Abstract
We report a case of a patient with more than 30 years of repeated syncopes, always following food intake. The patient was diagnosed with a swallow-related third-degree atrioventricular block and successfully treated with an artificial pacemaker.
Background
This case is important because, although syncopes among the population are common, in this case, the syncope was from a rare cause, and it was easily treatable with an artificial pacemaker. Furthermore, the patient's 30-year history of undiagnosed syncopes is interesting, as it shows for how long advanced atrioventricular (AV) block can perpetuate and still be correctable.
Case presentation
An otherwise healthy 62-year-old man was referred to the department of cardiology, for assessment of syncope. He had, at 32 years of age, experienced syncope after finishing breakfast. At the time, he was busy at a new work place and for this reason, only went to see his general practitioner (GP) once. Initially it was suspected that the incidence was probably related to ‘stress’ and no further investigations were undertaken. For 30 years, however, repeated syncopes, ranging from 1 to 4/year, continued to trouble him, always in relation to food intake, and always at the end of a meal. He never experienced syncope during physical exercise, orthostasis or in any other specific situation usually related to syncope. For almost 30 years, he experienced dizziness or syncope following meals and had done so with increasing frequency over the past few years. On some occasions, he could avert pre-syncope by grabbing the dining table hard and clenching his fists for some minutes. His wife, who observed the events on numerous occasions, explained how her husband suddenly lost consciousness and without warning lost muscle tone. He always woke up shortly after and was well. She eventually succeeded in persuading him to see his GP again and, alarmed to learn about his repeated syncopes, his GP now referred him for further investigation.
On the basis of the history, the patient was referred for Holter, echocardiography and physical investigation, to rule out post-prandial hypotension. Physical assessments including resting 12-lead ECG, transthoracic echocardiography, 24 h ambulatory blood pressure monitoring and full blood screening including thyroid-stimulating hormone, were all normal. The patient was referred for a ‘meal-test’, during which he ingested a full meal during monitoring of ECG, blood pressure, cardiac output, heart rate and systemic vascular resistance using a Finapress device. No changes were seen during or after the meal. Gastrointestinal studies were normal.
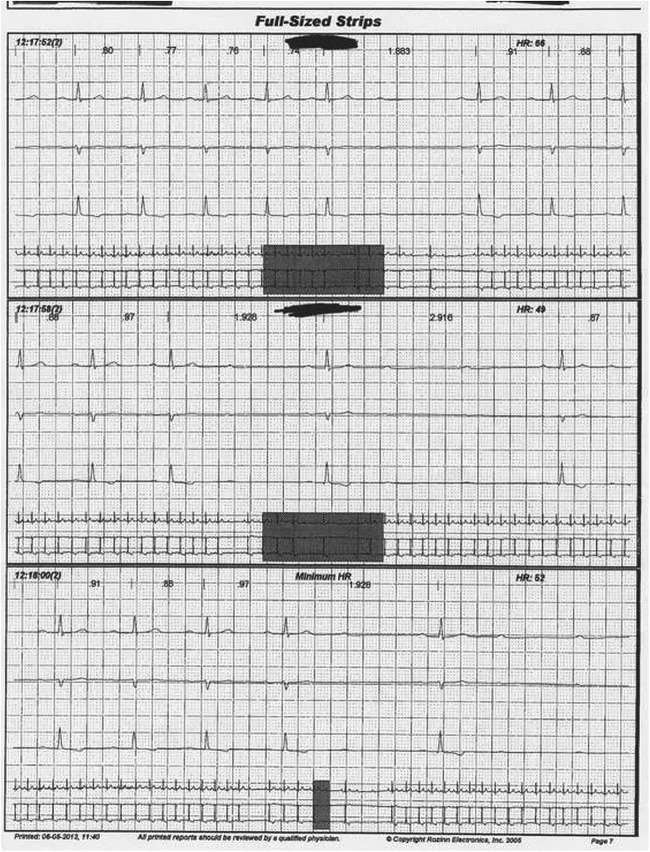
Two-day Holter monitoring, however, demonstrated intermittent second-degree Mobitz type 2 AV block and short periods of third-degree AV block on two consecutive dates at the exact time when he was having lunch (figure 1). The patient was referred for DDD-pacemaker implantation, and he has now been well without syncope for 2 years.
Figure 1.
ECG during a meal. Food ingestion is followed by second-degree Mobitz type 2 and by third-degree atrioventricular blockade.
Discussion
This report describes a case of year-long syncopes associated with paroxysmal third-degree AV block and second-degree Mobitz type 2 AV block secondary to food intake. Syncope during food intake is a rare problem and can be caused by the swallow reflex. Swallow syncope is usually grouped among the neurally mediated syncope syndromes. Swallow syncope was first reported in the English literature in 1973.1 Eighty-four cases have, until 2014, been published in the English literature.2–6
Neurally mediated syncopal syndromes include a number of related disturbances of cardiovascular controlled reflexes characterised by transient bradycardia or vasodilation of the vascular system,7 or both. The mechanism of swallow syncope is not completely understood, but administration of atropine is effective in preventing bradycardia and syncope, and hence the vagal reflex is involved in cardiovascular inhibition.8 In the cases published in the literature, implantation of an artificial pacemaker relieved symptoms for most;9 this is in some contrast to patients experiencing frequent vasovagal reactions from, for instance, orthostasis, where implantation of a pacemaker can be somewhat disappointing,10 since these patients may still faint from the vasodepressor feature of the reflex. Thus, it was early shown that, with vasovagal reaction, atropine may alleviate the bradycardia, but the syncope is still seen following widespread sympathicolysis-related vasodilation.8
Oesophageal mechanoreceptors, activated by stretching, play a role in initiating such periods of second-degree and third-degree AV block by stimulating the afferent pathway of the vagal nerve. Thus, such disturbances are known to occur in patients with organic or functional disorders of the oesophagus,11 but our patient was not so diagnosed. Wataru et al found several underlying conditions (cardiac disease, digestive disease, lung cancer, thoracic aortic aneurysm) causing swallow syncope, and also found a significant number of cases where no underlying disease could be identified. One case report, by Lambiris et al, was, likewise, concerning a patient with a 30-year history, but in that patient's case, swallow syncope was related to a vasovagal reaction (only demonstrating a second-degree AV block after ingestion of a large amount of a cold beverage, that is, a normal reaction to head-up tilt and sublingual nitroglycerin), whereas our patient had swallow syncope related to third-degree AV block.11 This was clearly documented to be present during everyday life; also, third-degree AV blocks are normally related to a severely diseased AV node and have not been previously reported for the duration experienced by our patient. Moreover, the efferent impulses travelling from the brainstem to the sinoatrial and AV nodes lead to bradycardia and, consequently, lowered cardiac output, causing temporal cerebral hypoperfusion and hence dizziness or even syncope.2 Other studies imply that syncope can occur when sympathetic withdrawal to the peripheral vessels lead to vasodilation and hypotension without the presence of bradycardia.2 Clenching of the fists, a manoeuvre the patient used to alleviate signs of cerebral hypoperfusion, is associated with a pressor reflex causing sympathetic stimulation and improvement of blood pressure.12 Thus, depression of sympathetic outflow may still be part of the problem but, nevertheless, our patient was completely relieved by insertion of an artificial pacemaker.
Vasodilation can be seen in postprandial patients, usually the elderly, without a vagal reflex and not initiated by oesophageal mechanoreceptors. These patients experience post-prandial arterial hypotension and, if not syncope, at least dizziness on standing. This is probably related to insulin-mediated vasodilation.13 Our patient had regularly been fainting since his early 30s, which is not typical of insulin-related vasodepression, and determination of cardiac output and peripheral vascular resistance was normal.
Swallow-related AV block is a rare incident that can be readily ameliorated by insertion of an artificial pacemaker.
Learning points.
Syncope during food intake is an uncommon condition and can be caused by the swallow reflex.
Swallow syncope is grouped among the neurally mediated syncope syndromes and is often related to atrioventricular block.
The condition can be improved by insertion of an artificial pacemaker.
Footnotes
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Tuzcu V, Halakatti R. Swallow syncope associated with complete atrioventricular block in an adolescent. Pediatr Cardiol 2007;28:409–11. 10.1007/s00246-006-0167-0 [DOI] [PubMed] [Google Scholar]
- 2.Mitra S, Ludka T, Rezkalla SH et al. Swallow syncope: a case report and review of the literature. Clin Med Res 2011;9:125–9. 10.3121/cmr.2010.969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lambiris I, Mendoza I, Helguera M et al. Thirty years of blackouts: a case report of swallow syncope. J Community Hosp Intern Med Perspect 2013;3 10.3402/jchimp.v3i1.20323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim C, Ko SM, Kim N et al. A case of swallow syncope associated with cold beverage ingestion. Korean Circ J 2012;42:212–15. 10.4070/kcj.2012.42.3.212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Foreman J, Vigh A, Wardrop RM. Hard to swallow. Am J Med 2011;124:218–20. 10.1016/j.amjmed.2010.10.009 [DOI] [PubMed] [Google Scholar]
- 6.Rezvani M, Casillas SG, Antanavicius G. Swallow syncope after laparoscopic vertical sleeve gastrectomy. Surg Obes Relat Dis 2013;9:e77–8. 10.1016/j.soard.2013.03.002 [DOI] [PubMed] [Google Scholar]
- 7.Kakuchi H, Sato N, Kawamura Y. Swallow syncope associated with complete atrioventricular block and vasovagal syncope. Heart 2000;83:702–4. 10.1136/heart.83.6.702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moya A, Sutton R, Ammirati F et al. Guidelines for the diagnosis and management of syncope (version 2009). Eur Heart J 2009;30:2631–71. 10.1093/eurheartj/ehp298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Raviele A, Giada F, Menozzi C et al. A randomized, double-blind, placebo-controlled study of permanent cardiac pacing for the treatment of recurrent tilt-induced vasovagal syncope. The vasovagal syncope and pacing trial (SYNPACE). Eur Heart J 2004;25:1741–8. 10.1016/j.ehj.2004.06.031 [DOI] [PubMed] [Google Scholar]
- 10.Lewis T. A Lecture on vasovagal syncope and the carotid sinus mechanism. BMJ 1932;1:873–6. 10.1136/bmj.1.3723.873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Omi W, Murata Y, Yaegashi T et al. Swallow syncope, a case report and review of the literature. Cardiology 2006;105:75–9. 10.1159/000089543 [DOI] [PubMed] [Google Scholar]
- 12.Clarke DA, Medow MS, Taneja I et al. Initial orthostatic hypotension in the young is attenuated by static handgrip. J Pediatr 2010;156:1019–22, 1022.e1 10.1016/j.jpeds.2010.01.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Okamoto M, Hashimoto M, Yamada T et al. Postprandial atrioventricular block in a patient with diabetes mellitus. Intern Med 1997;36:579–81. 10.2169/internalmedicine.36.579 [DOI] [PubMed] [Google Scholar]