Abstract
Little research has addressed whether neighborhood context influences associations between fast food price, diet, and cardiometabolic health. We investigated these associations using 25 years of Coronary Artery Risk Development in Young Adults (CARDIA) study data (n=4,469, observations=21,134). We found a negative association between fast food price and consumption, with stronger inverse associations in more (vs. less) deprived neighborhoods [3rd tertile: β=−0.68 (95% CI: (−0.85, −0.51); 1st tertile: β=−0.22 (95% CI: −0.42, −0.02) ; p-interaction-0.002], and a similar association for BMI [3rd tertile: β=−1.34 (95% CI: −1.54, −1.14); 1st tertile: β=−0.45 (95% CI: −0.66, −0.25); p-interaction<0.001], but not insulin resistance [3rd tertile: β=− 0.07 (95% CI: −0.24, 0.09); 1st tertile: β=0.09 (95% CI: −0.08, 0.26); p-interaction=0.40]. We observed no modification of fast food price by fast food availability. Future research on obesity disparities should consider potential differences in the association between fast food prices and health outcomes across neighborhood socioeconomic levels.
Keywords: Fast food, food price, food environment, diet, cardiometabolic health
BACKGROUND
Although overall fast food consumption has leveled off in the past decade,[1-3] daily energy intake from fast foods remains persistently high.[2] This is problematic given that greater frequency of fast food consumption is associated with higher caloric intake, greater portion sizes, and diets high in fat, carbohydrates, and added sugars.[4-7] Fast food intake and related dietary factors are also associated with weight gain and insulin resistance,[8-10] especially among low socioeconomic status (SES) individuals.[10, 11]
In response to these changes in diet behavior and cardiometabolic risk, there is consistent evidence that higher fast food prices are associated with lower fast food consumption,[12-14] lower body mass index (BMI),[11, 15] and higher insulin resistance,[14, 16] with greater price sensitivity in low SES sub-populations.[14, 15, 17] Additionally, observational studies have demonstrated that taxes on fast food are associated with meaningful decreases in fast food consumption,[16, 18] indicating that higher fast food prices may be useful in reducing cardiometabolic disease risk.
Previous studies also suggest that characteristics of the neighborhood environment may be associated with diet and health outcomes. Higher levels of neighborhood socioeconomic deprivation have been shown to be associated with increased consumption of fast foods and decreased intake of fruits and vegetables,[19, 20] as well as increased cardiometabolic risk [21-23]. Neighborhood SES may directly or indirectly modify associations with fast food price,[24] above and beyond differences due to associations with individual-level income. For example, the associations between fast food price, diet, and cardiometabolic outcomes may differ across neighborhood SES levels due to differences in the quality and variety of fast foods and other types of foods available in neighborhoods.[24]
Similarly, greater availability of neighborhood fast food restaurants has been shown to be associated with poorer overall diet quality [25, 26], higher fast food purchasing and intake [27-31], and increased risk of diabetes and obesity [32-35], although findings are not always consistent [36-38]. It is possible that neighborhood fast food restaurant availability and community-level fast food prices may act synergistically, with poorer diet behavior and greater cardiometabolic risk for individuals residing in neighborhoods with comparatively lower fast food prices and greater access to fast food restaurants. The implications of these associations are especially relevant in neighborhoods with populations of high percent minority and low income individuals due to greater health disparities [39], and according to a recent review, where fast food restaurants may be more prevalent [40].
Although several studies have examined the association between individual-level SES with changes in FF price,[13, 14, 27] to our knowledge no studies have examined whether neighborhood-level factors modify associations among fast food price, diet behaviors, and cardiometabolic risk factors. We sought to fill this gap using longitudinal community-level food price and neighborhood environment data, with individual-level diet and clinic-based data from 25 exam years of the Coronary Artery Risk Development in Young Adults (CARDIA) study. Given that access to fast food restaurants and alternative food retail locations may differ across neighborhoods, we conceptualized fast food price as our primary exposure of interest and hypothesized that the associations between fast food prices and diet/cardiometabolic outcomes differ across levels of neighborhood SES and as a function of availability of fast food restaurants. Based on this conceptual framework, we estimate associations between community-level FF prices and fast food consumption, BMI, and homeostasis model assessment insulin resistance (HOMA-IR); and test whether these associations vary by neighborhood socioeconomic deprivation and relative neighborhood fast food restaurant availability.
METHODS
Study Sample
CARDIA is a prospective study of cardiometabolic risk factors and disease in a geographically diverse, bi-racial, young adult sample. In 1985-86, 5,115 CARDIA participants were recruited and enrolled from four US metropolitan enrollment locations (Birmingham, AL; Chicago, IL; Minneapolis, MN; Kaiser Permanente Division of Research, Oakland, CA), with balanced representation by age (18-24 y or 25-30 y), race (white or black), gender, and education (≤high school or >high school). Follow-up examinations were conducted in 1987-1988 (Year 2), 1990-1991 (Year 5), 1992-1993 (Year 7), 1995-1996 (Year 10), 2000-2001 (Year 15), 2005–2006 (Year 20), and 2010-2011 (Year 25), with retention rates of 91%, 86%, 81%, 79%, 74%, 72%, and 72%, respectively.
Residential locations were determined from geocoded home addresses at baseline and exam years 7, 10, 15, 20, and 25, and included all locations for respondents remaining within or moving outside of the original four cities. Using a Geographic Information System (GIS), we geographically- and temporally-matched community-level FF price, neighborhood-level food stores and restaurants, and US Census data to CARDIA respondents’ residential addresses.
Diet, Anthropometrics, and Insulin Resistance
Dietary practices, behaviors, and attitudes were assessed at baseline and exam years 7, 10, 15, 20, and 25. Participants were asked: “How many times in a week or month do you eat breakfast, lunch or dinner in a place such as McDonald’s, Burger King, Wendy’s, Arby’s, Pizza Hut, or Kentucky Fried Chicken?” and responses were used to calculate weekly frequency of fast food consumption.
Trained study staff measured height to the nearest 0.5 cm and weight to the nearest 0.1 kg, which were used to calculate BMI (kg/m2). Fasting blood samples of insulin and glucose were obtained via venous blood draw and used to calculate HOMA-IR [fasting glucose (mmol/L) × fasting insulin (μU/L)]/22.5],[41] with values relative to normal insulin resistance of 1.00.[42] Higher values of HOMA-IR reflect greater insulin resistance, which corresponds to a higher risk of cardiovascular disease and type 2 diabetes.[43]
C2ER Fast Food Price
Neighborhood FF price was based on a simple average of prices for hamburger (1/4 pound burger), pizza (¼ of 12-13 inch cheese, thin crust), and fried chicken (2 pieces, thigh and drumstick) purchased away-from-home. Prices were derived from the Council for Community and Economic Research (C2ER) and standardized to baseline exam year dollars using the Consumer Price Index (CPI), using a 1982-84 reference base (CPI=1.0) to account for inflation.[44] C2ER data were collected in C2ER-reporting cities, which were located in either counties or Core Based Statistical Areas (CBSAs). Using the lowest geographic level provided by C2ER (county or CBSA), we merged C2ER data to individuals by their residential location and by quarter corresponding to the CARDIA exam year when participants were seen in the clinic. If a participant’s residential location did not have matching county- or CBSA-level data (20% of respondents across all exam years), we derived population-weighted state-level means from all C2ER-reporting cities within the participant’s state. More details regarding C2ER and the creation of FF prices are available in Supplemental Appendix A.
Neighborhood Socioeconomic Deprivation Score
Using US Census and American Community Survey data from 1980, 1990, 2000, 2005-9, and 2007-11 that were geographically- and temporally-matched to CARDIA respondents at the census-tract level, we derived a neighborhood socioeconomic deprivation score using principal components analysis of: (1) percentage of population with <high school education at age 25 y; (2) percentage of population with at least a college degree at age 25 y; (3) median household income; and (4) percentage of population with household income <150% of federal poverty level.[45]. A higher score indicates higher neighborhood socioeconomic deprivation.
Availability of Neighborhood Restaurants and Food Stores
For each exam year, restaurant and food store data were obtained from the Dun & Bradstreet (D&B) Duns Market Identifiers File (Dun & Bradstreet, Inc., Short Hills, NJ),[46] a commercial data set of US businesses. D&B has fair validity and reliability,[47-49] although evidence is cross-sectional and does not address earlier exam years, due to inability to conduct retrospective ground-truthing. Restaurants and food stores were classified according to 8-digit Standard Industrial Classification (SIC) codes. At baseline, four-digit codes were used for food stores since eight-digit codes were not available for 1985-1986. Based on previous research,[27] counts of restaurants and food stores were calculated within a 3-km street network distance from respondents’ residences with the intent of capturing neighborhood fast food restaurants in close proximity to respondent residences. In the primary analysis, we characterized neighborhood fast food restaurants by calculating the percentage of fast food restaurants (chain and non-chain) relative to total food stores and restaurants to capture the relative (versus absolute) availability of fast food restaurants.[50-52]
Covariates
A standardized questionnaire was used to collect self-reported individual-level sociodemographic characteristics at each exam year, including age, gender, race (black, white), and current educational attainment (years). Income was collected at exam years 5, 7, 10, 15, 20 and 25, and recorded with categorical responses (e.g., $5000-11999/year). Population within each area was derived from US Census block-group population count, and weighted according to the proportion of block-group area within each neighborhood buffer. County-level cost-of-living (COL) from C2ER and population density (per square 3-km Euclidean residential buffer) were geographically- and temporally-matched to CARDIA respondents’ residential addresses.
Analytic Sample
Participants with at least two repeated measures for fast food meals (n=4,600), BMI (n=4,615), or HOMA-IR (n=4,385) across the 25-year study period were eligible for the current study. We excluded participants with missing income or education data (n=374), resulting in a final sample size of 4,446 participants (person-observations=17,584) for fast food consumption models, 4,469 participants (person-observations=21,134) for BMI models, and 4,332 participants (person-observations=20,126) for HOMA-IR models. Individuals in the analytic sample were not statistically different from excluded subjects, with the exception of subjects missing HOMA-IR data who were older, had higher income and education, were more likely to be white, and had higher FF prices.
Statistical Analysis
We used repeated measures fixed effects regression to quantify within-person associations between FF price and weekly frequency of fast food consumption, BMI, and HOMA-IR over the 25-year follow-up period (1985-2011). We used fixed effects to address correlation between unobserved time-invariant characteristics and our explanatory variables (e.g., residential self-selection and neighborhood-level factors), which would be unaddressed in random effects regression (which combines within- and between-person variability). In contrast, fixed effects regression controls for all measured and unmeasured time-invariant characteristics, effectively using each individual as his/her own control over the follow-up period.[53]
To assess which model type would be most appropriate, we conducted a likelihood-ratio test, which showed that a negative binomial regression model was most appropriate (restrictions of the Poisson model were not warranted, thus estimated coefficients from the Poisson model would be biased and inconsistent). Therefore, we used negative binomial regression to model associations with frequency of weekly fast food meals and linear regression to model associations with BMI and HOMA-IR in unadjusted and adjusted analyses. Based on conceptual differences in access to alternative food retail locations across neighborhoods of varying SES and the possibility of synergy between fast food price and neighborhood availability of fast food restaurants, we were specifically interested in the differential associations by neighborhood deprivation score and the percentage of neighborhood fast food restaurants relative to total food stores and restaurants; therefore, we tested for statistical interactions of these two variables with FF price in separate regression models. In all models with statistical interaction, we adjusted for time-varying age, individual-level income (coded as the midpoint of the categorical response), COL (relative to a standard of 1 from years 1982-84), and population density; we also adjusted for total food outlets (continuous) in our models to address relative availability of fast food restaurants independent of an individual’s total food retail options. Because the models we used relied solely on within-person changes, coefficients for time-invariant variables were not estimated. We also adjusted for geographic level of food price data by including an indicator variable to all analyses (1=county/CBSA-level; 2=state-level). In models testing the interaction between community-level FF prices with the relative availability of neighborhood fast food restaurants, we also adjusted for neighborhood deprivation score.
In separate analyses, we examined linearity of regressors and interaction terms by categorizing variables into tertiles and by using quadratic terms. For ease of interpretation, we categorized neighborhood deprivation score and relative availability of neighborhood fast food restaurants into low (1st), medium (2nd), and high (3rd) tertile categories based on the sample distribution [allowing sufficient representation (>42%) of blacks and whites within each tertile]. Tests using natural log-transformed HOMA-IR did not meaningfully differ from results of HOMA-IR in its natural scale; therefore, we used HOMA-IR (non-transformed) in all analyses. We used Stata (version 13.0) for all analyses (-xtreg- for linear regression and -xtnbreg- for negative binomial regression) with the “fe” option for fixed effects regression and the “margins” post-estimation command to obtain estimated marginal means and associated confidence intervals.
In sensitivity analyses, we tested for interaction by count of fast food restaurants and by percentage of chain-only neighborhood fast food restaurants (relative to total food stores and restaurants), the latter of which may be less susceptible to temporal changes in D&B coding. In our primary analysis, we used neighborhood SES adjusting for individual-level income. However, we were interested in understanding whether these results would be similar to those from models using a 3-way interaction between neighborhood SES (tertiles), individual-level income (tertiles), and FF price. We also tested for 3-way interaction by time-varying age (FF price*age*modifier) with each outcome to justify our repeated measures approach.
RESULTS
Across the 25-year study period, FF prices and self-reported frequency of weekly fast food consumption statistically significantly decreased, whereas BMI and HOMA-IR statistically significantly increased (p<0.05; Table 1). Population density, neighborhood deprivation score, and total number of food stores and restaurants statistically significantly decreased over time, while individual-level income, COL, and percentage of neighborhood fast food restaurants statistically significantly increased. The count of convenience stores were statistically significantly higher in more (versus less) socioeconomically deprived neighborhoods [3rd tertile: 22.3 (SD=15.1); 1st tertile: 15.2 (SD=17.8); p<0.001]. In unadjusted analyses, fast food price was negatively associated with fast food consumption [β=−0.14 (95% CI: −0.29, 0.01); p=0.07], BMI [β=−9.3 (95% CI: −9.7, −8.8); p<0.001], and HOMA-IR [β=−1.1 (95% CI: −1.5, −0.8); p<0.001].
TABLE 1.
Characteristics of study sample at baseline (Year 0, 1985-86) and end of follow-up (Year 25, 2010-11) a
| Characteristic | Year 0 (1985- 86) |
Year 25 (2010- 11) |
|---|---|---|
| Individual-level factors | ||
| White (%) | 49.7 | 53.1* |
| Age, years | 25.0 | 50.0 |
| Male (%) | 45.2 | 43.4* |
| Income b (%) | ||
| ≤$34,999/y | 52.1 | 19.2* |
| $35,000-74,999/y | 31.2 | 22.8 |
| ≥$75,000/y | 16.8 | 57.8 |
| Individual-level diet behaviors and cardiometabolic outcomes | ||
| Weekly visits to fast food restaurants (median (IQR)) | 1.0 (0.5, 3.0) | 0.5 (0.0, 1.4)* |
| BMI, kg/m2 (median (IQR)) | 23.5 (21.1, 26.4) |
28.7 (24.9, 33.7)* |
| HOMA-IR (median (IQR)) | 1.43 (1.13, 1.88) |
2.06 (1.19, 3.55)* |
| Community-level factors | ||
| Neighborhood fast food price c (median (IQR)) | 1.52 (1.48, 1.55) |
1.48 (1.36, 1.52)* |
| Population density d (median (IQR)) | 3,133 (1,666, 4,138) |
1,312 (636, 2,628)* |
| Cost-of-living e (median (IQR)) | 1.03 (1.00, 1.11) |
1.12 (0.94, 1.31)* |
| Socioeconomic status | ||
| Education at age 25: <HS (%) | 29.9 | 12.5* |
| Education at age 25: ≥college (%) | 22.2 | 64.7* |
| Median household income (median (IQR)) | 14,288 (10,701, 18,705) |
58,068 (41,224, 81,250)* |
| % population <150% FPL | 28.9 | 23.2* |
| Total number of food stores and restaurants (median (IQR)) | 103 (49, 204) | 93 (39, 213)* |
| Count of fast food restaurants (median (IQR)) | 14 (5, 27) | 21 (9, 40)* |
| Percentage of fast food restaurants relative to total food stores and restaurants (median (IQR)) |
12.5 (9.1, 15.6) | 20.5 (15.6, 25.3)* |
| Count of fast food restaurants (chain only) (median (IQR)) | 3 (2, 6) | 7 (3, 11)* |
| Percentage of fast food restaurants (chain only) relative to total food stores and restaurants (median (IQR)) |
2.4 (1.6, 7.7) | 5.0 (3.0, 8.6)* |
BMI, body mass index; HOMA-IR, HOMA-insulin resistance; FPL, federal poverty line; SD=standard deviation; IQR=interquartile range
Statistically significant difference from baseline values at the p<0.05 level, using one-way analysis of variance for categorical variables; paired t-test for normally distributed continuous variables; and Wilcoxon signed rank sum test for non-normally distributed continuous variables
n=4,741 participants with income, education, and food price data across CARDIA Exam Years 0-25
Values for Year 0 correspond to Year 5, as income was collected from CARDIA years 5-25 only; one-way analysis of variance (exam year 0 versus 25 values) was used for all 3 categories simultaneously (p<0.05)
Neighborhood fast food price index based on simple average of hamburger (1/4 pound (lb) burger, purchased away-from-home), pizza (¼ of 12-13 inch cheese, thin crust purchased away-from-home), and fried chicken (pieces, thigh and drumstick, purchased away-from-home) in respondents’ corresponding metropolitan statistical area (MSA); prices derived from the Council for Community and Economic Research (C2ER) and inflated to corresponding quarterly exam year dollars using the consumer price index (CPI), with a 1982-84 reference base.
Population per square kilometer
Relative to a standard of 1 from years 1982-84
Associations with fast food consumption
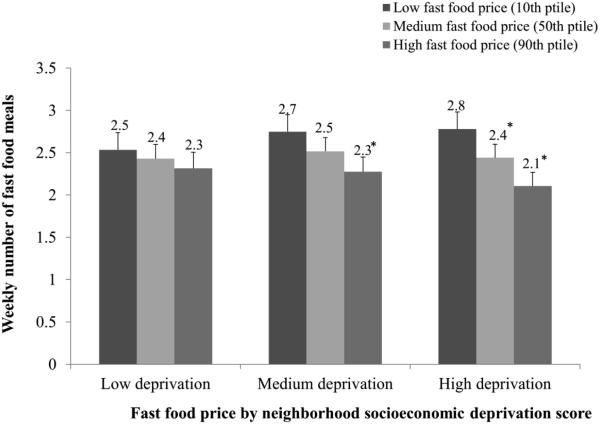
In multivariable-adjusted regression analysis, FF price was negatively associated with fast food consumption at all levels of neighborhood deprivation, with stronger inverse associations for respondents living in more compared to less socioeconomically deprived neighborhoods [3rd tertile: β=−0.68 (95% CI: (−0.85, −0.51); 1st tertile: β=−0.22 (95% CI: −0.42, −0.02); p-interaction=0.002] (Figure 1). For example, in neighborhoods of high socioeconomic deprivation, the predicted number of fast food meals/week was 2.8 (95% CI: 2.6, 3.0) at low FF prices (10th percentile), whereas the predicted mean fast food meals/week was 2.1 (95% CI: 1.9, 2.3) at high FF prices (90th percentile) (Table 2). Conversely, in neighborhoods with low socioeconomic deprivation the comparable frequency of fast food meals/week was 2.5 (95% CI: 2.3, 2.7) at the 10th percentile of FF price versus 2.3 (95% CI: 2.1, 2.5) meals/week at the 90th percentile.
FIGURE 1.
Adjusted meansa of weekly fast food meals at the 10th, 50th, and 90th percentiles of community-level fast food priceb and low, medium, and high tertile categories of neighborhood socioeconomic deprivation scorec, (CARDIA Exam Years 0-25)
Note: Higher neighborhood socioeconomic deprivation score reflects higher neighborhood deprivation (i.e., +1SD = highest deprivation)
* Indicates that weekly fast food consumption is statistically significantly different than referent (1th percentile of fast food consumption), within neighborhood deprivation tertile.
a Adjusted means of weekly fast food meals derived from pooled negative binomial regression models with fixed-effects (based on coefficients from Table 2, row (a))
b The 10th, 50th, and 90th percentiles of community-level fast food price are $1.27, $1.40, and $1.54, respectively
c Models were adjusted for time-varying age, income ($/yr), and community-level cost of living, and population density (pop/km2); because fixed effects models rely on within-person variation, coefficients for time-constant variables (study center, education, race, sex) were not estimated
TABLE 2.
Predicted multivariable-adjusted a marginal values b for the associations between community-level fast food price c and weekly fast food consumption, BMI, and HOMA-IR (from separate models) and their interaction with (a) neighborhood socioeconomic deprivation score, and (b) percentage of fast food restaurants (relative to total food stores and restaurants), (CARDIA Exam Years 0-25) d
| Weekly fast food meals (95% CI) |
BMI (kg/m2) (95% CI) |
HOMA-IR (95% CI) |
|
|---|---|---|---|
|
(a) Neighborhood deprivation score
(tertiles)e |
|||
| Low neighborhood deprivation score | |||
| Low fast food price (10th percentile) | 2.5 (2.3, 2.7) | 27.9 (27.8, 28.1) |
2.29 (2.17, 2.41) |
| Medium fast food price (50th percentile) | 2.4 (2.3, 2.6) | 27.7 (27.6, 27.8) |
2.33 (2.26, 2.41) |
| High fast food price (90th percentile) | 2.3 (2.1, 2.5) | 27.5 (27.3, 27.6) |
2.38 (2.27, 2.49) |
|
Medium neighborhood deprivation
score |
|||
| Low fast food price (10th percentile) | 2.7 (2.5, 2.9) | 28.0 (27.9, 28.2) |
2.44 (2.34, 2.55) |
| Medium fast food price (50th percentile) | 2.5 (2.4, 2.7) | 27.6 (27.6, 27.7) |
2.44 (2.38, 2.51) |
| High fast food price (90th percentile) | 2.3 (2.1, 2.4) | 27.2 (27.1, 27.3) |
2.44 (2.33, 2.55) |
| High neighborhood deprivation score | |||
| Low fast food price (10th percentile) | 2.8 (2.6, 3.0) | 28.2 (28.0, 28.3) |
2.31 (2.20, 2.42) |
| Medium fast food price (50th percentile) | 2.4 (2.3, 2.6) | 27.5 (27.4, 27.6) |
2.27 (2.19, 2.35) |
| High fast food price (90th percentile) | 2.1 (1.9, 2.3) | 26.8 (26.7, 27.0) |
2.23 (2.11, 2.35) |
|
(b) Percentage of neighborhood fast
food restaurants (tertiles) f |
|||
| Low percentage of fast food restaurants | |||
| Low fast food price (10th percentile) | 2.7 (2.5, 2.9) | 28.0 (27.9, 28.1) |
2.34 (2.25, 2.44) |
| Medium fast food price (50th percentile) | 2.5 (2.3, 2.6) | 27.7 (27.6, 27.7) |
2.39 (2.32, 2.45) |
| High fast food price (90th percentile) | 2.3 (2.1, 2.4) | 27.3 (27.1, 27.4) |
2.43 (2.32, 2.55) |
|
Medium percentage of fast food
restaurants |
|||
| Low fast food price (10th percentile) | 2.7 (2.5, 2.9) | 28.1 (28.0, 28.3) |
2.33 (2.23, 2.43) |
| Medium fast food price (50th percentile) | 2.4 (2.3, 2.6) | 27.7 (27.6, 27.7) |
2.33 (2.26, 2.39) |
| High fast food price (90th percentile) | 2.2 (2.0, 2.3) | 27.2 (27.1, 27.3) |
2.32 (2.21, 2.43) |
| High percentage of fast food restaurants | |||
| Low fast food price (10th percentile) | 2.8 (2.6, 3.0) | 28.0 (27.9, 28.2) |
2.40 (2.29, 2.50) |
| Medium fast food price (50th percentile) | 2.5 (2.3, 2.6) | 27.6 (27.5, 27.7) |
2.36 (2.29, 2.43) |
| High fast food price (90th percentile) | 2.2 (2.0, 2.3) | 27.1 (26.9, 27.2) |
2.31 (2.20, 2.43) |
Models were adjusted for time-varying age, individual-level income (units of $10,000 from midpoint of category), cost of living (relative to a standard of 1 from years 1982-84), population density (pop/km2), total food outlets (continuous), geographic level of food price data (1=county/CBSA-level; 2=state-level), neighborhood deprivation score (only for models in (b)).
Marginal values derived from pooled negative binomial and linear regression models with fixed-effects
Population-averaged values for the 10th, 50th, and 90th percentiles of community-level fast food price were equal to $1.27, $1.40, $1.54, respectively (pooled CARDIA Exam Years 0-25)
n=4,446 participants (fast food consumption models), 4,469 participants (BMI models), and 4,332 participants (HOMA-IR models) with at least two repeated outcome measures and no income or education data across CARDIA Exam Years 0, 7, 10, 15, 20, and 25
PCA-derived factor score of four census tract-level variables: (1) percentage of population with <high school education at age 25 y; (2) percentage of population with at least a college degree at age 25 y; (3) median household income; and (4) percentage of population with household income <150% of federal poverty level.[32]
Relative to total food stores and restaurants (within 3-km network buffer of respondent residence)
In contrast, the relative availability of neighborhood fast food restaurants did not significantly modify the association between FF price and fast food consumption [3rd tertile: β=−0.60 (95% CI: =0.80, −0.40); 1st tertile: β=−0.41 (95% CI: −0.58, −0.23); p-interaction=0.26]. The frequency of fast food meals/week at higher FF prices was similar in the lowest and highest tertiles of relative availability of neighborhood fast food restaurants (Table 2).
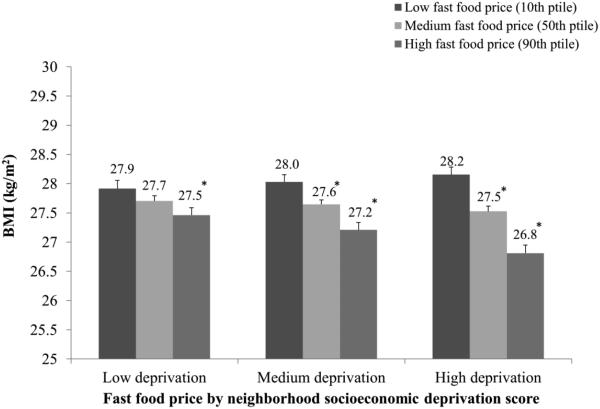
Associations with BMI
After adjustment for covariates, higher FF price was negatively associated with BMI at all levels of neighborhood deprivation, with a stronger inverse association in neighborhoods with high versus low socioeconomic deprivation [3rd tertile: β=−1.34 (95% CI: −1.54, −1.14); 1st tertile: β=−0.45 (95% CI: −0.66, −0.25); p-interaction<0.001] (Figure 2). In neighborhoods with high socioeconomic deprivation, the predicted BMI at higher FF prices (90th percentile) was 26.8 (95% CI: 26.7, 27.0) kg/m2, whereas the predicted BMI at lower FF prices (10th percentile) was 28.2 (95% CI: 28.0, 28.3) kg/m2. In neighborhoods with low socioeconomic deprivation, the predicted BMI was 27.5 (95% CI: 27.3, 27.6) kg/m2 at the 10th percentile of FF price versus 27.9 (95% CI: 27.8, 28.1) kg/m2 at the 90th percentile (Table 2).
FIGURE 2.
Adjusted meansa of BMI (kg/m2) at the 10th, 50th, and 90th percentiles of community-level fast food priceb and low, medium, and high tertile categories of neighborhood socioeconomic deprivation scorec, (CARDIA Exam Years 0-25)
Note: Higher neighborhood socioeconomic deprivation score reflects higher neighborhood deprivation (i.e., +1SD = highest deprivation)
* Indicates that BMI value is statistically significantly different than referent (10th percentile of fast food consumption)
a Adjusted means derived from pooled linear regression models with fixed-effects (based on coefficients from Table 2, row (a))
b The 10th, 50th, and 90th percentiles of community-level fast food price are $1.27, $1.40, and $1.54, respectively
c Models were adjusted for time-varying age, income ($/yr), and community-level cost of living, and population density (pop/km2); because fixed effects models rely on within-person variation, coefficients for time-constant variables (study center, education, race, sex) were not estimated
We did not observe statistically significant differences in the association between FF price and BMI by relative fast food restaurant availability [3rd tertile: β==0.96 (95% CI: −1.17, −0.75); 1st tertile: β=−0.74 (95% CI: −0.94, −0.55); p-interaction=0.22]. BMI values at higher FF prices were similar in the lowest and highest tertiles of relative availability of neighborhood fast food restaurants (Table 2).
Associations with HOMA-IR
Associations between FF price and HOMA-IR were negative although not statistically significant (Supplemental Table 1). Nor were there statistically significant interactions between FF price and HOMA-IR by neighborhood deprivation [3rd tertile: β=−0.07 (95% CI: −0.24, 0.09); 1st tertile: β=0.09 (95% CI: −0.08, 0.26); p-interaction=0.40] or relative availability of neighborhood fast food restaurant [3rd tertile: β=−0.08 (95% CI: −0.26, −0.10 ); 1st tertile: β=0.09 (95% CI: −0.08, 0.26); p-interaction=0.35].
Sensitivity Analyses
In multivariable-adjusted models, we tested whether associations with the relative availability of chain-only neighborhood fast food restaurants were similar to model results with relative availability of both chain and non-chain fast food restaurants. Similarly, we tested whether an absolute measure, the count of total fast food restaurants (chain and non-chain), influenced any of the associations with FF price. Neither the relative availability of chain-only neighborhood fast food restaurants nor the count of total fast food restaurants significantly modified the associations with any of the outcomes.
In sensitivity models, we tested whether associations in models using an interaction of neighborhood SES with individual-level income were similar to those using only neighborhood SES in the primary analysis. This sensitivity analysis suggested that the interaction of neighborhood SES by individual-level SES did not statistically significantly modify the associations between FF price and fast food consumption (p-interaction=0.98), BMI (p-interaction=0.11), or HOMA-IR (p-interaction=0.44). Finally, the interaction term for age by FF price by neighborhood deprivation score (or availability of fast food restaurants) was not statistically significant in any model, justifying our repeated measures approach.
DISCUSSION
Using over 25 years of population-based, prospective data, we tested whether neighborhood-level factors modified associations between community-level FF price and individual-level fast food consumption, BMI, and HOMA-IR. We observed negative associations with fast food consumption at all levels of neighborhood socioeconomic deprivation, with stronger inverse associations for those living in more (vs. less) socioeconomically deprived neighborhoods. In addition, higher community-level FF prices were more strongly inversely associated with BMI in more (vs. less) socioeconomically deprived neighborhoods. In contrast, we found no evidence of statistical modification by relative availability of neighborhood fast food restaurants, which we hypothesized would act synergistically with FF prices in association with diet and cardiometabolic outcomes.
In our earlier work, we found that associations with FF prices also varied by individual-level sociodemographic characteristics.[12, 14, 27] For example, Meyer et al. found greater fast food price sensitivity among blacks (vs. whites) and among participants with lower (vs. higher) education,[14] while others found a relatively stronger association between fast food prices and fast food intake in males and low-income participants in the CARDIA study.[12, 27] Our study provides new evidence that the associations between fast food price, diet, and BMI may be relatively stronger in individuals from low SES neighborhoods, after accounting for individual-level SES. It is possible that individuals evaluate the prices of foods in relation to the full retail environment and meal options.[24] Residents of low SES neighborhoods may have differential access to alternative retail locations, despite having equal exposure to fast food restaurants. For example, we observed a statistically significantly higher count of convenience stores in low (versus high) SES neighborhoods. As a result, residents of low SES neighborhoods may have more retail options from which to purchase inexpensive, energy-dense foods to replace fast food meals.
Our study also provides evidence that the influence of FF price does not differ by relative availability of neighborhood fast food restaurants. Contrary to our expectations, we did not observe a relatively stronger association between FF price and health outcomes in neighborhoods with a higher (versus lower) relative availability of fast food restaurants. Although the supply of fast food restaurants in a neighborhood may govern fast food prices at the market level, differential access to fast food restaurants may not influence the individual’s purchasing behavior once food prices are taken into account. Alternatively, differences in the estimated effect of FF price on fast food consumption, BMI, and HOMA-IR may be shaped by the full retail choice set, not just the availability of fast food restaurants. Our findings suggest that community-level FF price may be meaningful in neighborhoods across the spectrum of access to fast food restaurants. We did not observe statistically significant associations between FF availability and price with HOMA-IR score in any of our models, thus suggesting the role of other factors influencing insulin resistance.
To our knowledge, ours is the first study to examine the differential associations among FF price, diet, and health outcomes by neighborhood SES and neighborhood fast food restaurant availability. Although a few studies have included neighborhood-level measures in their analyses,[13, 15] these studies did not explicitly address modification by neighborhood food outlet availability or neighborhood SES. It is important to consider heterogeneity by neighborhood factors in order to achieve more consistent results across studies. Furthermore, these studies were limited by their focus on children, whereas we followed young adults to middle and late adulthood.
Our study has many strengths, including the use of a bi-racial, population-based cohort of young adults. Compared to the numerous existing cross-sectional studies, our study provides a longitudinal perspective on associations with fast food price, allowing us to quantify within-person effects with fixed effects regression and thus control for unmeasured factors, such as preferences for certain types of residential neighborhoods to the extent that such preferences are stable over time. Furthermore, we used comprehensive, theoretically-relevant measures of the socioeconomic and food environment domains, including a composite score of neighborhood deprivation as well as a relative measure of the food environment. Although the literature suggests that the relative composition of the food environment may be more meaningfully predictive of dietary behavior than absolute numbers of food outlets,[51, 52] we did not observe meaningful differences between the two measures in our study.
Our study also has several limitations. Although questions about dietary practices were administered by trained interviewers and previously validated,[54] self-reported measures are vulnerable to recall bias and reporting error.[55] The questionnaire also did not capture the specific food items purchased and consumed by participants; thus, our measure does not reflect specific foods consumed. Similarly, the C2ER food price data may not reflect the cost of actual fast food purchased by CARDIA participants. Although our food price data were assigned to participants at the smallest geographic unit possible (e.g., county-level), the C2ER data do not capture variability in price estimates within neighborhoods. However, the C2ER data are the only data available that provide information on food prices in the U.S. over the past 30 years, with broad coverage of metropolitan and non-metropolitan markets.[56] Despite differences in the precision of price data obtained from C2ER-reporting cities located within counties/CBSAs versus population-weighted state-level means, we expect that any such measurement error is likely to attenuate our results, especially with adjustment for geographic level of price data in our models. We were also unable to examine dietary substitution of energy from fast food meals with other nutrient-poor foods in response to changes in FF price. Finally, our findings may only be generalizable to urban areas in the U.S.
Overall, our findings suggest a differential association between FF price with fast food consumption and with BMI by neighborhood SES, but not by relative availability of neighborhood fast food restaurants. In socioeconomically deprived neighborhoods, we observed modest changes in fast food intake, as well as a comparatively stronger association between FF price and BMI, which suggests that the potential effectiveness of strategies to modify the economic environment (e.g., fast food taxes) may depend on neighborhood context. Natural experiments to examine changes in neighborhood FF prices and subsequent diet and food purchasing behaviors could be useful future directions, especially in socioeconomically deprived neighborhoods.
Supplementary Material
Highlights.
Examined associations between fast food price, diet and cardiometabolic health.
Observed stronger inverse associations with diet in more (vs. less) deprived areas.
Observed similar associations with weight status, but not insulin resistance.
Relative availability of fast food restaurants did not influence any associations.
Fast food price may be a target for future disparities research.
ACKNOWLEDGMENTS
The authors would like to acknowledge CARDIA Chief Reviewer Janne Boone-Heinonen, PhD, whose thoughtful suggestions improved the paper, as well as Marc Peterson, of the University of North Carolina, Carolina Population Center (CPC) and the CPC Spatial Analysis Unit for creation of the environmental variables. Pasquale E. Rummo, MPH had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of data analysis.
FUNDING
This work was funded by the National Heart, Lung, and Blood Institute (NHLBI) R01HL104580. The Coronary Artery Risk Development in Young Adults Study (CARDIA) is supported by contracts HHSN268201300025C, HHSN268201300026C, HHSN268201300027C, HHSN268201300028C, HHSN268201300029C, and HHSN268200900041C from the NHLBI, the Intramural Research Program of the National Institute on Aging (NIA), and an intra-agency agreement between NIA and NHLBI (AG0005). The authors are grateful to the Carolina Population Center, University of North Carolina at Chapel Hill, for general support (grant R24 HD050924 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development [NICHD]), the Nutrition Obesity Research Center (NORC), University of North Carolina (grant P30DK56350 from the National Institute for Diabetes and Digestive and Kidney Diseases [NIDDK]), and to the Center for Environmental Health Sciences (CEHS), University of North Carolina (grant P30ES010126 from the National Institute for Environmental Health Sciences [NIEHS]). NIH had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
COMPETING INTERESTS
The authors have no financial or other conflicts of interest to disclose.
CONTRIBUTOR STATEMENT
Pasquale E. Rummo, MPH had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Rummo, Meyer, Howard, Shikany, Guilkey, Gordon-Larsen.
Acquisition of data: Shikany, Gordon-Larsen.
Analysis and interpretation of data: Rummo, Meyer, Howard, Shikany, Guilkey, Gordon-Larsen.
Drafting of the manuscript: Rummo, Gordon-Larsen.
Critical revision of the manuscript for important intellectual content: Meyer, Howard, Shikany, Guilkey, Gordon-Larsen.
Statistical analysis: Rummo, Meyer, Howard, Guilkey.
Obtained funding: Gordon-Larsen.
Final approval of the version to be published: Gordon-Larsen.
Study supervision: Gordon-Larsen.
HUMAN PARTICIPANT PROTECTION
Written consent and study data were collected under protocols approved by Institutional Review Boards at each study center: University of Alabama at Birmingham, Northwestern University, University of Minnesota, and Kaiser Permanente. Geographic linkage and analysis for the current study was approved by the Institutional Review Board at the University of North Carolina at Chapel Hill.
Contributor Information
Penny Gordon-Larsen, Department of Nutrition, University of North Carolina at Chapel Hill, Carolina Population Center, 137 East Franklin Street, 6th floor, Campus Box #8120, Chapel Hill, NC 27514.
Pasquale E. Rummo, Department of Nutrition, University of North Carolina at Chapel Hill, Carolina Population Center, Chapel Hill, NC, USA, prummo@live.unc.edu
Katie A. Meyer, Department of Nutrition, University of North Carolina at Chapel Hill, Carolina Population Center, Chapel Hill, NC, USA, ktmeyer@email.unc.edu
Annie Green Howard, Department of Nutrition, University of North Carolina at Chapel Hill, Carolina Population Center, Chapel Hill, NC, USA, aghoward@email.unc.edu.
James M. Shikany, Division of Preventive Medicine, University of Alabama at Birmingham, Birmingham, AL, USA, jshikany@uabmc.edu
David K. Guilkey, Department of Economics, University of North Carolina at Chapel Hill, Carolina Population Center, Chapel Hill, NC, USA, david_guilkey@unc.edu
REFERENCES
- 1.Larson N, et al. Secular trends in fast-food restaurant use among adolescents and maternal caregivers from 1999 to 2010. Am J Public Health. 2014;104:e62–9. doi: 10.2105/AJPH.2013.301805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Powell LM, Nguyen BT, Han E. Energy intake from restaurants: demographics and socioeconomics, 2003-2008. Am J Prev Med. 2012;43:498–504. doi: 10.1016/j.amepre.2012.07.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Smith LP, Ng SW, Popkin BM. Trends in US home food preparation and consumption: analysis of national nutrition surveys and time use studies from 1965-1966 to 2007-2008. Nutr J. 2013;12:45. doi: 10.1186/1475-2891-12-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pereira MA, et al. Fast-food habits, weight gain, and insulin resistance (the CARDIA study): 15-year prospective analysis. Lancet. 2005;365:36–42. doi: 10.1016/S0140-6736(04)17663-0. [DOI] [PubMed] [Google Scholar]
- 5.Poti JM, Popkin BM. Trends in energy intake among US children by eating location and food source, 1977-2006. J Am Diet Assoc. 2011;111:1156–64. doi: 10.1016/j.jada.2011.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Powell LM, Nguyen BT. Fast-food and full-service restaurant consumption among children and adolescents: effect on energy, beverage, and nutrient intake. JAMA Pediatr. 2013;167:14–20. doi: 10.1001/jamapediatrics.2013.417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rosenheck R. Fast food consumption and increased caloric intake: a systematic review of a trajectory towards weight gain and obesity risk. Obesity Reviews. 2008;9:535–547. doi: 10.1111/j.1467-789X.2008.00477.x. [DOI] [PubMed] [Google Scholar]
- 8.Deer J, et al. Dietary models of insulin resistance. Metabolism. 2015;64:163–171. doi: 10.1016/j.metabol.2014.08.013. [DOI] [PubMed] [Google Scholar]
- 9.Duffey KJ, et al. Regular consumption from fast food establishments relative to other restaurants is differentially associated with metabolic outcomes in young adults. The Journal of nutrition. 2009;139:2113–2118. doi: 10.3945/jn.109.109520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pereira MA, et al. Fast-food habits, weight gain, and insulin resistance (the CARDIA study): 15-year prospective analysis. The Lancet. 2005;365:36–42. doi: 10.1016/S0140-6736(04)17663-0. [DOI] [PubMed] [Google Scholar]
- 11.Powell LM, Nguyen BT. Fast-food and full-service restaurant consumption among children and adolescents: effect on energy, beverage, and nutrient intake. JAMA pediatrics. 2013;167:14–20. doi: 10.1001/jamapediatrics.2013.417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gordon-Larsen P, Guilkey DK, Popkin BM. An economic analysis of community-level fast food prices and individual-level fast food intake: a longitudinal study. Health Place. 2011;17:1235–41. doi: 10.1016/j.healthplace.2011.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Khan T, Powell LM, Wada R. Fast food consumption and food prices: evidence from panel data on 5th and 8th grade children. J Obes. 2012;2012:857697. doi: 10.1155/2012/857697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Meyer KA, et al. Sociodemographic differences in fast food price sensitivity. JAMA internal medicine. 2014;174:434–442. doi: 10.1001/jamainternmed.2013.13922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Powell LM, Bao Y. Food prices, access to food outlets and child weight. Econ Hum Biol. 2009;7:64–72. doi: 10.1016/j.ehb.2009.01.004. [DOI] [PubMed] [Google Scholar]
- 16.Duffey KJ, et al. Food price and diet and health outcomes: 20 years of the CARDIA Study. Archives of internal medicine. 2010;170:420–426. doi: 10.1001/archinternmed.2009.545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Powell LM. Fast food costs and adolescent body mass index: evidence from panel data. J Health Econ. 2009;28:963–70. doi: 10.1016/j.jhealeco.2009.06.009. [DOI] [PubMed] [Google Scholar]
- 18.Khan T, Powell LM, Wada R. Fast food consumption and food prices: evidence from panel data on 5th and 8th grade children. Journal of obesity. 2012;2012 doi: 10.1155/2012/857697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Carroll-Scott A, et al. Disentangling neighborhood contextual associations with child body mass index, diet, and physical activity: the role of built, socioeconomic, and social environments. Soc Sci Med. 2013;95:106–14. doi: 10.1016/j.socscimed.2013.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Utter J, et al. Socio-economic differences in eating-related attitudes, behaviours and environments of adolescents. Public Health Nutr. 2011;14:629–34. doi: 10.1017/S1368980010001898. [DOI] [PubMed] [Google Scholar]
- 21.Dubowitz T, et al. The Women's Health Initiative: The food environment, neighborhood socioeconomic status, BMI, and blood pressure. Obesity (Silver Spring) 2012;20:862–71. doi: 10.1038/oby.2011.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ford PB, Dzewaltowski DA. Neighborhood deprivation, supermarket availability, and BMI in low-income women: a multilevel analysis. J Community Health. 2011;36:785–96. doi: 10.1007/s10900-011-9377-3. [DOI] [PubMed] [Google Scholar]
- 23.Laraia BA, et al. Place matters: neighborhood deprivation and cardiometabolic risk factors in the Diabetes Study of Northern California (DISTANCE) Soc Sci Med. 2012;74:1082–90. doi: 10.1016/j.socscimed.2011.11.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Black JL, Macinko J. Neighborhoods and obesity. Nutrition Reviews. 2008;66:2–20. doi: 10.1111/j.1753-4887.2007.00001.x. [DOI] [PubMed] [Google Scholar]
- 25.He M, et al. Obesogenic neighbourhoods: the impact of neighbourhood restaurants and convenience stores on adolescents' food consumption behaviours. Public Health Nutr. 2012;15:2331–9. doi: 10.1017/S1368980012000584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Moore LV, et al. Fast-food consumption, diet quality, and neighborhood exposure to fast food: the multi-ethnic study of atherosclerosis. Am J Epidemiol. 2009;170:29–36. doi: 10.1093/aje/kwp090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Boone-Heinonen J, et al. Fast food restaurants and food stores: longitudinal associations with diet in young to middle-aged adults: the CARDIA study. Arch Intern Med. 2011;171:1162–70. doi: 10.1001/archinternmed.2011.283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Duffey KJ, et al. Differential associations of fast food and restaurant food consumption with 3-y change in body mass index: the Coronary Artery Risk Development in Young Adults Study. Am J Clin Nutr. 2007;85:201–8. doi: 10.1093/ajcn/85.1.201. [DOI] [PubMed] [Google Scholar]
- 29.He M, et al. The influence of local food environments on adolescents' food purchasing behaviors. Int J Environ Res Public Health. 2012;9:1458–71. doi: 10.3390/ijerph9041458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Laxer RE, Janssen I. The proportion of excessive fast-food consumption attributable to the neighbourhood food environment among youth living within 1 km of their school. Appl Physiol Nutr Metab. 2014;39:480–6. doi: 10.1139/apnm-2013-0208. [DOI] [PubMed] [Google Scholar]
- 31.Burgoine T, et al. Associations between exposure to takeaway food outlets, takeaway food consumption, and body weight in Cambridgeshire, UK: population based, cross sectional study. BMJ. 2014;348 doi: 10.1136/bmj.g1464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bodor JN, et al. The association between obesity and urban food environments. J Urban Health. 2010;87:771–81. doi: 10.1007/s11524-010-9460-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kruger DJ, et al. Local Concentration of Fast Food Outlets Is Associated with Poor Nutrition and Obesity. Am J Health Promot. 2013 doi: 10.4278/ajhp.111201-QUAN-437. [DOI] [PubMed] [Google Scholar]
- 34.Li F, et al. Obesity and the built environment: does the density of neighborhood fast-food outlets matter? Am J Health Promot. 2009;23:203–9. doi: 10.4278/ajhp.071214133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Miura K, Turrell G. Reported consumption of takeaway food and its contribution to socioeconomic inequalities in body mass index. Appetite. 2014;74:116–124. doi: 10.1016/j.appet.2013.12.007. [DOI] [PubMed] [Google Scholar]
- 36.Richardson AS, et al. Neighborhood fast food restaurants and fast food consumption: a national study. BMC Public Health. 2011;11:543. doi: 10.1186/1471-2458-11-543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lamichhane AP, et al. Associations of built food environment with dietary intake among youth with diabetes. J Nutr Educ Behav. 2012;44:217–24. doi: 10.1016/j.jneb.2011.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Thornton LE, Bentley RJ, Kavanagh AM. Fast food purchasing and access to fast food restaurants: a multilevel analysis of VicLANES. Int J Behav Nutr Phys Act. 2009;6:28. doi: 10.1186/1479-5868-6-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Reitzel LR, et al. Density and proximity of fast food restaurants and body mass index among African Americans. Am J Public Health. 2014;104:110–6. doi: 10.2105/AJPH.2012.301140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fleischhacker SE, et al. A systematic review of fast food access studies. Obes Rev. 2011;12:e460–71. doi: 10.1111/j.1467-789X.2010.00715.x. [DOI] [PubMed] [Google Scholar]
- 41.Matthews DR, et al. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–9. doi: 10.1007/BF00280883. [DOI] [PubMed] [Google Scholar]
- 42.Wallace TM, Levy JC, Matthews DR. Use and abuse of HOMA modeling. Diabetes care. 2004;27:1487–1495. doi: 10.2337/diacare.27.6.1487. [DOI] [PubMed] [Google Scholar]
- 43.Ginsberg HN. Insulin resistance and cardiovascular disease. Journal of Clinical Investigation. 2000;106:453–458. doi: 10.1172/JCI10762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bureau of Labor Statistics Consumer Price Index. Access Date: December 2014. Available from: http://www.bls.gov/cpi/
- 45.Messer LC, et al. The development of a standardized neighborhood deprivation index. J Urban Health. 2006;83:1041–62. doi: 10.1007/s11524-006-9094-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.D&B - Dun's Market Identifiers. Dun & Bradstreet, Inc.; 2013. [Google Scholar]
- 47.Fleischhacker SE, et al. Validity of secondary retail food outlet data: a systematic review. American journal of preventive medicine. 2013;45:462–473. doi: 10.1016/j.amepre.2013.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Han E, et al. Classification bias in commercial business lists for retail food stores in the US. Int J Behav Nutr Phys Act. 2012;9:46. doi: 10.1186/1479-5868-9-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Liese AD, et al. Validation of 3 food outlet databases: completeness and geospatial accuracy in rural and urban food environments. American Journal of Epidemiology. 2010;172:1324–1333. doi: 10.1093/aje/kwq292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mason KE, Bentley RJ, Kavanagh AM. Fruit and vegetable purchasing and the relative density of healthy and unhealthy food stores: evidence from an Australian multilevel study. J Epidemiol Community Health. 2013;67:231–6. doi: 10.1136/jech-2012-201535. [DOI] [PubMed] [Google Scholar]
- 51.Spence JC, et al. Relation between local food environments and obesity among adults. BMC Public Health. 2009;9:192. doi: 10.1186/1471-2458-9-192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Thornton LE, Kavanagh AM. Association between fast food purchasing and the local food environment. Nutr Diabetes. 2012;2:e53. doi: 10.1038/nutd.2012.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Allison PD. Fixed Effects Regression Methods for Longitudinal Data Using SAS. SAS Institute; 2005. Available from: http://books.google.com/books?id=OIPExEh-tcMC. [Google Scholar]
- 54.McDonald A, et al. The CARDIA dietary history: development, implementation, and evaluation. J Am Diet Assoc. 1991;91:1104–12. [PubMed] [Google Scholar]
- 55.Willett W. Nutritional Epidemiology. Oxford University Press; USA: 1998. Available from: http://books.google.com/books?id=pcgCssTO0hwC. [Google Scholar]
- 56.Ng SW, Popkin BM. Monitoring foods and nutrients sold and consumed in the United States: dynamics and challenges. Journal of the Academy of Nutrition and Dietetics. 2012;112:41–45. e4. doi: 10.1016/j.jada.2011.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.