Abstract
Background:
There is no doubt that luteal phase support is essential to enhance the reproductive outcome in IVF cycles. In addition to progesterone and human chorionic gonadotropin, several studies have described GnRH agonists as luteal phase support to improve implantation rate, pregnancy rate and live birth rate, whereas other studies showed dissimilar conclusions. All of these studies have been done in fresh IVF cycles.
Objective:
To determine whether an additional GnRH agonist administered at the time of implantation for luteal phase support in frozen-thawed embryo transfer (FET) improves the embryo developmental potential.
Materials and Methods:
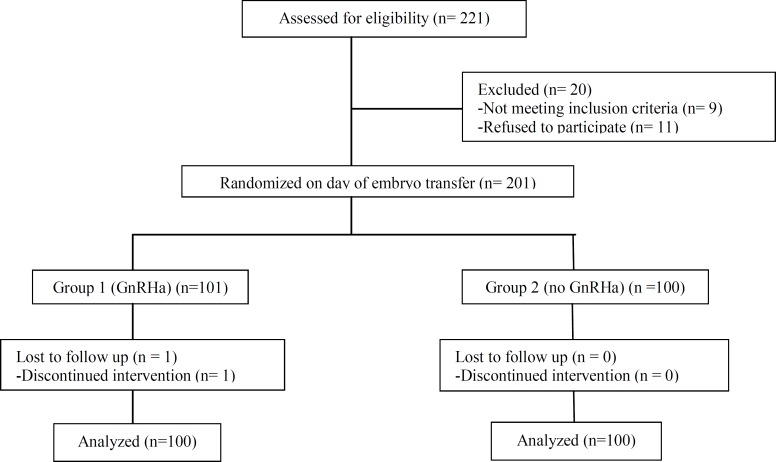
This is a prospective controlled trial study in 200 FET cycles, patients were randomized on the day of embryo transfer into group 1 (n=100) to whom a single dose of GnRH agonist (0.1 mg triptorelin) was administered three days after transfer and group 2 (n=100), who did not receive agonist. Both groups received daily vaginal progesterone suppositories plus estradiol valerate 6 mg daily. Primary outcome measure was clinical pregnancy rate. Secondary outcome measures were implantation rate, chemical, ongoing pregnancy rate and abortion rate.
Results:
A total of 200 FET cycles were analyzed. Demographic data and embryo quality were comparable between two groups. No statistically significant difference in clinical and ongoing pregnancy rates was observed between the two groups (26% versus 21%, p=0.40 and 21% versus 17%, p=0.37, respectively).
Conclusion:
Administration of a subcutaneous GnRH agonist at the time of implantation does not increase clinical or ongoing pregnancy.
Key Words: Frozen, Embryo transfer, GnRH agonist, Luteal phase
Introduction
The number of frozen-thawed embryo transfer (FET) cycles has already been increased in modern assisted reproduction treatment (ART), which partly reflects the increased use of single-embryo transfer in a fresh in vitro fertilization (IVF) cycles, and also as a result of improved laboratory techniques. Luteal phase defect is a current problem either in ART cycles due to very low Luteinizing hormone (LH) concentrations during the luteal phase in agonist and antagonist cycles and in artificial cycle FET (AC-FET), due to the lack of corpus luteum, thus support of corpus luteum function is mandatory (1-4).
Progesterone and human chorionic gonadotropin have been used as popular and effective luteal phase support (LPS) agents. In addition, estradiol and gonadotrophin-releasing hormone agonist (GnRH-a) are adjunct products offered as LPS to improve the outcome of assisted reproduction techniques (5-7).
The exact underlying mechanism of GnRH agonist is still not clear, although it has been hypothesized that GnRH agonist either supports the corpus luteum function by inducing LH secretion by the pituitary gonadotroph cells or stimulates the endometrium GnRH receptors (7, 8). The beneficial effect of GnRH agonist in the luteal phase in IVF/Intra-cytoplasmic sperm injection (ICSI) cycles on the outcome of pregnancy has also been shown in the recipients of donated oocytes (5). Currently, available data regarding the benefit of administration of GnRH agonist on pregnancy outcome in fresh ICSI cycles exist; However this is the first study regarding the frozen-thawed embryo transfer cycles (9). The aim of this study is to investigate the beneficial effect of GnRH agonist as LPS on pregnancy outcome in FET cycles.
Materials and methods
Study design
This study is a single-blind randomized clinical trial conducted at the Research and Clinical Center for Infertility, Yazd, Iran, between April 2014 to January 2015.
Tesarik, Hazout et al. showed that in egg-donation cycles, GnRH administration to recipients during the luteal phase (on day 6 after ICSI) increases the implantation rate from 25.1% to 36.9% and pregnancy rate from 54.3% to 67.4%. On the basis of this published data, the power was set at 80% and it was found that 100 cycles were needed in each group to detect this difference.
Study population
A total of 221 patients were assessed for eligibility. Exclusion criteria was patients below the age of 18 and over 40 years, oocyte recipients, patients who had systemic or endocrine disorders such as diabetes mellitus and thyroid disorders, endometriosis, submucous fibroids or intrauterine adhesions with or without history of previous surgery. Signed consent was obtained from all participants who were enrolled for randomization. This study was approved by the Ethical Committee of the Research and Clinical Center for Infertility, Yazd Iran. A computer-generated randomization table was created for the study population. Allocation concealment was ensured by the use of the day of embryo transfer.
Figure 1.
Flowchart of the study design
Patients were administered estradiol valerate 6 milligrams daily and ASA 80 mg from day 2 of the cycle, followed by daily vaginal progesterone suppositories (total dose 800 mg) since the endometrial thickness reached 8 mm. Randomization was done: group 1 (n=100) patients received 0.1 mg subcutaneous GnRHa injection (Decapepty l; Ferring, Germany) three days after embryo transfer; in group 2 (n=100), patients did not receive GnRHa. Both groups received daily progesterone suppositories (total dose 800mg), estradiol valerate 6 mg and ASA 80mg. Chemical pregnancy was diagnosed by serum β-subunit of hCG gonadotropin (β-hCG) concentration 12-14 days after embryo transfer. Clinical pregnancy was diagnosed by ultrasound detection of fetal heart activity 2 weeks after positive hCG test.
The primary outcome measure was clinical pregnancy rate and the secondary outcome measures were implantation rate, chemical pregnancy, ongoing pregnancy, and multiple pregnancy and abortion rates.
Statistical analysis
SPSS software (Statistical Package for the Social Sciences version 15.0, SPSS Inc., Chicago, IL, USA) was used for all statistical calculations. Chi-squared test and exact test was used for comparing categorical data. P<0.05 was considered statistically significant.
Results
A total of 200 patients underwent FET cycles. No significant difference was found in age, BMI, cause and duration of infertility, endometrial thickness at progesterone initiation day, number of transferred embryos and embryo score (Table I).
Table I.
Patient demographics and cycle characteristics (mean ± SD)
| Group 1 (GnRH agonist) (n=100) | Group 2 (non GnRH agonist) (n=100) | p-value | |
|---|---|---|---|
| BMI | 23.70 ±2.85 | 23.76± 2.78 | 0.89 |
| Age (years) | 30.03±5.16 | 30.08±5.21 | 0.94 |
| Duration of infertility (years) | 8.14±4.46 | 7.76±4.33 | 0.54 |
| Endometrial thickness at progesterone initiation day | 8.24±0.38 | 8.30±0.46 | 0.33 |
| Mean number of transferred embryos | 2.38±0.62 | 2.45±0.63 | 0.43 |
| Embryo score | 16.77±1.07 | 16.55±1.53 | 0.24 |
| Good quality embryos (%) | 64 | 58 | 0.21 |
Qui-square test
No significant difference was found in clinical and ongoing pregnancy rates and abortion rate between the two groups (Table II).
Table II.
Pregnancy outcome analysis in GnRHa and non-GnRHa groups
| Group 1 (GnRH agonist) (n=100) | Group 2 (non GnRH agonist) (n=100) | p-value | |
|---|---|---|---|
| Implantation rate | 14.66 | 13.07 | 0.31 |
| Chemical pregnancy rate | 27 | 27 | 1.00 |
| Clinical pregnancy rate | 26 | 21 | 0.40 |
| Ongoing pregnancy rate | 22 | 17 | 0.37 |
| Abortion rate | 5 | 8 | 0.39 |
Qui-square test
Although clinical pregnancy and ongoing pregnancy rates were slightly higher in the GnRHa group compared with the controls, the observed differences were short of reaching statistical significance.
Discussion
Several studies have described GnRH agonists as LPS to improve implantation rate, pregnancy rate and live birth rate. This study assessed the effect of a single dose of a GnRHa (0.1 mgtriptoreline) on implantation, clinical and ongoing pregnancy rates in FET cycles. No statistically significant differences in the clinical or ongoing pregnancy rates were found between two groups.
Several studies have reached similar conclusions to our study, (10). In a large randomized, study by Ata et al., (2008) one dose of GnRHa was injected 6 days after embryo transfer. No difference was found in pregnancy rate by GnRHa administration.
In another randomized study in IVF cycles with the long GnRHa protocol, three additional injections of 0.1 mg GnRHa on day 6 after embryo transfer did not affect the pregnancy rate (11).
They concluded that the continuous administration of the GnRHa in the luteal phase can lead to sustained down-regulated state of the GnRH receptors in the reproductive organs, which may cause ineffectiveness of GnRHa in improving the pregnancy rate, (12) studied the effect of continuing of GnRHa in the luteal phase on the outcome of assisted reproduction technique cycles, and found that duration did not affect the pregnancy rate. In a prospective randomized study, (Aboulghar, Marie et al. 2015) did not confirm the value of continuous administration of GnRHa for the whole luteal phase compared to much shorter durations in other studies (13).
Several studies have reported a positive effect of administration of GnRHa in the luteal phase. In a prospective randomized study, (Tesarik, Hazout et al. 2006) found a higher implantation rate and live birth rate after a single dose of 0.1 mg GnRHa administered 3 days after embryo transfer in both agonist and antagonist protocols.
The pregnancy rate, however, was not significantly improved (8). Previously, these investigators found that the administration of a single dose of GnRHa in the luteal phase increased pregnancy, implantation and live birth rates in recipients of donated oocytes in whom ovulation was suppressed and thus the corpus luteum was absent (5).
This study was more similar to ours, since preparation of egg-donated recipients resembles the frozen thawed embryo cycles. The hypothesis that a short-acting GnRH agonist administered to oocyte recipients as a single injection 6 days after ICSI will improve pregnancy outcomes excludes any possible effect on oocyte quality; thus the mechanism of the beneficial effect of luteal phase GnRH agonist administration might be explained by a direct effect on the embryo and/or on the endometrium (11, 14). Although molecular studies have suggested a direct effect of GnRHa on endometrial receptivity, current research failed to show any clinical relevant effect (15, 16). GnRH receptors are expressed at the mRNA level in vitro in cultured mouse embryos during the preimplantation period (morula to hatching blastocyst stages). In addition, it has been suggested that GnRH might play an important role on hCG synthesis and secretion either at placenta and preimplantation embryos. This is due to the fact that GnRH receptors are located not only in the trophectoderm, but also in the inner cell mass of the mouse blastocyst, (14).
There are two systematic reviews demonstrating that administration of a luteal phase single-dose GnRH agonist can significantly enhance IVF outcomes. The meta-analaysis, conducted by Kyrou, Kolibianakis et al. showed a positive effect of GnRHa on improving clinical pregnancy rate and live birth rate in both agonist and antagonist protocols. Kung, Chen et al. Confirmed in their study that a subgroup of patients with basal FSH >8 mIU/mL or mature oocytes ≤3 would benefit from luteal phase single-dose decapeptyl administration (9, 17). Yildiz, Sukur et al. (2014) compared single and sequential doses of leuprolide acetate 1 mg s.c. injections 3 and 6 days after ICSI-ET to control group following controlled ovarian stimulation (COS) with long luteal GnRH agonist protocol and resulted in higher implantation, clinical, ongoing and multiple pregnancy rates in both agonist groups (18). All available data are in fresh IVF cycles; however, this is the first prospective study designed to test this hypothesis in FET cycles which would assess the direct effect of GnRHa as the regulator of embryo-endometrial interactions and embryonic development.
Our study did not confirm the favorable effect of administration of a single dose of GnRHa in the luteal phase suggested by earlier studies (5, 19-20). In the study by Tesarik et al (2004) the mid-luteal GnRH agonist administration increased the implantation rate in an oocyte donation program in which the success rates were high even without this additional treatment. Razieh et al, (2009) did not find the possible mechanism of a single dose of GnRHa as LPS, meanwhile they believed that improvement in pregnancy rate was not related to the effect of GnRHa on the corpus luteum (20).
Larger studies are required to establish the role of GnRHa in the luteal phase especially in cases of repeated implantation failure or early pregnancy loss.
Acknowledgments
The financial supporter was Research and Clinical Center for Infertility, Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
Conflict of interest
The authors declare that there are no conflicts of interest related to the subject matter or materials discussed in this article.
References
- 1.Tavaniotou A, Albano C, Smitz J, Devroey P. Comparison of LH concentrations in the early and mid-luteal phase in IVF cycles after treatment with HMG alone or in association with the GnRH antagonist Cetrorelix. Hum Reprod. 2001;16:663–667. doi: 10.1093/humrep/16.4.663. [DOI] [PubMed] [Google Scholar]
- 2.Pritts E, Atwood A. Luteal phase support in infertility treatment: a meta-analysis of the randomized trials. Hum Reprod. 2002;17:2287–2299. doi: 10.1093/humrep/17.9.2287. [DOI] [PubMed] [Google Scholar]
- 3.Beckers N, Macklon GNS, Eijkemans MJ, Ludwig M, Felberbaum RE, Diedrich K, et al. Nonsupplemented luteal phase characteristics after the administration of recombinant human chorionic gonadotropin, recombinant luteinizing hormone, or gonadotropin-releasing hormone (GnRH) agonist to induce final oocyte maturation in in vitro fertilization patients after ovarian stimulation with recombinant follicle-stimulating hormone and GnRH antagonist cotreatment. J Clin Endocrinol Metabol. 2003;88:4186–4192. doi: 10.1210/jc.2002-021953. [DOI] [PubMed] [Google Scholar]
- 4.Daya S, Gunby J. Luteal phase support in assisted reproduction cycles. Cochrane Database Syst Rev. 2004:CD004830. doi: 10.1002/14651858.CD004830. [DOI] [PubMed] [Google Scholar]
- 5.Tesarik J, Hazout A, Mendoza C. Enhancement of embryo developmental potential by a single administration of GnRH agonist at the time of implantation. Hum Reprod. 2004;19:1176–1180. doi: 10.1093/humrep/deh235. [DOI] [PubMed] [Google Scholar]
- 6.Pirard C, Donnez J, Loumaye E. GnRH agonist as novel luteal support: results of a randomized, parallel group, feasibility study using intranasal administration of buserelin. Hum Reprod. 2005;20:1798–1804. doi: 10.1093/humrep/deh830. [DOI] [PubMed] [Google Scholar]
- 7.Pirard C, Donnez J, Loumaye E. GnRH agonist as luteal phase support in assisted reproduction technique cycles: results of a pilot study. Hum Reprod. 2006;21:1894–1900. doi: 10.1093/humrep/del072. [DOI] [PubMed] [Google Scholar]
- 8.Tesarik J, Hazout A, Mendoza-Tesarik R, Mendoza N, Mendoza C. Beneficial effect of luteal-phase GnRH agonist administration on embryo implantation after ICSI in both GnRH agonist-and antagonist-treated ovarian stimulation cycles. Hum Reprod. 2006;21:2572–2579. doi: 10.1093/humrep/del173. [DOI] [PubMed] [Google Scholar]
- 9.Kyrou D, Kolibianakis E, Fatemi H, Tarlatzi T, Devroey P, Tarlatzis B. Increased live birth rates with GnRH agonist addition for luteal support in ICSI/IVF cycles: a systematic review and meta-analysis. Hum Reprod update. 2011;17:734–740. doi: 10.1093/humupd/dmr029. [DOI] [PubMed] [Google Scholar]
- 10.Ata B, Yakin K, Balaban B, Urman B. GnRH agonist protocol administration in the luteal phase in ICSI–ET cycles stimulated with the long GnRH agonistprotocol: a randomized, controlled double blind study. Hum Reprod. 2008;23:668–673. doi: 10.1093/humrep/dem421. [DOI] [PubMed] [Google Scholar]
- 11.Inamdar DB, Majumdar A. Evaluation of the impact of gonadotropin-releasing hormone agonist as an adjuvant in luteal-phase support on IVF outcome. J of Hum Reprod Sci. 2012;5:279–284. doi: 10.4103/0974-1208.106341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Geber S, Sampaio M. Effect of duration of the GnRH agonists in the luteal phase in the outcome of assisted reproduction cycles. Gynecol Endocrinol. 2013;29:608–610. doi: 10.3109/09513590.2013.788635. [DOI] [PubMed] [Google Scholar]
- 13.Aboulghar MA, Marie H, Amin YM, Aboulghar MM, Nasr A, Serour GI, et al. Mansour. GnRH agonist plus vaginal progesterone for luteal phase support in ICSI cycles: a randomized study. Reprod Biomed Online. 2015;30:52–56. doi: 10.1016/j.rbmo.2014.09.017. [DOI] [PubMed] [Google Scholar]
- 14.Raga F, Casañ EM, Kruessel JS, Wen Y, Huang HY, Nezhat C, et al. Quantitative gonadotropin-releasing hormone gene expression and immunohistochemical localization in human endometrium throughout the menstrual cycle. Biol Reprod. 1998;59:661–669. doi: 10.1095/biolreprod59.3.661. [DOI] [PubMed] [Google Scholar]
- 15.Takeuchi S, Futamura N, Minoura H, Toyoda N. Possible direct effect of gonadotropin releasing hormone on human endometrium and decidua. Life Sci. 1998;62:1187–1194. doi: 10.1016/s0024-3205(98)00045-9. [DOI] [PubMed] [Google Scholar]
- 16.Fauser BC, Devroey P. Reproductive biology and IVF: ovarian stimulation and luteal phase consequences. Trends Endocrinol Metab. 2003;14:236–242. doi: 10.1016/s1043-2760(03)00075-4. [DOI] [PubMed] [Google Scholar]
- 17.Kung HF, Chen MJ, Guua HF, Chen YF, Yi YC, Yen-Ping Ho J, et al. Luteal phase support with decapeptyl improves pregnancy outcomes in intracytoplasmic sperm injection with higher basal follicle-stimulating hormone or lower mature oocytes. J Chin Med Assoc. 2014;77:524–530. doi: 10.1016/j.jcma.2014.07.001. [DOI] [PubMed] [Google Scholar]
- 18.Yildiz GA, Sukur YE, Ates C, Aytac R. The addition of gonadotrophin releasing hormone agonist to routine luteal phase support in intracytoplasmic sperm injection and embryo transfer cycles: a randomized clinical trial. Eur J Obstet Gynecol Reprod Biol. 2014;182:66–70. doi: 10.1016/j.ejogrb.2014.08.026. [DOI] [PubMed] [Google Scholar]
- 19.Isik AZ, Caglar GS, Sozen E, Akarsu C, Tuncay G, Ozbıcer T et al. Single-dose GnRH agonist administration in the luteal phase of GnRH antagonist cycles: a prospective randomized study. Reprod biomed online. 2009;19:472–477. doi: 10.1016/j.rbmo.2009.04.001. [DOI] [PubMed] [Google Scholar]
- 20.Dehghani Firouzabadi R, Ayazi Rozbahani M, Tabibnejad Beneficial Effect of Luteal-phase Gonadotropin-releasing Hormone Agonist Administration on Implantation Rate Afterintracytoplasmic Sperm Injection. Taiwan J Obstet Gynecol. 2009;48:245–248. doi: 10.1016/S1028-4559(09)60297-7. [DOI] [PubMed] [Google Scholar]