Abstract
The glymphatic system is a recently discovered macroscopic waste clearance system that utilizes a unique system of perivascular channels, formed by astroglial cells, to promote efficient elimination of soluble proteins and metabolites from the central nervous system. Besides waste elimination, the glymphatic system may also function to help distribute non-waste compounds, such as glucose, lipids, amino acids, and neurotransmitters related to volume transmission, in the brain. Intriguingly, the glymphatic system function mainly during sleep and is largely disengaged during wakefulness. The biological need for sleep across all species may therefore reflect that the brain must enter a state of activity that enables elimination of potentially neurotoxic waste products, including β-amyloid. Since the concept of the glymphatic system is relatively new, we will here review its basic structural elements, organization, regulation, and functions. We will also discuss recent studies indicating that glymphatic function is suppressed in various diseases and that failure of glymphatic function in turn might contribute to pathology in neurodegenerative disorders, traumatic brain injury and stroke.
Keywords: The glymphatic system, Astrocytes, Perivascular spaces, Virchow-Robin space, Cerebrospinal fluid secretion, Sleep, Aging, Neurodegenerative diseases, Traumatic brain injury
Introduction
Clearance of excess fluid and interstitial solutes is critical for tissue homeostasis. In the peripheral tissues soluble material, proteins and fluid from the interstitial space are returned to the general circulation by the lymphatic system [1]. The lymphatic network extends throughout all parts of the peripheral tissues and the density of lymph vessels correlates with the rate of tissue metabolism. Although the brain and spinal cord are characterized by a disproportionally high metabolic rate [2], and synaptic transmission is exquisitely sensitive to changes in their environment, the central nervous system (CNS) completely lacks conventional lymphatic vessels. This review addresses recent findings that shed light on this paradox and discusses these findings within the broader context of what is known about waste elimination from the CNS. Finally, we discuss our recent findings indicating that this system might also serve to distribute non-waste compounds such as lipids and glucose within the brain.
CSF production
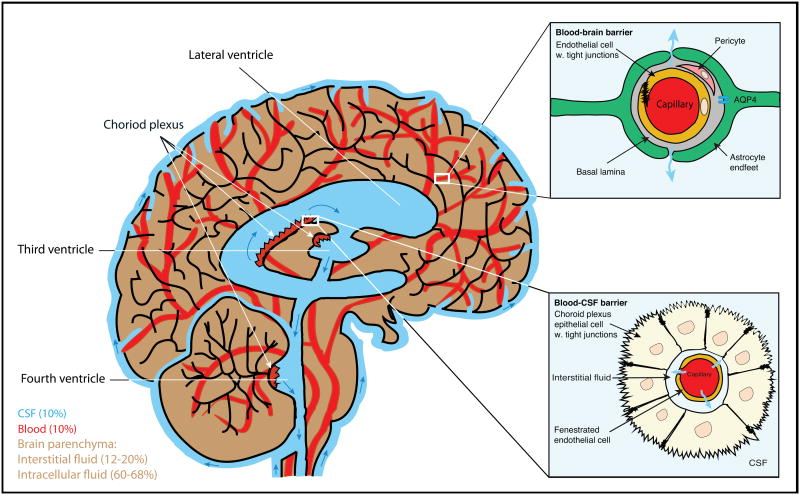
The brain consists of four fluid compartments: cerebrospinal fluid (CSF), interstitial fluid, intracellular fluid, and the blood vasculature (Fig. 1). The blood is kept separate from the brain parenchyma and CSF by the blood-brain and blood-CSF barriers, respectively. These barriers are essential in maintaining the extracellular environment of the brain because they regulate the ionic and biochemical composition of the different fluid compartments [3]. The blood-brain barrier is comprised by blood vessel endothelial cells, where as the blood-CSF barrier is formed primarily between the choroid plexus epithelial cells [4]. Because the plexus capillary endothelial cells, unlike other capillaries in the brain, are devoid of tight junctions, they are more permeable to macromolecules [3]. Choroid plexus epithelial cells, in turn, are connected by tight junctions. At the choroid plexus, the trans-epithelial transport of macromolecules regulated by epithelial transporters therefore determines which macromolecules that enter CSF from the blood (Fig. 1 and 2).
Fig. 1. Schematic representation of the brain's fluid compartments and barriers.
The fluid compartments in the brain consist of intracellular fluid (ICF) (60-68%), interstitial fluid (ISF) (or extracellular fluid) (12-20%), blood (10%) and the cerebrospinal fluid (CSF) (10%) [5, 10]. The blood is separated from the CSF and interstitial fluid by the blood brain barrier (BBB) and blood-CSF barrier, respectively. Tight junctions between the blood endothelial cells constitute the BBB, restricting macromolecules to move freely from the blood to the brain parenchyma. Fluid and solutes in the perivascular space located between endothelial cells and astrocytic endfeet, expressing the water channel aquaporin-4 (AQP4) diffuses into the brain parenchyma. The blood-CSF barrier is formed by tight junctions between the choroid plexus epithelial cells. Macromolecules from the blood can move freely between the fenestrated endothelial cells to the interstitial fluid but is restricted by tight junctions in the choroid plexus epithelial cells, which therefore are believed to be the main players in determining CSF composition.
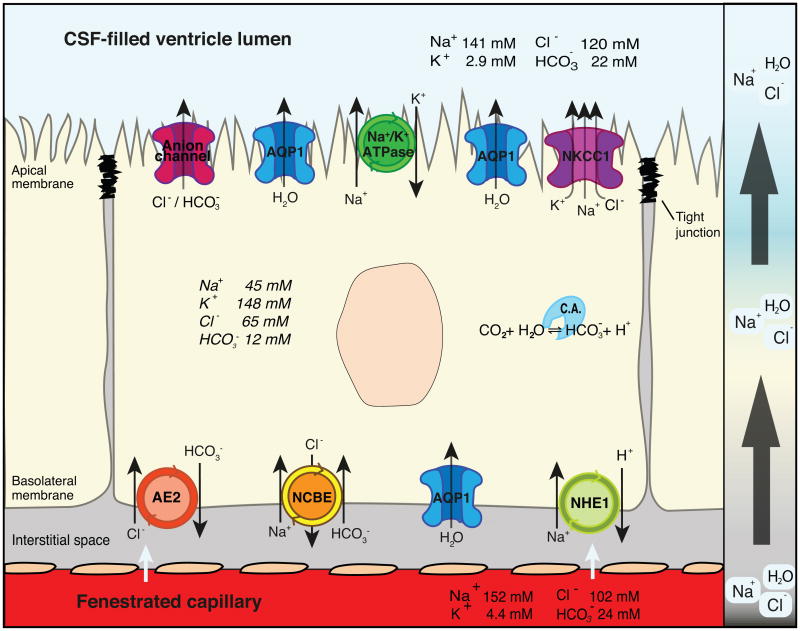
Fig. 2. Ion composition and transport across the choroid plexus epithelial cells.
According to the classical hypothesis, ion transporters and channels in the choroid plexus epithelial cells account for the main part of cerebrospinal fluid (CSF) production. The apically expressed Na+/K+-ATPase, central to CSF secretion, creates the electrochemical gradient for Na+ that is imported via the Na+/H+ exchanger, NHE1 and/or the Na+-HCO3- co-transporter, NCBE in the basolateral membrane. Co-import of HCO3- via NCBE and hydration of CO2 by carbonic anhydrase (C.A) increase the intracellular concentration of HCO3-, which creates an electrochemical gradient that drives the efflux of HCO3- via the basolateral-located Cl-/HCO3- exchanger, AE2 and apical HCO3- channels. The operation of AE2 generates a rise in intracellular Cl- driving the apical export of Cl- through the NKCC1 and Cl- channels. The final result of these processes at the choroid plexus epithelium is a net flux of Na+, HCO3- and Cl- from the blood across the epithelium to the ventricles, which generates the osmotic gradient that makes water move through AQP1 thereby producing the CSF.
In mammals, CSF comprises 10% of the total fluid volume within the cranial cavity [5]. The CSF flows through the four ventricles that are linked by channels or foramina into the subarachnoid space of the cortex and spinal cord (Fig. 1). From the cortical subarachnoid space it penetrates the brain parenchyma perivascularly and bathes the brain before it exits the CNS and drains into the lymphatic system.
CSF is thought to be produced primarily by the choroid plexuses, which are expansions of the ependymal epithelium, lining the lateral, third, and fourth ventricles [6]. The choroid plexuses are highly folded and vascularized structures consisting of a single layered cuboidal or low cylindrical epithelium residing on a basement membrane. The luminal surface area of the choroid plexus epithelial cells is densely covered by microvilli and possess either one primary cilia or small tufts of motile cilia [4, 7].
CSF production at the choroid plexus is mediated by exchange and transport of ions (especially Cl-, Na+ and HCO3-) across the epithelial cells, which generates an osmotic gradient that drives the movement of water from the blood to the ventricle lumen [3, 4, 8]. The importance of ionic transporters in CSF production was originally established using pharmacological tools, which in more recent years have been supported by genetic studies. The following will briefly describe some of the key ionic transport mechanisms that drive the CSF production. For more comprehensive reviews on the role of the choroid plexus in CSF production, we refer to [4, 8].
The Na+/K+-ATPase localized in the apical membrane of the choroid plexus epithelial cell is central for CSF production [4, 8–10]. Data from several labs show that ouabain, which inhibits the Na+/K+-ATPase, reduces CSF production by 50-60% [9, 11, 12]. The Na+/K+-ATPase actively pumps out Na+ from the epithelial cell to the CSF in the ventricular lumen, thereby keeping the intracellular Na+ concentration low (45 mM compared to the extracellular 141-152 mM) [10]. This creates a transmembrane gradient, which drives the import of Na+ across the basolateral membrane possibly via the Na+-dependent HCO3- co-transporter, NCBE [13] and/or the Na+/H+ exchanger NHE1 [10]. The pivotal role of Na+ transport across the choroid plexus epithelium for CSF production has been best demonstrated in studies using amiloride, an inhibitor of sodium transport, or by genetic depletion of Na+ transporters in mice. Amiloride reduces CSF production by 50% [11, 12] and brain ventricle size by 80% [14]. Similarly, deletion of the Slc4a10 gene encoding the Na+-dependent HCO3- co-transporter, NCBE, decreases the expression of the Na+/K+-ATPase and of the water channel AQP1 in mouse choroid plexus [15].
HCO3- and its transcellular exchange with Cl- have also been demonstrated to be important for CSF production. Application of acetazolamide or DIDS, inhibitors of carbonic anhydrases and anion exchange, respectively, reduces CSF formation by 30-50% [9, 16–18]. The mechanisms by which HCO3- and Cl- and their exchange contribute to regulation of CSF production is still unclear [8]. It is speculated that intracellular accumulation of HCO3- (as a consequence of HCO3- co-import with Na+ via NCBE, and intracellular HCO3- formation by carbonic anhydrase-catalyzed hydration of CO2) drives the outward transport of HCO3- down its electrochemical gradient via HCO3- channels and the HCO3-/Cl- exchanger, AE2 in the basolateral membrane. The exchange of HCO3- with Cl- then causes accumulation of intracellular Cl- [8, 10], and generates an electrochemical gradient for Cl-. As a result, Cl- leaves the cell via apically-located Cl- channels and transporters such as NKCC1 (that also exports Na+ and K+ to the ventricles) [8, 19] (Fig. 2). Overall, the abovementioned processes generate a net movement of Na+, Cl- and HCO3- from the blood across the choroid plexus epithelium to the ventricles. This outward movement of Na+, Cl- and HCO3- is believed to generate the osmotic gradient that drives water in the same direction across the apical membrane [4, 8, 10]. Water fluxes across the choroid plexus epithelium take place mainly through the highly water permeable channel, AQP1, located primarily in the apical membrane and to a smaller degree in the basolateral membrane of the choroid plexus epithelial cells [19–23]. It is debated whether AQP1 is the sole route for water transport across the choroid plexus, however, AQP1 is critical for CSF production since knockout of AQP1 in mice reduces the CSF production rate by 35% and choroid plexus water permeability by 80% compared to wildtype littermates [24, 25]. Overall, the net result of ion and water movement across the choroid plexus epithelium is production of CSF that, compared to the blood, is lower in protein and K+ [26], and higher in Na+, Cl- and Mg2+ and has a 99% water content compared to a water content of 92% in plasma [3, 5].
Despite decades of research, surprisingly little is known about the physiological processes regulating CSF production. It is expected that CSF production is regulated by intracranial pressure, but existing reports are contradictory and suggest that intracranial pressure must be increased significantly or chronically to suppress CSF production [4, 27]. Additionally, CSF production is possibly also regulated by the autonomic nervous system, but again the literature is complex possibly reflecting technical limitations [28].
The choroid plexus as the sole source of CSF is debated
CSF is continuously produced. In humans and mice CSF is renewed approximately four and 12 times each 24hours, respectively, and the total CSF volume of 150-160 mL in human and 0.04 mL in mice is kept constant by removal of CSF [3, 25, 29]. CSF is drained into the peripheral lymphatic system by efflux via the olfactory bulb and along cranial and spinal nerves [20, 30, 31]. Recently, the importance of the arachnoid granulations in CSF removal has been questioned [32]. Hence, efflux along cranial and spinal nerves and the olfactory route might represent the most important efflux pathways for CSF [30, 33].
According to the classical model, the choroid plexuses alone are responsible for the vast majority (80-90%) of CSF formation [34–36]. Evidence for the significant involvement of the rodent choroid plexus in transport of solutes was underscored in a proteomic study reporting that 6.7% of the total number of proteins in the choroid plexus is involved in transmembrane ion transport. This is a larger proportion than in the kidney, where the proportion of proteins estimated to be involved in ion transmembrane transport activity was 4.8% [37]. However, discrepancies between experimental results from fundamental studies of CSF formation and the classical hypothesis, have provided the basis for researchers, among whom are Bulat, Orešković and Klarica, toadvocate for a new model of CSF hydrodynamics [36, 38]. Basically, Bulat, Orešković and Klarica propose that CSF formation occurs by filtration and flux of fluid through the capillary walls, and that the respective volumes of CSF and interstitial fluid mainly depend on hydrostatic and osmotic forces between the CSF and brain parenchyma created by gradients of proteins and inorganic ions across the capillary membrane [36, 39]. Accordingly, under physiological conditions, water is filtered from capillaries with high capillary pressure, to the interstitial fluid and CSF. In these capillaries, the permeability of plasma electrolytes such as Na+ and Cl− is low and the electrolytes are therefore retained. This generates an osmotic counter pressure that opposes the water filtration so when plasma reaches the low hydrostatic pressure capillaries and venules, water is reabsorbed into vessels from the interstitial fluid and CSF [36]. Hence, according to this newer hypothesis, CSF and interstitial fluid are continuously interchanging and the volume occupied by each compartment depends on hydrostatic and osmotic forces.
Recently, Buishas, Gould and Linninger introduced a third hypothesis namely a computational model that is based on existing empirical data. Their model attempts to combine the two above-mentioned hypotheses and takes into account the evidence of the glymphatic pathway [40] explained below. The mathematical model is proposed to “predict the effects the osmolarity of ECS (extracellular space), blood, and CSF on water flux in the brain, establishing a link between osmotic imbalances and pathological conditions such as hydrocephalus and edema” [40]. This novel model needs validation, but could turn out to provide unique insight into CSF dynamics during normal physiology and pathology.
Brain vasculature and the perivascular space
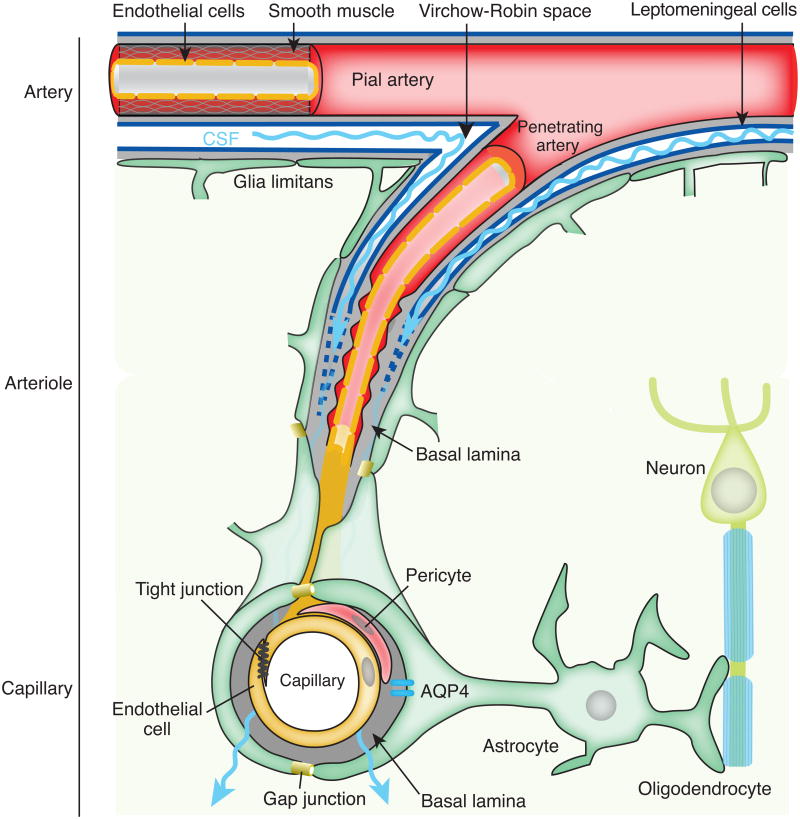
The brain's vasculature has several unique features that distinguishes it from the vasculature in the rest of the body [41]. The arterial cerebral circulation consists of an anterior cerebral circulation and posterior cerebral circulation supplied by the internal carotid arteries and the vertebral arteries, respectively. The anterior circulation, which includes the middle and anterior cerebral arteries, communicates with the posterior circulation, the basilar artery and posterior cerebral arteries, via anterior and posterior communicating arteries at the Circle of Willis [42]. From the Circle of Willis, the anterior circulation perfuse the evolutionary younger parts of the brain including the neocortex of the cerebral hemispheres, while the posterior circulation supplies the brainstem and cerebellum [42]. At the cortical surface, cerebral arteries extend into pial arteries running through the CSF-containing subarachnoid space and the subpial space [43, 44]. As pial arteries dive down into the brain parenchyma they transition into penetrating arterioles (Fig. 3) [41] and create a perivascular space, known as the Virchow-Robin space. The Virchow-Robin spaces are filled with CSF and bordered by a leptomeningeal cell layer on both the inner wall facing the vessel and on the outer wall facing perivascular astrocytic endfeet. In fact, a unique feature of the CNS vasculature is that all arterioles, capillaries, and venules within the brain parenchyma are surrounded by astrocytic vascular endfeet. These vascular endfeet create the outer wall of the perivascular space resembling a donut-shaped tunnel surrounding the vasculature. As the penetrating arterioles narrow deeper down in the brain parenchyma, the Virchow-Robin spaces become continuous with the basal lamina. Thus, the Virchow-Robin space disappears before the capillary level where the perivascular space consists solely of basal lamina. The basal lamina is a thin sheet of extracellular matrix composed primarily of laminin, fibronectin, type IV collagen in which heparin sulfate proteoglycan and other extracellular matrix component reside. The endothelial cells, pericytes and astrocytes are separated by the basal lamina. These three cells types and the other two cellular components of “the neurovascular unit”, smooth muscle cells and neurons, are tightly linked to the extracellular matrix of the basal lamina by adhesion molecules, including integrins and dystroglycan [5, 45]. Due to the porous structure of extracellular matrix the basal lamina provides minimal resistance to CSF influx.
Fig. 3. The neurovascular unit.
The structure and function of the neurovascular unit allow bidirectional communication between the microvasculature and neurons, with astrocytes playing intermediary roles. Pial arteries in the subarachnoid space bathed in CSF become penetrating arteries upon diving into the brain parenchyma. The perivascular space around penetrating arteries is termed the Virchow-Robin space. As the penetrating arteries branch into arterioles and capillaries the CSF-containing Virchow-Robin spaces narrow and finally disappear. However, the perivascular space extends to arterioles and capillaries to venules where it is made up by the basal lamina's extracellular matrix that provides a continuity of the fluid space between arterioles and venules. Astrocytic vascular endfeet expressing aquaporin-4 (AQP4) surround the entire vasculature and form the boundary of the perivascular spaces.
In addition to constituting a low resistance pathway for influx of CSF, the perivascular spaces are also important sites for delivery of energy substrate and regulation of blood flow. In pathological conditions, such as stroke, the innate inflammatory response and edema formation is initiated in the perivascular spaces [45].
From the cerebral capillaries blood continues into the post-capillary venules where the basement membranes of endothelial cells and astrocytes enlarge to again provide a CSF-drained perivascular space [46]. In general, blood from the brain's interior, including the deep white and gray matter surrounding the lateral and third ventricles flows into the larger central/deeps veins and exits the cerebral cortex and subcortical white matter via the cortical veins that extend to the brain surface as pial veins [47, 48]. However, in contrast to the arterial cerebral circulation, where territories are restricted to separate anterior vs. posterior arteries, the territories drained by the central veins and cortical veins reveal a marked degree of overlapping. Hence in certain regions, the territories of cortical veins extend far down to the ventricular wall and in other areas a central vein territory can include areas of the subcortical layers [47]. The superficial cortical veins anastomose with the deep veins and empty into the superior sagittal sinus. Cerebral venous blood from the superior sagittal sinus and the deep veins leave the brain via a confluence of sinuses draining into the sigmoid sinuses and jugular veins [48].
The glymphatic system
Recent studies have demonstrated that CSF and interstitial fluid (ISF) continuously interchange. This exchange is facilitated by convective influx of CSF along the periarterial space [49]. From the subarachnoid space, CSF is driven into the Virchow-Robin spaces by a combination of arterial pulsatility, respiration, and CSF pressure gradients and the loose fibrous matrix of the perivascular space can be viewed as a low resistance highway for CSF influx. The subsequent transport of CSF into the dense and complex brain parenchyma is facilitated by AQP4 water channels expressed in a highly polarized manor in astrocytic endfeet that ensheathe the brain vasculature [49, 50]. CSF movement into the parenchyma drives convective interstitial fluid fluxes within the tissue toward the perivenous spaces surrounding the large deep veins. The interstitial fluid is collected in the perivenous space from where it drains out of brain toward the cervical lymphatic system [30, 33]. This highly polarized macroscopic system of convective fluid fluxes with rapid interchange of CSF and interstitial fluid was entitled the glymphatic system based on its similarity to the lymphatic system in the peripheral tissue in function, and on the important role of glial AQP4 channels in the convective fluid transport.
In 2012, the dynamics of the glymphatic system was characterized for the first time in vivo using two-photon microscopy in mice [49]. By labeling of CSF with fluorescent tracers injected into the cisterna magna, Iliff et al. showed that CSF rapidly enters the brain along the cortical pial arteries. The entry was followed by influx into the Virchow-Robin spaces along penetrating arterioles (Fig. 4) [49]. It was evident that the CSF tracers, rather than being diffusely and randomly distributed in the parenchyma, entered the parenchyma through a periarterial pathway surrounding the vascular smooth muscle cells bounded by perivascular astrocytic endfeet, and ex vivo evidence showed that tracers rapidly exited the brain primarily along central deep veins and the lateral-ventral caudal rhinal veins [49]. The following analyses showed that the convective movement of periarterial CSF into and through the brain parenchyma facilitated the clearance of interstitial solutes to perivenous drainage pathways, thereby extending earlier studies with labeled proteins and small molecules (reviewed in [51]). As proposed by Weller and colleagues [52–54], such a macroscopic clearance mechanism of interstitial solutes may be of particular importance for neurodegenerative diseases including Alzheimer's disease, which is characterized by the accumulation of proteins, including amyloid plaques and tau tangles. To evaluate whether β-amyloid is cleared by the glymphatic pathway, Iliff et al. injected fluorescent or radiolabeled amyloid β1–40 into the mouse striatum, and found that β-amyloid was rapidly cleared from the mouse brain along the glymphatic paravenous efflux pathway [49]. Furthermore, imaging of CSF tracer movement in AQP4 knockout mice revealed a ∼65% reduction in CSF fluid flux through the parenchyma compared to wildtype control mice and a clearance of intrastriatal injected radio-labeled β-amyloid, which was reduced by 55% [49]. It was therefore proposed that the paravascular glymphatic pathway driven by AQP4-dependent bulk flow constitutes a major clearance pathway of interstitial fluid solutes from the brain's parenchyma [50].
Fig. 4. In vivo two-photon imaging of glymphatic influx in the mouse cortex.

A) Schematic representation of the imaging setup; Periarterial CSF influx of tracers injected in the cisterna magna into the subarachnoid CSF was assessed in vivo using two-photon microscopy through a closed cranial window. Lower bar: Imaging conducted at the cortical surface in 1-min intervals. B) 5 min after injection of small (TR-d3, dark blue) and large (FITC-d2000, green) molecular weight tracers and C-E) 100μm below the cortical surface 10, 20 and 30 min after injection of the tracers. Merge (light blue) indicates co-localization of TR-d3 and FITC-d2000. The cerebral vasculature was visualized with intra-arterial flourescent tracer (CB-d10), and arteries (A) and veins (V) were identified morphologically. Immediately after intracisternal injection, CSF tracer moved along the outside of the pial arteries, but not veins, and after 20-30 min they diffused into the brain parenchyma. Red circles, arterioles; blue circles, venules. Scale bars 100μm. Reprinted from [49] with permission.
Lipid transport by the glymphatic system
The human brain weighs 2% of the body's total weight but contains 25% of the cholesterol in the human body [55]. Despite the brain being highly enriched in cholesterol, the blood-brain-barrier prevents influx of lipids and lipoproteins, including cholesterol, from the blood to the brain. Unlike peripheral tissues, which obtain blood-borne cholesterol secreted by the liver, the brain synthesizes all its cholesterol de novo. Excess cholesterol is eliminated from the brain by hydroxylation of cholesterol to 24-OH cholesterol. In fact, 80% of the 24-OH cholesterol in the body is found in the brain and the circulatory system acts as sink for excess cholesterol produced in the brain [56, 57]. The brain is well equipped for internal lipid transport via its own supply of lipid carrier particles of the high density lipoprotein type secreted by astrocytes [58]. Secretion of high density lipoprotein particles from astrocytes is dependent on lipoproteins, mainly Apolipoprotein E and J, and allows delivery of lipids such as cholesterol to neurons [58]. Apolipoprotein carriers also mediate clearance of excess hydroxylated cholesterol and β-amyloid [59]. The Apolipoprotein E allel 4 is a major genetic risk factor for Alzheimer's disease, indicating that this lipid carrier is important for maintaining homeostasis necessary for a healthy environment of the brain [60, 61]. Apolipoprotein E is particularly concentrated in astrocytic processes at the pial surface and around the blood vessels [62]. In addition, the choroid plexus and tanycytes in the wall of the third ventricle also produce Apolipoprotein E [62, 63]. Thus, Apolipoprotein E production is co-localized with CSF production sites and transport pathways suggesting that lipids are transported by the glymphatic system. Injections of lipophilic CSF tracers showed that several different lipophilic molecules of sizes <1 kDa, similar to the size of cholesterol (0.387 kDa) and a larger 3 kDa lipophilic molecule all entered the brain via periarterial routes and exited perivenously [64], similar to hydrophilic molecules [49]. In this way the glymphatic system was comparable to the peripheral lymphatic system that transports the dietary fat, incl. cholesterol, absorbed in the intestine. However, only the <1 kDa lipophilic tracers diffused into the brain parenchyma whereas the larger tracers were largely confined to the perivascular routes [64]. This suggests that the glymphatic system plays a central role in macroscopic distribution of lipids in the brain and that medium to large lipid soluble molecules might require carrier particles in order to be delivered via the CSF. Astrocytes thus play a key role in lipid synthesis and lipid distribution by releasing lipid carrier proteins, such as Apolipoprotein E, and in maintaining the highway for distribution, the glymphatic system.
What drives glymphatic influx?
Glymphatic transport of CSF along the periarterial spaces, followed by convective flow through the brain parenchyma, and exit of interstitial fluid (ISF) along the perivenous space to the cervical lymph system, is an energy requiring process that is driven by multiple mechanisms. The constant production of CSF by the choroid plexus creates a pressure that dictates the direction of the fluid flow through the ventricular system to the subarachnoid space. In addition, several lines of work show that respiration is instrumental in movement of CSF through the aqueduct [65, 66]. Entry of CSF along the perivascular space is crucial for facilitating glymphatic ISF-CSF exchange and clearance function. Using reporter mice to distinguish arteries from veins (Ds-red fluorescent protein expressed under the NG2 promoter in pericytes and smooth muscle cells) [67, 68], it was demonstrated that CSF tracers follow arteries at the pial surface running across the cortical surface and descend along penetrating arteries, which dive perpendicularly into the brain to reach capillary beds [49, 69]. What drives the entry of CSF along perivascular space of penetrating leptomeningeal arteries specifically? Particular to arteries, pulsation generated by smooth muscle cells creates pulse waves along the whole length of the pial artery and penetrating arteries diving into the brain from the cortical surface [70–73]. Dobutamine, an adrenergic agonist, increased pulsatile effect significantly when administrated to mice and resulted in a larger amount of CSF penetration into the parenchyma. The opposite effect was obtained when arterial pulsatility was dampened by internal carotid artery ligation. Additionally, the reduction of pulse waves decreased CSF-ISF exchange [70]. This suggests that glymphatic activity, at least in part, is driven by arterial pulsatility and explains why perivascular influx occurs preferentially around pulsating arteries and not cerebral veins.
The glymphatic system is turned on during sleep
While sleep is essential for all mammals, sleep is also a vulnerable state since the decreased alertness during sleep increase the chance of being targeted by predators. This compromise in alertness versus rest suggests that sleep serves a fundamental biological function. Multiple studies indicating that sleep enhances memory consolidation, which could be important for competition amongst species [74–77], however, the basic biological need for sleep is unclear [78]. Brain energy metabolism only declines by 25% during sleep suggesting that sleep does not simply serve to conserve energy [79]. Recent analysis shows that the sleep state is unique in the sense that glymphatic activity is dramatically enhanced, while its function is suppressed during wakefulness. In vivo 2-photon imaging of glymphatic function showed that the CSF influx in the awake state was reduced by 90% compared to anesthetized mice [80]. In order to test if this was specific to the unconscious state or a side effect of the anesthetics used, the same experiment was performed in naturally sleeping mice. This analysis of CSF influx showed a striking similarity between true sleep and anesthetized mice. The sleep-wake difference in glymphatic influx correlated with the volume fraction of interstitial space that was 13-15% in the awake state an expanded to 22-24% in both sleep and anesthetized mice [80]. This observation indicates that the sleep state is particularly conducive to convective fluid fluxes and thereby to clearance of metabolites. Thus, a major function of sleep appears to be that the glymphatic system is turned on and that the brain clears itself of neurotoxic waste products produced during wakefulness.
The observation that glymphatic function is highly active in both anesthetized mice and naturally sleeping mice but not awake mice indicates that it is differences in the sleep versus wakeful state and not daily circadian rhythms that regulate glymphatic activity. A major driver of arousal is the neuromodulator norepinephrine [81]. Our analysis showed that norepinephrine also is a key regulator of glymphatic activity and that norepinephrine might be responsible for suppression of glymphatic during wakefulness. Local application of a cocktail of norepinephrine receptor antagonists in awake mice resulted in an increase in CSF tracer influx almost comparable to that observed during sleep or anesthesia [80]. In contrast, norepinephrine application, mimicking the wakeful state, significantly decreased the interstitial volume fraction. An increase in interstitial space volume in the sleep state reduces tissue resistance towards convective flow thus permitting CSF-ISF exchange. Thus the burst release of norepinephrine during arousal increases the cellular volume fraction resulting in a decrease in the interstitial space [82]. In turn, the resistance toward convective exchange of CSF and ISF increases and this results in a suppression of glymphatic fluxes during wakefulness. Norepinephrine also acts directly on choroid plexus epithelial cells and inhibits CSF production. Conversely, removal of norepinephrine signaling, mimicking the sleep state, enhances CSF production [83]. The concerted effect of norepinephrine thus acts via different mechanisms on both fluid availability and convective fluxes to suppress glymphatic function and norepinephrine can therefore be considered both a key regulator of the switch between the sleep and wakeful state and solute clearance from the brain.
Convective CSF fluxes in aging and pathology
Glymphatic activity decreases sharply during aging
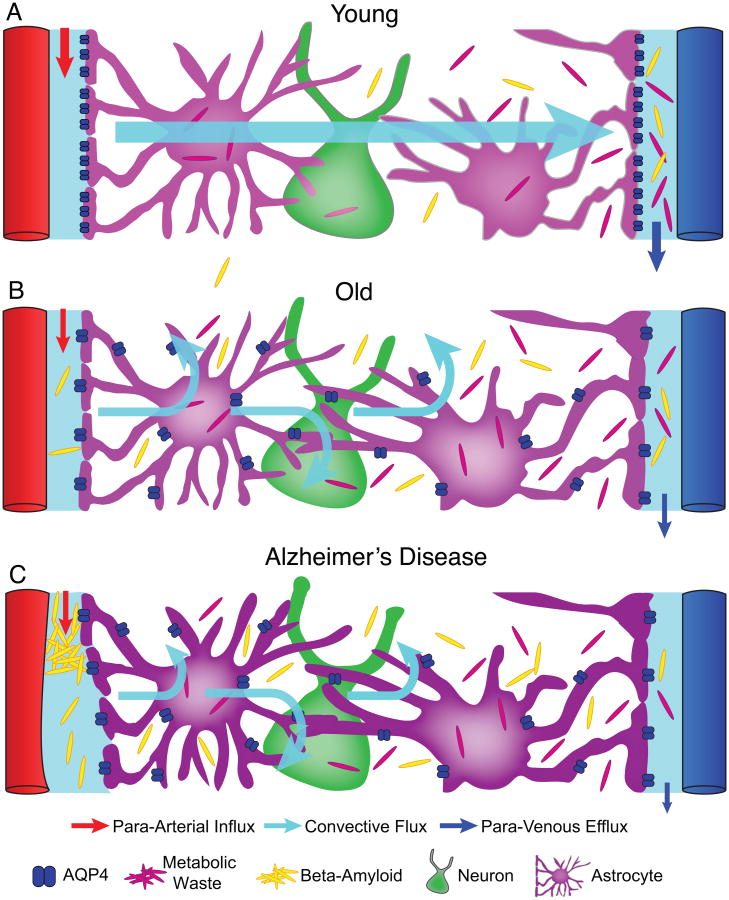
A recent assessment of glymphatic function in old versus young mice showed a dramatic reduction by ∼80-90% in aged compared to young mice [84]. The suppression of glymphatic activity included both influx of CSF tracers and clearance of radiolabeled β–amyloid and inulin. Reactive gliosis, defined by hypertrophy of GFAP+ astrocyte processes, increases with aging [85] and might contribute to the age-related decline in glymphatic function, although the mechanism of how changes in GFAP expression might contribute to altered glymphatic function remains unclear. AQP4, which in young animals is localized to astrocytic endfeet, plays a central role in facilitating CSF-ISF exchange along periarterial influx pathways as well as interstitial solute clearance through perivascular drainage pathways [49] (Fig. 5A). The genetic deletion of AQP4 was previously shown to impair CSF-ISF exchange by ∼65% and reduce the clearance of β–amyloid by ∼55% [49]. The lack of parity between decline in CSF-ISF exchange and β–amyloid clearance is likely attributable to some fraction of injected β–amyloid being cleared directly to the blood via LRP-1/RAGE mediated trans-endothelial transport [86]. However, the vascular polarization of astrocytic AQP4 is partly lost in reactive astrocytes in old brains, i.e. AQP4 is no longer confined to astrocytic endfeet but present in astrocytes parenchymal processes [84] (Fig. 5B). The findings that aging was associated with loss of perivascular AQP4 polarization, specifically along penetrating arterioles, and that presence of cortical parenchymal AQP4 was found to correlate with CSF-ISF exchange, suggests that the age related decline in glymphatic function might be in part attributable to dysregulation of astroglial water transport. Other factors perhaps contributing to the reduction of glymphatic activity with aging are the decline in CSF production by 66% and CSF pressure by 27% percent [70, 87, 88]. Aging is also accompanied by stiffening of the arterial wall leading to a reduction in arterial pulsatility, which is one of the drivers of glymphatic influx [70, 89]. The observation of age-related decline in glymphatic activity is important because the highest risk factor identified for neurodegenerative diseases is aging. The failure of the glymphatic system in aging might thus contribute to the accumulation of misfolded and hyperphosphorylated proteins and thereby render the brain more vulnerable to developing a neurodegenerative pathology or perhaps escalate the progression of cognitive dysfunction.
Fig. 5. Model of glymphatic function in young, old and in Alzheimer's disease.
A) In young and healthy people, CSF enters the brain parenchyma via periarterial pathways, washes out solutes from the interstitial space and empties along the veins. B) With aging, glymphatic function is reduced, possibly due to astrocytes becoming reactive and AQP4 de-polarized from the vascular endfeet to parenchymal processes. C) In Alzheimer's disease perivascular space of penetrating arteries are subject to accumulation of β-amyloid peptides. We hypothesize that accumulation of β-amyloid might be caused by impairment of the glymphatic system and that the perivascular pathways are further blocked by protein aggregates such as β-amyloid. In this model, the resulting changes in the perivascular environment lead to abnormal enlargement of perivascular space downstream, which further decreases glymphatic clearance.
Indeed, all prevalent neurodegenerative diseases are characterized by accumulation of aggregated proteins [90]. Prior work on protein degradation in CNS has primarily focused on intracellular processes, i.e. proteasomal or lysosomal degradation [91]. However, more recent studies have revealed that toxic protein monomers, oligomers, and aggregates are also present in the interstitial fluid and CSF: misfolded β–amyloid and fibrillary tangles of tau in Alzheimer's disease, misfolded α-synuclein in Parkinson's disease and misfolded superoxide dismutase in mouse models of amyotrophic lateral sclerosis [52, 92–96]. Deposits of β-amyloid are found in hippocampal synapses where activity of the neurons might lead to increased shedding making synapses a source of extracellular β-amyloid [97]. In concert with this, β-amyloid production is highest during the awake state when neuronal activity is highest [98]. However, β-amyloid is not only produced by neurons. In fact, all cells produce β-amyloid and in particular oligodendrocytes and their precursor cells [99], which, at least in part, might account for the myelin disorders observed in Alzheimer's disease. The emerging concept of a prion-like spread of neurotoxic proteins aggregates highlights the importance of the interstitial space regarding deposits of aggregated protein, such as β-amyloid in Alzheimer's disease[100, 101]. The production and turnover of β-amyloid is strikingly rapid in humans. In healthy, young subjects 8.3% of total β-amyloid is cleared each hour via the CSF [102]. Perivascular drainage pathways function as a sink for interstitial β-amyloid in Alzheimer's disease and perivascular spaces are a sites for both amyloid deposits and Alzheimer's disease pathology [103]. Bulk clearance by the glymphatic system might in combination with transport across the blood-brain barrier [59] provide necessary and sufficient removal of extracellular β-amyloid until the end of the reproductive lifespan around which time failure in adequate CSF bulk flow leads to accumulation of β-amyloid [84] (Fig. 5). This suggests that low activity of the glymphatic system could be a major risk factor for development of neurodegenerative diseases. The anatomical routes of interstitial bulk flow in the perivascular space are consistent with sites of β-amyloid accumulation, although β-amyloid accumulates predominantly at cerebral arteries. Periarterial accumulation of β-amyloid around arteries could reflect recirculation of β-amyloid-rich CSF that deposits aggregates after being taken up by smooth muscles cells [104], although the concept of recirculation of CSF is controversial [44]. In turn, vascular amyloidosis might reduce glymphatic CSF influx and the stagnation of CSF influx might accelerate β-amyloid accumulation. In addition, monocytic engulfment of β-amyloid appears to occur selectively at veins [105]. Abnormal enlargement of the perivascular space is more frequently observed in Alzheimer's disease compared to aged-matched control subjects suggesting a spiral of protein accumulation, deformation of glymphatic routes and further reduction in protein clearance and pathology (Fig. 6).
Fig. 6. Abnormal perivascular spaces in Alzheimer's disease.
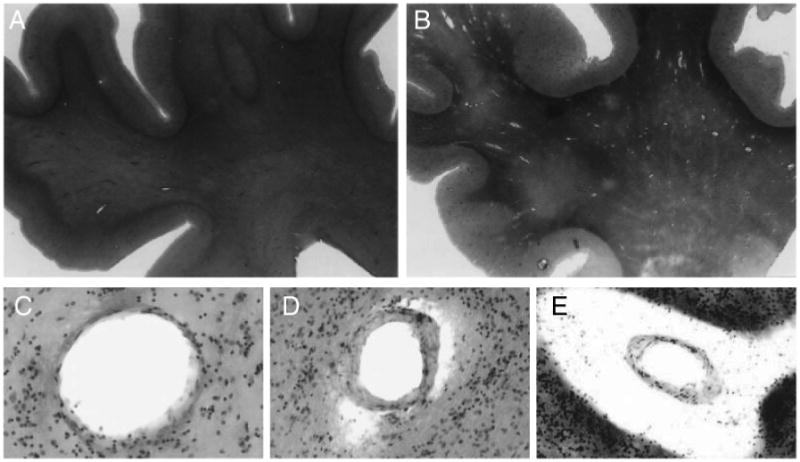
2.5× magnification of hematoxylin and eosin staining of superior frontal gyrus and underlying white matter. A) The white matter of a 74-year old with no CNS diagnosis shows homogenously stained white matter with normal perivascular spaces. B) The white matter of an 80-year old Alzheimer's disease patient contains patches with paler staining and a large number of abnormally enlarged perivascular spaces. 100× magnification of normal C), slightly dilated D) and severely dilated E) perivascular spaces in an Alzheimer's disease patient. Reprinted from [112] with permission.
However, abnormalities at the perivascular space are also prominent in non-Alzheimer's dementia. Only surpassed by Alzheimer's disease, vascular dementias are the second most common cause of dementia and these diseases are also characterized by deformation of the perivascular space [106, 107]. Changes in or surrounding cerebral blood vessels due to hypertension, atherosclerosis or hereditary diseases can cause vascular dementia [107]. Vascular dementia is often caused by pathology in small cerebral blood vessels and capillaries, collectively termed small vessel disease. In small vessel disease enlargement of the perivascular space is frequently observed [108]. An example of this is the disease cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy [109, 110]. We speculate that these anatomical abnormalities in the perivascular space could have a profound impact on glymphatic fluxes due to altered physical, and perhaps also cellular signaling pathways in ways that are non-permissive for bulk flow in the perivascular spaces. In fact, numerous case reports found abnormal widening of perivascular space in dementia patients otherwise in good health [111]. One explanation for widening of the perivascular space could be periarterial blockage leading to local obstruction of glymphatic fluxes, perhaps affecting the width of the downstream periarterial space (Fig. 5). Roher et al. hypothesized that the enlargement of perivascular space in the white matter occurs as a secondary effect of clogging of perivascular space in the upstream artery, usually located in the grey matter [112]. Myelin-rich tissue may be more sensitive to obstruction of convective interstitial fluid fluxes, perhaps explaining why vascular diseases, including cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy, primarily affect white matter [113]. It is important to note, that the potential role of glymphatic fluxes in diseases with prominent enlargement of perivascular spaces has yet to be addressed experimentally, but that gross changes of the perivascular space are likely to negatively affect glymphatic functions. A suppression of glymphatic function could in turn exacerbate pathology.
Traumatic brain injury and its implications for neurodegenerative diseases
Traumatic brain injury, which most frequently affects military personnel or athletes, increases the risk of premature dementia and Alzheimer's disease [114, 115]. Multiple studies have shown that repeated traumatic events, and even single events of moderate to severe head trauma, can lead to progressive neurodegeneration. However, it is currently not understood why a subpopulation of individuals develops chronic traumatic encephalopathy, whereas other exposed to the same degree of initial brain injury are not affected [116]. Traumatic brain injury induces release of β-amyloid peptide and of C-tau, a proteolytically cleaved product of MAP-tau, which is a highly abundant intracellular microtubule protein in axons [117–119]. C-tau is a biomarker of brain injury since it is released in vast quantities and correlates with severity of traumatic brain injury [120]. An emerging hypothesis is that the large amplitude increases of interstitial tau lead to cellular uptake and initiation of fibrillary aggregates, which attracts additional tau leading to formation of neurofibrillary tangles ultimately resulting in a prion-like spread of the pathology [100, 101]. Traumatic brain injury is linked to formation of large astroglial scars and persistent activation of innate neuroinflammation [121]. Strikingly, in a model of repetitive moderate traumatic brain injury, influx of CSF into the brain and CSF-mediated clearance was impaired in the ipsilateral hemisphere already at day 1 post injury. The reduction of glymphatic function persisted until at least 28 days post injury. The severe decrease in glymphatic function was associated with glial scars characterized by hypertrophic GFAP-positive processes in the ipsilateral hemispheres. In addition, mis-localization of AQP4 from vascular endfeet to parenchymal processes was observed, similar to AQP4 mislocation noted in aging [84]. By intracortical injections of human tau Iliff et al. were able to track the clearance pathway of tau. Human tau accumulated around large veins and the amount of tau remaining in the tissue correlated with a decrease in glymphatic clearance [121]. This suggests that CSF-mediated removal of tau via glymphatic routes is crucial for limiting secondary neuronal damage following traumatic brain injury. Another study using magnetic resonance imaging (MRI) to assess glymphatic function provided further indication that head trauma, such as subarachnoid hemorrhage, severely impairs glymphatic function [122]. Freshly isolated arterial blood injected into the CSF was enough to block influx pathways of CSF into the brain, but not the cerebellum, suggesting that cerebral hemorrhage can cause a widespread inhibition of glymphatic function. In this model of subarachnoid hemorrhage tissue-type application of plasminogen activator that removes fibrin clots improved glymphatic perfusion. Embolic ischemic stroke produced a transient inhibition of glymphatic flow in the hours following ischemia, however, function was spontaneously recovered at 24 hours after transient ischemia [122]. This suggests that short-term inhibition of glymphatic function, either by decreased arterial pulsation or occlusion of perivascular pathways caused by mild stroke, can resolve and is linked to improved recovery.
Glymphatic efflux play a key role in transport of biomarkers of traumatic brain injury
Due to the difficulties in diagnosing the severity of traumatic brain injury based on clinical examination alone, considerable effort has gone into developing plasma biomarkers of brain injury. Although it is known that CSF drains into cervical lymph nodes, prior efforts gave minute attention to how cellular proteins, e.g. neuron-specific enolase, GFAP and S100B, enter the blood [123]. Most reviews have suggested that these biomarkers enter the general circulation through opening of the blood-brain barrier in the setting of tissue injury [124]. Instead, we recently showed that the biomarkers of traumatic brain injury exit the brain via the glymphatic system. Inhibition of glymphatic activity by four mechanistically distinct manipulations, including sleep deprivation, cisterna magna puncture, inhibition of CSF production using acetazolamide, or genetic deletion of AQP4 resulted in marked reduction of astrocytic proteins GFAP, S100B and neuron-specific enolase in plasma following traumatic brain injury [125]. Several of these manipulations are clinical relevant. For example, sleep deprivation is common in the emergency room as vitals are taken frequently. Thus, plasma biomarkers may not be a useful approach to asses the severity of traumatic injury if it is the activity of the glymphatic system that determines the extend by which the biomarkers are transported from the injured brain tissue to the blood compartment. If a patient with traumatic brain injury is unable to sleep or if a decompressive ventriculostomy is performed, the transfer of biomarkers from CSF plasma will be low. The low level of biomarkers in the blood under these conditions will not reflect the degree of tissue injury but rather that glymphatic activity is low.
Thus, several studies have shown that acute injury, including traumatic brain injury, subarachnoid bleeding or stroke, profoundly impact glymphatic function and impair convective fluid flow. The suppression of CSF-ISF exchange has immediate implications regarding the limitations of the diagnostic relevance of plasma biomarkers in traumatic brain injury [122, 125]. Most importantly, impairment of glymphatic function could further exacerbate injury due to accumulation of both normal metabolic waste as well as injury-induced debris. The degree by which glymphatic function is suppressed after traumatic brain injury might therefore contribute to the variability in outcome. Future studies will define the clinical relevance of pharmacological manipulations of the glymphatic system after acute traumatic injury.
Prior observations had documented the existence of perivascular fluid transport
Albeit, the concept of the glymphatic system was developed just three years ago, many aspects of this highly organized pathway of CSF-ISF fluid exchange had already been described. In the mid 80's a young investigator, Patricia Grady noted that when horseradish peroxidase, a 44 kDa glycoprotein, was injected in CSF, the entire vasculature of dogs or cats was outlined by the tracer just 4-5 min later [126, 127]. This observation, which depicted widespread influx of a large CSF tracer along the perivascular space, justifiably received considerable attention among the more established groups. Such rapid influx of CSF could not be justified by the slow process of diffusion. Only convective fluxes along the perivascular space could explain the distribution of horseradish peroxidase. However, the inability of other groups to repeat Patricia Grady's findings led to the incorrect conclusion that CSF only inconsistently and to a minor extent entered the perivascular space[128]. In retrospect, the discrepancy between the observations can be explained by the fact that Patricia Grady used larger animals that were exposed to minimal surgery, whereas subsequent studies prepared open cranial windows in rats, which eliminated the pressure gradients that drive convective CSF fluxes. Later, in a series of elegant studies Gerald Dienel showed that metabolites of glucose, including lactate, are rapidly released in large quantities during brain activation [129, 130]. Most interestingly, the metabolites of glucose or tracers of similar molecular weights could later be identified in the perivascular space and in cervical lymph nodes. Thus, the work by Gerald Dienel convincingly identified the perivascular space as a pathway for removal of metabolic waste products. Even older studies from the group of Bradbury had documented that radiolabeled tracers injected into the brain parenchyma later could be found in both the olfactory bulb and the cervical lymph vessels [123].
Future perspectives
Accumulating evidence suggests that age-related decline in glymphatic clearance in significant ways contributes to accumulation of protein aggregation. Glymphatic activity decreases by 80-90% in old mice and several lines of evidence have documented that β-amyloid and tau exit the brain via the glymphatic system[84, 121]. Moreover, work from David Holtzman documents that the concentration of β-amyloid in CSF follows the sleep-wake cycle in human subjects [131]. It is therefore imperative that a diagnostic test of glymphatic activity capable of identifying patients with premature decline in glymphatic clearance is developed. Using the same logic, assessment of glymphatic activity in patients following traumatic brain injury may pinpoint patients with the most severe suppression of glymphatic clearance and thereby identify the individuals who are at higher risk for developing chronic traumatic encephalopathy. Helene Benveniste's group has made headway with regard to developing a glymphatic diagnostic test based on MRI scans. By delivering contrast agent into cisterna magna, the movement of CSF could be followed in real time across the entire brain [69]. These observations made in rats confirmed and extended the notion of the existence of a brain-wide glymphatic system. In particular the MRI analysis revealed fast influx kinetics at two key nodes, the pituitary and pineal gland recesses [69]. Interestingly both of these regions are involved in regulation of the sleep wake cycle [132, 133]. These studies using contrast-enhanced MRI provide the experimental groundwork for evaluating glymphatic pathway function in the human brain and in the future assess whether failure of CSF fluxes contributes to Alzheimer's disease progression. Development of a safe and minimally invasive imaging approach to visualize glymphatic function is therefore necessary for future translational effort. It is in this regard important to note that subsequent analysis showed that intrathecal lumbar injections, which are routinely used in clinical myelographic studies, provide a viable alternative route to assess the basic parameters of glymphatic function [134]. The first studies of the glymphatic system in human subject is expected to be published soon, as intrathecal administration of contrast agents already is approved for study of CSF fluxes in patients undergoing treatment for spontaneous intracranial hypotension and CSF rhinorrhea [135, 136].
Future studies with focus on the glymphatic system are expected to identify functions of convective CSF fluxes beyond removal of metabolic waste products. We have recently found that glymphatic influx can serve as a distribution system for lipids [64] and glucose [137], and we speculate that glymphatic influx provides an essential route for distribution of electrolytes, macromolecules, and other larger compounds that enter the brain predominantly via the blood-CSF barrier at the choroid plexus. Likewise, the glymphatic system might serve as a path for delivery and distribution of drugs including cancer drugs within the brain [138]. Furthermore, we expect that growth factors produced by the choroid plexus, as well as neuromodulators released by several brain stem nuclei positioned close to the ventricular system, are distributed widely across the CNS by the glymphatic system. Thus, volume transmission may, in addition to microscopic release of neuromodulators from local nerve terminals followed by local diffusion, also involve circulation by macroscopic convective CSF fluxes via the glymphatic system.
Acknowledgments
This study was supported by NIH (NINDS NS075177 and NS078304). We thank Gerry Dienel, Ben Kress, and Rashid Deane for comments on the manuscript.
Footnotes
Conflict of Interest: The authors declare that they have no conflict of interest.
References
- 1.Liao S, Padera TP. Lymphatic function and immune regulation in health and disease. Lymphat Res Biol. 2013;11:136–43. doi: 10.1089/lrb.2013.0012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang Z, Ying Z, Bosy-Westphal A, et al. Evaluation of Specific Metabolic Rates of Major Organs and Tissues: Comparison Between Nonobese and Obese Women. Obesity. 2012;20:95–100. doi: 10.1038/oby.2011.256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Johanson CE, Duncan J, Klinge PM, et al. Multiplicity of cerebrospinal fluid functions: New challenges in health and disease. Cerebrospinal Fluid Res. 2008;5:10. doi: 10.1186/1743-8454-5-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Damkier HH, Brown PD, Praetorius J. Cerebrospinal fluid secretion by the choroid plexus. Physiol Rev. 2013;93:1847–92. doi: 10.1152/physrev.00004.2013. [DOI] [PubMed] [Google Scholar]
- 5.Thrane AS, Rangroo Thrane V, Nedergaard M. Drowning stars: reassessing the role of astrocytes in brain edema. Trends Neurosci. 2014;37:620–628. doi: 10.1016/j.tins.2014.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Keep RF, Jones HC. A morphometric study on the development of the lateral ventricle choroid plexus, choroid plexus capillaries and ventricular ependyma in the rat. Brain Res Dev Brain Res. 1990;56:47–53. doi: 10.1016/0165-3806(90)90163-S. [DOI] [PubMed] [Google Scholar]
- 7.Banizs B, Pike MM, Millican CL, et al. Dysfunctional cilia lead to altered ependyma and choroid plexus function, and result in the formation of hydrocephalus. Development. 2005;132:5329–39. doi: 10.1242/dev.02153. [DOI] [PubMed] [Google Scholar]
- 8.Brown P, Davies S, Speake T, Millar I. Molecular mechanisms of cerebrospinal fluid production. Neuroscience. 2004;129:957–70. doi: 10.1016/j.neuroscience.2004.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ames A, Higashi K, Nesbett FB. Effects of Pco2 acetazolamide and ouabain on volume and composition of choroid-plexus fluid. J Physiol. 1965;181:516–524. doi: 10.1113/jphysiol.1965.sp007780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Johanson CE. Neurosci Med. 2008. Choroid plexus - Cerebrospinal fluid circulatory dynamics: Impact on brain growth, metabolism, and repair. [Google Scholar]
- 11.Davson H, Segal MB. The effects of some inhibitors and accelerators of sodium transport on the turnover of 22Na in the cerebrospinal fluid and the brain. J Physiol. 1970;209:131–153. doi: 10.1113/jphysiol.1970.sp009159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Segal MB, Burgess AM. A combined physiological and morphological study of the secretory process in the rabbit choroid plexus. J Cell Sci. 1974;14:339–350. doi: 10.1242/jcs.14.2.339. [DOI] [PubMed] [Google Scholar]
- 13.Christensen HL, Nguyen AT, Pedersen FD, Damkier HH. Na(+) dependent acid-base transporters in the choroid plexus; insights from slc4 and slc9 gene deletion studies. Front Physiol. 2013;4:304. doi: 10.3389/fphys.2013.00304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jacobs S, Ruusuvuori E, Sipilä ST, et al. Mice with targeted Slc4a10 gene disruption have small brain ventricles and show reduced neuronal excitability. Proc Natl Acad Sci U S A. 2008;105:311–6. doi: 10.1073/pnas.0705487105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Damkier HH, Praetorius J. Genetic ablation of Slc4a10 alters the expression pattern of transporters involved in solute movement in the mouse choroid plexus. Am J Physiol Cell Physiol. 2012;302:C1452–9. doi: 10.1152/ajpcell.00285.2011. [DOI] [PubMed] [Google Scholar]
- 16.Saito Y, Wright EM. Bicarbonate transport across the frog choroid plexus and its control by cyclic nucleotides. J Physiol. 1983;336:635–48. doi: 10.1113/jphysiol.1983.sp014602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mayer SE, Sanders-Bush E. Sodium-dependent antiporters in choroid plexus epithelial cultures from rabbit. J Neurochem. 1993;60:1308–1316. doi: 10.1111/j.1471-4159.1993.tb03291.x. [DOI] [PubMed] [Google Scholar]
- 18.Deng QS, Johanson CE. Stilbenes inhibit exchange of chloride between blood, choroid plexus and cerebrospinal fluid. Brain Res. 1989;501:183–187. doi: 10.1016/0006-8993(89)91041-X. [DOI] [PubMed] [Google Scholar]
- 19.Praetorius J, Nielsen S. Distribution of sodium transporters and aquaporin-1 in the human choroid plexus. Am J Physiol Cell Physiol. 2006;291:C59–67. doi: 10.1152/ajpcell.00433.2005. [DOI] [PubMed] [Google Scholar]
- 20.Praetorius J. Water and solute secretion by the choroid plexus. Pflugers Arch. 2007;454:1–18. doi: 10.1007/s00424-006-0170-6. [DOI] [PubMed] [Google Scholar]
- 21.Nielsen S, Smith BL, Christensen EI, Agre P. Distribution of the aquaporin CHIP in secretory and resorptive epithelia and capillary endothelia. Proc Natl Acad Sci U S A. 1993;90:7275–7279. doi: 10.1073/pnas.90.15.7275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Damkier HH, Brown PD, Praetorius J. Epithelial pathways in choroid plexus electrolyte transport. Physiology (Bethesda) 2010;25:239–49. doi: 10.1152/physiol.00011.2010. [DOI] [PubMed] [Google Scholar]
- 23.Papadopoulos MC, Verkman AS. Aquaporin water channels in the nervous system. Nat Rev Neurosci. 2013;14:265–77. doi: 10.1038/nrn3468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Oshio K, Song Y, Verkman AS, Manley GT. Aquaporin-1 deletion reduces osmotic water permeability and cerebrospinal fluid production. Acta Neurochir Suppl. 2003;86:525–528. doi: 10.1007/978-3-7091-0651-8_107. [DOI] [PubMed] [Google Scholar]
- 25.Oshio K, Watanabe H, Song Y, et al. Reduced cerebrospinal fluid production and intracranial pressure in mice lacking choroid plexus water channel Aquaporin-1. FASEB J. 2005;19:76–78. doi: 10.1096/fj.04-1711fje. [DOI] [PubMed] [Google Scholar]
- 26.Husted RF, Reed DJ. Regulation of cerebrospinal fluid potassium by the cat choroid plexus. J Physiol. 1976;259:213–221. doi: 10.1113/jphysiol.1976.sp011462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Silverberg GD, Huhn S, Jaffe R, et al. Downregulation of cerebrospinal fluid production in patients with chronic hydrocephalus. J Neurosurg. 2002;97:1271–5. doi: 10.3171/jns.2002.97.6.1271. [DOI] [PubMed] [Google Scholar]
- 28.Lindvall M, Owman C. Autonomic nerves in the mammalian choroid plexus and their influence on the formation of cerebrospinal fluid. J Cereb Blood Flow Metab. 1981;1:245–66. doi: 10.1038/jcbfm.1981.30. [DOI] [PubMed] [Google Scholar]
- 29.Szentistványi I, Patlak CS, Ellis RA, Cserr HF. Drainage of interstitial fluid from different regions of rat brain. Am J Physiol. 1984;246:F835–F844. doi: 10.1152/ajprenal.1984.246.6.F835. [DOI] [PubMed] [Google Scholar]
- 30.Johnston M, Zakharov A, Papaiconomou C, et al. Evidence of connections between cerebrospinal fluid and nasal lymphatic vessels in humans, non-human primates and other mammalian species. Cerebrospinal Fluid Res. 2004;1:2. doi: 10.1186/1743-8454-1-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Koh L, Zakharov A, Johnston M. Integration of the subarachnoid space and lymphatics: is it time to embrace a new concept of cerebrospinal fluid absorption? Cerebrospinal Fluid Res. 2005;2:6. doi: 10.1186/1743-8454-2-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Biceroglu H, Albayram S, Ogullar S, et al. Direct venous spinal reabsorption of cerebrospinal fluid: a new concept with serial magnetic resonance cisternography in rabbits. J Neurosurg Spine. 2012;16:394–401. doi: 10.3171/2011.12.SPINE11108. [DOI] [PubMed] [Google Scholar]
- 33.Murtha LA, Yang Q, Parsons MW, et al. Cerebrospinal fluid is drained primarily via the spinal canal and olfactory route in young and aged spontaneously hypertensive rats. Fluids Barriers CNS. 2014;11:12. doi: 10.1186/2045-8118-11-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kimelberg HK. Water homeostasis in the brain: basic concepts. Neuroscience. 2004;129:851–60. doi: 10.1016/j.neuroscience.2004.07.033. [DOI] [PubMed] [Google Scholar]
- 35.Redzic Z. Molecular biology of the blood-brain and the blood-cerebrospinal fluid barriers: similarities and differences. Fluids Barriers CNS. 2011;8:3. doi: 10.1186/2045-8118-8-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Oresković D, Klarica M. The formation of cerebrospinal fluid: nearly a hundred years of interpretations and misinterpretations. Brain Res Rev. 2010;64:241–62. doi: 10.1016/j.brainresrev.2010.04.006. [DOI] [PubMed] [Google Scholar]
- 37.Sathyanesan M, Girgenti MJ, Banasr M, et al. A molecular characterization of the choroid plexus and stress-induced gene regulation. Transl Psychiatry. 2012;2:e139. doi: 10.1038/tp.2012.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bulat M, Lupret V, Orehković D, Klarica M. Transventricular and transpial absorption of cerebrospinal fluid into cerebral microvessels. Coll Antropol. 2008;32(Suppl 1):43–50. [PubMed] [Google Scholar]
- 39.Orešković D, Klarica M. A new look at cerebrospinal fluid movement. Fluids Barriers CNS. 2014;11:16. doi: 10.1186/2045-8118-11-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Buishas J, Gould I, Linninger A. A computational model of cerebrospinal fluid production and reabsorption driven by starling forces. Croat Med J. 2014;0 doi: 10.3325/cmj.2014.55.481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kulik T, Kusano Y, Aronhime S. Regulation of cerebral vasculature in normal and ischemic brain. Neuropharmacology. 2008;55:281–8. doi: 10.1016/j.neuropharm.2008.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Prince E, Ahn S. Basic vascular neuroanatomy of the brain and spine: what the general interventional radiologist needs to know. Semin Intervent Radiol. 2013;30:234–9. doi: 10.1055/s-0033-1353475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zlokovic BV. Neurovascular pathways to neurodegeneration in Alzheimer's disease and other disorders. Nat Rev Neurosci. 2011;12:723–38. doi: 10.1038/nrn3114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zhang ET, Inman CB, Weller RO. Interrelationships of the pia mater and the perivascular (Virchow-Robin) spaces in the human cerebrum. J Anat. 1990;170:111–123. [PMC free article] [PubMed] [Google Scholar]
- 45.Del Zoppo GJ, Moskowitz M, Nedergaard M. The Neurovascular Unit and Responses to Ischemia. Stroke Pathophysiol. Diagnosis, Manag 2015 [Google Scholar]
- 46.Engelhardt B, Ransohoff RM. Capture, crawl, cross: the T cell code to breach the blood-brain barriers. Trends Immunol. 2012;33:579–89. doi: 10.1016/j.it.2012.07.004. [DOI] [PubMed] [Google Scholar]
- 47.Schlesinger B. The venous drainage of the brain, with special reference to the galenic system. Brain. 1939;62:274–291. doi: 10.1093/brain/62.3.274. [DOI] [Google Scholar]
- 48.Cipolla M. Anatomy and Ultrastructure. Cereb Circ 2010 [Google Scholar]
- 49.Iliff JJ, Wang M, Liao Y, et al. A paravascular pathway facilitates CSF flow through the brain parenchyma and the clearance of interstitial solutes, including amyloid β. Sci Transl Med. 2012;4:147ra111. doi: 10.1126/scitranslmed.3003748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Iliff JJ, Nedergaard M. Is there a cerebral lymphatic system? Stroke. 2013;44:S93–5. doi: 10.1161/STROKEAHA.112.678698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bradbury M, Cserr H. Drainage of cerebral interstitial fluid and of cerebrospinal fluid into lymphatics. In: Johnston M, editor. Exp Biol Lymphat Circ. Elsevier; New York, NY: 1985. pp. 355–94. [Google Scholar]
- 52.Weller RO, Subash M, Preston SD, et al. Perivascular drainage of amyloid-beta peptides from the brain and its failure in cerebral amyloid angiopathy and Alzheimer's disease. Brain Pathol. 2008;18:253–266. doi: 10.1111/j.1750-3639.2008.00133.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Carare RO, Bernardes-Silva M, Newman TA, et al. Solutes, but not cells, drain from the brain parenchyma along basement membranes of capillaries and arteries: Significance for cerebral amyloid angiopathy and neuroimmunology. Neuropathol Appl Neurobiol. 2008;34:131–144. doi: 10.1111/j.1365-2990.2007.00926.x. [DOI] [PubMed] [Google Scholar]
- 54.Hawkes C, Härtig W, Kacza J, et al. Perivascular drainage of solutes is impaired in the ageing mouse brain and in the presence of cerebral amyloid angiopathy. Acta Neuropathol. 2011;121:431–443. doi: 10.1007/s00401-011-0801-7. [DOI] [PubMed] [Google Scholar]
- 55.Bjorkhem I, Meaney S. Brain cholesterol: long secret life behind a barrier. Arter Thromb Vasc Biol. 2004;24:806–815. doi: 10.1161/01.ATV.0000120374.59826.1b. [DOI] [PubMed] [Google Scholar]
- 56.Björkhem I, Lütjohann D, Diczfalusy U, et al. Cholesterol homeostasis in human brain: turnover of 24S-hydroxycholesterol and evidence for a cerebral origin of most of this oxysterol in the circulation. J Lipid Res. 1998;39:1594–1600. [PubMed] [Google Scholar]
- 57.Lütjohann D, Breuer O, Ahlborg G, et al. Cholesterol homeostasis in human brain: evidence for an age-dependent flux of 24S-hydroxycholesterol from the brain into the circulation. Proc Natl Acad Sci U S A. 1996;93:9799–9804. doi: 10.1073/pnas.93.18.9799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Fagan AM, Holtzman DM, Munson G, et al. Unique lipoproteins secreted by primary astrocytes from wild type, apoE (-/-), and human apoE transgenic mice. J Biol Chem. 1999;274:30001–30007. doi: 10.1074/jbc.274.42.30001. [DOI] [PubMed] [Google Scholar]
- 59.Deane R, Sagare A, Hamm K, et al. apoE isoform – specific disruption of amyloid β peptide clearance from mouse brain. J Clin Invest. 2008;118:4002–4013. doi: 10.1172/JCI36663DS1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Strittmatter WJ, Saunders AM, Schmechel D, et al. Apolipoprotein E: high-avidity binding to beta-amyloid and increased frequency of type 4 allele in late-onset familial Alzheimer disease. Proc Natl Acad Sci U S A. 1993;90:1977–1981. doi: 10.1073/pnas.90.5.1977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Corder EH, Saunders AM, Strittmatter WJ, et al. Gene dose of apolipoprotein E type 4 allele and the risk of Alzheimer's disease in late onset families. Science. 1993;261:921–923. doi: 10.1126/science.8346443. [DOI] [PubMed] [Google Scholar]
- 62.Boyles JK, Pitas RE, Wilson E, et al. Apolipoprotein E associated with astrocytic glia of the central nervous system and with nonmyelinating glia of the peripheral nervous system. J Clin Invest. 1985;76:1501–1513. doi: 10.1172/JCI112130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Xu Q, Bernardo A, Walker D, et al. Profile and regulation of apolipoprotein E (ApoE) expression in the CNS in mice with targeting of green fluorescent protein gene to the ApoE locus. J Neurosci. 2006;26:4985–4994. doi: 10.1523/JNEUROSCI.5476-05.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Rangroo Thrane V, Thrane AS, Plog B, et al. Paravascular microcirculation facilitates rapid lipid transport and astrocyte signaling in the brain. Sci Rep. 2013;3:2582. doi: 10.1038/srep02582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Klose U, Strik C, Kiefer C, Grodd W. Detection of a relation between respiration and CSF pulsation with an echoplanar technique. J Magn Reson Imaging. 2000;11:438–444. doi: 10.1002/(SICI)1522-2586(200004)11:4<438∷AID-JMRI12>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- 66.Yamada S, Miyazaki M, Yamashita Y, et al. Influence of respiration on cerebrospinal fluid movement using magnetic resonance spin labeling. Fluids Barriers CNS. 2013;10:36. doi: 10.1186/2045-8118-10-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Murfee WL, Skalak TC, Peirce SM. Differential arterial/venous expression of NG2 proteoglycan in perivascular cells along microvessels: identifying a venule-specific phenotype. Microcirculation. 2005;12:151–160. doi: 10.1080/10739680590904955. [DOI] [PubMed] [Google Scholar]
- 68.Zhu X, Bergles DE, Nishiyama A. NG2 cells generate both oligodendrocytes and gray matter astrocytes. Development. 2008;135:145–157. doi: 10.1242/dev.004895. [DOI] [PubMed] [Google Scholar]
- 69.Iliff JJ, Lee H, Yu M, et al. Brain-wide pathway for waste clearance captured by contrast-enhanced MRI. J Clin Invest. 2013;123:1299–1309. doi: 10.1172/JCI67677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Iliff JJ, Wang M, Zeppenfeld DM, et al. Cerebral arterial pulsation drives paravascular CSF-interstitial fluid exchange in the murine brain. J Neurosci. 2013;33:18190–9. doi: 10.1523/JNEUROSCI.1592-13.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Schroth G, Klose U. Cerebrospinal fluid flow - I. Physiology of cardiac-related pulsation. Neuroradiology. 1992;35:1–9. doi: 10.1007/BF00588270. [DOI] [PubMed] [Google Scholar]
- 72.Stoodley MA, Brown SA, Brown CJ, Jones NR. Arterial pulsation-dependent perivascular cerebrospinal fluid flow into the central canal in the sheep spinal cord. J Neurosurg. 1997;86:686–693. doi: 10.3171/jns.1997.86.4.0686. [DOI] [PubMed] [Google Scholar]
- 73.Bilston LE, Stoodley MA, Fletcher DF. The influence of the relative timing of arterial and subarachnoid space pulse waves on spinal perivascular cerebrospinal fluid flow as a possible factor in syrinx development. J Neurosurg. 2010;112:808–813. doi: 10.3171/2009.5.JNS08945. [DOI] [PubMed] [Google Scholar]
- 74.Buzsáki G. Memory consolidation during sleep: a neurophysiological perspective. J Sleep Res. 1998;7(Suppl 1):17–23. doi: 10.1046/j.1365-2869.7.s1.3.x. doi:10.1046/j.1365-2869.7.s1.3.x, 10.1046/j.1365-2869.7.s1.3.x. [DOI] [PubMed] [Google Scholar]
- 75.Fishbein W, Gutwein BM. Paradoxical sleep and memory storage processes. Behav Biol. 1977;19:425–464. doi: 10.1016/S0091-6773(77)91903-4. [DOI] [PubMed] [Google Scholar]
- 76.Huber R, Ghilardi MF, Massimini M, Tononi G. Local sleep and learning. Nature. 2004;430:78–81. doi: 10.1038/nature02663. [DOI] [PubMed] [Google Scholar]
- 77.Tucker MA, Hirota Y, Wamsley EJ, et al. A daytime nap containing solely non-REM sleep enhances declarative but not procedural memory. Neurobiol Learn Mem. 2006;86:241–247. doi: 10.1016/j.nlm.2006.03.005. [DOI] [PubMed] [Google Scholar]
- 78.Siegel JM. Clues to the functions of mammalian sleep. Nature. 2005;437:1264–1271. doi: 10.1038/nature04285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Madsen PL, Schmidt JF, Wildschiødtz G, et al. Cerebral O2 metabolism and cerebral blood flow in humans during deep and rapid-eye-movement sleep. J Appl Physiol. 1991;70:2597–2601. doi: 10.1152/jappl.1991.70.6.2597. [DOI] [PubMed] [Google Scholar]
- 80.Xie L, Kang H, Xu Q, et al. Sleep drives metabolite clearance from the adult brain. Science. 2013;342:373–7. doi: 10.1126/science.1241224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Berridge CW, Waterhouse BD. The locus coeruleus-noradrenergic system: Modulation of behavioral state and state-dependent cognitive processes. Brain Res Rev. 2003;42:33–84. doi: 10.1016/S0165-0173(03)00143-7. [DOI] [PubMed] [Google Scholar]
- 82.O'Donnell J, Zeppenfeld D, McConnell E, et al. Norepinephrine: a neuromodulator that boosts the function of multiple cell types to optimize CNS performance. Neurochem Res. 2012;37:2496–2512. doi: 10.1007/s11064-012-0818-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Nilsson C, Lindvall-Axelsson M, Owman C. Neuroendocrine regulatory mechanisms in the choroid plexus-cerebrospinal fluid system. Brain Res Rev. 1992;17:109–138. doi: 10.1016/0165-0173(92)90011-A. [DOI] [PubMed] [Google Scholar]
- 84.Kress BT, Iliff JJ, Xia M, et al. Impairment of paravascular clearance pathways in the aging brain. Ann Neurol. 2014:1–17. doi: 10.1002/ana.24271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Sabbatini M, Barili P, Bronzetti E, et al. Age-related changes of glial fibrillary acidic protein immunoreactive astrocytes in the rat cerebellar cortex. Mech Ageing Dev. 1999;108:165–172. doi: 10.1016/s0047-6374(99)00008-1. [DOI] [PubMed] [Google Scholar]
- 86.Deane R, Zlokovic BV. Role of the blood-brain barrier in the pathogenesis of Alzheimer's disease. Curr Alzheimer Res. 2007;4:191–197. doi: 10.2174/156720507780362245. [DOI] [PubMed] [Google Scholar]
- 87.Chen RL, Kassem NA, Redzic ZB, et al. Age-related changes in choroid plexus and blood-cerebrospinal fluid barrier function in the sheep. Exp Gerontol. 2009;44:289–296. doi: 10.1016/j.exger.2008.12.004. [DOI] [PubMed] [Google Scholar]
- 88.Fleischman D, Berdahl JP, Zaydlarova J, et al. Cerebrospinal fluid pressure decreases with older age. PLoS One. 2012;7:e52664. doi: 10.1371/journal.pone.0052664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Zieman SJ, Melenovsky V, Kass DA. Mechanisms, pathophysiology, and therapy of arterial stiffness. Arter Thromb Vasc Biol. 2005;25:932–943. doi: 10.1161/01.ATV.0000160548.78317.29. [DOI] [PubMed] [Google Scholar]
- 90.Ross CA, Poirier MA. Protein aggregation and neurodegenerative disease. Nat Med. 2004;10(Suppl 1):S10–7. doi: 10.1038/nm1066. [DOI] [PubMed] [Google Scholar]
- 91.Takalo M, Salminen A, Soininen H, et al. Protein aggregation and degradation mechanisms in neurodegenerative diseases. Am J Neurodegener Dis. 2013;2:1–14. [PMC free article] [PubMed] [Google Scholar]
- 92.Frost B, Jacks RL, Diamond MI. Propagation of tau misfolding from the outside to the inside of a cell. J Biol Chem. 2009;284:12845–12852. doi: 10.1074/jbc.M808759200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Grad LI, Yerbury JJ, Turner BJ, et al. Intercellular propagated misfolding of wild-type Cu/Zn superoxide dismutase occurs via exosome-dependent and -independent mechanisms. Proc Natl Acad Sci U S A. 2014;111:3620–3625. doi: 10.1073/pnas.1312245111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Kordower JH, Chu Y, Hauser RA, et al. Lewy body-like pathology in long-term embryonic nigral transplants in Parkinson's disease. Nat Med. 2008;14:504–506. doi: 10.1038/nm1747. [DOI] [PubMed] [Google Scholar]
- 95.Li JY, Englund E, Holton JL, et al. Lewy bodies in grafted neurons in subjects with Parkinson's disease suggest host-to-graft disease propagation. Nat Med. 2008;14:501–503. doi: 10.1038/nm1746. [DOI] [PubMed] [Google Scholar]
- 96.Yamada K, Cirrito JR, Stewart FR, et al. In vivo microdialysis reveals age-dependent decrease of brain interstitial fluid tau levels in P301S human tau transgenic mice. J Neurosci. 2011;31:13110–13117. doi: 10.1523/JNEUROSCI.2569-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Palop JJ, Mucke L. Amyloid-beta-induced neuronal dysfunction in Alzheimer's disease: from synapses toward neural networks. Nat Neurosci. 2010;13:812–818. doi: 10.1038/nn.2583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Bero AW, Yan P, Roh JH, et al. Neuronal activity regulates the regional vulnerability to amyloid-beta deposition. Nat Neurosci. 2011;14:750–756. doi: 10.1038/nn.2801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Skaper SD, Evans NA, Rosin C, et al. Oligodendrocytes are a novel source of amyloid peptide generation. Neurochem Res. 2009;34:2243–2250. doi: 10.1007/s11064-009-0022-9. [DOI] [PubMed] [Google Scholar]
- 100.Guo JL, Lee VM. Seeding of normal Tau by pathological Tau conformers drives pathogenesis of Alzheimer-like tangles. J Biol Chem. 2011;286:15317–15331. doi: 10.1074/jbc.M110.209296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Jucker M, Walker LC. Pathogenic protein seeding in Alzheimer disease and other neurodegenerative disorders. Ann Neurol. 2011;70:532–540. doi: 10.1002/ana.22615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Bateman RJ, Munsell LY, Morris JC, et al. Human amyloid-beta synthesis and clearance rates as measured in cerebrospinal fluid in vivo. Nat Med. 2006;12:856–861. doi: 10.1038/nm1438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Sagare AP, Bell RD, Zlokovic BV. Neurovascular dysfunction and faulty amyloid beta-peptide clearance in Alzheimer disease. Cold Spring Harb Perspect Med. 2012 doi: 10.1101/cshperspect.a011452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Maurizi CP. Recirculation of cerebrospinal fluid through the tela choroidae is why high levels of melatonin can be found in the lateral ventricles. Med Hypotheses. 1991;35:154–158. doi: 10.1016/0306-9877(91)90041-V. [DOI] [PubMed] [Google Scholar]
- 105.Michaud JP, Bellavance MA, Prefontaine P, Rivest S. Real-time in vivo imaging reveals the ability of monocytes to clear vascular amyloid beta. Cell Rep. 2013;5:646–653. doi: 10.1016/j.celrep.2013.10.010. [DOI] [PubMed] [Google Scholar]
- 106.Ferrer I. Cognitive impairment of vascular origin: neuropathology of cognitive impairment of vascular origin. J Neurol Sci. 2010;299:139–149. doi: 10.1016/j.jns.2010.08.039. [DOI] [PubMed] [Google Scholar]
- 107.Thal DR, Grinberg LT, Attems J. Vascular dementia: different forms of vessel disorders contribute to the development of dementia in the elderly brain. Exp Gerontol. 2012;47:816–824. doi: 10.1016/j.exger.2012.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Gouw AA, Seewann A, van der Flier WM, et al. Heterogeneity of small vessel disease: a systematic review of MRI and histopathology correlations. J Neurol Neurosurg Psychiatry. 2011;82:126–135. doi: 10.1136/jnnp.2009.204685. [DOI] [PubMed] [Google Scholar]
- 109.Groeschel S, Chong WK, Surtees R, Hanefeld F. Virchow-Robin spaces on magnetic resonance images: normative data, their dilatation, and a review of the literature. Neuroradiology. 2006;48:745–754. doi: 10.1007/s00234-006-0112-1. [DOI] [PubMed] [Google Scholar]
- 110.Tournier-Lasserve E, Joutel A, Melki J, et al. Cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy maps to chromosome 19q12. Nat Genet. 1993;3:256–259. doi: 10.1038/ng0393-256. [DOI] [PubMed] [Google Scholar]
- 111.Buerge C, Steiger G, Kneifel S, et al. Lobar Dementia due to Extreme Widening of Virchow-Robin Spaces in One Hemisphere. Case Rep Neurol. 2011;3:136–140. doi: 10.1159/000329267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Roher AE, Kuo YM, Esh C, et al. Cortical and Leptomeningeal Cerebrovascular Amyloid and White Matter Pathology in Alzheimer's Disease. Mol Med. 2003;9:112–122. [PMC free article] [PubMed] [Google Scholar]
- 113.Joutel A, Corpechot C, Ducros A, et al. Notch3 mutations in CADASIL, a hereditary adult-onset condition causing stroke and dementia. Nature. 1996;383:707–710. doi: 10.1038/383707a0. [DOI] [PubMed] [Google Scholar]
- 114.Moretti L, Cristofori I, Weaver SM, et al. Cognitive decline in older adults with a history of traumatic brain injury. Lancet Neurol. 2012;11:1103–1112. doi: 10.1016/S1474-4422(12)70226-0. [DOI] [PubMed] [Google Scholar]
- 115.Plassman BL, Havlik RJ, Steffens DC, et al. Documented head injury in early adulthood and risk of Alzheimer's disease and other dementias. Neurology. 2000;55:1158–1166. doi: 10.1212/WNL.55.8.1158. [DOI] [PubMed] [Google Scholar]
- 116.Irimia A, Wang B, Aylward SR, et al. Neuroimaging of structural pathology and connectomics in traumatic brain injury: Toward personalized outcome prediction. Neuroimage Clin. 2012;1:1–17. doi: 10.1016/j.nicl.2012.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Pop V, Sorensen DW, Kamper JE, et al. Early brain injury alters the blood-brain barrier phenotype in parallel with beta-amyloid and cognitive changes in adulthood. J Cereb Blood Flow Metab. 2013;33:205–214. doi: 10.1038/jcbfm.2012.154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Shaw GJ, Jauch EC, Zemlan FP. Serum cleaved Tau protein levels and clinical outcome in adult patients with closed head injury. Ann Emerg Med. 2002;39:254–257. doi: 10.1067/mem.2002.121214. [DOI] [PubMed] [Google Scholar]
- 119.Zemlan FP, Jauch EC, Mulchahey JJ, et al. C-tau biomarker of neuronal damage in severe brain injured patients: Association with elevated intracranial pressure and clinical outcome. Brain Res. 2002;947:131–139. doi: 10.1016/S0006-8993(02)02920-7. [DOI] [PubMed] [Google Scholar]
- 120.Gabbita SP, Scheff SW, Menard RM, et al. Cleaved-tau: a biomarker of neuronal damage after traumatic brain injury. J Neurotrauma. 2005;22:83–94. doi: 10.1089/neu.2005.22.83. [DOI] [PubMed] [Google Scholar]
- 121.Iliff JJ, Chen MJ, Plog BA, et al. Impairment of glymphatic pathway function promotes tau pathology after traumatic brain injury. J Neurosci. 2014;34:16180–16193. doi: 10.1523/JNEUROSCI.3020-14.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Gaberel T, Gakuba C, Goulay R, et al. Impaired glymphatic perfusion after strokes revealed by contrast-enhanced MRI: a new target for fibrinolysis? Stroke. 2014;45:3092–3096. doi: 10.1161/STROKEAHA.114.006617. [DOI] [PubMed] [Google Scholar]
- 123.Bradbury MW, Cserr HF, Westrop RJ. Drainage of cerebral interstitial fluid into deep cervical lymph of the rabbit. Am J Physiol. 1981 doi: 10.1152/ajprenal.1981.240.4.F329. [DOI] [PubMed] [Google Scholar]
- 124.Mondello S, Muller U, Jeromin A, et al. Blood-based diagnostics of traumatic brain injuries. Expert Rev Mol Diagn. 2011;11:65–78. doi: 10.1586/erm.10.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Plog BA, Dashnaw ML, Hitomi E, et al. Biomarkers of Traumatic Injury Are Transported from Brain to Blood via the Glymphatic System. J Neurosci. 2015;35:518–26. doi: 10.1523/JNEUROSCI.3742-14.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Rennels ML, Gregory TF, Blaumanis OR, et al. Evidence for a “paravascular” fluid circulation in the mammalian central nervous system, provided by the rapid distribution of tracer protein throughout the brain from the subarachnoid space. Brain Res. 1985;326:47–63. doi: 10.1016/0006-8993(85)91383-6. [DOI] [PubMed] [Google Scholar]
- 127.Rennels ML, Blaumanis OR, Grady PA. Rapid solute transport throughout the brain via paravascular fluid pathways. Adv Neurol. 1990;52:431–439. [PubMed] [Google Scholar]
- 128.Ichimura T, Fraser P, Cserr HF. Distribution of extracellular tracers in perivascular spaces of the rat brain. Brain Res. 1991;545:103–113. doi: 10.1016/0006-8993(91)91275-6. [DOI] [PubMed] [Google Scholar]
- 129.Ball KK, Cruz NF, Mrak RE, Dienel GA. Trafficking of glucose, lactate, and amyloid-beta from the inferior colliculus through perivascular routes. J Cereb Blood Flow Metab. 2010;30:162–176. doi: 10.1038/jcbfm.2009.206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Gandhi GK, Cruz NF, Ball KK, Dienel GA. Astrocytes are poised for lactate trafficking and release from activated brain and for supply of glucose to neurons. J Neurochem. 2009;111:522–536. doi: 10.1111/j.1471-4159.2009.06333.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Ju YES, McLeland JS, Toedebusch CD, et al. Sleep quality and preclinical Alzheimer disease. JAMA Neurol. 2013;70:587–93. doi: 10.1001/jamaneurol.2013.2334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Tonsfeldt KJ, Chappell PE. Clocks on top: the role of the circadian clock in the hypothalamic and pituitary regulation of endocrine physiology. Mol Cell Endocrinol. 2012;349:3–12. doi: 10.1016/j.mce.2011.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Axelrod J. The pineal gland: a neurochemical transducer. Science. 1974;184:1341–1348. doi: 10.1126/science.184.4144.1341. [DOI] [PubMed] [Google Scholar]
- 134.Yang L, Kress BT, Weber HJ, et al. Evaluating glymphatic pathway function utilizing clinically relevant intrathecal infusion of CSF tracer. J Transl Med. 2013;11:107. doi: 10.1186/1479-5876-11-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Aydin K, Terzibasioglu E, Sencer S, et al. Localization of cerebrospinal fluid leaks by gadolinium-enhanced magnetic resonance cisternography: a 5-year single-center experience. Neurosurgery. 2008;62:584–589. doi: 10.1227/01.neu.0000317306.39203.24. [DOI] [PubMed] [Google Scholar]
- 136.Schick U, Musahl C, Papke K. Diagnostics and treatment of spontaneous intracranial hypotension. Minim Invasive Neurosurg. 2010;53:15–20. doi: 10.1055/s-0030-1247552. [DOI] [PubMed] [Google Scholar]
- 137.Lundgaard I, Li B, Xie L, et al. Direct neuronal glucose uptake heralds activity-dependent increases in cerebral metabolism. Nat Commun. 2015 doi: 10.1038/ncomms7807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Hadaczek P, Yamashita Y, Mirek H, et al. The “Perivascular Pump” Driven by Arterial Pulsation Is a Powerful Mechanism for the Distribution of Therapeutic Molecules within the Brain. Mol Ther. 2006;14:69–78. doi: 10.1016/j.ymthe.2006.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]