a 6-week early recovery symptom management (SM) intervention delivered by telehealth device to improve the physical activity level of women following CABS. To determine the cost effectiveness of the SM intervention, the cost-effectiveness analysis (CEA) was conducted to compute the incremental cost-effectiveness ratio (ICER), using physical activity as the outcome measure. The parent study was a randomized control trial (RCT) that reported a SM intervention delivered by a telehealth device improved physical activity measures (daily estimated energy expenditure [EEE] and minutes spent on moderate-to-vigorous intensity activity) in female patients who had undergone CABS (Zimmerman, 2011); therefore, only women were used in this secondary analysis.
The specific aims of the study were to:
-
Determine the differences in physical activity measures between SM and usual care (UC) groups for women at 3 months following CABS.
Determine the differences in daily estimated energy expenditure (EEE; Kcal/kg) between groups.
Determine the differences in minutes spent on activity of moderate-to-vigorous intensity (minutes/day) between groups.
Determine the differences in the health care costs between the SM and UC groups for women at 3 months following CABS, including the direct costs of the SM intervention and the potential savings due to the intervention.
-
Determine the ICER of the SM intervention for women at 3 months following CABS on the following physical activity measures:
Daily EEE (dollars/[Kcal/{Kg*day}]).
Minutes spent on activity of moderate-to-vigorous intensity per day (dollars/[minutes/day]).
BACKGROUND AND SIGNIFICANCE
The Cost-Effectiveness of the Intervention
Cost effectiveness is defined as the additional dollars spent on the intervention to gain one unit of effectiveness in a selected health outcome (Drummond, Sculpher, Torrance, O’Brien, & Stoddart, 2005) (physical activity was used in this study). Using Drummond’s economic evaluation model, the cost effectiveness is expressed as the incremental cost-effectiveness ratio (ICER), which is the ratio of the incremental costs (Δ costs) to the incremental effectiveness (Δ effectiveness) resulting from the intervention compared to no intervention (Drummond et al., 2005). The intervention with a lower ICER is considered more cost effective because it produces equivalent or greater effectiveness with lower costs (Drummond et al., 2005). Specific to the analysis in this study, we defined the incremental costs of the SM intervention (Δ costs) as the difference in the costs of post CABS care between the SM and UC groups. The incremental effectiveness of the SM intervention (Δ effectiveness) is defined as the difference in the physical activity measures between the SM and UC groups. In summary, the incremental ICER of the SM intervention is the ratio of the incremental costs (Δ costs) to the incremental effectiveness (Δ effectiveness) in the physical activity measures associated with the SM intervention.
The Need to Conduct a Cost-Effectiveness Evaluation
Compared to men, women have been identified as a vulnerable group of CABS patients that tend to have poorer outcomes after CABS, such as lower physical functioning levels (Guru, Fremes, Austin, Blackstone, & Tu, 2006; Vaccarino et al., 2003a), higher symptom burden (Sawatzky & Naimark, 2009a), and higher health care expenditures related to CABS (Bestawros, Filion, Haider, Pilote, & Eisenberg, 2005; Dolansky et al., 2010; Murphy et al., 2008; Saleh, Racz, & Hannan, 2009; Sawatzky & Naimark, 2009a; Swaminathan et al., 2009). Previous nursing interventions are effective in improving both men and women’s symptoms (Deyirmenjian, Karam, & Salameh, 2006; Lie, Arnesen, Sandvik, Hamilton, & Bunch, 2007; Rollman, Schulberg, & Reynolds, 2010; Utriyaprasit, Moore, & Chaiseri, 2010), physical activity and functioning (Eder, 2010; Rollman et al., 2010; Utriyaprasit et al., 2010), self-care and monitoring ability (Cebeci & Celik, 2008; Doering, Cross, Vredevoe, Martinez-Maza, & Cowan, 2007; Kleinpell & Avitall, 2007), and health-related quality of life (HRQoL) (Freedland et al., 2009; Rollman et al., 2010), in addition to reducing their health care utilization (HCU) costs (Diez, Korb, Waehner, Silber, & Niemann, 2006).
The proportion of female CABS patients is expected to increase dramatically because women are projected to account for 65% of the older population in 2030 (Centers for Disease Control and Prevention, 2009), which poses significant financial and care burdens to society and their families (Bestawros et al., 2005). With health care resources becoming more limited, it is critical to examine the cost effectiveness of the interventions targeting post-CABS populations before implementing them. In summary, conducting the evaluation of the interventions will help distribute scarce health care resources cost effectively, prioritize the resources to the most vulnerable populations (e.g., women), and accelerate the clinical translation of research findings.
Physical Activity Measures to Assess the Effectiveness of the Intervention
To determine the cost effectiveness of the intervention, the information regarding the effectiveness of the intervention needs to be assessed first. The effectiveness of the intervention is defined as the degree of the improved health state (e.g., physical activity and functioning) caused by the intervention (Drummond et al., 2005). According to Drummond’s theory, effectiveness can be measured as a final health outcome (e.g., life-years gained, disease-free days) or intermediate outcome (e.g., improved cholesterol levels, improved physical activity levels) (Drummond et al., 2005). When the final health outcome measure is not available, which is very common in nursing intervention studies, the effectiveness can be measured by an intermediate outcome that is related to a final health outcome (Drummond et al., 2005).
The parent study demonstrated that the SM intervention improved the physical activity of women following CABS (Zimmerman et al., 2007; Zimmerman, 2011). In the older cardiac population, consistent evidence has supported that physical activity, an intermediate outcome, is associated with the final health outcomes, such as all-cause mortality (Kruk, 2007; Mullen, 2006; Weisser, Preuss, & Predel, 2009), recurrent cardiac events (Conn, Hafdahl, Moore, Nielsen, & Brown, 2009), and HRQoL (Conn et al., 2009). In post-menopausal women, improved physical activity was associated with reduced risk for many health conditions, including cardiovascular disease (cardiovascular disease [CVD]; 28%–58% reduction) (Brown, Burton, & Rowan, 2007; Pines & Berry, 2007; Pines, 2009); diabetes (14%–46% reduction) (Brown et al., 2007); breast cancer (11%–75% reduction) (Pines, 2009); endometrial cancer (68%–90% reduction) (Brown et al., 2007); colon cancer (31%–46% reduction) (Brown et al., 2007); fall and hip fracture (45% reduction) (Moayyeri, 2008); depression (22%–46% reduction) (Pines, 2009); and cognitive impairment (1.3%–2% reduction) (Pines, 2009). Increased physical activity also contributes to improvements in other intermediate outcomes that are known cardiac risk factors, such as body mass index (BMI), body fat composition (Dalleck, Borresen, Wallenta, Zahler, & Boyd, 2008), carbohydrate handling and lipid profile (Dalleck et al., 2008; Kemmler et al., 2007), and blood pressure (Dalleck et al., 2008). Improvements in these intermediate outcomes lead to improved final health outcomes such as mortality and morbidity of CVD. Compared to sedentary women, active women have a 40% decrease in age-adjusted relative risk for cardiovascular events (Pines & Berry, 2007). Daily EEE and time spent on activity of moderate-to-vigorous intensity are most frequently used to measure physical activity (Manini et al., 2006) because of the strong association with final health outcomes, such as mortality, HRQoL, and CVD risk (Church et al., 2007; Della Valle, Grimaldi, & Farinaro, 2008; Gruppo di Lavoro della Societa Italiana di Cardiologia, 2007; Manini et al., 2006). In the post-CABS population, these physical activities measures were strong indicators of early convalescence (Vogel et al., 2009; Zimmerman & Barnason, 2007). In summary, using physical activity measures to assess the effectiveness of the SM intervention is meaningful and relevant to women’s final health outcomes following CABS.
Health Care Costs of the Intervention
Cost is defined as the resource consumed by the intervention, including health care costs, patient costs, and other costs (e.g., meal delivery and housekeeping services) (Drummond et al., 2005). What costs to consider in a CEA depends on what viewpoint or perspective is being used to guide the analysis. Drummond suggests using the societal perspective as the first choice because it provides the most comprehensive cost information and is the most relevant to the objective of evaluation, such as informing decision on resource allocation to improve health in the society as a whole (Drummond et al., 2005). A comprehensive review of the CABS-related studies indicated that the HCU costs have been predominately used to reflect the costs of the interventions related to CABS and associated followup care (Ketcham & Furukawa, 2008; Kurki, Hakkinen, Lauharanta, Ramo, & Leijala, 2001; Saleh et al., 2009; Speir, Kasirajan, Barnett, & Fonner, 2009; Swaminathan et al., 2009). The health care utilization costs are commonly defined as the costs of outpatient visits (Porter, 1998), emergency department (ED) visits (Sawatzky & Naimark, 2009b), and hospitalizations (Speir et al., 2009). Medicare reimbursement rates are considered best estimates of HCU costs in the older population (Barnett, 2009; Konski et al., 2008; Tumeh, Moore, Shapiro, & Flowers, 2005) because (a) Medicare is the largest payer of health care expenditure in the older adult population; (b) other public and private insurers follow Medicare reimbursement methodology; and (c) Medicare is supported and regulated by U.S. taxes, which is most representative of public interest and societal perspective (Tumeh et al., 2005). In conclusion, the cost of the SM intervention can be defined as the direct costs of the SM program and the potential savings of HCU costs due to the SM intervention as compared to the UC group. The savings of HCU costs related to post-CABS care are the differences in Medicare reimbursements of HCU costs between SM and UC groups. Since Medicare reimbursement is used to assess the HCU costs related to post-CABS care; this also represents the closest estimation of HCU costs from a societal perspective (Tumeh et al., 2005). Therefore, the analysis presented in this study is presented from the societal perspective.
METHODS
Design
The parent study was a two-group, repeated-measure RCT examining the effect of an SM intervention on recovery outcomes (symptoms, physical activity, and functioning) following CABS. The intervention group (n=109) received the SM intervention delivered by a telehealth device called Health Buddy® (manufactured by Health Hero Network, Palo Alto, CA) for 6 weeks (42 daily sessions) in the patients’ homes, in addition to the usual followup care. The UC group (n=123) received the routine followup care provided by the primary providers and cardiac specialists (which was a 2-week followup call). The detailed information regarding the intervention and the measures can be reviewed in the previously published manuscript (Barnason, Zimmerman, Nieveen et al., 2009). The parent study did not find any significant differences in the physical activity and functioning between the SM and UC groups (Barnason Zimmerman, Nieveen et al., 2009). However, the SM intervention was effective in improving selected symptoms (fatigue, depression, sleep problems, and pain) and physical activity in women only (Zimmerman et al., 2007; Zimmerman, 2011). Therefore, the analysis (CEA) was conducted in all the female subjects from the parent study (SM=23, UC=17).
Study Model
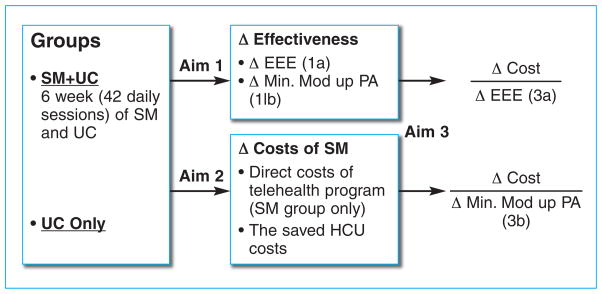
The SM intervention was designed to improve women’s symptoms and physical activity measures. Aim 1 tested whether the SM and UC groups differed in two physical activity measures: daily EEE (Aim 1a) and the minutes spent on moderate-to-vigorous activity (Aim 1b). In general, symptoms and physical activity levels are the primary sources of health care utilization in older adults (Clarke, 2010). Therefore, the assumption was made that if the SM intervention were to improve patients’ symptoms and functioning, the costs of HCU for post-CABS care would be reduced and/or saved (Barnason, Zimmerman, Schulz, & Tu, 2009). Aim 2 tested whether there were differences in the costs of HCU between SM and UC groups. In Aim 3, the incremental costs (Δ costs) and incremental effectiveness (Δ effectiveness) caused by the SM intervention were used to compute the incremental cost-effectiveness ratio for each physical activity measure, which reflect the cost effectiveness of the SM intervention. The incremental costs of the SM intervention (Δ costs) included the direct costs of the telehealth program in the SM group and the HCU costs saved by the SM intervention. The incremental effectiveness (Δ effectiveness) was the difference in physical activity measures between SM and UC groups. To calculate the ICER, the numerator was the incremental costs of the SM intervention (Δ costs). The denominator was figured in two ways: the incremental daily EEE (Δ EEE) and the incremental minutes spent on moderate-to-vigorous activity (Δ min. mod up PA) (see Figure 1).
Figure 1.
Study Framework
Variables and Measures
Demographic and patient characteristics
A demographic and patient characteristic tool was used to collect the background and clinical information to describe the sample (e.g., age, income, co-morbidity, etc.).
Physical activity measures
The 3-day Physical Activity and Exercise Diary, a self-report instrument designed for the parent study, was used to collect post-discharge activity at 3 months after CABS. Subjects recorded the amount of time they spent in sleep and in light, moderate, and vigorous activities. The average daily minutes spent in activities of moderate-to-vigorous intensity were computed by averaging these minutes for the 3 days. Duration and metabolic equivalent of task value for each level of physical activity was used to calculate the daily EEE (Kcal/Kg*day) (Barnason, Zimmerman, Nieveen et al., 2009). The correlation of total EEE produced by the 3-day activity diary and the accelerometer (RT3) in this population was 0.77 at 3 weeks, 0.72 at 6 weeks, and 0.57 at 3 months, which provides evidence that the self-reported activity level was a valid assessment of physical activity (Hertzog et al., 2007).
Costs of the SM intervention
The incremental costs of SM intervention are the differences in the costs of post-CABS care at 3 months after surgery between SM and UC groups, including the direct costs of the telehealth program and the savings on HCU costs due to the SM intervention (Aim 2). The incremental costs of SM are used to compute ICER (Aim 3).
Direct costs
Direct costs of the SM program include: (a) the cost of the telehealth device per subject (one-time hook-up fee and monthly service fee), which is collected from monthly rental statements for the Health Buddy and receipts of the initial hook-up fee, and (b) the wage of the registered nurse (RN) who managed the telehealth program. The RN’s wage was calculated by multiplying the hourly wage by the time spent per subject. A daily log was used to record the time (to the closest minute) the RN spent on each subject for monitoring, followup phone calls, and troubleshooting tasks during the 6-week intervention period. The RN’s hourly wage was $26.76 for RNs in Nebraska during the intervention period (Bureau of Labor Statistics, 2003, 2004, 2005, 2006).
HCU savings
The improved symptoms and physical functioning resulting from the SM intervention has the potential to reduce the need for patients to access health care services for followup care regarding their post CABS problems and concerns. The HCUs surveyed in the previous RCT included outpatient visits (physician office visits and hospital outpatient visits), ED visits, and hospital readmissions. The costs of HCU were operationalized as Medicare reimbursements for each type of service. The costs of physician office visits were collected with the Center for Medicare and Medicaid Services Claim Form (CMS-1500), and the costs of hospital-based services (hospital outpatient service, ED visits, and re-admission) were collected with the Uniform Billing Form (UB-92). If there were no savings on HCU costs, the incremental costs of the SM intervention would be the direct costs of the telehealth program.
Procedure
Prior to data analysis, institutional review board approval was obtained at the University of Nebraska Medical Center. Physical activity variables (daily EEE and minutes spent on moderate-to-vigorous activity) at 3 months after CABS were available in the parent study’s database. For cost data, all health care costs were evaluated for inclusion based on the diagnosis codes (ICD-9) and date of service (up to 3 months after CABS). The health care costs were included if at least one diagnostic code (ICD-9) indicated the visit was for the following conditions or treatment: (a) heart diseases (414.00–99); (b) risk factors or conditions that contribute to heart diseases (e.g., 401 for hypertension, 250 for diabetes, 272 for lipoid metabolic disorders, etc.); (c) postoperative complications (e.g., 427.3 for atrial fibrillation, v58.61 for anticoagulant therapy, 280 for anemia, 428 for heart failure, etc.); and (d) post-CABS followup care (e.g., v45.81).
To calculate the costs of outpatient visits, Current Procedural Terminology codes (CPT) were used to compute Medicare reimbursements based on the physician fee schedule published by the CMS (2009a). The costs of laboratory and diagnostic testing were computed using the Medicare clinical diagnostic laboratory fee schedule published on the CMS web site (CMS, 2009b). Ambulatory Payment Classifications codes (APC) were used to compute Medicare reimbursements for ED visits (CMS, 2009c). The APC code assigned to each service was based on the procedural codes (CPT) listed in Medicare billing form UB-92 (CMS, 2009d). For each hospital re-admission cost, the diagnosis-related group code obtained from form UB-92 was used to calculate the specific Medicare payment rate using Prospective Payment System Pricer software published on the CMS web site (CMS, 2009e). All the costs were adjusted to 2009 U.S. dollars.
Data Analysis
Descriptive statistics were used to describe the women’s background and clinical information. Normality testing (Shapiro-Wilk test) indicated significant non-normal distributions for both HCU cost (p=0.01) and physical activity outcome measures (p= 0.02), thus nonparametric testing (Mann-Whitney U test) was used to determine if there were differences in the physical activity measures (Aim 1) and health care costs (Aim 2) between SM and UC groups for women at 3 months following CABS. Due to the small sample size of women (n=40), the significance level of p values was set at 0.10 for Aim 1 and 2. The analysis (CEA) was conducted to determine the ICER of the SM intervention (Aim 3). The ICER was computed for each physical activity measure: daily EEE (Aim 3a) and the minutes spent on moderate-to-vigorous intensity activity (Aim 3b). To follow the principle of conducting the CEA, the mean differences in the costs and physical activity measure between the groups were used to calculate the increments in the costs and effectiveness associated with the SM intervention (Drummond et al., 2005).
RESULTS
Sample Profile
The women (SM=23, UC=17) in this analysis had a mean age of 72 (SD=5.41), 13 (SD=2.18) years of education, and an annual household income of $30,295 (SD=$20,259). The majority was White (97.5%), married (55%), retired (75%), had Medicare benefits (93%), and lived in a rural community (73%). From a clinical perspective, they were all first-time CABS patients. Most were classified as New York Heart Classification I–II (90%), having an average ejection fraction of 57% (SD=10.76%). The average BMI was 28.63 (SD=5.05), and the average baseline physical functioning (Duke Activity Status Index or DASI) score was 25.36 (SD=12.22). There were no significant differences between the SM and UC groups on demographic or clinical variables.
Aim 1: Determine the Differences in Physical Activity Outcomes between SM and UC Groups
Aim 1a: Determine the differences in daily EEE (Kcal/kg*day) between groups
The median daily EEE was 24.67 Kcal/kg (range: 21.33–36.48) for the SM group and 23.45 Kcal/kg (range: 21.85–34.05) for the UC group. The nonparametric test (Mann-Whitney) showed a significant difference (Mann-Whitney U=97.0, df=3, p<0.10) in this measure between the SM and UC groups at 3 months after surgery. The mean difference of daily EEE between SM and UC groups was 2.16 kcal/kg (see Table 1), which were used to calculate the incremental effectiveness for ICER of daily EEE (Aim 3a).
Table 1.
ICER of the SM Intervention for Women at 3 Months after CABS
| SM (n=23) | UC (n=17) | Δ Cost or Δ Effectiveness | ICER | |
|---|---|---|---|---|
| Cost of SM (dollars) | $10.33 | 0 | $10.33 | $0.17/minute |
| Mean time spent on moderate-to-vigorous activity per day (minutes) | 165 | 104 | 61 | ($5.10/30 minutes or $10.20/hour) |
| Mean energy expenditure per day (Kcal/kg) | 27.19 | 25.03 | 2.16 | $4.78/kcal/kg |
SM = symptom management
UC = usual care
ICER = incremental cost-effectiveness ratio
Aim 1b: Determine the differences in minutes spent on moderate-to-vigorous intensity activity (minutes/day) between groups
The median time spent on moderate-to-vigorous intensity physical activity was 120 minutes (range: 10–410 minutes) for the SM group and 55 minutes (range: 15–350 minutes) for the UC group at 3 months after surgery. Mann-Whitney U results indicated a significant difference (Mann-Whitney U=97.5, df=3, p<0.10) in this measure between the SM and UC groups at 3 months after surgery. The mean difference of minutes spent on moderate-to-vigorous intensity activity between SM and UC groups was 61 minutes per day (see Table 1), which was used to compute the incremental effectiveness for ICER of minutes spent on moderate-to-vigorous activity (Aim 3b).
Aim 2: Determine the Differences in the Costs of Post-CABS Care between SM and UC Groups
The median costs of HCU for followup care were $399 (range: $60–$14,362) for the SM group and $267 (range: $60–$15,345) for the UC group. Mann-Whitney U results showed no significant difference (Mann-Whitney U=181, p=0.691) in these costs between groups at 3 months. Since there were no savings on HCU costs, the incremental costs of the SM intervention were simplified as the direct costs of the telehealth program. The costs of the SM program per subject consisted of the Health Buddy’s one-time hook-up fee ($100) and monthly service fee ($56 for 42 days), the RN’s wages, the costs of followup phone calls (long distance only), and the costs of troubleshooting services. The average RN’s wage was calculated by multiplying the RN’s hourly wage by time spent managing the SM program for each subject (daily minutes multiplied by 42 days), which was $276.30 per subject during the intervention period. The average cost of long distance phone calls was $10.56 per subject. The average cost for troubleshooting services was $1.20 per subject. In sum, the average cost of the SM intervention per subject for 6-week intervention period was $434.06 or $10.33 per day for each subject.
Aim 3: Determine the ICER of SM Intervention
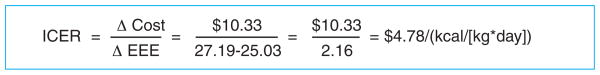
Aim 3a: Determine the ICER for daily EEE (Dollars/[Kcal/{Kg*day}])
For daily EEE, the ICER was $4.78/(Kcal/[kg*day]), which means the cost of the SM intervention to gain one Kcal/kg EEE was $4.78 per day for each woman in the SM group. The calculation is Figure 2.
Figure 2.
Calculation for Determining the ICER for Daily EEE
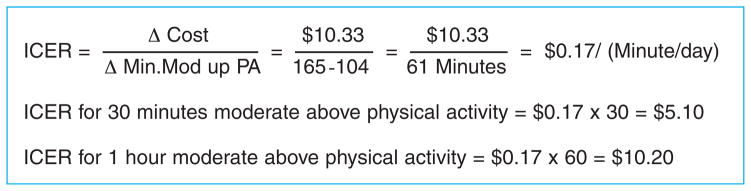
Aim 3b: Determine the ICER for minutes spent on moderate-to-vigorous intensity activity per day (Dollars/[Minutes/day])
For the minutes spent on physical activity of moderate-to-vigorous intensity per day, the ICER was $0.17/(minutes/day), or $5.10/(30 minutes/day), or $ 10.20/(hour/day), which means the additional cost of the SM intervention to add 30 minutes of moderate-to-vigorous intensity activity was $5.10 or $10.20 for an hour per day for each woman in the SM group (see Table 1 & Figure 3).
Figure 3.
ICER for 30 Minutes and 1 Hour
LIMITATIONS
The following are limitations of this study: (a) the study is not fully powered to produce significant findings due to its small sample size (n=40), (b) generalizability of these results to the greater female CABS population is limited by the convenience sampling from U.S. Midwestern regions only and the lack of diversity, and (c) the results are limited by using self-report for measuring physical activity. Additionally, comparability of our results is substantially limited because of the lack of studies in the literature related to cost effectiveness of a telehealth intervention for post-CABS patients.
DISCUSSION
Results from this study must be interpreted cautiously, as findings were based on a secondary analysis and the parent study was not powered for a gender by group difference analysis. However, study findings do show promise for the SM intervention delivered by telehealth device to be cost effective to improve the older women’s physical activity level after their bypass surgeries. The cost of increasing 30 minutes of moderate-to-vigorous intensity physical activity was $5.10 per day per patient at 3 months after bypass surgery. The cost to gain one Kcal/kg*day estimated energy expenditure was $4.78 for each woman at 3 months after surgery.
To date, this is the first study to examine the cost effectiveness of using a home-based telehealth intervention to improve physical activity outcomes in older women during the early stage of their recovery after CABS (3 months). The cost effectiveness of nursing interventions targeting the post-cardiac surgical population has not been reported, which restricts us from comparing results across similar interventions. As reported by a recent meta-analysis, the average increase of physical activity measures caused by physical activity interventions were 368.9 Kcal/week (52.7 Kcal/day, 0.70 Kcal/kg*day) for EEE or 48 minutes/week (7 minutes/day) for moderate-to-vigorous physical activity level (Conn, 2008; Conn et al., 2009). Our study findings indicate that women in the intervention group had a increase of 2.16 Kcal/kg in daily EEE and a 61-minute increase in moderate-to-vigorous intensity activity per day compared to women from the usual care group. Unfortunately, the incremental cost-effectiveness ratios for physical activity measures have not been reported in cardiac populations (including post-cardiac surgery patients), nor have they addressed any potential gender disparities. However, compared to the physical activity interventions conducted in the general population, the SM intervention may be cost effective, given a cost of $5.10 per 30 minutes of increase in moderate-to-vigorous activity per day in the post-CABS population.
To bring substantial health benefits, the older adults should do at least 150 minutes a week of moderate-to-vigorous intensity activity (U.S. Department of Health and Human Services, 2008). From a practical perspective, for as little as $5.00 a day, older women in the early recovery stage after bypass surgery were able to meet this physical activity goal. For post-menopausal women, a minimal 150 minutes a week of moderate-to-vigorous intensity physical activity is associated with an 18%–24% risk reduction for recurrent cardiovascular events, an annual savings of $2,581 ($7.071 per day) in per capita medical expenses for CVD, a 37% risk reduction for CVD-related hospitalization, and a 55% risk reduction for CVD death (Albright & Thompson, 2006).
The results of the study have several important implications for nursing practice:
It is possible to deliver an effective nursing intervention in the community setting with low cost. The nurse plays an important role in developing and implementing the cost-effective home-based nursing interventions to improve postoperative outcomes in CABS. The U.S. health care system is shifting from hospital to community settings as evidenced by the shorter length of hospital stay after cardiac surgery (Bohmer, Newell, & Torchiana, 2002; Honey & North, 2008). At the same time, the aging of the U.S. population contributes to the growing numbers of people with chronic, complex diseases, and high prevalence of co-morbidities (Honey & North, 2008; Schofield et al., 2011). Therefore, there is increasing expectation that patients can recover safely and effectively at home with the assistance of community-based nursing care that is cost effective (Schofield et al., 2011).
The results of the study provide some evidence of cost effectiveness of this nursing intervention aimed to promote physical activity level in post-CABS women. A larger study designed for women is warranted before further implications can be derived to support the development of recovery guidelines for women who have undergone heart surgery.
In comparison to medical and pharmaceutical interventions, few nursing interventions have been directly reimbursed by either federal or private insurers due to the lack of evidence related to cost effectiveness of nursing interventions (Spetz, 2005). Therefore, it is essential nurses participate in cost-effectiveness studies that demonstrate the value of nursing interventions.
This study provides a basic understanding of conducting a cost-effectiveness analysis. This type of cost analysis is relevant to the scope of practice of nursing leaders, and they can use it as a fundamental tool to assist decision making on the distribution of resources (Douglas & Normand, 2005). The CEA specifically may provide nursing leaders with methods to determine the cost effectiveness of interventions, which helps reduce unnecessary health care expenditure, effectively allocates limited health care resources, and leads to improved quality of care (Dochterman et al., 2010).
CONCLUSION
This home-based symptom management intervention has the potential to reduce the risk of recurrent cardiac events and health care cost by improving women’s physical activity level after surgery. Being the first study to assess the cost effectiveness of a nursing SM intervention delivered to post-CABS older women, we are unable to compare it to other similar interventions and determine if our intervention is more cost effective than other interventions. More nursing interventions need to be evaluated in relation to their cost effectiveness. This information is vital to nursing leaders in making resource decisions regarding followup care of women who have had heart surgery.
Executive Summary.
Older women have lower levels of physical functioning and higher associated health care costs than men after coronary artery bypass surgery (CABS).
Clinical trials have demonstrated that interventions to increase physical activity levels can reduce the risk of recurrent cardiac events, reduce health care expenditures, prolong life, improve functional capacity, and increase quality of life in the elderly cardiac population.
It is important for the patients, providers, health care payers, and policymakers to identify a cost-effective recovery intervention that has the potential to increase women’s physical activity and functioning during their early recovery from CABS, especially in this time of limited health care resources.
This home-based symptom management intervention has the potential to reduce the risk of recurrent cardiac events and health care cost by improving women’s physical activity level after surgery.
This information is vital to nursing leaders in making resource decisions regarding followup care of women who have had heart surgery.
Contributor Information
Lufei Young, Assistant Professor, University of Nebraska Medical Center, College of Nursing, Lincoln, NE.
Lani Zimmerman, Professor, University of Nebraska Medical Center, College of Nursing, Lincoln, NE.
Bunny Pozehl, Professor, University of Nebraska Medical Center, College of Nursing, Lincoln, NE.
Susan Barnason, Professor, University of Nebraska Medical Center, College of Nursing, Lincoln, NE.
Hongmei Wang, Assistant Professor, Department of Health Services Research, University of Nebraska Medical Center, College of Public Health, Omaha, NE.
References
- Ahmed WA, Tully PJ, Knight JL, Baker RA. Female sex as an independent predictor of morbidity and survival after isolated coronary artery bypass grafting. The Annals of Thoracic Surgery. 2011;92(1):59–67. doi: 10.1016/j.athoracsur.2011.02.033. [DOI] [PubMed] [Google Scholar]
- Albright C, Thompson DL. The effectiveness of walking in preventing cardiovascular disease in women: A review of the current literature. Journal of Women’s Health. 2006;15(3):271–280. doi: 10.1089/jwh.2006.15.271. [DOI] [PubMed] [Google Scholar]
- Angevaren M, Aufdemkampe G, Verhaar HJ, Aleman A, Vanhees L. Physical activity and enhanced fitness to improve cognitive function in older people without known cognitive impairment. Cochrane Database of Systematic Reviews. 2008;3(3):CD005381. doi: 10.1002/14651858.CD005381.pub3. [DOI] [PubMed] [Google Scholar]
- Barnason S, Zimmerman L, Schulz P, Tu C. Influence of an early recovery telehealth intervention on physical activity and functioning after coronary artery bypass surgery among older adults with high disease burden. Heart & Lung: The Journal of Critical Care. 2009;38(6):459–468. doi: 10.1016/j.hrtlng.2009.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnason S, Zimmerman L, Nieveen J, Schulz P, Miller C, Hertzog M, Tu C. Influence of a symptom management telehealth intervention on older adults’ early recovery outcomes after coronary artery bypass surgery. Heart & Lung: The Journal of Acute and Critical Care. 2009;38(5):364–376. doi: 10.1016/j.hrtlng.2009.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett PG. An improved set of standards for finding cost for cost-effectiveness analysis. Medical Care. 2009;47(7):S82–S88. doi: 10.1097/MLR.0b013e31819e1f3f. [DOI] [PubMed] [Google Scholar]
- Bestawros A, Filion KB, Haider S, Pilote L, Eisenberg MJ. Coronary artery bypass graft surgery: Do women cost more? The Canadian Journal of Cardiology. 2005;21(13):1195–1200. [PubMed] [Google Scholar]
- Bohmer RM, Newell J, Torchiana DF. The effect of decreasing length of stay on discharge destination and readmission after coronary bypass operation. Surgery. 2002;132(1):10–15. doi: 10.1067/msy.2002.125358. [DOI] [PubMed] [Google Scholar]
- Brown WJ, Burton NW, Rowan PJ. Updating the evidence on physical activity and health in women. American Journal of Preventive Medicine. 2007;33(5):404–411. doi: 10.1016/j.amepre.2007.07.029. [DOI] [PubMed] [Google Scholar]
- Bureau of Labor Statistics. Occupational employment and wages. 2003 Retrieved from http://www.bls.gov/oes/2003/november/oes291111.htm.
- Bureau of Labor Statistics. Occupational employment and wages. 2004 Retrieved from http://www.bls.gov/oes/2004/november/oes291111.htm.
- Bureau of Labor Statistics. Occupational employment and wages. 2005 Retrieved from http://www.bls.gov/oes/2005/may/oes291111.htm.
- Bureau of Labor Statistics. Profile for registered nurses. 2006 Retrieved from http://www.bls.gov/oes/2006/may/figure8.pdf.
- Bypass Surgery in Women. Treatment: New surgical options for treating women’s coronary artery disease. 2010 Retrieved from http://my.cleve-landclinic.org/heart/women/treatment_cabg.aspx.
- Cartier R, Bouchot O, El-Hamamsy I. Influence of sex and age on long-term survival in systematic off-pump coronary artery bypass surgery. European Journal of Cardio-Thoracic Surgery. 2008;34(4):826–832. doi: 10.1016/j.ejcts.2008.07.024. [DOI] [PubMed] [Google Scholar]
- Cebeci F, Celik SS. Discharge training and counseling increase self-care ability and reduce postdischarge problems in CABG patients. Journal of Clinical Nursing. 2008;17(3):412–420. doi: 10.1111/j.1365-2702.2007.01952.x. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) Women’s health. 2009 Retrieved from http://www.cdc.gov/women.
- Centers for Medicare and Medicaid Services (CMS) Physician fee schedule. 2009a Retrieved from http://www.cms.hhs.gov/pfslookup/02_PFSsearch.asp?agree=yes&next=Accept.
- Centers for Medicare and Medicaid Services (CMS) Clinical laboratory fee schedule. 2009b Retrieved from http://www.cms.hhs.gov/ClinicalLabFeeSched/02_clinlab.asp#TopOfPage.
- Centers for Medicare and Medicaid Services (CMS) Hospital outpatient PPS. 2009c Retrieved from http://www.cms.hhs.gov/HospitalOutpatientPPS/AU/list.asp#TopOfPage.
- Centers for Medicare and Medicaid Services (CMS) Pass-through payment status and new technology ambulatory payment classification (APC) 2009d Retrieved from http://www.cms.gov/HospitalOutpatientPPS/04_passthrough_payment.asp#TopOfPage.
- Centers for Medicare and Medicaid Services (CMS) Inpatient prospective payment system (PPS) pricer. 2009e Retrieved from https://www.cms.gov/PCPricer/03_inpatient.asp#TopOfPage.
- Church TS, Earnest CP, Skinner JS, Blair SN. Effects of different doses of physical activity on cardiorespiratory fitness among sedentary, overweight or obese post-menopausal women with elevated blood pressure: A randomized controlled trial. JAMA. 2007;297(19):2081–2091. doi: 10.1001/jama.297.19.2081. [DOI] [PubMed] [Google Scholar]
- Clarke SP. Healthcare utilization. In: Sibley A, editor. Nursing outcomes. 2. Sudbury, MA: Jones & Bartlett Learning; 2010. pp. 439–485. [Google Scholar]
- Conn VS. Meta-analysis of patient education interventions to increase physical activity among chronically ill adults. Patient Education and Counseling. 2008;70(2):157. doi: 10.1016/j.pec.2007.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conn VS, Hafdahl AR, Cooper PS, Ruppar TM, Mehr DR, Russell CL. Interventions to improve medication adherence among older adults: Meta-analysis of adherence outcomes among randomized controlled trials. The Gerontologist. 2009;49(4):447–462. doi: 10.1093/geront/gnp037. [DOI] [PubMed] [Google Scholar]
- Conn VS, Hafdahl AR, Moore SM, Nielsen PJ, Brown LM. Meta-analysis of interventions to increase physical activity among cardiac subjects. International Journal of Cardiology. 2009;133(3):307–320. doi: 10.1016/j.ijcard.2008.03.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corrà U, Piepoli MF, Carré F, Heuschmann P, Hoffmann U, Verschuren M, Schmid P. Secondary prevention through cardiac rehabilitation: Physical activity counseling and exercise training. European Heart Journal. 2010;31(16):1967–1974. doi: 10.1093/eurheartj/ehq236. [DOI] [PubMed] [Google Scholar]
- Czech B, Kucewicz-Czech E, Pacholewicz J, Wojarski J, Puzio J, Przybylski R, Zembala M. Early results of coronary artery bypass graft surgery in women. Kardiologia Polska. 2007;65(6):627–633. [PubMed] [Google Scholar]
- Dalleck LC, Borresen EC, Wallenta JT, Zahler KL, Boyd EK. A moderate-intensity exercise program fulfilling the American College of Sports Medicine net energy expenditure recommendation improves health outcomes in premenopausal women. Journal of Strength and Conditioning Research. 2008;22(1):256–262. doi: 10.1519/JSC.0b013e31815f9246. [DOI] [PubMed] [Google Scholar]
- Della Valle E, Grimaldi R, Farinaro E. Importance of physical activity for prevention of chronic diseases [L’importanza dell’attivita fisica nella prevenzione delle malattie cronico degenerative] Annali Di Igiene: Medicina Preventiva e Di Comunita. 2008;20(5):485–493. [PubMed] [Google Scholar]
- Deyirmenjian M, Karam N, Salameh P. Preoperative patient education for open-heart patients: A source of anxiety? Patient Education and Counseling. 2006;62(1):111–117. doi: 10.1016/j.pec.2005.06.014. [DOI] [PubMed] [Google Scholar]
- Diez C, Korb H, Waehner M, Silber RE, Niemann B. Telemedical monitoring of electrocardiograms after cardiac surgery — Results from a pilot study among 208 patients[Telemedizinisches EKG-Monitoring nach herzchirurgischen Operationen: Ergebnisse einer Pilotstudie mit 208 Patienten] Herzschrittmachertherapie & Elektrophysiologie. 2006;17(4):191–196. doi: 10.1007/s00399-006-0531-z. [DOI] [PubMed] [Google Scholar]
- Dochterman JM, Bulechek G, Head B, Ahrens D, Androwich I, Clarke M, Cullen P, Vlasses F. Determining cost of nursing interventions: A beginning. Nursing Economic$ 2010;19(4):146–160. [Google Scholar]
- Doering LV, Cross R, Vredevoe D, Martinez-Maza O, Cowan MJ. Infection, depression, and immunity in women after coronary artery bypass: A pilot study of cognitive behavioral therapy. Alternative Therapies in Health and Medicine. 2007;13(3):18–21. [PubMed] [Google Scholar]
- Dolansky MA, Xu FM, Zullo MA, Shishehbor MD, Moore SM, Rimm AA. Post-acute care services received by older adults following a cardiac event: A population-based analysis. Journal of Cardiovascular Nursing. 2010;25(4):342–349. doi: 10.1097/JCN.0b013e3181c9fbca. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Douglas HR, Normand C. Economic evaluation: What does a nurse manager need to know? Journal of Nursing Management. 2005;13(5):419–427. doi: 10.1111/j.1365-2834.2005.00586.x. [DOI] [PubMed] [Google Scholar]
- Drummond MF, Sculpher MJ, Torrance GW, O’Brien BJ, Stoddart GL. Methods for the economic evaluation of health care programmes. 3. London, England: Oxford University Press; 2005. [Google Scholar]
- Duvernoy CS, Smith DE, Manohar P, Schaefer A, Kline-Rogers E, Share D, Moscucci M. Gender differences in adverse outcomes after contemporary percutaneous coronary intervention: An analysis from the Blue Cross Blue Shield of Michigan cardiovascular consortium (BMC2) percutaneous coronary intervention registry. American Heart Journal. 2010;159(4):677–683. e1. doi: 10.1016/j.ahj.2009.12.040. [DOI] [PubMed] [Google Scholar]
- Eder B. Early 4-week cardiac rehabilitation exercise training in elderly patients after heart surgery. Journal of Cardiopulmonary Rehabilitation. 2010;30(2):85. doi: 10.1097/HCR.0b013e3181be7e32. [DOI] [PubMed] [Google Scholar]
- Freedland KE, Skala JA, Carney RM, Rubin EH, Lustman PJ, Davila-Roman VG, Hogue VW. Treatment of depression after coronary artery bypass surgery: A randomized controlled trial. Archives of General Psychiatry. 2009;66(4):387–396. doi: 10.1001/archgenpsychiatry.2009.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruppo di Lavoro della Societa Italiana di Cardiologia. The heart of women[Il cuore delle donne] Giornale Italiano Di Cardiologia (2006) 2007;8(1):3–27. [PubMed] [Google Scholar]
- Gu MO, Conn VS. Meta-analysis of the effects of exercise interventions on functional status in older adults. Research in Nursing & Health. 2008;31(6):594–603. doi: 10.1002/nur.20290. [DOI] [PubMed] [Google Scholar]
- Guru V, Fremes SE, Austin PC, Blackstone EH, Tu JV. Gender differences in outcomes after hospital discharge from coronary artery bypass grafting. Circulation. 2006;113(4):507–516. doi: 10.1161/CIRCULATIONAHA.105.576652. [DOI] [PubMed] [Google Scholar]
- Hertzog MA, Nieveen JL, Zimmerman LM, Barnason SA, Schulz PM, Miller CL, Rasmussen DA. Longitudinal field comparison of the RT3 and an activity diary with cardiac patients. Journal of Nursing Measurement. 2007;15(2):105–120. doi: 10.1891/106137407782156363. [DOI] [PubMed] [Google Scholar]
- Honey M, North N. Supporting workforce development of nurses: Exploiting the synergies between technology in education and practice. 2008 Retrieved May 28, 2011, from http://www.hinz.org.nz/uploads/file/2008conference/P30.pdf.
- Johnson NA, Lim LL, Bowe SJ. Multicenter randomized controlled trial of a home walking intervention after outpatient cardiac rehabilitation on health-related quality of life in women. European Journal of Cardiovascular Prevention and Rehabilitation. 2009;16(5):633–637. doi: 10.1097/HJR.0b013e32832e8eba. [DOI] [PubMed] [Google Scholar]
- Katircibasi MT, Koçum HT, Baltali M, Erol T, Tekin A, Yigit F, Müderrisoglu H. Effect of female gender on the outcome of coronary artery bypass surgery for left main coronary artery disease. Anatolian Journal of Cardiology. 2007;7(2):134–139. [PubMed] [Google Scholar]
- Kemmler W, Engelke K, von Stengel S, Weineck J, Lauber D, Kalender WA. Long-term four-year exercise has a positive effect on menopausal risk factors: The Erlangen fitness osteoporosis prevention study. Journal of Strength and Conditioning Research. 2007;21(1):232–239. doi: 10.1519/R-20826.1. [DOI] [PubMed] [Google Scholar]
- Ketcham JD, Furukawa MF. Hospital-physician gainsharing in cardiology. Health Affairs (Project Hope) 2008;27(3):803–812. doi: 10.1377/hlthaff.27.3.803. [DOI] [PubMed] [Google Scholar]
- Kleinpell RM, Avitall B. Integrating telehealth as a strategy for patient management after discharge for cardiac surgery: Results of a pilot study. The Journal of Cardiovascular Nursing. 2007;22(1):38–42. [PubMed] [Google Scholar]
- Konski A, Bhargavan M, Owen J, Paulus R, Cooper J, Fu KK, Watkins-Bruner D. Feasibility of using administrative claims data for cost-effectiveness analysis of a clinical trial. Journal of Medical Economics. 2008;11(4):611–623. doi: 10.3111/13696990802496740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kruk J. Physical activity in the prevention of the most frequent chronic diseases: An analysis of the recent evidence. Asian Pacific Journal of Cancer Prevention. 2007;8(3):325–338. [PubMed] [Google Scholar]
- Kurki TS, Hakkinen U, Lauharanta J, Ramo J, Leijala M. Evaluation of the relationship between preoperative risk scores, postoperative and total length of stays and hospital costs in coronary bypass surgery. European Journal of Cardio-Thoracic Surgery. 2001;20(6):1183–1187. doi: 10.1016/s1010-7940(01)00988-5. [DOI] [PubMed] [Google Scholar]
- Lie I, Arnesen H, Sandvik L, Hamilton G, Bunch EH. Effects of a home-based intervention program on anxiety and depression 6 months after coronary artery bypass grafting: A randomized controlled trial. Journal of Psychosomatic Research. 2007;62(4):411–418. doi: 10.1016/j.jpsychores.2006.11.010. [DOI] [PubMed] [Google Scholar]
- Liu-Ambrose TY, Khan KM, Eng JJ, Gillies GL, Lord SR, McKay HA. The beneficial effects of group-based exercises on fall risk profile and physical activity persist 1 year post-intervention in older women with low bone mass: Follow-up after withdrawal of exercise. Journal of the American Geriatrics Society. 2005;53(10):1767–1773. doi: 10.1111/j.1532-5415.2005.53525.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maganti M, Rao V, Cusimano RJ. Sex differences in resource use after on-pump and off-pump coronary artery bypass surgery: A propensity score-matched cohort. The Canadian Journal of Cardiology. 2009;25(5):e151–6. doi: 10.1016/s0828-282x(09)70498-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manini TM, Everhart JE, Patel KV, Schoeller DA, Colbert LH, Visser M, Harris TB. Daily activity energy expenditure and mortality among older adults. JAMA. 2006;296(2):171–179. doi: 10.1001/jama.296.2.171. [DOI] [PubMed] [Google Scholar]
- Müller-Riemenschneider F. Cost-effectiveness of interventions promoting physical activity. British Journal of Sports Medicine. 2009;43(1):70. doi: 10.1136/bjsm.2008.053728. [DOI] [PubMed] [Google Scholar]
- Moayyeri A. The association between physical activity and osteoporotic fractures: A review of the evidence and implications for future research [Abstract] Annals of Epidemiology. 2008;18(11):827–835. doi: 10.1016/j.annepidem.2008.08.007. [DOI] [PubMed] [Google Scholar]
- Mullen EJ. Choosing outcome measures in systematic reviews: Critical challenges. Research on Social Work Practice. 2006;16(1):84–90. [Google Scholar]
- Murphy BM, Elliott PC, Le Grande MR, Higgins RO, Ernest CS, Goble AJ, Worcester MU. Living alone predicts 30-day hospital readmission after coronary artery bypass graft surgery. European Journal of Cardiovascular Prevention and Rehabilitation. 2008;15(2):210–215. doi: 10.1097/HJR.0b013e3282f2dc4e. [DOI] [PubMed] [Google Scholar]
- Patel S, Smith JM, Engel AM. Gender differences in outcomes after off-pump coronary artery bypass graft surgery. The American Surgeon. 2006;72(4):310–313. [PubMed] [Google Scholar]
- Pines A. Lifestyle and diet in post-menopausal women. Climacteric. 2009;12(Suppl 1):62–65. doi: 10.1080/13697130902785449. [DOI] [PubMed] [Google Scholar]
- Pines A, Berry EM. Exercise in the menopause – An update. Climacteric. 2007;10:42–46. doi: 10.1080/13697130701600153. [DOI] [PubMed] [Google Scholar]
- Porter HB. Health resource utilization and quality of life outcomes of low-risk coronary artery bypass graft patients: A comparison study. Canadian Journal of Cardiovascular. 1998;9(1):10–15. [PubMed] [Google Scholar]
- Rollman BL, Schulberg HC, Reynolds CF., III Telephone-delivered collaborative care for treating post-CABG depression. JAMA. 2010;303(13):1252-a-1253. doi: 10.1001/jama.2009.1670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saleh SS, Racz M, Hannan E. The effect of preoperative and hospital characteristics on costs for coronary artery bypass graft. Annals of Surgery. 2009;249(2):335–341. doi: 10.1097/SLA.0b013e318195e475. [DOI] [PubMed] [Google Scholar]
- Sawatzky JA, Naimark BJ. The coronary artery bypass graft surgery trajectory: Gender differences revisited. European Journal of Cardiovascular Nursing. 2009a;8(4):302–308. doi: 10.1016/j.ejcnurse.2009.02.003. [DOI] [PubMed] [Google Scholar]
- Sawatzky JA, Naimark BJ. Coronary artery bypass graft surgery: Exploring a broader perspective of risks and outcomes. The Journal of Cardiovascular Nursing. 2009b;24(3):198–206. doi: 10.1097/JCN.0b013e31819b534e. [DOI] [PubMed] [Google Scholar]
- Schofield R, Ganann R, Brooks S, McGugan J, Bona KD, Betker C, Watson C. Community health nursing vision for 2020: Shaping the future. Western Journal of Nursing Research. 2011;33(8):1047–1068. doi: 10.1177/0193945910375819. [DOI] [PubMed] [Google Scholar]
- Siegrist PT, Husmann L, Knabenhans M, Gaemperli O, Valenta I, Hoefflinghaus T, Kaufmann PA. (13)N-ammonia myocardial perfusion imaging with a PET/CT scanner: Impact on clinical decision making and cost-effectiveness. European Journal of Nuclear Medicine and Molecular Imaging. 2008;35(5):889–895. doi: 10.1007/s00259-007-0647-3. [DOI] [PubMed] [Google Scholar]
- Speir AM, Kasirajan V, Barnett SD, Fonner E., Jr Additive costs of postoperative complications for isolated coronary artery bypass grafting patients in Virginia. The Annals of Thoracic Surgery. 2009;88(1):40–45. doi: 10.1016/j.athoracsur.2009.03.076. [DOI] [PubMed] [Google Scholar]
- Spetz J. The cost and cost-effectiveness of nursing services in health care [Abstract] Nursing Outlook. 2005;53(6):305–309. doi: 10.1016/j.outlook.2005.05.006. [DOI] [PubMed] [Google Scholar]
- Swaminathan M, Phillips-Bute BG, Patel UD, Shaw AD, Stafford-Smith M, Douglas PS, Mathew JP. Increasing healthcare resource utilization after coronary artery bypass graft surgery in the United States. Circulation: Cardiovascular Quality and Outcomes. 2009;2(4):305–312. doi: 10.1161/CIRCOUTCOMES.108.831016. [DOI] [PubMed] [Google Scholar]
- Tumeh JW, Moore SG, Shapiro R, Flowers CR. Practical approach for using medicare data to estimate costs for cost–effectiveness analysis. Expert Review of Pharmacoeconomics and Outcomes Research. 2005;5(2):153–162. doi: 10.1586/14737167.5.2.153. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. 2008 physical activity guidelines for Americans. 2008 Retrieved, from http://www.health.gov/PAGuidelines.
- Utriyaprasit K, Moore SM, Chaiseri P. Recovery after coronary artery bypass surgery: Effect of an audiotape information programme. Journal of Advanced Nursing. 2010;66(8):1747–1759. doi: 10.1111/j.1365-2648.2010.05334.x. [DOI] [PubMed] [Google Scholar]
- Vaccarino V, Lin ZQ, Kasl SV, Mattera JA, Roumanis SA, Abramson JL, Krumholz HM. Gender differences in recovery after coronary artery bypass surgery. Journal of the American College of Cardiology. 2003a;41(2):307–314. doi: 10.1016/s0735-1097(02)02698-0. [DOI] [PubMed] [Google Scholar]
- Vaccarino V, Lin ZQ, Kasl SV, Mattera JA, Roumanis SA, Abramson JL, Krumholz HM. Sex differences in health status after coronary artery bypass surgery. Circulation. 2003b;108(21):2642–2647. doi: 10.1161/01.CIR.0000097117.28614.D8. [DOI] [PubMed] [Google Scholar]
- Vogel T, Brechat PH, Lepretre PM, Kaltenbach G, Berthel M, Lonsdorfer J. Health benefits of physical activity in older patients: A review. International Journal of Clinical Practice. 2009;63(2):303–320. doi: 10.1111/j.1742-1241.2008.01957.x. [DOI] [PubMed] [Google Scholar]
- Weisser B, Preuss M, Predel HG. Physical activity for prevention and therapy of internal diseases in the elderly[Korperliche Aktivitat und Sport zur Pravention und Therapie von inneren Erkrankungen im Seniorenalter] Medizinische Klinik. 2009;104(4):296–302. doi: 10.1007/s00063-009-1055-1. [DOI] [PubMed] [Google Scholar]
- Williams ML, Trivedi JR, Doughtie C, Slaughter MS. Is female sex an independent risk factor for perioperative transfusion in coronary artery bypass graft surgery? Journal of the American College of Surgeons. 2011;212(3):362–366. doi: 10.1016/j.jamcollsurg.2010.12.008. [DOI] [PubMed] [Google Scholar]
- Zimmerman L, Barnason S. Use of a telehealth device to deliver a symptom management intervention to cardiac surgical patients. The Journal of Cardiovascular Nursing. 2007;22(1):32–37. doi: 10.1097/00005082-200701000-00005. [DOI] [PubMed] [Google Scholar]
- Zimmerman L, Barnason S, Schulz P, Nieveen J, Miller C, Hertzog M, Rasmussen D. The effects of a symptom management intervention on symptom evaluation, physical functioning, and physical activity for women after coronary artery bypass surgery. The Journal of Cardiovascular Nursing. 2007;22(6):493–500. doi: 10.1097/01.JCN.0000297379.06379.b6. [DOI] [PubMed] [Google Scholar]
- Zimmerman L. Gender differences in recovery outcomes after an early recovery symptom management intervention. Heart and Lung. 2011;40(5):429–439. doi: 10.1016/j.hrtlng.2010.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]