Abstract
Syphilis can show unexpected clinical characteristics rendering its diagnosis difficult. We report on two cases of secondary syphilis presenting with atypical histories of knee or cervical pain and cough. Both had bone involvement and one, pulmonary involvement, documented by MRI, CT scan and PCR. Both responded well to therapy with intravenous aqueous penicillin G followed by intramuscular benzathine penicillin G, but a pulmonary adenocarcinoma was diagnosed during follow-up in one case.
Background
Following a decline towards the end of the last century, syphilis is currently re-emerging, probably secondary to a change in sexual behaviour following improvements in HIV therapy, and particularly in men who have sex with men (MSM).1 Nowadays, physicians could thus see more patients with syphilis, a disease no longer well recognised that can adopt unexpected clinical pictures. We report on two cases of atypical secondary syphilis that were not diagnosed on first presentation, one of which was later diagnosed with lung adenocarcinoma.
Cases presentation
The first patient, a 47-year-old HIV-positive MSM, mentioned a slight pain on the internal side of his left knee during a routine outpatient visit. Antiretroviral therapy (ART) consisting of tenofovir, emtricitabin and efavirenz had been started 1 month earlier, while the patient was still asymptomatic and had not experienced any opportunistic infection. At that time, his CD4 lymphocyte count was 596 cells/mm3 and his HIV viral load was 104 856 copies/mL. Serology for syphilis had been negative 2 and 1 year before starting ART. Clinical examination was unremarkable. White cell count (WCC), haemoglobin, thrombocytes and serum creatinine were in normal ranges. The patient's HIV-viral load was 438 copies/mL. A topical non-steroidal anti-inflammatory gel was prescribed for his knee, ART was continued and a new visit planned. Six weeks later, he presented with worsening pain in his left knee, mainly at night, and myalgias in his lower limbs, alongside polyarthralgia, fatigue and malaise. He had lost 2 kg. Desquamating lesions were seen on his palms and soles (figure 1A, B).
Figure 1.

Desquamating skin lesions of palms and soles associated with secondary syphilis.
The second patient, a 49-year-old HIV-negative woman, a smoker, diagnosed with chronic hepatitis C 9 months earlier, presented to the emergency room, with a 1-week history of disabling cervical pain. She had visited her family physician 2 weeks before for low-grade fever, night sweats and dry cough. Clinical examination was unremarkable except for bilateral cervical lymphadenopathy. WCC was 12 100 cells/mm3, C reactive protein 42.6 mg/L, alanine aminotransferase (ALAT) 36 UI/L, aspartate aminotransferase (ASAT) 57 UI/L, γ-glutamyl transpeptidase 107 UI/L and alkaline phosphatase 162 UI/L. Chest X-ray, later confirmed by CT scan, revealed an upper left lung infiltrate (figure 2A). Cervical MRI showed osteitis of the dens of the axis with inflammatory infiltration of pre-vertebral soft tissues (figure 3A). Tuberculosis was suspected and the patient was hospitalised for further investigations. Four days later, skin lesions of the soles were noticed (figure 4).
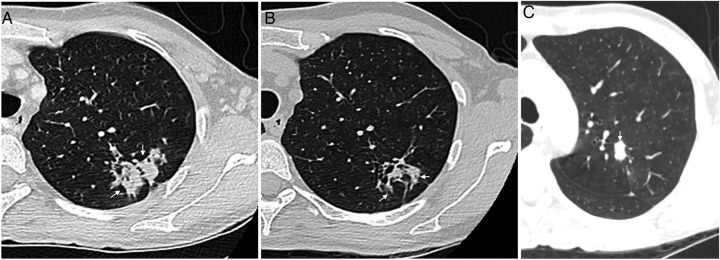
Figure 2.
CT scan with a left upper lung lobe parenchymal lesion due to T. pallidum before (A) and after (B) treatment with penicillin, and adenocarcinoma diagnosed 1 year later (C).
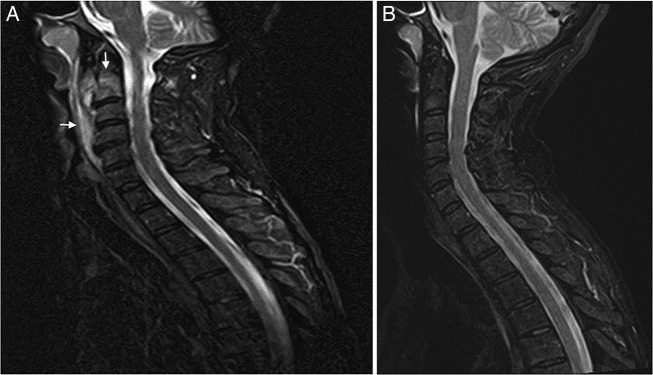
Figure 3.
Cervical MRI (T2 with fat saturation) with osteitis of the axis and tumefaction of prevertebral soft tissue associated with secondary syphilis (A), and complete resolution after treatment with penicillin (B).
Figure 4.

Skin lesions of soles associated with secondary syphilis.
Investigations
First patient: Serum rapid plasma reagin (RPR) and Treponema pallidum particle agglutination (TPPA) were 1:256 and >1:20 480, respectively. Knee X-ray and MRI revealed osteitis (figure 5A, B). Cerebrospinal fluid (CSF) showed 11 leucocytes/µL (91% neutrophils) and an elevated protein concentration of 970 mg/L. CSF RPR and TPPA were 1:2 and 1:1024, respectively. T. pallidum was detected by PCR in the knee biopsies but histological changes corresponded to unspecific inflammation without Treponema seen on Whartin-Starry stains.
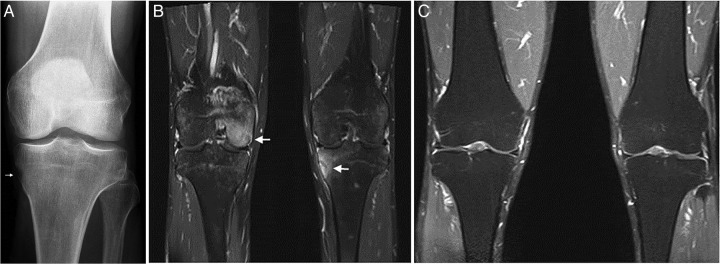
Figure 5.
Left knee X-ray with cortical erosion (A), and MRI of both knees (T1 with fat saturation) with femoral and tibial osteitis due to T. pallidum (B), and complete resolution after treatment with penicillin (C).
Second patient: RPR and TPPA were 1:32 and >1:20 480, respectively. Gynaecological examination revealed a possible chancre's scar in the right labia majora. CSF showed no abnormalities. T. pallidum was detected by PCR in bronchioalveolar lavage and bronchial aspirate, which contained neither malignant cells in cytological analysis nor mycobacteria in cultures. No biopsies were performed.
Treatment
Both patients were treated with 4 million units of intravenous aqueous penicillin G every 4 h for 14 days, followed by two weekly doses of 2.4 million units of intramuscular benzathine penicillin G.
Outcome and follow-up
Symptoms and cutaneous lesions resolved within 2–3 weeks in both patients.
First patient: RPR titres at 6, 16 and 24 months were 1:32, 1:16 and 1:4, respectively. Follow-up MRIs, performed 2 and 6 months later, showed a clear improvement of the knee osteitis (figure 5C).
Second patient: RPR titres were 1:1 and 0:1 at 6 and 12 months, respectively. Follow-up MRI showed a clear improvement of the axis osteitis (figure 3B). Initial follow-up thoracic CT scans revealed, at 2 and 6 months, a decrease of the left lung infiltrate, but persistence of a retractile fibromatous scar (figure 2B). One year later, a new thoracic CT scan revealed a newly appearing lesion below the fibromatous scar (figure 2C). Biopsies showed an adenocarcinoma. No metastasis was found and a lobectomy was successfully performed.
Discussion
The classic description of syphilis corresponds to the characteristic clinical presentation of its three stages: chancre of primary syphilis, skin rash of secondary syphilis, or aortic insufficiency and neurological manifestations of tertiary syphilis.1 The two cases of secondary syphilis described here had unusual initial presentations consisting of gonalgia due to an osteolytic lesion in one patient, and cervicalgia and cough due to osteitis of the dens of the axis and pulmonary involvement in the other. They were diagnosed only weeks after they had first reported their symptoms, once skin lesions were present or noticed, and motivated serological testing.
Whereas bone involvement is well-known in congenital and tertiary syphilis, it has only rarely been reported in secondary syphilis. Recently, Park et al2 reviewed 37 cases of secondary syphilis with osteitis, 11 of whom had HIV infection with a median CD4 lymphocyte count of 343 cells/mm3. As in our patients, syphilis was suspected based on the mucocutaneous findings in 76% of these cases, corresponding most often to a maculopapular rash and sometimes to a recent history of genital ulcer. In nine patients (24%), no mucocutaneous lesions were present and the only evidence of early syphilis was the results of non-treponemal serological tests. The bones most often affected were the long bones of the limbs, followed by the skull, ribs, clavicles, spine and sternum.2 An additional case published since then showed osteitis of the dens of the axis, with MRI findings very similar to those of our second patient.3 Bone pain, often worsening during the night, was the commonest complaint in secondary syphilis with osteitis.
Lung involvement in secondary syphilis has been reported even more rarely. In 2006, David et al4 reviewed nine cases of secondary pulmonary syphilis that had been published in the English language literature since 1967. We could find eight more English language case reports from 2009 to 2014.5–12 One of them presented with both bone and lung lesions, as did our second patient.12 Concomitant HIV infection was present in four patients, absent in seven and unknown in six. Signs and symptoms could be absent but varied and included cough, dyspnoea and chest pain. Radiological presentation included infiltrates and solitary or multiple nodules, sometimes associated with pleural effusion and mimicking malignant lesions. Our second case shows that this similarity in lung imaging could be misleading and falsely reassuring because both diseases (syphilis and carcinoma) can coexist, rendering long-term follow-up necessary.
Diagnosis of osseous or pulmonary syphilis in reported cases was most often made on the basis of radiological images resolving on penicillin in the context of positive serology. Identification of spirochetes in bones or lungs often proved difficult. They were only rarely seen by darkfield microscopy or on Warthin-Starry-stained biopsies.2 4 Access to new diagnostic tools during the last decades, such as PCR, CT scan and MRI, might soon reveal that bone and lung involvement is not as rare as previously thought in secondary syphilis.
It is also possible that such unknown lesions were cured in the past with the administration of one single dose of 2.4 million units of intramuscular benzathine penicillin G, as still currently recommended for classical secondary syphilis.13 Most of the reported cases with bone or lung involvement were, nevertheless, treated for prolonged periods with intramuscular or intravenous penicillin G. As stated by Park et al,2 since the appropriate regimens for these forms of syphilis have not yet been determined in clinical trials, the single-dose regimen should only be used with caution in such situations. Waiting for more data, we concur with their conclusion and believe that 2–4 weeks of treatment with either intramuscular or intravenous penicillin should be preferred for patients with secondary syphilis and proven or suspected lung or bone involvement, not ignoring that a careful follow-up is warranted, particularly in the presence of risk factors for malignancy.
Learning points.
Syphilis is re-emerging, and secondary syphilis can have atypical presentations, including bone and lung lesions, with or without skin rash.
Osseous and pulmonary involvement have rarely been reported in secondary syphilis, but might be more frequent than commonly thought.
X-ray, CT scan or MRI findings showing osteitis, lung infiltrates or lung nodules and associated with a skin rash, should suggest secondary syphilis.
Consider bone biopsy or bronchoalveolar lavage with PCR for Treponema pallidum in case of osseous or pulmonary lesions associated with serological findings typical for syphilis.
Secondary syphilis with microbiologically proven lung involvement does not rule out lung malignancy, particularly in patients with risk factors.
Acknowledgments
The authors acknowledge Dr Mohamed Ehab Kamel for the choice of pictures from CT scans and MRIs.
Footnotes
Contributors: FC and VA were responsible for the patients’ care, and drafted the manuscript. GG participated in the diagnosis and follow-up, and proof read the manuscript. NT supervised the diagnosis and treatment, and finalised the manuscript.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Mattei PL, Beachkofsky TM, Gilson RT et al. Syphilis: a reemerging infection. Am Fam Physician 2012;86:433–40. [PubMed] [Google Scholar]
- 2.Park KH, Lee MS, Hong IK et al. Bone involvement in secondary syphilis: a case report and systematic review of the literature. Sex Transm Dis 2014;41:532–7. 10.1097/OLQ.0000000000000164 [DOI] [PubMed] [Google Scholar]
- 3.Fabricius T, Winther C, Ewertsen C et al. Osteitis in the dens of the axis caused by Treponema pallidum. BMC Infect Dis 2013;13:347 10.1186/1471-2334-13-347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.David G, Perpoint T, Boibieux A et al. Secondary pulmonary syphilis: report of a likely case and literature review. Clin Infect Dis 2006;42:e11–15. 10.1086/499104 [DOI] [PubMed] [Google Scholar]
- 5.Meroni L, Trovati S, Antinori S. Generalised maculopapular rash and multiple nodular pulmonary lesions in an HIV-infected man. Thorax 2009;64:100 10.1136/thx.2008.098178 [DOI] [PubMed] [Google Scholar]
- 6.McCready JB, Skrastins R, Downey JF et al. Necrotic pulmonary nodules in secondary syphilis. CMAJ 2011;183:E163–6. 10.1503/cmaj.091479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim HJ, Seon HJ, Shin HH et al. Case report: pulmonary syphilis mimicking pulmonary hematogenous metastases on chest CT and integrated PET/CT. Indian J Radiol Imaging 2011;21:34–7. 10.4103/0971-3026.76052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alrajab S, Payne K, Areno J et al. A 40-year-old man with a nodular lung disease and skin rash. Chest 2012;141:1611–17. 10.1378/chest.11-1100 [DOI] [PubMed] [Google Scholar]
- 9.Elzouki AN, Al-Kawaaz M, Tafesh Z. Secondary syphilis with pleural effusion: case report and literature review. Case Rep Infect Dis 2012;2012:409896 10.1155/2012/409896 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kim SJ, Lee JH, Lee ES et al. A case of secondary syphilis presenting as multiple pulmonary nodules. Korean J Intern Med 2013;28:231–5. 10.3904/kjim.2013.28.2.231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sprenger K, Furrer H. Chameleons everywhere. BMJ Case Rep 2014;2014:bcr2014205608 10.1136/bcr-2014-205608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Manríquez J, Andino-Navarrete R, Andrighetti C. Skin rash, dyspnea and bone pain: secondary syphilis. Braz J Infect Dis 2015;19:96–7. 10.1016/j.bjid.2014.10.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Clement ME, Okeke NL, Hicks CB. Treatment of syphilis: a systematic review. JAMA 2014;312:1905–17. 10.1001/jama.2014.13259 [DOI] [PMC free article] [PubMed] [Google Scholar]