Abstract
A 62-year-old woman with idiopathic cardiomyopathy and class IIIB/stage C heart failure sustained right pulmonary artery injury from a Swan-Ganz catheter during a pretransplant work up. Postprocedure, it was noted that the patient's segmental pulmonary artery catheter was wedged for an unclear period of time. The patient developed a small volume of blood-tinged sputum and a chest CT revealed a 1.3 cm pseudoaneurysm in the right middle lobe medial segment pulmonary artery and a small area of haemorrhage. The patient underwent pulmonary artery preserving coil embolisation of the pseudoaneurysm to prevent further right heart strain, given an ejection fraction of 20%, which resolved haemoptysis. Imaging studies showed preserved distal outflow and no evidence of residual pseudoaneurysm filling.
Background
A pulmonary artery pseudoaneurysm (PAP) is an uncommon vascular defect—an often clinically silent enlargement of a pulmonary artery that can lead to sudden rupture and death from haemorrhage.1–3 While causes of PAPs include genetics, cardiovascular disease and neoplasms, a large number of cases are iatrogenic.1 The incidence of pulmonary artery rupture secondary to catheterisation is only ∼0.2%, but studies have shown the mortality rate to be as high as 50%.4 PAP is a cause for emergent intervention, which may either be surgical or endovascular. Coil embolisation is an effective minimally invasive method of PAP resolution that can preserve vascular outflow.1 We report a case of PAP resulting from Swan-Ganz catheterisation in a complicated patient with a history of heart failure and pulmonary hypertension. Coil embolisation was able to successfully stop the haemoptysis, resolve the pseudoaneurysm and preserve blood flow to the distal lung tissue.
Case presentation
A 62-year-old woman with cardiomyopathy and class III/stage C heart failure presented with haemoptysis and lung haemorrhage after undergoing a routine pretransplant work up. After the procedure, it was discovered that the Swan-Ganz catheter had been wedged for an unknown period of time, causing damage to the medial segment of the right middle lobe pulmonary artery. Chest CT scan revealed a 1.3 cm pulmonary artery pseudoaneurysm (figure 1) and a small area of haemorrhage in the lung parenchyma. The patient's medical history was notable for a 14-year history of non-ischaemic cardiomyopathy diagnosed after a venous thrombosis-induced cardiac arrest. Her history was also notable for class III congestive heart failure, conduction system abnormalities and pulmonary hypertension. Her family history was significant for a father and brother diagnosed with congestive heart failure and cardiomyopathy, respectively. The social history was unremarkable. The patient's ejection fraction was 20% and it was determined that coil embolisation of the aneurysm would be the appropriate therapy in an effort to preserve the distal outflow, and avoid exacerbation of existing pulmonary hypertension and heart failure.
Figure 1.
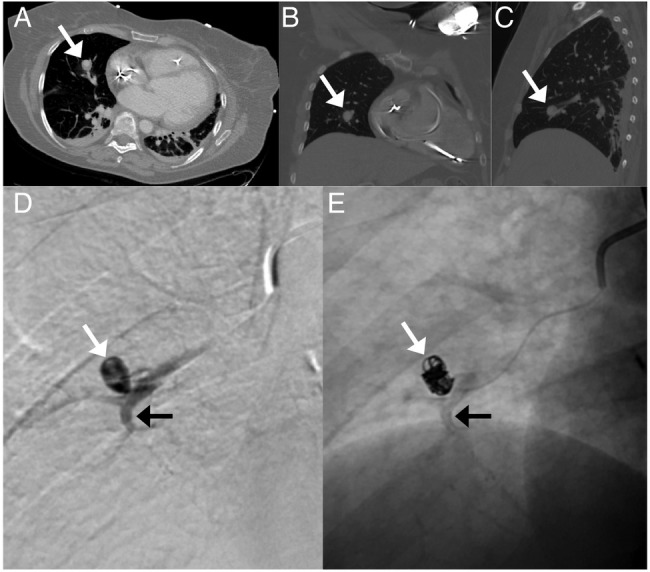
CT and digital subtraction angiography (DSA) images of the pulmonary artery pseudoaneurysm. Axial (A), coronal (B) and sagittal (C) views of the pseudoaneurysm in the right middle lobe (white arrow). (D) DSA following contrast injection from the microcatheter inside the pseudoaneurysm (white arrow) arising from a right middle lobe medial segment artery (black arrow). (E) Subsequent coil embolisation of the pseudoaneurysm (white arrow); flow to the distal pulmonary artery (black arrow) is preserved.
Differential diagnosis
Bronchitis/bronchiectasis
Pulmonary embolism
Pulmonary arteriovenous malformations
Neoplasm
Airway trauma
Infection
Immune disorders
Coagulopathy
Treatment
Following an episode of haemoptysis and CT diagnosis of pseudoaneurysm, the patient underwent superselective coil embolisation of a right middle lobe medial segment pulmonary artery pseudoaneurysm (figure 1). Access was through the right femoral vein, under local anaesthetic. A microcatheter was meticulously navigated into the microscopic defect in the arterial wall to enter the pseudoaneurysm sac; multiple 2–3 mm fibred coils were delivered into the sac only, preserving flow in the segmental pulmonary artery (figure 1). The treatment was uncomplicated and recovery proceeded as expected.
Outcome and follow-up
Postembolisation angiography showed no filling of the pseudoaneurysm. Distal outflow was preserved to the middle lobe of the lung. Haemoptysis ceased after treatment. No complications were noted in follow-up. At 2-month follow-up the lungs were well inflated and clear with no oedema or haemorrhage. Neither heart failure nor pulmonary hypertension was reported to be exacerbated following coil embolisation.
Discussion
Pulmonary artery pseudoaneurysms are serious though rare conditions, most often associated with interventional procedures, pulmonary neoplasms, collagenous disease and chest trauma. Regardless of their aetiology, it is important to identify and treat PAPs quickly to prevent rupture, haemorrhage and, ultimately, death.4 5 The most common clinical presentation of a PAP is haemoptysis, which may also be preceded or accompanied by respiratory insufficiency, asphyxia and hypovolaemic shock. If a PAP is suspected, imaging should be used to confirm the diagnosis.4 6 Pseudoaneurysm and haemorrhage into the lung may be identified with CT. Arterial angiography is also useful and any extravasation of contrast medium should be noted. The ultimate goal of treatment is to prevent the filling of the pseudoaneurysm and any extravasation of blood.1 7
Since a large number of PAP cases are iatrogenic, it is vital to adjust and optimise practice standards to minimise this serious complication.4 Although treatments for PAPs range from watchful waiting to embolisation and surgical intervention, no gold standard treatment exists due to a lack of controlled studies.7–9 Treatment should be tailored to the patient's specific clinical presentation and complications. In some cases it is not necessary to preserve distal outflow, as in the cases of lung resection or lobectomy; such cases have successfully been handled by both surgery and embolisation. In other cases, preservation of outflow is vital. In some instances, surgical interventions can be complicated by bleeding risks or adhesions from previous surgeries, thereby necessitating endovascular intervention. Coil embolisation is effective and circumvents the need to undergo more invasive surgery.2 4 10 Coil embolisation can also preserve distal outflow while effectively and completely preventing filling of the pseudoaneurysm.
Learning points.
Pulmonary artery pseudoaneurysms are rare; however, iatrogenic causes are more common.
In patients with compromised pulmonary or cardiac function, it is vital to preserve distal blood flow of pulmonary arteries.
Minimally invasive coil embolisation can be used to resolve pulmonary artery pseudoaneurysms while preserving flow.
Footnotes
Twitter: Follow Rahmi Oklu at @rahmioklu
Contributors: RO, MGP and KB were responsible for conception and design, acquisition of data or analysis and interpretation of data. RO, MGP and KB were responsible for drafting the article or revising it critically for important intellectual content. RO, MGP and KB were responsible for final approval of the version published.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Matsumura Y, Shiono S, Saito K et al. Pulmonary artery pseudoaneurysm after lung resection successfully treated by coil embolization. Interact Cardiovasc Thorac Surg 2010;11:364–5. 10.1510/icvts.2010.236661 [DOI] [PubMed] [Google Scholar]
- 2.Zhang J, Jiang S. Massive haemoptysis from central pulmonary arterial pseudoaneurysm secondary to advanced lung cancer: successful treatment by Guglielmi detachable coil embolization. Clin Respir J 2015. EPUB July 14, 2015 10.1111/crj.12333 [DOI] [PubMed] [Google Scholar]
- 3.Nistri M, Acquafresca M, Pratesi A et al. Bronchial artery embolization with detachable coils for the treatment of haemoptysis: preliminary experience. La Radiologa Medica 2008;113:452–60. 10.1007/s11547-008-0253-x [DOI] [PubMed] [Google Scholar]
- 4.Keymel S, Merx MW, Zeus T et al. Stenting as a rescue treatment of a pulmonary artery false aneurysm caused by Swan-Ganz catheterizaiton. Case Rep Pulmonol 2014;2014:893647 10.1155/2014/893647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wong KP, Young N, Marksen G. Bronchial artery embolization to control haemoptysis. Australas Radiol 1994;38:256–9. 10.1111/j.1440-1673.1994.tb00193.x [DOI] [PubMed] [Google Scholar]
- 6.Chun JY, Belli AM. Immediate and long-term outcomes of bronchial and non-bronchial systemic artery embolization for the management of haemoptysis. Eur Radiol 2010:20;558–65. 10.1007/s00330-009-1591-3 [DOI] [PubMed] [Google Scholar]
- 7.Sheehy N, Ford S, McDermott R et al. Ultrasonographically guided percutaneous embolization of a pulmonary pseudoaneurysm. J Vasc Interv Radiol 2006;17:895–8. 10.1097/01.RVI.0000217939.77021.85 [DOI] [PubMed] [Google Scholar]
- 8.Kim YG, Yoon HK, Ko GY et al. Long-term effect of bronchial artery embolization in Korean patients with haemoptysis. Respiratory 2006;11:776–81. [DOI] [PubMed] [Google Scholar]
- 9.Trambert JJ, Abubaker SJ, Kanner BJ. Giant mycotic pulmonary artery pseudoaneurysm treated by guide wire and coil embolization. J Vasc Interv Radiol 2014;25:1643 10.1016/j.jvir.2014.05.003 [DOI] [PubMed] [Google Scholar]
- 10.Davidoff AB, Udoff EJ, Schonfeld SA. Intraaneurysmal embolization of a pulmonary artery aneurysm for control of hemoptysis. Am J Roentgenol 1964;142:1019–20. 10.2214/ajr.142.5.1019 [DOI] [PubMed] [Google Scholar]


