Abstract
Traditional risk factors of cardiovascular death in the general population, including body mass index (BMI), serum cholesterol, and blood pressure (BP), are also found to relate to outcomes in the geriatric population, but in an opposite direction. Some degrees of elevated BMI, serum cholesterols, and BP are reportedly associated with lower – instead of higher – risk of death among the elderly. This phenomenon is termed “reverse epidemiology” or “risk factor paradox” (such as obesity paradox) and is also observed in a variety of chronic disease states such as end-stage renal disease requiring dialysis, chronic heart failure, rheumatoid arthritis, and AIDS. Several possible causes are hypothesized to explain this risk factor reversal: competing short-term and long-term killers, improved hemodynamic stability in the obese, adipokine protection against tumor necrosis factor-α, lipoprotein protection against endotoxins, and lipophilic toxin sequestration by the adipose tissue. It is possible that the current thresholds for intervention and goals levels for such traditional risk factors as BMI, serum cholesterol, and BP derived based on younger populations do not apply to the elderly, and that new levels for such risk factors should be developed for the elderly population. Reverse epidemiology of conventional cardiovascular risk factors may have a bearing on the management of the geriatric population, thus it deserves further attention.
Keywords: Reverse Epidemiology, Risk Factor Paradox, Obesity Paradox, Cardiovascular Risk Factors, Mortality
INTRODUCTION
Geriatric population comprise a sizable proportion of the US population with more than 40 million individuals being 65+ years old (yo), 1 and it will reach more than 20% of the general population by 2050. 2 Cardiovascular (CV) sequelae are the leading cause of death in all Americans and their attributable deaths are even higher in the elderly population. 3 Therefore, mitigation of mortality risk among the elderly seems to benefit the most from CV risk factor modification. However, albeit counterintuitive, some conventional CV risk factors such as elevated body mass index (BMI), serum cholesterol, and blood pressure (BP) are reportedly linked to lower – instead of higher – risk of death among the elderly. 4–12 The phenomenon of established CV risk factors having a markedly different and even opposite predictive pattern is termed “reverse epidemiology” or “risk factor paradox” and it is also observed in a variety of chronic disease states such as end-stage renal disease requiring dialysis, chronic heart failure, rheumatoid arthritis, and AIDS. 13–15 These observations call into question the practice of extrapolating CV risk factor targets derived from the general population to the getiartic population. Hence, a better understanding of this phenomenon and its potential underlying causes may help refine treatment goals and yield improved outcomes among the elderly.
WEIGHT AND BODY COMPOSITION: IS OBESITY FAVORABLE?
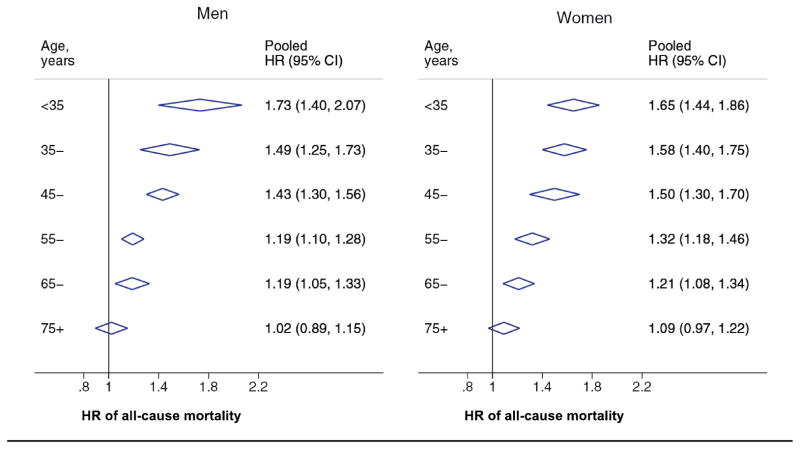
Obesity, defined as excess body weight or fat, is a major risk factor for CV diasease and mortality. 16,17 Body mass index (BMI), an anthropometric measure of obesity, has a U-shaped relationship with all-cause mortality in which BMI values in the normal range (BMI: 20–<25) are associated with minimun death risk whereas incrementally lower or higher BMI values are associated with progressively higher death risk among the general population. 18,19 However, BMI–mortality association reportedly changes with increasing age. In a large cohort study of 129,904 Austrians, the BMI associated with minimun mortality increased with aging from values within normal range at the age of 20 to values within overweight range (BMI: 25–<30) at the age of 54 and 59, respectively, for the male and female participants. 4 In addition, a meta-analysis of 20 prospective cohort studies (total n: 4,664,198) revealed that the associated of obesity (defined as BMI≥30) with all-cause mortality weakened with increasing age and it became non-significant after the age of 75 (Figure 1). 20
Figure 1.
The association of obesity (BMI≥30) with mortality association weakens with increasing age and it becomes non-significant after the age of 75. HR: Hazard Ratio. From a meta-analysis of 20 cohort studies (total n: 4,664,198) by Wang et al 20, with permission.*
* Pending obtaining permission
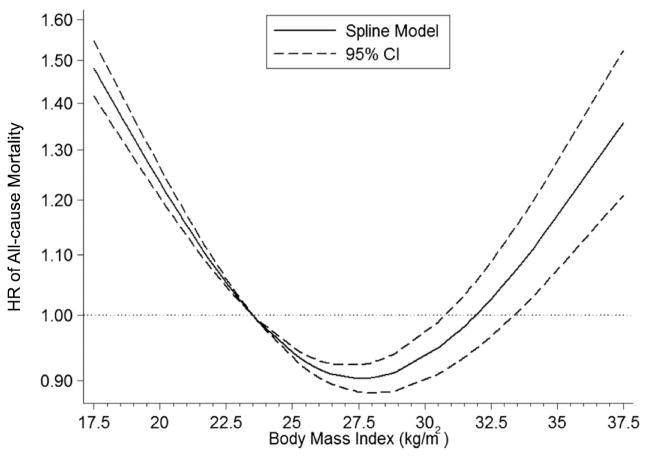
In a seven-year cohort study of 12,725 African-American, and Mexian American, and White participants aged ≥65 years, Al Snih et al 5 showed that compared to normal BMI, being overweight (BMI: 25–<30) or grade I obese (BMI: 30–<35) at baseline was associatied with lower mortality, and in addition, being grade II obese (BMI: 35–<40) or grade III obese (BMI: ≥40) was not associated with any significantly higher risk of death. In addition, the hazard ratio (HR) of death associated with BMI <22 was higher than HR associated with BMI of 40, indicating that being grade grade III obese is still favorable to being low normal or underweight in this population. In another study of 144,054 non-Hispanic White participants of the National Health Interview Survey aged 50–80 years, the lowest risk of all-cause, CV, cancer, and respiratory mortality was associated with BMI values in the high-normal to overweight ranges, and in addition, being low-normal or underweight was associated with markedly increased risk of death particularly due to respiratory disease. However, BMI was directly associated with diabetes mortality. 21 In addition, a long-term investigation of BMI trajectories and mortality in 16,203 males participating in the Oslo Study revealed that the minimum risk of death was associated with an increase of BMI from <25 at midlife to 25–30 at the old age. Also, a decrease of BMI from 25–30 to <25 was associated with increased risk of death. Nevertheless, BMI ≥30 at midlife was associated with increased mortality regardless of the subsequent BMI trajectory. 22 Moreover, a meta-analysis of 32 prospective cohort studies (total n: 197,940) on community-living adults aged ≥65 years reported that BMI of 27–27.9 was associated with minimun death risk and the death risk did not begin to significantly increase again until BMIs >33 kg/m2 (Figure 2). 6 Not only obesity is paradoxically associated with survival advantage in the geriatric population, the benefits of weight reduction have also been questioned. A systematic review of 26 randomized controlle trials (RCTs) on subjects aged ≥60 years with baseline BMI ≥27 favored maintaining weight in older persons who became obese after the age of 65 unless they had ischemic heart disease (IHD), diabetes mellitus type 2, osteoarthritis, or reduced physical function. 23
Figure 2.
In the geriatric population, the optimal BMI associated with minimum risk of death shifts towards overweight/obesity. HR: Hazard Ratio. From a meta-analysis of 32 cohort studies (total n: 197,940) by Winter et al 6, with permission. *
* Pending obtaining permission
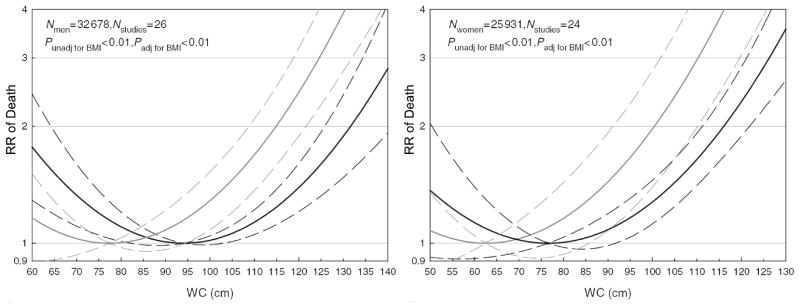
Studies of other anthropometric measures and body composition also suggest that the obesity–mortality association may be altered among the elderly. A study of 1,569 non-institutionalized participants of the National Health and Nutrition Examination Surveys (NHANES) III aged >60 years showed that neither high BMI, waist circumference (WC), waist to his ratio WHR), % body fat, nor lean mass had any significant bearing on all-cause mortality. 24 Also, in a long cohort study of 4,574 community-dwelling women aged ≥75 years, higher-than-normal values of BMI (28.6), WC (88), and hip circumference (106) were associated with the lowest mortality, and in addition, WHR and lean mass index (calculated as leas mass/height2) had no significant link with mortality. Moreover, in a significant inverse relationship, each 10% increase in fat mass was associated with a 12% reduction of mortality risk. 25 Also, a meta-analysis of 29 cohort studies (total n: 58,609) of adults aged 65–74 years showed that the minimum risk of death was associated with WC values close to the high WC threshold in both males and females; however, the optimal WC values were decreased with adjustment for BMI, (Figure 3). 26 Moreover, another prospective cohort of 4,331 men aged 65–93 years showed that >5% loss of body weight, total lean mass, or total fat mass is respectively associated with 78%, 84%, and 72% higher risk of death. 27 In spite of the presented evidence, the U.S. Preventive Services Task Force recommends offering or referring overweight/obese adults with additional CV risk factors to intensive behavioral counseling interventions irrespective of their age. 28
Figure 3.
In the general population, waist circumference (WC) values >102 cm in males or > 88 cm in females are considered “high risk”. In the geriatric population, however, WC values associated with the lowest risk of death are reportedly close to these “high risk” thresholds (black lines). Nevertheless, the optimal WC values are decreased with adjustment for BMI (grey lines). RR: Relative Risk. Solid and dashed lines, respectively, illustrate RR values and their 95% confidence intervals. From a meta-analysis of 29 cohort studies (total n: 58,609) of elderly individuals by de Hollander et al 26, with permission. *
* Pending obtaining permission
SERUM CHOLESTEROLS: IS HYPERCHOLESTEROLEMIA DESIRABLE?
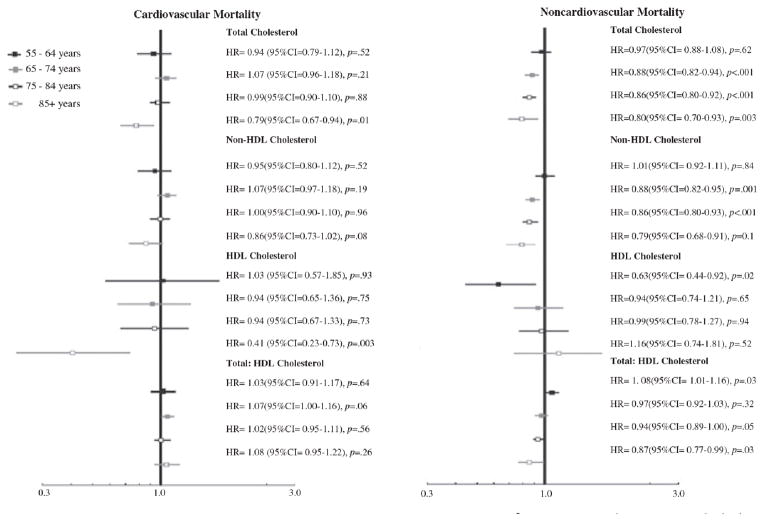
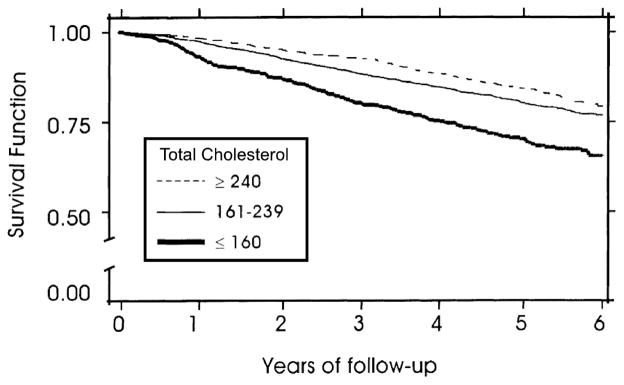
Although hypercholesterolemia is a recognized risk factor for cardiovasculary morbidity and mortality in the general population, 29 the association of cholesterol with clinical outcomes seemingly changes with aging. Newson et al 7 modeled serum cholesterols with both CV and non-CV mortality in consecutive age subgroups of 5,750 Rotterdam Cohort participants aged 55–99 years and observed that higher total cholesterl (TC) was inveresely associated with CV or non-CV mortality after the ages of 85 and 65 years, respectively, beyond which higher TC became incermentally protective. In addition, higher non-high-density lipoprotein cholesterl (non-HDL-C) was not associated with CV mortality and it became incrementally protective against non-CV mortality after the age of 65 years. Also, TC/HDL-C was not associated with CV mortality and it was protective against non-CV mortality after the age of 85 years (Figure 4). Robust epidemiologic studies support the presence of the “cholesterol paradox” in the geriatric population. In a prospective cohort study of 2,556 Medicare recipients aged 65–103 years, higher non-HDL-C was associated with a survival advantage among Whites, and in addition, the lowest quintiles of non-HDL-C, low-density lipoprotein cholesterol (LDL-C), and TC were all associated with higher mortality among African-Americans and Whites.. These lipoprotein determinations had no bearing on mortality among Hispanics and HDL-C and triglycerides were not associated with mortality across any ethnicitiy. 8 Moreover, in a long prospective cohort study of 3,120 Italian adults aged ≥65 years, higher baseline LDL-C was associated with lower all-cause mortality among females, and in addition, LDL-C values close to 150 mg/dl were associated with not only mimimum all-cause mortality among males but also minimum CV mortality among both sexes. 30 Also, a prospective cohort study of 490 home-dwelling elderly persons aged ≥75 years from Finland reported that higher TC was associated with survival advantage even in those with heart disease or current/previous hypertension. In this study, each 1 mmol/l (38.6 mg/dl) increase in TC was linked to 18% lower risk of death. 9 Furthermore, a prospective cohort study of 2,182 adults aged >70 years failed to confirm the role of TC, HDL-C, or TC/HDL-C as significant risk factors for acute coronary syndrome, CV mortality, or all-cause mortality. 31 In another prospective cohort study of 4,066 adults aged ≥65 years, TC or HDL-C were not signficantly associatied with all-cause mortality; however, TC ≥200 or HDL-C <35 were associated with increased risk of death due to coronary heart disease. 32 In the largest prospective cohort study of TC–mortality association examining 4,128 adults aged ≥70 years, having high (TC: ≥240) or normal/borderline (TC: 161–239) values was associated with survival advantage compared to having low (TC: ≤160) values (Figure 5). 10 Also, in a systematic review regarding cholesterol and mortality in 80+ yo people, Pertersen et al 33 synthesized the results of 21 observational studies and four RCTs and concluded that the highest risk of death was associated with the lowest TC and also the lowest risk was mostly associated with either the highest or higher-than-recommended TC values. In this analysis, lipid-lowering treatment was not associated with better survival in patients with CV disease and it was seemingly detrimental in those without CV disease. In the JUPITER trial on 15,548 healthy men and women aged ≥50 and ≥60 years, respectively, rosuvastatin pharmacological intervention was associated with reduced cardiovascular events and death from any cause compared to placebo. 34 Its effect on CV mortality was unclear since CV mortality was a component of “cardiovascular events” as a composite outcome. In addition, its effect on all-cause mortality did not reach statistical significance in a subgroup of 5,695 participants aged ≥70 years 36 In a meta-analysis of eight RCTs (total n: 24,678) on patients aged ≥65 years without established CV disease who received statins compared to placebo, intervention reduced the risk of myocardial infarction and stroke among the study participants but did not result in reduced all-cause or CV death (Supplemental Figure S1), 37 Also, the latest ACC/AHA guideline on the subject did not recommend routine initiation of statins for primary prevention of atherosclerotic cardiovascular disease (ASCVD) among all individuals >75 years of age without clinical ASCVD. 38
Figure 4.
Aging alters the association of total cholesterol (TC), non-high-density lipoprotein (non-HDL) cholesterol, and HDL cholesterol with cardiovascular and non-cardiovascular mortality. Hazard ratios (HR) are calculated per 1 mmol/l (=38.6 mg/dl) increase. From a study of 5,750 Rotterdam Cohort participants by Newson et al 7, with permission. *
* Pending obtaining permission
Figure 5.
Among the elderly, higher total cholesterol is reportedly associated with better survival. From a cohort study of 4,128 adults aged ≥70 years by Volpato et al 10, with permission. *
* Pending obtaining permission.*
* Pending obtaining permission
BLOOD PRESSURE: IS HYPERTENSION ADVANTAGEOUS?
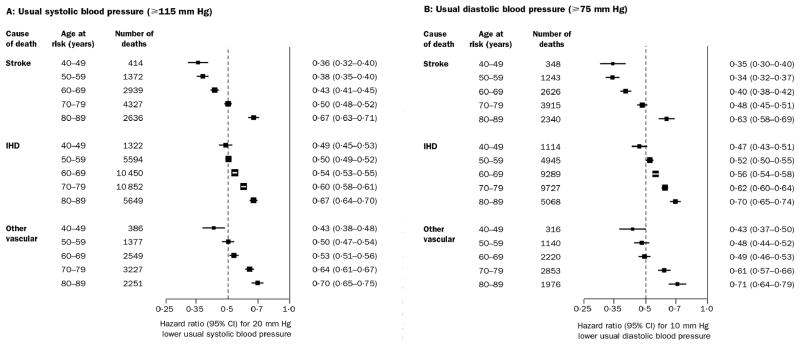
Hypertension (HTN), defined as high systolic blood pressure (SBP), diastolic blood pressure (DBP), or both, is an indisputable risk factor for cardiovascular and cerebrovascular events in the general population. 39 However, the association of HTN with CV mortality is reportedly attenuated with aging, and in addition, some degrees of HTN seemingly becomes protective against all-cause mortality. In a large meta-analysis, Lewington et al 40 synthesized the results of 61 prospective observational studies (total n: 1 million) involving adults with no previous vascular disease and observed that aging was associated with a progressive attenuation in the protective effects of lower SBP or DBP (while remaining above 115 and 75, respectively) against mortality cause by stroke, IHD, or other vascular sequalae (Figure 6). Also, Morkedal et al 41 observed that the association of higher SBP or DBP with IHD mortality is stronger in middle age than in older age in a long prospective cohort study of 71,382 Norwegians aged ≥20 years (Supplemental Figure S2).
Figure 6.
The protective effects of lower systolic or diastolic blood pressure against vascular mortality attenuates with increasing age depicted by hazard ratios getting closer to one (null effect) in consecutive decades. IHD: Ischemic Heart Disease. From a meta-analysis of 61 studies (total n: 1 million) by Lewington et al 40, with permission. *
* Pending obtaining permission
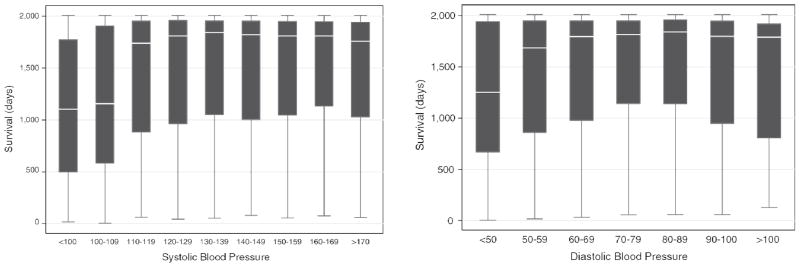
While aging attenuates the BP–CV mortality association, 40,41 its influence on the association between BP and all-cause mortality shows a risk factor reversal. In a cohort study of 4,071 US veterans aged ≥80 years, lowest death rates were associated with BP values within the prehypertensive range (SBP: 120–140; DBP: 80–90), and in addition, higher SBP or DBP within the hypertensive rane were not associated with any increased all-cause mortality (Figure 7). 11 Also, another long cohort study of 1,560 Spanish adults aged ≥65 years reported a U-shaped relationship between SBP (as a time-dependent covariate) and all-cause mortality, with a nadir at the value of 147 mmHg; also, the relationship between DBP (as a time-dependent covariate) and mortality was reverse J-shaped, in which higher DBP had survival advantage below the value of 80 mmHg and it had no bearing on mortality over that value. 12 Not only some degrees of HTN are suggested to have survival advantage or at least no survival disadvantage, the benefits of tight blood pressure control have also been suspected in advanced age. The pooled results of a meta-analysis of eight RCTs (total n: 6,701) involving hypertensive patients aged ≥80 years showed that antihypertensive treatment did not yield any significantly reduced all-cause, CV, coronary, or stroke death compared to either placebo or no treatment (Supplemental Figure S3); in addition, the few trials showing reduced mortality were the ones with the lowest intensity of therapy and the least BP reductions. 42 Also, in a similar meta-analysis of 10 RCTs (total n: 8,667) recruiting hypertensive patients aged ≥75 years, antihypertensive medications did not yield any significantly reduced all-cause mortality. 43 However, both meta-analyses showed that treatment decreased CV events, stroke, and heart failure. 42,43 Although evidence supporting the hypertension paradox is not as vigorous as the support around obesity or cholesterol paradoxes, the latest Evidence-Based Guideline for the Management of High Blood Pressure in Adults recommended a 10-point higher SBP (150 mmHg instead of the traditional 140) as the goal of treatment among adults aged ≥60 years; in addition, the guideline did not make any recommendation for a BP goal among people aged ≥70 years with moderately to severely reduced kidney function (GFR <60 mL/min/1.73 m2). 44
Figure 7.
Higher systolic or diastolic blood pressure (SBP or DBP) is associated with better survival within non-hypertensive range (SBP <140 or DBP <90, respectively) and it is not associated with any significantly different mortality within hypertensive range (SBP ≥140 or DBP ≥90). The box plots illustrate median, interquartile range, and total range of survival for each SBP or DBP class. From a cohort study of 4,071 individuals aged ≥80 years by Oates et al 11, with permission. *
* Pending obtaining permission
PATHOPHYSIOLOGY OF REVERSE EPIDEMIOLOGY
Several possible hypothesis have been suggested to explain reverse epidemiology in the geriatric population as well as in other chronic states such as chronic kidney disease or chronic heart failure:
Competing short-term and long-term killers
Patients with chronic disease states may not live long enough to die from overnutrition sequelea as they are more likely to die earlier from undernutrition ramifications. In fact, short-term death risk is excessively high in these chronic states, and therefore, such individuals would not live long enough to die from the consequeces of obesity or hypercholesterolemia evolved through years. Thus, excess weight or fat may protect against death due to undernutrition over short term outweighing the associated CV sequelae and death over long term. 45,46 This hypothesis can explain why strict treatment goals for such traditional risk factors may be irrelevant in the elderly and in other populations with risk factor paradoxes.
Improved hemodynamic stability
Higher systemic blood pressure associated with overweight, obesity and hypercholestrolemia is hypothetically protective against cardiovascular instability in individuals with chronic states. In fact, obese patients may better tolerate CV or other adverse events that would otherwise occur frequently in the setting of wasting disease associated with chronic disease states. 13,47
Adipokine protection against TNF-α
As tumor necrosis factor-α(TNF-α) is a proinflammatory cytokine damaging tissues and inducing other inflammatory cytokines and adhesion molecules, it can eventually cause deterioration of wasting disease and incerase the risk of death in those with chronic disease states. 48,49 Adipose tissue generates adiponectins and soluble TNF-α receptors that can potentially neutralize the adverse biologic effects of TNF-α. 50,51. From this perspective, more adipose tissue associated with obesity and hyperlipidemia can be beneficial in such chronic conditions.
Lipoprotein protection against endotoxins
Exposure to endotoxin, a component of gram-negative bacterial cell walls, is widespread in many industrial and ambient environments and it is associated with chronic non-resolving inflammation. 52,53 Lipoproteins can actively bind to and neutralize circulaing endotoxins protecting against their adverse ramifications if remained unbound. 51,54 Therefore, a higher pool of lipoproteins associated with obesity or hypercholesterolemia can exert a survival advantage in individuals with chronic conditions.
Lipophilic toxin sequestration by adipose tissue
Weight loss and reduced adipose tissue reserve is associated with imminent release of, and signficant increase in, circulating lipophilic toxins such as hexachlorobenzene and other chlorinated hydrocarbons. 55 As many chronic disease states are associated with higher cataboic rates leading to the excessive release of lipophilic toxins, abundant adipose tissue can more effectively sequester the released toxins. 56
Reverse causation
It is possible that lower cardiovascular risk factors (such as BMI, cholesterol, or BP) are not a cause but a consequence of underlying conditions that cuncurrently lead to poor outcomes in the populations with risk factor paradoxes. This so-called “reverse causation” is a possible source of bias in epidemiologic studies that examine associations with unclear direction of the causal pathway. 57 However, reverse causation alone cannot explain the observed survival advantage of obesity, including morbid obesity, in populations with risk factor paradoxes including those with chronic heart failure or with end-stage renal disease receiving hemodialysis. 13,15,46
Survival selection
Octogenarians (i.e. aged 80–89 years) or nonagenarians (i.e. aged 90–99 years) are no more than 5% of the US population. People with advance age are substantially selected by survival and it makes them significantly different from the general population. In fact, such individuals with distinct survival advantages to reach an advanced age may be genetically protectied against the ramifications of CV diseaes or other fatal conditions. 13,15,46 Similarly, chronic heart failure or dialysis patients represent highly-selected survivors of the larger pool of patients with cardiovascular or chronc kindey diseases, respectively. This hypothesis, however, cannot explain the survival paradoxes in chronic conditions with relatively long survival such as rheumatoic arthritis. Also, it cannot explain why reserve epidemiology is reverted back to normal risk factor–mortality associations following successful heart or kidney transplantation. 58,59
CLINICAL IMPLICATIONS
Risk factor paradoxes have contributed to a growing confusion regarding whether to treat obesity, hypercholesterolemia, or hypertension among the geriatric population as well as in other chronic disease states, collectively representing more than 30 million Americans. 13 The concept of reverse epidemiology challenges traditional paradigms and remains controversial. However, dismissing this concept as counterintuitive and harmful is not the appropriately scientific approach to dealing with this emerging conundrum. If complex set of conditions related to malnutrition and inflammation (namely wasting disease) represents the etiology of this risk factor reversal and high death rate, and if the short-term death risk due to wasting outweighs the long-term sequelae of over-nutrition, then the key to improving survival in 30 million Americans with a reverse epidemiology may be interventions addressing wasting disease. If weight loss over time is associated with poor outcomes and if weight gain yields improved survival, then the most promising management strategies in these populations may be nutritional and anti-inflammatory interventions, rather than weight reduction and lipid lowering interventions.
In conclusion, tight control of weight, serum cholesterols, and blood pressure to achieve targets derived from the epidemiologic studies of younger populations may not be appropriate for the geriatric population. Nevertheless, premature conclusions to lower doses or discontinue weight reduction, anti-hyperlipidemic, or antihypertensive strategies and treatments should be avoided until being tested and approved by strong evidence provided by RCTs. We recommend that decisions about the choice and intensity of CV risk factor modification strategies for older persons be carefully considered on an individualized basis with special attention to the unique characteristics and medical conditions of each individual.
Supplementary Material
Figure S1: Statins have no significant effect on all-cause or cardiovascular mortality in the elderly population. From a meta-analysis of eight randomized controlled trials (total n: 71,382) by Savarese et al 37, with permission. *
*Pending obtaining permisson
Figure S2: The ischemic heart disease (IHD) mortality associated with systolic or diastolic hypertension is attenuated among the elderly population. RR: Relative risk; SBP: Systolic blood pressure; DBP: Diastolic blood pressure. Diagrams created based on the results of a cohort study of 71,382 Norwegians by Mordedal et al 41.
Figure S3: Anti-hypertensive medications have no significant effect on all-cause or cause-specific mortality in hypertensive patients aged ≥80 years; however, they reduce cardiovascular events, stroke, and heart failure. From a meta-analysis of eight randomized controlled trials (total n: 6,701) by Bejan-Angoulvant et al 42, with permission. *
*Pending obtaining permisson
Table 1.
Reverse Epidemiology of Cardiovascular Risk Factors in Geriatric Population.
| Risk Factors of Cardiovascular Disease | Direction of the Association Between Risk Factors and Outcomes
|
Comments | |
|---|---|---|---|
| General Population | Geartric Popultion | ||
| Obesity | Obesity (High BMI, waist circumference, or % body fat) is deleterious. 18,19 | Some degrees of obesity seems protective.5,6,23,25 | Patients with CKD, CHF, COPD, rheumatoic arthritis, AIDS and malignancies have obesity paradoxes similar to the geriatric population.13,15,45,46,56 |
| Hypercholesterolemia | Hypercholesterolemia (high total cholesterol or non-HDL cholesterol) is deleterious.29 | Hypercholesterolemia seems protective.7–10,33 | Similar lipid paradoxes are reported in patients with CKD, CHF, COPD and rheumatoic arthritis.13,45,46 |
| Hypertension | Hypertension (high systolic or diastolic blood pressure) is deleterious.39 | Low blood pressure is deleterious but hypertension is not.11,12 | Blood pressure paradoxes is also reported in patients with CKD and CHF. 45,46 |
BMI: Body mass index; CKD: Chronic kidney disease; CHF: chronic heart failure; COPD: chronic obstructive pulmonary disease; AIDS: Acquired immune deficiency syndrome; non-HDL cholesterol: Non-high density lipoprotein cholesterol.
Acknowledgments
Funding: This work was supported by KKZ’s research grants from the NIH/NIDDK (K24-DK091419 and R01-DK078106) and philanthropic grants from Harold Simmons, Joseph Lee, Louis Chang, and AVEO.
Footnotes
Potential Conflicts of Interest: KKZ has received honoraria from Abbott, Abbvie, Alexion, Amgen, ASN, Astra-Zeneca, Aveo, Chugai, DaVita, Fresenius, Genetech, Haymarket Media, Hospira, Kabi, Keryx, NIH, NKF, Relypsa, Resverlogix, Sanofi, Shire, Vifor, ZS-Pharma, and other manufacturers of phosphorus binders, nutritional supplements, or medications and items related to dialysis patients.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.U.S. Administration on Aging. [accessed 04/27/2015];US Population Totals by Age Group and Sex in the 2010 and 2000 Censuses. http://www.aoa.acl.gov/Aging_Statistics/Census_Population/census2010/Index.aspx.
- 2.U.S. Administration on Aging. [accessed 04/27/2015];Projected Future Growth of the Older Population: 1900 to 2050. http://www.aoa.acl.gov/Aging_Statistics/future_growth/future_growth.aspx-aging.
- 3.Arnold AM, Psaty BM, Kuller LH, Burke GL, Manolio TA, Fried LP, et al. Incidence of cardiovascular disease in older Americans: the cardiovascular health study. J Am Geriatr Soc. 2005;53(2):211–8. doi: 10.1111/j.1532-5415.2005.53105.x. [DOI] [PubMed] [Google Scholar]
- 4.Peter RS, Mayer B, Concin H, Nagel G. The effect of age on the shape of the BMI-mortality relation and BMI associated with minimum all-cause mortality in a large Austrian cohort. Int J Obes (Lond) 2015;39(3):530–4. doi: 10.1038/ijo.2014.168. [DOI] [PubMed] [Google Scholar]
- 5.Al Snih S, Ottenbacher KJ, Markides KS, Kuo Y-F, Eschbach K, Goodwin JS. The effect of obesity on disability vs mortality in older Americans. Arch Intern Med. 2007;167(8):774–80. doi: 10.1001/archinte.167.8.774. [DOI] [PubMed] [Google Scholar]
- 6.Winter JE, MacInnis RJ, Wattanapenpaiboon N, Nowson CA. BMI and all-cause mortality in older adults: a meta-analysis. Am J Clin Nutr. 2014;99(4):875–90. doi: 10.3945/ajcn.113.068122. [DOI] [PubMed] [Google Scholar]
- 7.Newson RS, Felix JF, Heeringa J, Hofman A, Witteman JCM, Tiemeier H. Association between serum cholesterol and noncardiovascular mortality in older age. J Am Geriatr Soc. 2011;59(10):1779–85. doi: 10.1111/j.1532-5415.2011.03593.x. [DOI] [PubMed] [Google Scholar]
- 8.Akerblom JL, Costa R, Luchsinger JA, Manly JJ, Tang M-X, Lee JH, et al. Relation of plasma lipids to all-cause mortality in Caucasian, African-American and Hispanic elders. Age Ageing. 2008;37(2):207–13. doi: 10.1093/ageing/afn017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tuikkala P, Hartikainen S, Korhonen MJ, Lavikainen P, Kettunen R, Sulkava R, et al. Serum total cholesterol levels and all-cause mortality in a home-dwelling elderly population: a six-year follow-up. Scand J Prim Health Care. 2010;28(2):121–7. doi: 10.3109/02813432.2010.487371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Volpato S, Leveille SG, Corti MC, Harris TB, Guralnik JM. The value of serum albumin and high-density lipoprotein cholesterol in defining mortality risk in older persons with low serum cholesterol. J Am Geriatr Soc. 2001;49(9):1142–7. doi: 10.1046/j.1532-5415.2001.49229.x. [DOI] [PubMed] [Google Scholar]
- 11.Oates DJ, Berlowitz DR, Glickman ME, Silliman RA, Borzecki AM. Blood pressure and survival in the oldest old. J Am Geriatr Soc. 2007;55(3):383–8. doi: 10.1111/j.1532-5415.2007.01069.x. [DOI] [PubMed] [Google Scholar]
- 12.Gutiérrez-Misis A, Sánchez-Santos MT, Banegas JR, Zunzunegui MV, Sánchez-Martinez M, Castell MV, et al. Association between blood pressure and mortality in a Spanish cohort of persons aged 65 years or over: a dynamic model. Rev Esp Cardiol (Engl Ed) 2013;66(6):464–71. doi: 10.1016/j.rec.2012.11.014. [DOI] [PubMed] [Google Scholar]
- 13.Kalantar-Zadeh K, Horwich TB, Oreopoulos A, Kovesdy CP, Younessi H, Anker SD, et al. Risk factor paradox in wasting diseases. Curr Opin Clin Nutr Metab Care. 2007;10(4):433–42. doi: 10.1097/MCO.0b013e3281a30594. [DOI] [PubMed] [Google Scholar]
- 14.Kalantar-Zadeh K, Rhee CM, Amin AN. To legitimize the contentious obesity paradox. Mayo Clin Proc. 2014;89(8):1033–5. doi: 10.1016/j.mayocp.2014.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Park J, Ahmadi S-F, Streja E, Molnar MZ, Flegal KM, Gillen D, et al. Obesity paradox in end-stage kidney disease patients. Prog Cardiovasc Dis. 2014;56(4):415–25. doi: 10.1016/j.pcad.2013.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Manson JE, Willett WC, Stampfer MJ, Colditz GA, Hunter DJ, Hankinson SE, et al. Body weight and mortality among women. N Engl J Med. 1995;333(11):677–85. doi: 10.1056/NEJM199509143331101. [DOI] [PubMed] [Google Scholar]
- 17.Calle EE, Thun MJ, Petrelli JM, Rodriguez C, Heath CW. Body-mass index and mortality in a prospective cohort of U.S. adults. N Engl J Med. 1999;341(15):1097–105. doi: 10.1056/NEJM199910073411501. [DOI] [PubMed] [Google Scholar]
- 18.Berrington de Gonzalez A, Hartge P, Cerhan JR, Flint AJ, Hannan L, MacInnis RJ, et al. Body-mass index and mortality among 1. 46 million white adults. N Engl J Med. 2010;363(23):2211–9. doi: 10.1056/NEJMoa1000367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Prospective Studies C. Whitlock G, Lewington S, Sherliker P, Clarke R, Emberson J, et al. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009;373(9669):1083–96. doi: 10.1016/S0140-6736(09)60318-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang Z. Age-dependent decline of association between obesity and mortality: a systematic review and meta-analysis. Obes Res Clin Pract. 2015;9(1):1–11. doi: 10.1016/j.orcp.2014.01.006. [DOI] [PubMed] [Google Scholar]
- 21.Zajacova A, Burgard SA. Shape of the BMI-mortality association by cause of death, using generalized additive models: NHIS 1986–2006. J Aging Health. 2012;24(2):191–211. doi: 10.1177/0898264311406268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Holme I, Tonstad S. Survival in elderly men in relation to midlife and current BMI. Age Ageing. 2015;44(3):434–9. doi: 10.1093/ageing/afu202. [DOI] [PubMed] [Google Scholar]
- 23.Bales CW, Buhr G. Is obesity bad for older persons? A systematic review of the pros and cons of weight reduction in later life. J Am Med Dir Assoc. 2008;9(5):302–12. doi: 10.1016/j.jamda.2008.01.006. [DOI] [PubMed] [Google Scholar]
- 24.Batsis JA, Singh S, Lopez-Jimenez F. Anthropometric measurements and survival in older americans: results from the third national health and nutrition examination survey. J Nutr Health Aging. 2014;18(2):123–30. doi: 10.1007/s12603-013-0366-3. [DOI] [PubMed] [Google Scholar]
- 25.Rolland Y, Gallini A, Cristini C, Schott A-M, Blain H, Beauchet O, et al. Body-composition predictors of mortality in women aged ≥ 75 y: data from a large population-based cohort study with a 17-y follow-up. Am J Clin Nutr. 2014;100(5):1352–60. doi: 10.3945/ajcn.114.086728. [DOI] [PubMed] [Google Scholar]
- 26.de Hollander EL, Bemelmans WJ, Boshuizen HC, Friedrich N, Wallaschofski H, Guallar-Castillón P, et al. The association between waist circumference and risk of mortality considering body mass index in 65- to 74-year-olds: a meta-analysis of 29 cohorts involving more than 58 000 elderly persons. Int J Epidemiol. 2012;41(3):805–17. doi: 10.1093/ije/dys008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lee CG, Boyko EJ, Nielson CM, Stefanick ML, Bauer DC, Hoffman AR, et al. Mortality risk in older men associated with changes in weight, lean mass, and fat mass. J Am Geriatr Soc. 2011;59(2):233–40. doi: 10.1111/j.1532-5415.2010.03245.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.LeFevre ML Force USPST. Behavioral counseling to promote a healthful diet and physical activity for cardiovascular disease prevention in adults with cardiovascular risk factors: U.S Preventive Services Task Force Recommendation Statement. Ann Intern Med. 2014;161(8):587–93. doi: 10.7326/M14-1796. [DOI] [PubMed] [Google Scholar]
- 29.Klag MJ, Ford DE, Mead LA, He J, Whelton PK, Liang KY, et al. Serum cholesterol in young men and subsequent cardiovascular disease. N Engl J Med. 1993;328(5):313–8. doi: 10.1056/NEJM199302043280504. [DOI] [PubMed] [Google Scholar]
- 30.Tikhonoff V, Casiglia E, Mazza A, Scarpa R, Thijs L, Pessina AC, et al. Low-density lipoprotein cholesterol and mortality in older people. J Am Geriatr Soc. 2005;53(12):2159–64. doi: 10.1111/j.1532-5415.2005.00492.x. [DOI] [PubMed] [Google Scholar]
- 31.Krumholz HM, Seeman TE, Merrill SS, Mendes de Leon CF, Vaccarino V, Silverman DI, et al. Lack of association between cholesterol and coronary heart disease mortality and morbidity and all-cause mortality in persons older than 70 years. Jama. 1994;272(17):1335–40. [PubMed] [Google Scholar]
- 32.Corti MC, Guralnik JM, Salive ME, Harris T, Ferrucci L, Glynn RJ, et al. Clarifying the direct relation between total cholesterol levels and death from coronary heart disease in older persons. Ann Intern Med. 1997;126(10):753–60. doi: 10.7326/0003-4819-126-10-199705150-00001. [DOI] [PubMed] [Google Scholar]
- 33.Petersen LK, Christensen K, Kragstrup J. Lipid-lowering treatment to the end? A review of observational studies and RCTs on cholesterol and mortality in 80+-year olds. Age Ageing. 2010;39(6):674–80. doi: 10.1093/ageing/afq129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ridker PM, Danielson E, Fonseca FA, Genest J, Gotto AM, Kastelein JJ, et al. Reduction in C-reactive protein and LDL cholesterol and cardiovascular event rates after initiation of rosuvastatin: a prospective study of the JUPITER trial. Lancet. 2009;373(9670):1175–82. doi: 10.1016/S0140-6736(09)60447-5. [DOI] [PubMed] [Google Scholar]
- 35.Ridker PM, Pradhan A, MacFadyen JG, Libby P, Glynn RJ. Cardiovascular benefits and diabetes risks of statin therapy in primary prevention: an analysis from the JUPITER trial. Lancet. 2012;380(9841):565–71. doi: 10.1016/S0140-6736(12)61190-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Glynn RJ, Koenig W, Nordestgaard BG, Shepherd J, Ridker PM. Rosuvastatin for primary prevention in older persons with elevated C-reactive protein and low to average low-density lipoprotein cholesterol levels: exploratory analysis of a randomized trial. Annals of internal medicine. 2010;152(8):488–96. W174. doi: 10.1059/0003-4819-152-8-201004200-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Savarese G, Gotto AM, Paolillo S, D'Amore C, Losco T, Musella F, et al. Benefits of statins in elderly subjects without established cardiovascular disease: a meta-analysis. J Am Coll Cardiol. 2013;62(22):2090–9. doi: 10.1016/j.jacc.2013.07.069. [DOI] [PubMed] [Google Scholar]
- 38.Stone NJ, Robinson J, Lichtenstein AH, Merz CN, Blum CB, Eckel RH, et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. Circulation. 2013;129(Sup 2):S1–72. doi: 10.1161/01.cir.0000437738.63853.7a. [DOI] [PubMed] [Google Scholar]
- 39.Vasan RS, Larson MG, Leip EP, Evans JC, O'Donnell CJ, Kannel WB, et al. Impact of high-normal blood pressure on the risk of cardiovascular disease. N Engl J Med. 2001;345(18):1291–7. doi: 10.1056/NEJMoa003417. [DOI] [PubMed] [Google Scholar]
- 40.Lewington S, Clarke R, Qizilbash N, Peto R, Collins R Prospective Studies C. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360(9349):1903–13. doi: 10.1016/s0140-6736(02)11911-8. [DOI] [PubMed] [Google Scholar]
- 41.Mørkedal B, Romundstad PR, Vatten LJ. Mortality from ischaemic heart disease: age-specific effects of blood pressure stratified by body-mass index: the HUNT cohort study in Norway. J Epidemiol Community Health. 2011;65(9):814–9. doi: 10.1136/jech.2009.094110. [DOI] [PubMed] [Google Scholar]
- 42.Bejan-Angoulvant T, Saadatian-Elahi M, Wright JM, Schron EB, Lindholm LH, Fagard R, et al. Treatment of hypertension in patients 80 years and older: the lower the better? A meta-analysis of randomized controlled trials. J Hypertens. 2010;28(7):1366–72. doi: 10.1097/HJH.0b013e328339f9c5. [DOI] [PubMed] [Google Scholar]
- 43.Schall P, Wehling M. Treatment of arterial hypertension in the very elderly: a meta-analysis of clinical trials. Arzneimittelforschung. 2011;61(4):221–8. doi: 10.1055/s-0031-1296191. [DOI] [PubMed] [Google Scholar]
- 44.James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8) JAMA. 2014;311(5):507–20. doi: 10.1001/jama.2013.284427. [DOI] [PubMed] [Google Scholar]
- 45.Kalantar-Zadeh K, Block G, Humphreys MH, Kopple JD. Reverse epidemiology of cardiovascular risk factors in maintenance dialysis patients. Kidney Int. 2003;63(3):793–808. doi: 10.1046/j.1523-1755.2003.00803.x. [DOI] [PubMed] [Google Scholar]
- 46.Kalantar-Zadeh K, Block G, Horwich T, Fonarow GC. Reverse epidemiology of conventional cardiovascular risk factors in patients with chronic heart failure. J Am Coll Cardiol. 2004;43(8):1439–44. doi: 10.1016/j.jacc.2003.11.039. [DOI] [PubMed] [Google Scholar]
- 47.Horwich TB, Fonarow GC, Hamilton MA, MacLellan WR, Woo MA, Tillisch JH. The relationship between obesity and mortality in patients with heart failure. J Am Coll Cardiol. 2001;38(3):789–95. doi: 10.1016/s0735-1097(01)01448-6. [DOI] [PubMed] [Google Scholar]
- 48.Kuwano K, Hara N. Signal transduction pathways of apoptosis and inflammation induced by the tumor necrosis factor receptor family. Am J Respir Cell Mol Biol. 2000;22(2):147–9. doi: 10.1165/ajrcmb.22.2.f178. [DOI] [PubMed] [Google Scholar]
- 49.Strieter RM, Kunkel SL, Bone RC. Role of tumor necrosis factor-alpha in disease states and inflammation. Crit Care Med. 1993;21(10 Suppl):S447–63. doi: 10.1097/00003246-199310001-00006. [DOI] [PubMed] [Google Scholar]
- 50.Stenvinkel P, Marchlewska A, Pecoits-Filho R, Heimbürger O, Zhang Z, Hoff C, et al. Adiponectin in renal disease: relationship to phenotype and genetic variation in the gene encoding adiponectin. Kidney Int. 2004;65(1):274–81. doi: 10.1111/j.1523-1755.2004.00370.x. [DOI] [PubMed] [Google Scholar]
- 51.Mohamed-Ali V, Goodrick S, Bulmer K, Holly JM, Yudkin JS, Coppack SW. Production of soluble tumor necrosis factor receptors by human subcutaneous adipose tissue in vivo. Am J Physiol. 1999;277(6 Pt 1):E971–5. doi: 10.1152/ajpendo.1999.277.6.E971. [DOI] [PubMed] [Google Scholar]
- 52.Lundin JI, Checkoway H. Endotoxin and cancer. Environ Health Perspect. 2009;117(9):1344–50. doi: 10.1289/ehp.0800439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Morris MC, Gilliam EA, Li L. Innate immune programing by endotoxin and its pathological consequences. Front Immunol. 2014;5:680. doi: 10.3389/fimmu.2014.00680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Rauchhaus M, Coats AJ, Anker SD. The endotoxin-lipoprotein hypothesis. Lancet. 2000;356(9233):930–3. doi: 10.1016/S0140-6736(00)02690-8. [DOI] [PubMed] [Google Scholar]
- 55.Jandacek RJ, Anderson N, Liu M, Zheng S, Yang Q, Tso P. Effects of yo-yo diet, caloric restriction, and olestra on tissue distribution of hexachlorobenzene. Am J Physiol Gastrointest Liver Physiol. 2005;288(2):G292–9. doi: 10.1152/ajpgi.00285.2004. [DOI] [PubMed] [Google Scholar]
- 56.Kalantar-Zadeh K, Kopple JD. Obesity paradox in patients on maintenance dialysis. Contrib Nephrol. 2006;151:57–69. doi: 10.1159/000095319. [DOI] [PubMed] [Google Scholar]
- 57.Macleod J, Davey Smith G. Psychosocial factors and public health: a suitable case for treatment? J Epidemiol Community Health. 2003;57(8):565–70. doi: 10.1136/jech.57.8.565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kalantar-Zadeh K, Abbott KC, Kronenberg F, Anker SD, Horwich TB, Fonarow GC. Epidemiology of dialysis patients and heart failure patients. Semin Nephrol. 2006;26(2):118–33. doi: 10.1016/j.semnephrol.2005.09.005. [DOI] [PubMed] [Google Scholar]
- 59.Ahmadi S-F, Zahmatkesh G, Streja E, Molnar MZ, Rhee CM, Kovesdy CP, et al. Body mass index and mortality in kidney transplant recipients: a systematic review and meta-analysis. Am J Nephrol. 2014;40(4):315–24. doi: 10.1159/000367812. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1: Statins have no significant effect on all-cause or cardiovascular mortality in the elderly population. From a meta-analysis of eight randomized controlled trials (total n: 71,382) by Savarese et al 37, with permission. *
*Pending obtaining permisson
Figure S2: The ischemic heart disease (IHD) mortality associated with systolic or diastolic hypertension is attenuated among the elderly population. RR: Relative risk; SBP: Systolic blood pressure; DBP: Diastolic blood pressure. Diagrams created based on the results of a cohort study of 71,382 Norwegians by Mordedal et al 41.
Figure S3: Anti-hypertensive medications have no significant effect on all-cause or cause-specific mortality in hypertensive patients aged ≥80 years; however, they reduce cardiovascular events, stroke, and heart failure. From a meta-analysis of eight randomized controlled trials (total n: 6,701) by Bejan-Angoulvant et al 42, with permission. *
*Pending obtaining permisson