Abstract
Background
Metabolic syndrome (MetS) is a risk factor for cardiovascular disease. Very limited work has evaluated associations of sociocultural processes with prevalence of the MetS.
Purpose
The purpose of the present study was to evaluate associations between family environment (cohesion/conflict) and the MetS, in a multi-site sample of US Hispanics/Latinos.
Methods
A total of 3278 participants from the Hispanic Community Health Study/Study of Latinos underwent a clinical exam and completed psychosocial measures including family environment (cohesion and conflict) as part of the Sociocultural Ancillary Study.
Results
The association between family environment and the MetS was moderated by sex. Among all women, higher family conflict was associated with MetS prevalence. Results by ancestry group showed that only among Cuban women, higher conflict was associated with the MetS, whereas only among Dominican men, greater cohesion was associated with the MetS.
Conclusions
The family context may be a sociocultural protective or risk factor among Hispanics/Latinos in terms of MetS risk, but these associations may vary by sex and Hispanic background.
Keywords: Family environment, Cohesion, Conflict, Sex, Metabolic syndrome, Hispanics-Latinos
Introduction
Hispanics/Latinos (hereafter referred to as Hispanics) are the largest US ethnic/racial minority and are projected to account for nearly one third of the 2050 US population. Hispanics face several health challenges (e.g., obesity and diabetes), and there is increasing interest in understanding possible protective roles of psychosocial and sociocultural processes that may impact intermediate risk factors of these conditions and cardiovascular disease (CVD)—the second leading cause of death among Hispanics in the USA [1].
The metabolic syndrome (MetS) (i.e., abdominal obesity, insulin resistance, dyslipidemia, and elevated blood pressure) [2] is associated with increased CVD, type 2 diabetes (T2D), and all-cause mortality [3, 4]. Prevalence of the MetS varies by sex and ethnicity with excess MetS found among women of Mexican origin [5]. Beyond traditional behavioral (e.g., sedentary lifestyle) and biological (e.g., hyperlipidemia) risk factors, studies have shown that psychosocial factors are also associated with risk and prevalence for the MetS [6–8]. For example, stress and negative emotions such as depression, anxiety, and hostility are risk factors for poor health outcomes, including CVD, through their influences on varied behavioral (e.g., sedentary behavior) and physiological (e.g., inflammation) processes [8–10]. Independent of traditional risk factors, depressive symptoms are associated with greater prevalence of the MetS [11, 12], while protective factors such as positive emotions and optimism are associated with lowered CVD risk [13, 14].
Perceived social support [15] and efficacious social networks [16] are reportedly associated with decreased CVD risk and MetS components. Furthermore, compromised family relations in childhood and adolescence influence cardiometabolic health and MetS prevalence in adulthood [17, 18]. Among adult women, marital distress has been significantly associated with a greater likelihood of MetS prevalence after controlling for socioeconomic status (SES), and health behaviors such as cigarette smoking and physical activity [19].
Hispanics share a set of core family values that reflect a communal view with emphasis on strong attachments to the nuclear and extended family that may have protective health effects [20]. There is a growing interest in understanding how culturally driven values such as a strong family attachment and affiliation that promotes reliance within the family structure may impact health among Hispanics [21]. In fact, it has been suggested that the “Hispanic Paradox” (i.e., the notion that Hispanics on the whole often experience better health outcomes than non-Hispanic whites despite socioeconomic disadvantage) can be partly explained by sociocultural processes such as strong and cohesive family structures [22, 23].
Sociocultural processes may serve as risk and protective factors for both risk behavior, psychological well-being [24, 25], and physical health [26, 27] in Hispanics. Studies that support the protective role of cohesive family structures among Hispanics suggest that cohesive family systems are related to better emotional well-being [28, 29], less perceived burden among dementia caregivers [30], and adoption of favorable health behaviors and seeking medical attention [31] when such behaviors are perceived to provide a benefit to the entire family [32]. In contrast, higher family conflict and lower family-based support have been related to psychological distress and risk behaviors [25, 33]. Work addressing the influence of familial dynamics on MetS is limited, but some have shown that a family structure that reflects a cohesive and supportive family system is related to a lower likelihood of having the MetS [34].
Present Study
This study sought to report associations between family environment (i.e., cohesion and conflict), and the MetS. The study also evaluated whether the relationship between family environment and the MetS varied by sex as prior work shows that family conflict (e.g., marital distress) unfavorably impacts cardiometabolic health but only in women. We hypothesized that a more cohesive and less conflicted family would be associated with less MetS prevalence.
Methods
Participants
The Sociocultural Ancillary Study (SCAS) to the Hispanic Community Health Study/Study of Latinos (HCHS/SOL) was designed to examine additional socioeconomic, sociocultural, and psychological factors in a subgroup of HCHS/SOL participants. The HCHS/SOL is a prospective, population-based study of the prevalence of multiple health conditions and their risk factors among 16,415 diverse Hispanic/Latinos ages 18–74 residing in four US metropolitan areas between 2008 and 2011 [35]. All participants underwent an 8-h baseline clinical exam that involved anthropometric measures, fasting blood draw for lipids, fasting glucose, insulin and other CVD risk biomarkers, and self-reported measures of SES and demographic factors, health behaviors, and health history. Participants were 18–74 years of age and included Hispanics who self-identified as Cuban, Central American, Dominican, Mexican, Puerto Rican, South American, and other Hispanic/Latino heritage and were recruited from four defined metropolitan communities in the Bronx, NY; Chicago, IL; Miami, FL; and San Diego, CA.
Eligibility for participation in the SCAS included a completed baseline in the parent study and willingness to attend an additional visit for a comprehensive psychosocial and sociocultural assessment within 9 months of their parent study clinic visit. A total of 5313 were enrolled in the SCAS. Participants less than 45 years of age (n=2035) were excluded from the current analyses (n=3278) because the prevalence of the MetS is significantly lower in younger adults [36].
Procedure
Participant Sampling and Recruitment
Parent study recruitment used a two-stage area household probability design stratified by 2000 Census areas near the four field centers and by key demographic variables (age, Hispanic concentration, and SES). A more detailed description of the sampling method has been published previously [37]. Participants aged 45–74 years were over-sampled. Persons who met the eligibility criteria and agreed to participate were scheduled for an IRB-approved consenting and assessment appointment at the field center clinic. Participants eligible for the SCAS were contacted by phone interviewers within 9 months of their baseline examination. SCAS assessments required 1–2 hours to complete in English or Spanish and were administered by trained, bi-lingual, bi-cultural research assistants.
Measures
Descriptive Measures and Covariates
Sociodemographic and behavioral variables included as covariates were age, sex, marital status, Hispanic background, acculturation (using the Short Acculturation Scale for Hispanics [SASH] Language & Ethnic Social Relations Subscales [38]), education, yearly household income, family network size, alcohol consumption (drinks per week), smoking status (never, former, current), depressive symptoms (i.e., ten-item Center for Epidemiologic Studies Depression Scale; [39]), and perceived social support (i.e., Interpersonal Support Evaluation List; [40]).
Family Cohesion and Family Conflict
Two subscales of the Family Environment Scale were used: (a) Family Cohesion (i.e., commitment and support) and (b) Family Conflict (i.e., expressed anger and conflict; [41]). Items are answered in a true/false format. Sample items from the cohesion and conflict subscale include “My family members really help and support one another” and “We fight a lot in our family,” respectively. A sum score can be obtained for each subscale, with higher scores indicating higher family cohesion or higher family conflict. Confirmatory factor analyses (CFAs) showed adequate structural validity in both measures, as well as factorial invariance across the Spanish and English versions for the measures [42].
The Metabolic Syndrome
MetS was the primary study outcome. At the parent HCHS/SOL clinic examination, waist circumference (cm) and brachial blood pressure (mmHg) were measured using standardized methods. Fasting blood was sampled for serum triglycerides, HDL cholesterol, and fasting plasma glucose levels. Detailed parent study data collection methods are described in Sorlie et al. [35]. MetS was defined based on National Cholesterol Education Program (NCEP) Adult Treatment Panel (ATP) III updated guidelines [43].
Data Analysis
Descriptive analyses were conducted using IBM SPSS statistics 19.0 with complex sampling procedures and were weighted to account for sampling probability and non-response. Variables were evaluated for missing data, outliers, and univariate normality. Logistic regression was used to test the main effects of family cohesion and sex (0 = female, 1 = male), as well as the two-way interaction between these variables, in addition to entering control variables. Prevalence of the MetS was specified as a categorical outcome (prevalent or not prevalent). A separate logistic regression model was used to test the main effects of family conflict and sex, as well as the two-way interaction between these variables, in addition to entering control variables. We then combined both family cohesion and family conflict and their interactions with sex in a single model. Age, income, education, acculturation, family network size, alcohol use, depressive symptoms, and perceived social support were mean-centered and entered as continuous control variables. Marital status and cigarette use (never, former, current) were dummy coded and also entered as control variables. The maximum likelihood robust (MLR) estimation procedure in Mplus Version 7.0 was used to estimate model parameters. Prior to computing the interaction term, family cohesion and family conflict were mean-centered (mean = 0) to reduce multi-collinearity. Interaction terms were then specified by taking the product of family cohesion and sex and the product of family conflict and sex. A significant interaction effect (p<0.05) was further evaluated via post hoc simple slopes as described by Aiken and West [44].
Results
Preliminary Analyses
Weighted HCHS/SCAS sample demographics of 3278 participants aged 45 and older and individual MetS prevalence and components, psychosocial and lifestyle variables antihypertensive and anti-diabetic medication use, and smoking status are provided in Tables 1 and 2, respectively.
Table 1.
Weighted HCHS/SOL Sociocultural Ancillary Study (SCAS) sample demographic characteristics in participants aged 45 and older (Total N=3278)
| Characteristic | M (SE) |
|---|---|
| Age (in years) | 56.84 (.24) |
| Family network sizea | 8.40 (.11) |
| SASH language | 1.75 (.04) |
| SASH ethnic relations | 2.15 (.02) |
| % | |
| Age 45 or older in SCAS sample | 43.5 |
| Female sex | 56.4 |
| Spanish language interview | 84.7 |
| Hispanic background | |
| Central American | 6.3 |
| Cuban | 28.3 |
| Dominican | 10.4 |
| Mexican | 28.7 |
| Puerto Rican | 19.0 |
| South American | 5.9 |
| More than one/other | 1.3 |
| Yearly household income | |
| Less than $10,000 | 23.1 |
| $10,001–$20,000 | 33.5 |
| $20,001–40,000 | 28.3 |
| $40,001–75,000 | 9.2 |
| More than $75,000 | 5.9 |
| Education level | |
| <HS diploma/GED | 40.6 |
| At most HS diploma/GED | 20.4 |
| >HS diploma/GED | 39.2 |
| Marital status | |
| Single | 19.2 |
| Married/living with partner | 49.2 |
| Separated, divorced, widow | 31.6 |
Family Network Size includes spouse, number of children, number of parents living, and number of relatives with whom considered close
Table 2.
Weighted descriptive statistics for psychosocial indicators, lifestyle covariates, and the metabolic syndrome for participants aged 45 and older (total N=3278)
| Variable | M (SE) or % men | M (SE) or % women |
M (SE) or % total sample |
|---|---|---|---|
| Family cohesion | 6.89 (0.07) | 6.86 (0.07) | 6.87 (0.05) |
| Family conflict | 1.92 (0.08) | 1.96 (0.06) | 1.94 (0.05) |
| Depression (CES-D) | 7.18 (0.23) | 8.90 (0.21)* | 8.15 (0.17) |
| Social support (ISEL) | 26.28 (0.24) | 25.68 (0.25) | 25.94 (0.18) |
| Alcohol (drinks/week) | 3.97 (0.30) | 0.53 (0.05)* | 2.03 (0.14) |
| Waist circumference (cm) | 101.23 (0.42) | 99.04 (0.39)* | 100.00 (0.32) |
| HDL-cholesterol (mg/dL) | 45.43 (0.55) | 52.83 (0.45)* | 49.60 (0.37) |
| Fasting glucose (mg/dL) | 111.32 (1.32) | 104.63 (1.09)* | 107.55 (0.89) |
| Triglycerides (mg/dL) | 167.77 (8.78) | 139.97 (2.31)* | 152.12 (4.17) |
| Systolic BP (mmHg) | 130.36 (0.77) | 128.43 (0.65) | 129.27 (0.47) |
| Diastolic BP (mmHg) | 76.28 (0.44) | 74.90 (0.38)* | 75.50 (0.31) |
| Metabolic syndrome | 45.8 % | 51.6 %* | 49.1 % |
| Anti-hypertensive meds | 29.2 % | 27.9 % | 28.5 % |
| Anti-diabetic meds | 17.9 % | 18.6 % | 18.3 % |
| Cigarette use | |||
| Never | 42.1 % | 63.5 %* | 54.2 % |
| Former | 32.9 % | 20.2 %* | 25.7 % |
| Current | 25.0 % | 16.3 %* | 20.1 % |
M mean, SE standard error, BP blood pressure
Values for men and women differ significantly at p<.05
Logistic Regression Analyses
In a univariate model, family cohesion was not significantly associated with the MetS (odds ratio (OR)=0.99, 95 % confidence interval (CI) 0.94–1.03). Similarly, family conflict was not significantly associated with the MetS (OR=1.02, 95 % CI 0.96–1.08). Sex was significantly associated with the MetS (OR=0.79, 95 % CI 0.65–0.97), without adjusting for other variables, such that men were significantly less likely than women to have the MetS.
The following covariates entered as predictors in separate unadjusted univariate analyses were significantly associated with greater odds of having the MetS: age (OR=1.05, 95 % CI=1.04–1.07), income (OR=0.78, 95% CI=0.70–0.86), education (OR=0.82, 95 % CI=0.72–0.93), Cuban background (Reference group=Mexican; OR=1.39, 95 % CI=1.05–1.84;), being married (reference group=single; OR=0.76, 95 % CI=0.60–0.95), SASH Language Subscale (OR=0.87, 95%CI=0.77–0.98), SASH Ethnic Relations Subscale (OR= 0.79, 95 % CI=0.65–0.96), and former cigarette use (reference group=never smoked; OR=1.57, 95 % CI=1.26–1.96). Family size, alcohol use, depression symptoms, and perceived social support were not significantly associated with the MetS. Female sex, older age, lower income, being married, larger family size, and former cigarette use remained significantly associated with prevalence of the MetS in adjusted analyses that included family cohesion, family conflict, and sex by family cohesion and conflict interaction terms.
Results of adjusted logistic regression analyses including family cohesion, its interaction with sex, and all covariates indicated that there was a significant interaction between family cohesion and sex (OR=1.12, 95 % CI 1.004–1.26) in relation to MetS prevalence. Similarly, in a separate model replacing family cohesion with family conflict, there was a significant interaction between family conflict and sex (OR=0.87, 95 % CI= 0.76–0.99) in relation to MetS prevalence. When family cohesion, family conflict, and each of their interactions with sex were entered as predictors simultaneously in one model with all covariates, the interactions no longer remained significant in relation to MetS prevalence (cohesion by sex OR=1.07, 95 % CI=0.92–1.07; conflict by sex OR=0.90, 95 % CI=0.76–1.07).
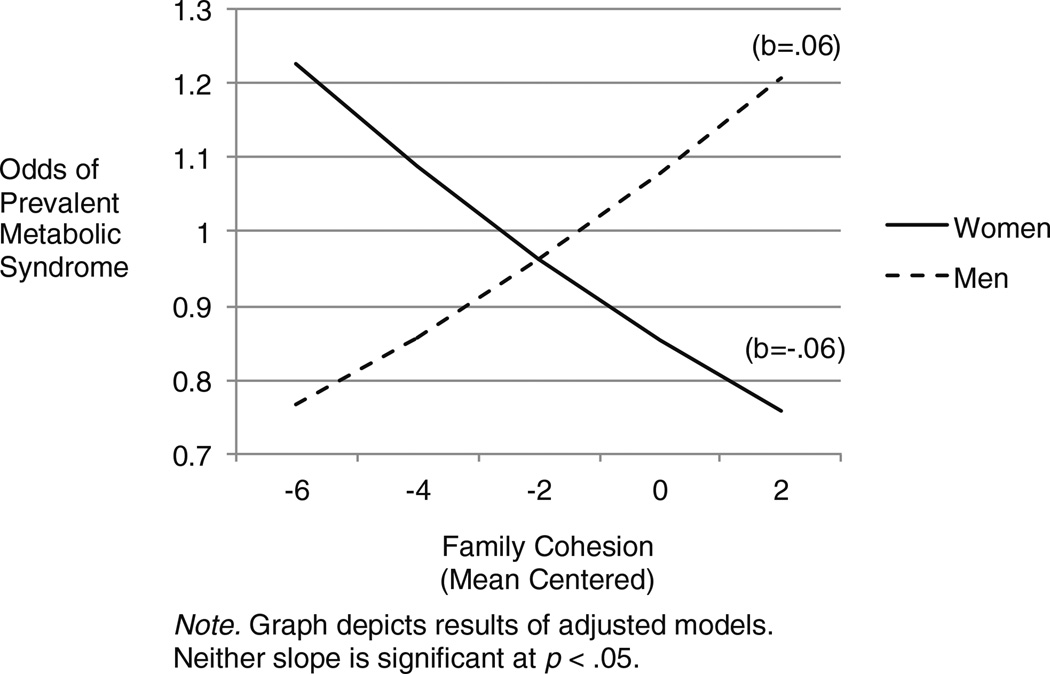
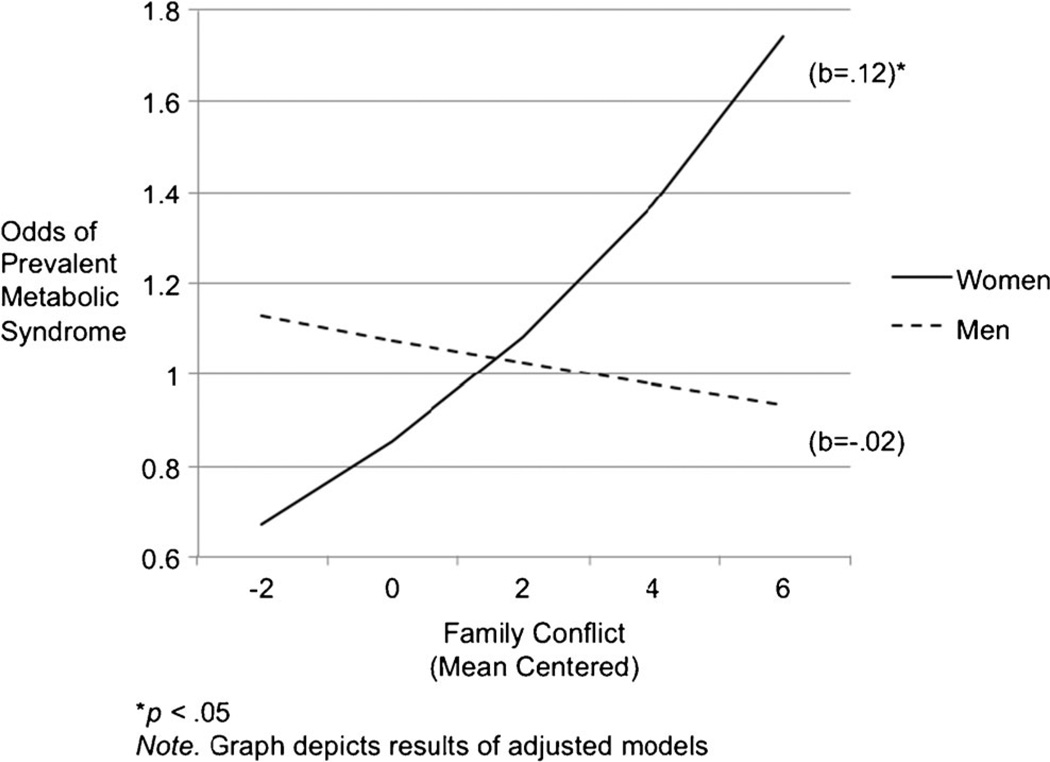
Post Hoc Probing of Interaction effects
As a follow-up to the significant family cohesion by sex interaction, two post hoc logistic regression analyses were run. New interaction terms were computed by multiplying family cohesion with a conditional sex variable in each model. One regression generated the simple slope for women and the second regression generated the simple slope for men. Although the simple slopes for women and men were significantly different, as indicated by the significant family cohesion by gender interaction, results of adjusted post hoc logistic regression analyses indicated that family cohesion was not associated with having the MetS in women (OR=0.94, 95 % CI 0.88–1.01), or in men (OR=1.06, 95 % CI 0.96–1.17). Similar post hoc regression analyses evaluated the significant family conflict by sex interaction. In women, higher family conflict was associated with significantly greater odds of having the MetS (OR=1.13, 95 % CI=1.02–1.24). In men, family conflict was not significantly associated with having the MetS (OR=0.98, 95 % CI=0.88–1.08). Graphs depicting the relationship between family cohesion and conflict (mean-centered) and the MetS, as moderated by sex, are provided in Figs. 1 and 2, respectively.
Fig. 1.
Associations between family cohesion and metabolic syndrome prevalence as moderated by sex. Note: Graph depicts results of adjusted models. Neither slope is significant at p<.05
Fig. 2.
Associations between family conflict and metabolic syndrome prevalence as moderated by sec. *p<.05. Note: Graph depicts results of adjusted models
Differences by SES and Hispanic Ancestry
To determine whether the interactions of family cohesion or family conflict with sex in relation to the MetS were significantly different across levels of socioeconomic status, we examined three-way interactions of family cohesion and family conflict with sex and yearly household income level (i.e., ≤$20,000 or >$20,000). Results of adjusted analyses indicated that the three-way interactions of family cohesion (OR=1.18, 95 % CI 0.91–1.52) and family conflict (OR=1.07, 95 % CI 0.97–1.18) with sex and income level were not significant.
We also explored whether the interactions found in the entire sample were significantly different across Hispanic background groups. The three-way interactions of family cohesion and family conflict with sex, and with each of five dummy-coded background groups (i.e., Cuban, Puerto Rican, Central/South American, Dominican, other/more than one, and Mexican as reference group) were examined. As an omnibus test of whether the family cohesion or conflict interactions with sex in relation to the MetS differed significantly across Hispanic background group, we examined the significance of the difference in model R2 (i.e., percentage of variance explained) between a model including all possible two-way interactions between family cohesion or conflict, sex, and background (e.g., conflict × sex, conflict × background), and a model that also included all possible three-way interactions (e.g., conflict × sex × Cuban background). There was a significant change in R2 between models examining the two-way versus the three-way interactions (family cohesion, F[5, 3238]=8.02, p<.05, and family conflict F[5, 3238]=2.91, p<.05), suggesting that the two-way interactions found in the entire sample differ significantly across at least two Hispanic ancestry groups.
The original analyses were run separately by Hispanic background group to determine how the interactions between family cohesion or conflict with sex in relation to the MetS varied across Hispanic ancestry. The interaction of family cohesion and sex in relation to the MetS remained significant only in Dominicans (OR=2.00, 95 % CI 1.10–3.65) and Puerto Ricans (OR=1.23, 95 % CI 1.02–1.49) when examined separately. Post hoc probing in each group indicated that family cohesion was not significantly associated with having the MetS in women or in men across Hispanic subgroups with the exception of Dominicans in the sample. Among Dominicans, men with higher levels of family cohesion were significantly more likely to have the MetS (OR=1.97, 95 % CI 1.09–3.55). Results of similar analyses indicated that the interaction of family conflict and sex in relation to the MetS remained significant only in Cubans (OR=0.70, 95 % CI 0.50–0.97) when examined separately. Post hoc probing of the interaction in Cubans indicated that results were comparable to those found in the entire sample, with higher levels of family conflict significantly associated with higher odds of having the MetS only in female Cubans (OR=1.27, 95 % CI 1.07–1.51).
Discussion
In our study, family cohesion and conflict were not associated with overall MetS prevalence. Among women, higher levels of family conflict were associated with significantly greater odds of MetS prevalence, independent of other risk factors. This finding is significant because Hispanic women are at greater risk for the MetS [1] and suggests that a family context that involves expressed anger, conflict, and hostility may be a risk factor. Our findings are consistent with other work showing that interpersonal resources may be protective for women and may be associated with lower risk factors for CVD [25, 30, 33]. That female sex moderated this relationship is also consistent with prior work that has shown that marital discord, a probable correlate of high conflict within the family, is related to the MetS among women but not among men [19]. Although the current study did not specifically evaluate marital relations or satisfaction, marital stress, or communication patterns, there is some prior evidence suggesting that family relations and specifically marital discord may indeed have a greater impact on cardiometabolic health and possibly MetS prevalence among women only. Prior work has also shown differences in how men and women approach and utilize support from family systems and that the association between social support and CVD outcomes varies by sex [45–47], where women often are at greater risk when operating in disrupted social systems. It is possible that in our sample, operating within a less conflicted family system may have favorably impacted health behaviors among women but not among men. This would be consistent with prior work in non-Hispanic samples that has shown that supportive family environments facilitate modifying dietary habits and specifically with the use of strategies to reduce fat consumption, increase fiber intake and with fewer barriers to obtaining fruits and vegetables [48].
The study also explored whether SES moderated the association between family cohesion or conflict, sex, and the MetS. As expected, we found that the associations did not vary as a function of SES. However, while we did not hypothesize that our proposed associations would vary by Hispanic ancestry group, we found that among Dominican men, greater family cohesion was associated with greater prevalence of the MetS. Additionally, we found that the association between greater family conflict, female sex, and prevalence of the MetS only held among our Cuban female participants. Very few studies have examined the effects of the family environment on health among diverse Hispanics in the USA, and available studies have not disaggregated Hispanic ancestry subgroups or included Dominicans in the sample. However, prior work has shown that among Cubans and Mexicans, but not Puerto Ricans, greater family conflict is associated with higher psychological distress [49]. Furthermore, family conflict among Cubans, but not Mexican Americans and Puerto Ricans, has also been associated with greater risk behaviors such as smoking [50]. Therefore, our findings are somewhat consistent with prior studies showing that family conflict may differentially impact Hispanics ancestry subgroups. It is important to acknowledge, however, that other factors that may vary across Hispanic ancestry groups that we did not evaluate such as martial relations/discord, stress, coping styles, immigration factors, and intergenerational conflict may explain the differential influence of family conflict and cohesion on the MetS [51]. Nonetheless, it remains unclear why a greater cohesive family system would be associated with greater prevalence of the MetS only in Dominican men, or why family conflict would be associated with greater MetS prevalence, only in Cuban female participants. It is important to note that the background groups are not equally distributed across field centers and it is therefore difficult to disentangle influences due to background group versus geographic context. As work evaluating family patterns and their relationship to CVD risk factors across Hispanic groups is very limited, future research should evaluate how men and women in different Hispanic ancestry groups approach and utilize support from the family and include other factors that may impact how family systems may differentially impact the MetS.
Despite these novel findings, there are several limitations in our study. The cross-sectional design precludes any causal inferences from these findings. The effects of family environment were independent of traditional risk factors (e.g., smoking); however, we did not evaluate other potentially significant explanatory pathways such as stress, marital discord, hostility, and stress-mediated physiological mechanisms [52]. Also, family cohesion and conflict are only two domains representing a wide range of familial processes that may impact health. In our study, we did not assess other indices of family dynamics such as expressiveness and control. A more comprehensive evaluation of family systems may allow examination of more robust underlying factors that combine elements of cohesion, conflict, and other family dynamics such as expressiveness and control [53]. Notably, when both conflict and cohesion were entered in a single model, along with terms reflecting their interactions with sex, neither factor uniquely contributed to the MetS, suggesting that the shared variance between cohesion and conflict may explain their associations with MetS prevalence rather than the unique influence of each predictor. Furthermore, because participants were residing in one of four US cities, we cannot generalize these findings to all Hispanics living in the USA. Nonetheless, despite these limitations, this study begins to shed light on the possible role of Hispanic cultural processes in MetS prevalence.
Conclusions
Hispanic women with higher levels of family conflict were more likely to have met MetS criteria independent of traditional risk factors, but this association only held among Cuban women in our sample. To our knowledge, this is the first study to report the associations between the family environment and prevalence of the MetS in a relatively large multi-site sample of Hispanics in the USA and by Hispanic ancestry group. Our findings are the first to suggest that, while family dynamics are not directly associated with the MetS, sex moderates the association between the family environment and prevalence of the MetS and that Cuban women in more conflicted family systems, and Dominican men in more cohesive family systems are at greater risk for prevalence of the MetS. Thus, our findings suggest that one must consider how family dynamics and sex are differentially related to the MetS across Hispanic ancestry groups and that future work should incorporate other possible social and physiological factors that may influence this association.
Acknowledgments
Funding/Support: The Hispanic Community Health Study/Study of Latinos was a collaborative study supported by contracts from the National Heart, Lung, and Blood Institute (NHLBI) to the University of North Carolina (N01-HC65233), University of Miami (N01-HC65234), Albert Einstein College of Medicine (N01-HC65235), Northwestern University (N01-HC65236), and San Diego State University (N01-HC65237). A complete list of staff and investigators was published in Ann Epidemiol. 2010;20:642–649 and is available on the study website, http://www.cscc.unc.edu/hchs/. The HCHS/SOL Sociocultural Ancillary Study was supported by grant 1 RC2 HL101649 from the NIH/NHLBI (Gallo/Penedo MPIs). The funding agency had a role in the design and conduct of the study; in the collection, analysis, and interpretation of the data; and in the review and approval of the manuscript.
Footnotes
Authors’ Statement of Conflict of Interest
Authors Frank J. Penedo, Carrie E. Brintz, Maria M. LLabre, William Arguelles, Carmen R. Isasi, Elva M. Arredondo, Elena L. Navas-Nacher, Krista Perreira, Hector M. González, Carlos J. Rodriguez, Martha Daviglus, Neil Schneiderman, and Linda C. Gallo declare that they have no conflict of interest.
Adherence to Ethical Standards
All procedures, including the informed consent process, were conducted in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000.
References
- 1.Rodriguez CJ, Allison M, Daviglus ML, et al. On behalf of the American Heart Association Council on Epidemiology and Prevention. Council on Clinical Cardiology, and Council on Cardiovascular and Stroke Nursing. Status of cardiovascular disease and stroke in Hispanics/Latinos in the United States. Circulation. 2014;130:1–33. [Google Scholar]
- 2.Grundy SM. Metabolic syndrome: a multiplex cardiovascular risk factor. J Clin Endocr Metab. 2007;92:399–404. doi: 10.1210/jc.2006-0513. [DOI] [PubMed] [Google Scholar]
- 3.Gami AS, Witt BJ, Howard DE, et al. Metabolic syndrome and risk of incident cardiovascular events and death: A systematic review and meta-analysis of longitudinal studies. J Am Coll Cardiol. 2007;49(4):403–414. doi: 10.1016/j.jacc.2006.09.032. [DOI] [PubMed] [Google Scholar]
- 4.Haffner SM. Relationship of metabolic risk factors and development of cardiovascular disease and diabetes. Obesity (Silver Spring) 2006;14(Suppl 3):121S–127S. doi: 10.1038/oby.2006.291. [DOI] [PubMed] [Google Scholar]
- 5.Ervin RB. Prevalence of metabolic syndrome among adults 20 years of age and over by sex, age, race and ethnicity, and body mass index: United States, 2003–2006. Natl Health Stat Report. 2009;13:1–7. [PubMed] [Google Scholar]
- 6.Matthews KA, Raikkonen K, Gallo LC, et al. Association between socioeconomic status and metabolic syndrome in women: testing the reserve capacity model. Health Psychol. 2006;27:576–583. doi: 10.1037/0278-6133.27.5.576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Räikkönen K, Matthews KA, Kuller LH. Depressive symptoms and stressful life events predict metabolic syndrome among middle-aged women. Diabetes Care. 2007;30(4):872–877. doi: 10.2337/dc06-1857. [DOI] [PubMed] [Google Scholar]
- 8.Everson-Rose SA, Lewis TT. Psychosocial factors and cardiovascular diseases. Annu Rev of Publ Health. 2005;26:469–500. doi: 10.1146/annurev.publhealth.26.021304.144542. [DOI] [PubMed] [Google Scholar]
- 9.Steptoe A, Kivimäki M. Stress and cardiovascular disease. Nat Rev Cardiol. 2012;9(6):360–370. doi: 10.1038/nrcardio.2012.45. [DOI] [PubMed] [Google Scholar]
- 10.Steptoe A, Kivimäki M. Stress and cardiovascular disease: An update on current knowledge. Annu Rev Public Health. 2013;34:337–354. doi: 10.1146/annurev-publhealth-031912-114452. [DOI] [PubMed] [Google Scholar]
- 11.Butnoriene J, Bunevicius A, Norkus A, et al. Depression but not anxiety is associated with metabolic syndrome in primary care based community sample. Psychoneuroendocrinology. 2014;40:269–276. doi: 10.1016/j.psyneuen.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 12.Pan A, Keum N, Okereke OI, et al. Bidirectional association between depression and metabolic syndrome: A systematic review and meta-analysis of epidemiological studies. Diabetes Care. 2012;35(5):1171–1180. doi: 10.2337/dc11-2055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cohen S, Pressman SD. Positive affect and health. Curr Dir in Psychol Sci. 2006;15:122. [Google Scholar]
- 14.Kubzansky LD, Sparrow D, Vokonas P, et al. Is the glass half empty or half full? a prospective study of optimism and coronary heart disease in the normative aging study. Psychosom Med. 2001;63(6):910–916. doi: 10.1097/00006842-200111000-00009. [DOI] [PubMed] [Google Scholar]
- 15.Bell CN, Thorpe RJ, Jr, Laveist TA. Race/Ethnicity and hypertension: The role of social support. Am J Hypertens. 2010;23(5):534–540. doi: 10.1038/ajh.2010.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Whittaker KS, Krantz DS, Rutledge T, et al. Combining psychosocial data to improve prediction of cardiovascular disease risk factors and events: The National Heart, Lung, and Blood Institute–sponsored Women’s Ischemia Syndrome Evaluation study. Psychosom Med. 2012;74(3):263–270. doi: 10.1097/PSY.0b013e31824a58ff. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gustafsson PE, Hammarström A. Socioeconomic disadvantage in adolescent women and metabolic syndrome in mid-adulthood: An examination of pathways of embodiment in the Northern Swedish Cohort. Soc Sci Med. 2012;74:1630–1638. doi: 10.1016/j.socscimed.2012.01.044. [DOI] [PubMed] [Google Scholar]
- 18.Miller GE, Lachman ME, Chen E, et al. Pathways to resilience: maternal nurturance as a buffer against the effects of childhood poverty on metabolic syndrome at midlife. Psychol Sci. 2011;22(12):1591–1599. doi: 10.1177/0956797611419170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Whisman MA, Uebelacker LA, Settles TD. Marital distress and the metabolic syndrome: Linking social functioning with physical health. J Fam Psychol. 2010;24(3):367–370. doi: 10.1037/a0019547. [DOI] [PubMed] [Google Scholar]
- 20.Perez GK, Cruess D. The impact of familism on physical and mental health among Hispanics in the U.S. Health Psychol Rev. 2011:1–33. doi: 10.1080/17437199.2011.569936. [DOI] [PubMed] [Google Scholar]
- 21.Katiria Perez G, Cruess D. The impact of familism on physical and mental health among Hispanics in the United States. Health Psychol Rev. 2014;8(1):95–127. doi: 10.1080/17437199.2011.569936. doi:10.1080/17437199.2011.569936. [DOI] [PubMed] [Google Scholar]
- 22.Gallo LC, Penedo FJ, Espinosa de los Monteros K, et al. Resiliency in the face of disadvantage: do Hispanic cultural characteristics protect health outcomes? J Pers. 2009;77(6):1707–1746. doi: 10.1111/j.1467-6494.2009.00598.x. [DOI] [PubMed] [Google Scholar]
- 23.Medina-Inojosa J, Jean N, Cortes-Bergoderi M, et al. The Hispanic paradox in cardiovascular disease and total mortality. Prog Cardiovasc Dis. 2014;57(3):286–292. doi: 10.1016/j.pcad.2014.09.001. doi:10.1016/j.pcad.2014.09.001. [DOI] [PubMed] [Google Scholar]
- 24.Hovey JD, Magana C. Acculturative stress, anxiety, and depression among Mexican farmworkers in the midwest United States. J Immigr Health. 2000;2:119–131. doi: 10.1023/A:1009556802759. [DOI] [PubMed] [Google Scholar]
- 25.Rodriguez N, Mira CB, Paez ND, et al. Exploring the complexities of familism and acculturation: central constructs for people of Mexican origin. Am J Community Psychol. 2007;39:61–77. doi: 10.1007/s10464-007-9090-7. [DOI] [PubMed] [Google Scholar]
- 26.Diez-Roux AV, Detrano R, Jackson DR, Jr, et al. Acculturation and socioeconomic position as predictors of coronary calcification in a multiethnic sample. Circulation. 2005;112(11):1557–1565. doi: 10.1161/CIRCULATIONAHA.104.530147. [DOI] [PubMed] [Google Scholar]
- 27.Koya DL, Egede LE. Association between length of residence and cardiovascular disease risk factors among an ethnically diverse group of United States immigrants. J Gen Intern Med. 2007;22:841–846. doi: 10.1007/s11606-007-0163-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bird HR, Canino GJ, Davies M, et al. Prevalence and correlates of antisocial behaviors among three ethnic groups. J Abnorm Child Psych. 2001;29:465–478. doi: 10.1023/a:1012279707372. [DOI] [PubMed] [Google Scholar]
- 29.Page RL. Positive pregnany outcomes in Mexican immigrants: What can we learn? J Obstet Gynecol Neonatal Nurs. 2004;33(6):783–790. doi: 10.1177/0884217504270595. [DOI] [PubMed] [Google Scholar]
- 30.Losada A, et al. Cross-cultural study comparing the association of familism with burden and depressive symptoms in two samples of Hispanic dementia caregivers. Aging Ment Health. 2006;10(1):69–76. doi: 10.1080/13607860500307647. [DOI] [PubMed] [Google Scholar]
- 31.Lawsin C, Erwin D, Bursac Z, et al. Heterogeneity in breast and cervical cancer screening practices among female Hispanic immigrants in the United States. J Immigr Minor Health. 2011;13(5):834–841. doi: 10.1007/s10903-010-9378-9. doi:10.1007/s10903-010-9378-9.PubMed. [DOI] [PubMed] [Google Scholar]
- 32.Ashing-Giwa KT, Padilla GV, Bohorquez DE, et al. Understanding the breast cancer experience of Latina women. J Psychosoc Oncol. 2006;24(3):19–52. doi: 10.1300/J077v24n03_02. [DOI] [PubMed] [Google Scholar]
- 33.Mulvaney-Day NE, Alegria M, Sribney W. Social cohesion, social support, and health among Latinos in the United States. Soc Sci Med. 2007;64(2):477–495. doi: 10.1016/j.socscimed.2006.08.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lehman BJ, Taylor SE, Kiefe CI, et al. Relation of childhood socioeconomic status and family environment to adult metabolic functioning in the CARDIA study. Psychosom Med. 2005;67(6):846–854. doi: 10.1097/01.psy.0000188443.48405.eb. [DOI] [PubMed] [Google Scholar]
- 35.Sorlie PD, Avilés-Santa LM, Wassertheil-Smoller S, et al. Design and implementation of the Hispanic community health study/study of Latinos. Ann Epidermiol. 2010;20(8):629–641. doi: 10.1016/j.annepidem.2010.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Grundy SM. Atlas of atherosclerosis and the metabolic syndrome. 5th ed. New York: Spring Science and Business Media; 2011. [Google Scholar]
- 37.LaVange LM, Kalsbeek WD, Sorlie PD, et al. Sample design and cohort selection in the Hispanic community health study/study of Latinos. Ann Epidemiol. 2010;20:642–649. doi: 10.1016/j.annepidem.2010.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ellison J, Jandorf L, Duhamel K. Assessment of the Short Acculturation Scale for Hispanics (SASH) among low-income, immigrant Hispanics. J Cancer Educ. 2011;26(3):478–483. doi: 10.1007/s13187-011-0233-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Andresen EM, Malmgren JA, Carter WB, et al. Screening for depression in well oder adults: Evaluation of a short form of the CESD (Center for Epidemiologic Studies Depression scale) Am J Prev Med. 1994;10:77–84. [PubMed] [Google Scholar]
- 40.Cohen S, Memelstein R, Kamarck T, et al. Measuring the functional components of social support. In: Sarason IG, Sarason B, editors. Social support: Theory, research and application. The Hague: Martinus Nijhoff; 1985. pp. 73–94. [Google Scholar]
- 41.Moos RH, Moos BS. Family environment scale. Manual. 3rd ed. Palo Alto: Consulting Psychologists Press; 1994. [Google Scholar]
- 42.Dimitrov DM. Testing for factorial invariance in the context of construct validation. Measurement and Evaluation in Counseling and Development. 2010;43:121–149. [Google Scholar]
- 43.Grundy SM, Cleeman JI, Daniels SR, et al. Diagnosis and management of the metabolic syndrome. An American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005;112:2735–2752. doi: 10.1161/CIRCULATIONAHA.105.169404. [DOI] [PubMed] [Google Scholar]
- 44.Aiken LS, West SG. Multiple Regression: Testing and Interpreting Interactions. Newbury Park, CA: Sage; 1991. [Accessed June 26, 2013]. US Department of Health and Human Services. The Office of Minority Health. http://minorityhealth.hhs.gov/templates/browse.aspx?lvl=2%lvlID=54. [Google Scholar]
- 45.Mair CA, Cutchin MP, Kristen PM. Allostatic load in an environmental riskscape: The role of stressors and gender. Health Place. 2011;17(4):978–987. doi: 10.1016/j.healthplace.2011.03.009. doi:10.1016/j.healthplace.2011.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Schmaltz HN, Southern D, Ghali W, et al. Living alone, patient sex and mortality after acute myocardial infarction. J Gen Intern Med. 2007;22(5):572–578. doi: 10.1007/s11606-007-0106-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Coyne JC, Rohrbaugh MJ, Shoham V, et al. Prognostic importance of marital quality for survival of congestive heart failure. Am J Cardiol. 2001;88(5):526–529. doi: 10.1016/s0002-9149(01)01731-3. [DOI] [PubMed] [Google Scholar]
- 48.Schmied EA, Parada H, Horton LA, Madanat H, Ayala GX. Family support is associated with behavioral strategies for healthy eating among Latinas. Health Educ Behav. 2013 doi: 10.1177/1090198113485754. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 49.Rivera FI, Guarnaccia PJ, Mulvaney-Day N, et al. Family cohesion and its relationship to psychological distress among Latino groups. Hisp J behave Sci. 2008;30(3):357–378. doi: 10.1177/0739986308318713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Li S, Horner P, Delva J. Social capital and cigarette smoking among Latinos in the United States. Subst Abuse Rehabil. 2012;(Supplement 1):83–92. doi: 10.2147/SAR.S31164. PMID: 22706166 [PubMed] PMCID: PMC3374601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Estrada-Martinez LM, Padilla MB, Caldwell CH, et al. Examining the influence of family environments on youth violence: A comparison of Mexican, Puerto Rican, Cuban, non-Latino Black, and non-Latino White adolescents. J Youth Adolesc. 2011;40(8):1039–1051. doi: 10.1007/s10964-010-9624-4. [DOI] [PubMed] [Google Scholar]
- 52.Lehman BJ, Taylor SE, Kiefe CI, et al. Relation of childhood socioeconomic status and family environment to adult metabolic functioning in the CARDIA study. Psychosom Med. 2005;67(6):846–854. doi: 10.1097/01.psy.0000188443.48405.eb. [DOI] [PubMed] [Google Scholar]
- 53.Zeller MH, Reiter-Purtill J, Modi AC, et al. Controlled study of critical parent and family factors in the obesigenic environment. Obesity. 2007;15(1):126–136. doi: 10.1038/oby.2007.517. [DOI] [PubMed] [Google Scholar]