Abstract
Purpose
The purpose of this report was to present the case of a patient with bleeding diathesis on whom we performed ankle arthroplasty for the first time.
Materials and methods
A 29-year old male patient with bleeding diathesis, who had been treated and followed up over a long period, underwent ankle arthroplasty because of osteoarthritis of the ankle. The patient was prepared for surgery by the haematology department in accordance with the guidelines for surgical preparation, diagnosis and management of haemophilia. After ankle arthroplasty was performed, the preoperative and two-year postoperative clinical outcomes were evaluated using a subjective foot score and Maryland foot score.
Results
Preoperative factor VIII levels were raised to the target level of haemostasis prior to the surgical procedure. The factor VIII levels were maintained within the normal range up to postoperative day 14. The subjective foot score of the patient was 40 preoperatively and 85 postoperatively, whereas their Maryland foot scores were 33 preoperatively and 90 postoperatively. Both scoring systems indicate an excellent clinical outcome.
Conclusion
As observed, the early and mid-term functional outcomes are promising for patients with bleeding diathesis who undergo ankle arthroplasty.
Keywords: Bleeding diathesis, Ankle arthroplasty
Highlights
-
•
We tried to present an ankle arthroplasty in a bleeding disorder patient.
-
•
We wanted to show ankle arthritis treatment with arthroplasty can be made in this kind of patients.
-
•
Care has to be taken to treatment of bleeding disorder before the surgery.
1. Introduction
Surgical techniques have long been avoided for patients with bleeding diathesis because of the increased risk of uncontrolled bleeding and high rates of infection. However, recent improvements in the medical treatment of bleeding diathesis have enabled the safe and successful performance of total joint arthroplasties. Despite reports of successful long-term outcomes of hip and knee arthroplasties, our literature review revealed only a few series reporting the outcomes of ankle arthroplasty [1]. In the present case, our patient received ankle arthroplasty because he had developed ankle osteoarthritis due to severe bleeding into the joint over several years. Preoperative and postoperative 2-year clinical outcomes were evaluated according to the subjective and Maryland foot scores of the patient.
2. Case report
The case presented here is that of a 29-year-old male with ankle osteoarthritis (Fig. 1a, b). The department of surgical haematology defined the planned surgical procedure as a major surgery in accordance with the guidelines for surgical preparation, diagnosis and management of haemophilia. Accordingly, an attempt was made to increase the patient's preoperative factor level to the target level of 80–100% for haemostasis. Once the plasma factor VIII concentration reached 92%, the patient underwent ankle arthroplasty. Preoperatively, the patient was administered 60 IU of factor VIII/kg of body weight as a bolus infusion as recommended in the 2011 guidelines for surgical preparation, diagnosis and management of haemophilia. The same guidelines recommend an additional dose of 20 IU (40% of factor level) of factor VIII/kg of body weight if the surgery lasts longer than 4 h. However, his surgical procedure lasted for approximately 2 h and 15 min, and the patient required no additional replacement products. The postoperative factor VIII level was maintained at 72.3% (recommended 60–80%) for the first 3 days and at 53.1% (recommended level 40–60%) for days 4–6. The patient attained a mean factor VIII level of 44.9% (recommended level 30–50%) without the need for replacement therapy on postoperative days 7–14 and was discharged on postoperative day 10. Follow-ups were then executed on a weekly basis in our clinic. The patient had a mean factor VIII level of 36.0% (recommended 30–40%) on postoperative week 3. The patient experienced no surgical complications (Fig. 2a, b). Preoperative and two-year postoperative clinical outcomes of the patient were evaluated according to his subjective and Maryland foot scores. The subjective foot score (maximum score 100) evaluates pain, daily living activities, walking surfaces, walking distance and use of walking aids. The subjective foot score of the patient was 40 preoperatively, which increased to 85 postoperatively. The Maryland foot score of the patient was 33 preoperatively, and it increased to 90 postoperatively. The results of these two scoring systems indicate an excellent clinical outcome.
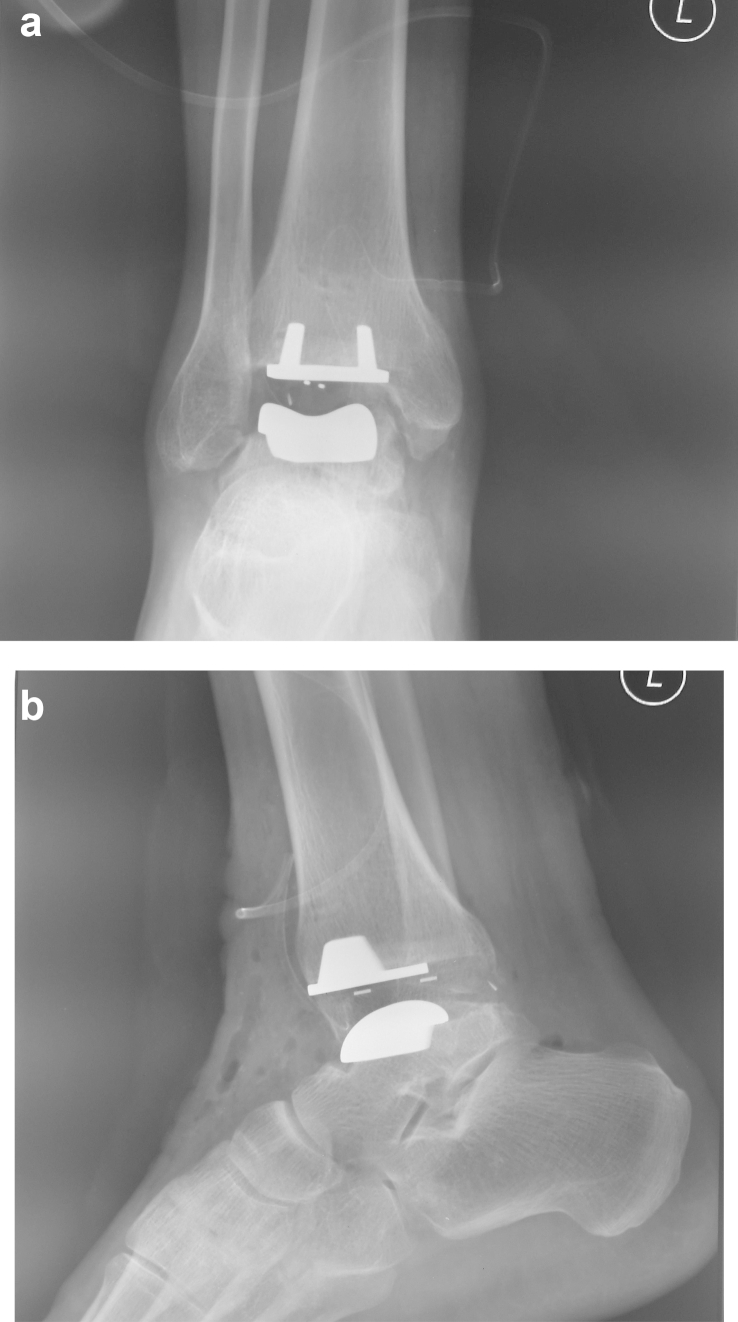
Fig. 1.
(a,b) Preoperative X-rays of the patient.
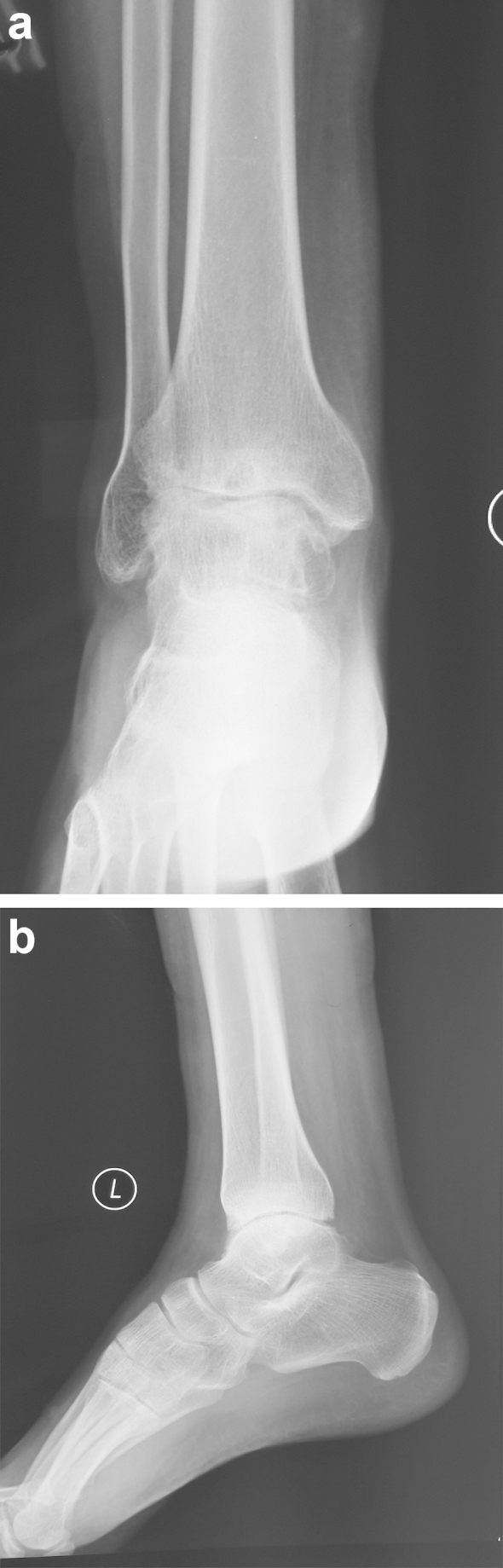
Fig. 2.
(a,b) Postoperative X-rays of the patient.
3. Discussion
In patients with bleeding diathesis, the most common bleeding joints include the knees, ankles and elbows. Arthropathy caused by bleeding diathesis begins with bleeding into the joints, which induces synovial inflammation and hypertrophy because of the absorption of blood breakdown products (particularly iron) by the synovium. In a study of 406 patients conducted by Valderrabano et al., posttraumatic ankle osteoarthritis was observed in 78% of the cases; thus, it was the most common underlying aetiology. Haemophilia, rheumatoid arthritis, haemochromatosis, congenital foot deformity, gout, aseptic necrosis of the talus and intraarticular infections were the other causes of secondary osteoarthritis of the ankle in this study (with prevalence rates of 10–15%) [2]. Once the iron absorption capacity of the synovium is exceeded, cells disintegrate and this results in the release of lysosomal enzymes, which both increase synovial tissue inflammation and lead to joint destruction. An increase of proteolytic enzymes such as acid phosphatase and cathepsin D leads to joint destruction. Blood breakdown products also affect the chondrocytes. Iron deposition in the synovium induces an increase in the levels of TNF, IL-1 and IL-6. Repeated bleeds into joints due to traumas and similar causes since childhood can result in the rapid development of joint destruction. In advanced stage arthropathy, the joint cartilage appears similar to that observed in osteoarthritis, but brown pannus tissue also fills the joint space, which results in pain and joint deformities as the main clinical manifestations [3], [4]. The radiologic classification of haemophilic arthropathy developed by Petterson et al., which was recommended by the World Federation of Hemophilia in 1981 and simplified by Greene in 1989, is still commonly used [3]. In addition, younger patients may also present with advanced osteoarthritis. With ever-improving technology, it is essential to seek remedies for these patients and enable them to benefit from the best possible treatment options for the rest of their lives [5], [6]. In a study evaluating the medium-term results of five total ankle replacements in three haemophilic patients, Van der Heide et al. reported good to excellent results and no signs of loosening after a median follow up of 4.3 years [7]. In a similar study, which evaluated the mid-term outcome of 10 haemophilic ankles in eight patients who were treated with total ankle replacement and followed up for a minimum of 2.7 years, Barg et al. reported that the AOFAS-hindfoot score increased from 38 (range 8–57) preoperatively to 81 postoperatively (range 69–95); furthermore, the whole patient cohort's pain level decreased from 7.1 (range 4–9) preoperatively to 0.8 (range 0–3) postoperatively, which indicated a significant improvement [1].
Recent studies have demonstrated that adequate factor VIII replacement in patients with bleeding diathesis is associated with the safe performance of surgical or medical interventions. In these cases, the appropriate dose and duration of factor replacement therapy depends on the severity of the disease and type of surgical procedure or intervention, and haematologists should perform the therapy [7], [8]. An appropriate factor level should be maintained for 10–14 days after major surgery. In contrast, the factor levels may need to be maintained for longer periods after some orthopaedic procedures, particularly when physical therapy and rehabilitation are also required. One issue of great importance in factor replacement is venous thromboembolism. The rate of venous thromboembolism among adult patients receiving factor replacement in major surgery is similar to that in non-haemophilic patients. Therefore, after factor replacement is performed, anticoagulant prophylaxis with LMWH is required. The duration and dosing of thromboprophylaxis administered is the same in haemophilic and non-haemophilic individuals. However, mechanical thromboprophylaxis rather than pharmacologic thromboprophylaxis is recommended in haemophilic patients with an inhibitor. Thromboprophylaxis with LMWH is recommended in patients without inhibitors who undergo arthroplasty, whereas thromboprophylaxis using mechanical methods should be performed in inhibitor patients treated with bypassing agents and those who undergo arthroscopic surgery. Preoperative administration of thromboprophylaxis is not recommended. We did not observe thrombosis in our patient. LMWH can be initiated 6–12 h postoperatively to minimize the risk of bleeding for a period of no less than 4 weeks. In addition, intravenous injections and arterial interventions should be avoided in patients with bleeding diathesis [8]. General anaesthesia, rather than deep block anaesthesia and combined spinal-epidural anaesthesia, is recommended. Moreover, ASA and non-steroidal agents should be avoided as analgesics during procedures. The common dose for acetaminophen is 500 mg to 1 g in adults and 10–15 mg/kg/dose in children, with administration every 4–6 h. In the presence of persistent or severe pain, a weak or potent opioid can be administered [9]. All of these ground rules require the compliance and collaboration of several departments, including haematology, anaesthesiology, algology and orthopaedics, in relation to patients scheduled to undergo arthroplasty, which is defined as a major surgery. In the present patient's case, thromboprophylaxis and analgesia were administered in accordance with the recommendations of the haematology department.
As seen in our patient's case, early and mid-term functional outcomes of ankle arthroplasty in patients with bleeding diathesis are promising. As we observed, where factor replacement is administered at appropriate doses, major bleeding can be managed.
Ethical approval
Consent form was taken from the patient
Funding
There is no funding in our research.
Author contribution
BY Study Design.
BK Data Collection, Writing.
GÖ Data Analysis.
NH Data Collection.
Conflicts of interest
There is no conflict of interest.
Guarantor
The all authors are guarantors of the study.
References
- 1.Barg A., Elsner A., Hefti D., Hintermann B. Haemophilic arthropathy of the ankle treated by total ankle replacement: a case series. Haemophilia. 2010 Jul 1;16(4):647–655. doi: 10.1111/j.1365-2516.2010.02221.x. [DOI] [PubMed] [Google Scholar]
- 2.Hintermann B., Knupp M., Zwicky L., Barg A. Total ankle replacement for treatment of end-stage osteoarthritis in elderly patients. J. Aging Res. 2012;2012:345237. doi: 10.1155/2012/345237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Greene W.B., McMillan C.W. Nonsurgical management of hemophilic arthropathy. Instr. Course Lect. 1989;38:367–381. [PubMed] [Google Scholar]
- 4.Philipp C. The aging patient with hemophilia: complications, comorbidities and management issues. Hematol. Am. Soc. Hematol. Educ. Program. 2010:191–196. doi: 10.1182/asheducation-2010.1.191. [DOI] [PubMed] [Google Scholar]
- 5.Petterson H., Ahlberg A., Nilsson I.M. A radiologic classification of hemophilic arthropathy. Clin. Orthop. 1980;149:153–159. [PubMed] [Google Scholar]
- 6.Konkle B.A., Kessler C., Aledort L., Andersen J., Fogarty P., Kouides P., Quon D., Ragni M., Zakarija A., Ewenstein B. Emerging clinical concerns in the ageing haemophilia patient. Haemophilia. 2009;15(6):1197–1209. doi: 10.1111/j.1365-2516.2009.02066.x. [DOI] [PubMed] [Google Scholar]
- 7.Van der Heide H.J., Novakova I., de Waal Malefijit M.C. The feasibility of total ankle prosthesis for severe arthropathy in haemophilia and prothrombin deficiency. Haemophilia. 2006 Nov;12(6):679–682. doi: 10.1111/j.1365-2516.2006.01350.x. [DOI] [PubMed] [Google Scholar]
- 8.Hermans C., Altisent C., Batorova A., Chambost H., De Moerloose P., Karafoulidou A. European haemophilia therapy standardization board. Replacement therapy for invasive procedures in patients with haemophilia: literature review, European survey and recommendations. Haemophilia. 2009;15(3):639–658. doi: 10.1111/j.1365-2516.2008.01950.x. [DOI] [PubMed] [Google Scholar]
- 9.Peerlinck K., Jacqueminn M. Mild hemophilia: a disease with many faces and many unexpected pitfalls. Hemophilia. 2010;16(Suppl. 5):100–106. doi: 10.1111/j.1365-2516.2010.02306.x. [DOI] [PubMed] [Google Scholar]