Abstract
Background: Squamous cell carcinoma is a severe malignant tumor but was rare in the chronic osteomyelitis. The purpose of this study was to present the results from a retrospective study the cases of squamous cell carcinoma arising from chronic osteomyelitis. Material and methods: Between 1974 and 2010, eight cases of squamous cell carcinoma after chronic osteomyelitis were treated. The patients had an average age of 55 years (range 45 to 66 years), with a male predominance (6 men and 2 woman). We analyzed the time up to cancerization, localization and histopathological types of the carcinoma, and types and results of the treatment. Results: The mean delay between the initial injury and the diagnosis of malignant transformation was 28 years (range 8 to 50 years). The carcinoma resulted from tibia osteomyelitis in six cases, femur in one case and ankle in one case. The pathological examination showed two cases of a well-differentiated squamous cell carcinoma with bone invasion and six cases of invasive squamous cell carcinoma. Curative amputation was performed in all patients but one who refused. No recurrence or metastasis occurred during follow-up time. Conclusion: Amputation appears to be an effective treatment method in squamous carcinoma secondary to chronic osteomyelitis.
Keywords: Osteomyelitis, epithelial neoplasms, squamous cell carcinoma, amputation
Introduction
The incidence of cutaneous neoplasms continues to increase dramatically despite the increasing awareness of the disease process and advances in diagnosis and treatment [1]. This is likely secondary to the advancing age of the population, the growing sun exposure, the increasing prevalence of immunosuppressive therapy for dermatologic and rheumatologic conditions, and an improved awareness leading to early detection.
Cancerization of chronic osteomyelitis has been known since the 19th century. In 1835, Hawkins was the first to document the presence of squamous cell carcinoma arising in chronic osteomyelitis [2]. This malignant transformation is defined by a change in the clinical, radiological, bacteriological and histological symptomatology of the chronic osteomyelitis [3]. It is a rare and late complication developing 20 to 40 years after a chronic bone infection. This degeneration may involve the skin orifice or the fistula and sinus tract. It is particularly seen after long bone infections and results most often in squamous cell carcinoma and rarely in a sarcoma or lymphoma. The physiopathological mechanism of cancerization is unknown. Chronic irritation of the skin or soft tissue exposure to different growth factors may play an important role. Biopsy is essential for appropriate diagnosis and treatment to these suspicious lesions [1,4]. In this study, we report eight cases representative for various aspects of this potentially fatal complication.
Material and methods
This study was approved by the Ethics Committee of Shandong Provincial Hospital, and the informed consent was obtained from all patients. Eight cases of cancerous degeneration resulting from chronic osteomyelitis were treated in the Department of Orthopedics; Shandong Provincial Hospital affiliated to Shandong University between 1974 and 2010. The patients had an average age of 55 years (ranged from 45 to 66), with a male predominance (6 men, 2 woman). All patients who were included in the study had malignant transformation of a chronic skin lesion or ulceration associated with a chronic bone infection. Diagnostic for a chronic osteomyelitis was an evident bone infection with a fistula discharge for over one year. Patients presented with clinical symptoms suggesting cancerization including constant and disabling pain. A fistula adjacent to the osteomyelitis bone site produced a purulent discharge with an unpleasant odor in all patients (Figure 1). Patients had no palpable lymph nodes on physical examination. All 8 patients had plain radiograms and CT scan. In 4 patients magnetic resonance imaging (MRI) was performed as an additional imaging study to reveal bone lesions and soft tissue masses (Figures 2, 3 and 4). Microbiological sampling was positive in 5 cases. Most patients presented with mixed infections. Staphylococcus was the most common organism. The malignancy was confirmed with histopathological examination in all cases (Figure 5). We analyzed the time to cancerization, the localization and histopathological types of the carcinoma, and the results of the treatment.
Figure 1.

A 58-year-old man with 50-year history of osteomyelitis of the left tibia presented with painful ulceration of the anterior lower limb. The clinical photograph showed the ulceration with a purulent discharge and an unpleasant odor.
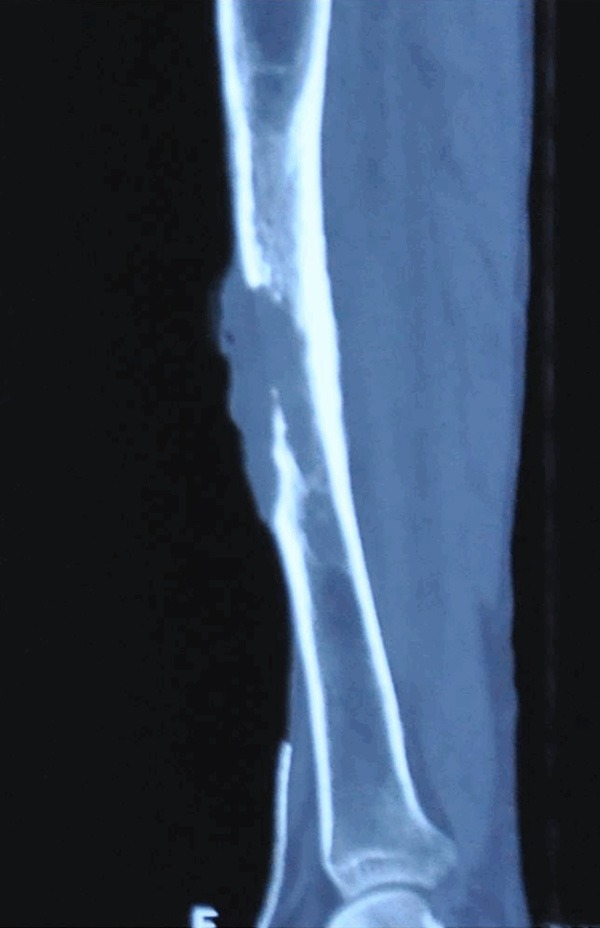
Figure 2.

Anteroposterior and lateral radiographs reveal findings compatible with chronic osteomyelitis and osteolysis of the tibia.
Figure 3.
The CT scan documents squamous cell carcinoma with osteolysis of the tibia.
Figure 4.
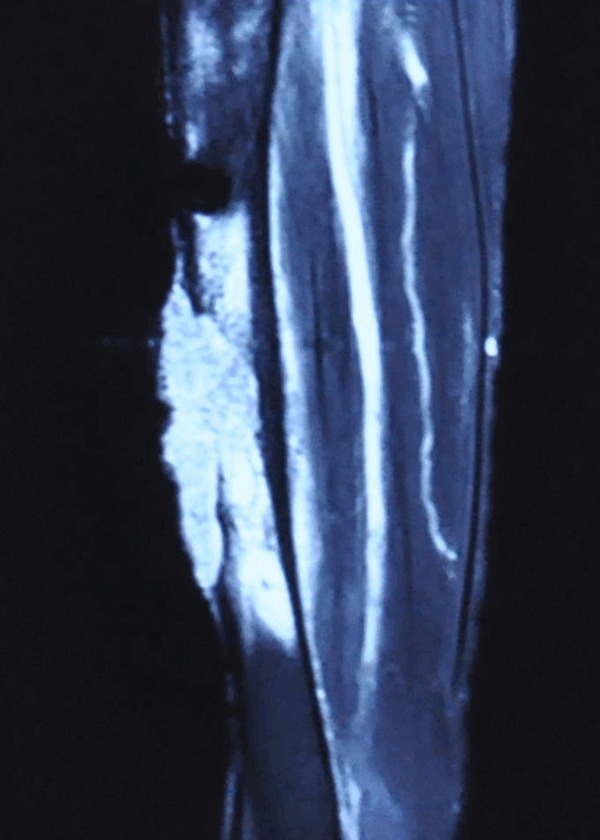
The MRI demonstrates the soft-tissue mass with invasion into the bone.
Figure 5.
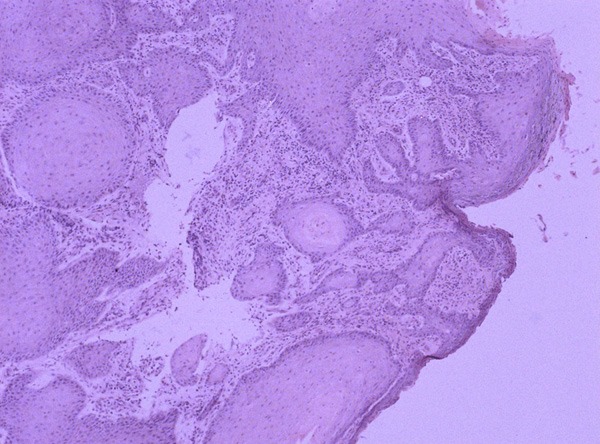
Haematoxylin-Eosin staining reveals a squamous cell carcinoma and keratin pearls.
Results
The mean time between the occurrence of the initial injury and the diagnosis of malignant transformation was 28 years (ranged from 8 to 50 years). Six cases had chronic osteomyelitis. In two cases the osteomyelitis occurred after a fracture, of which one had an open fracture. The tibia was the most common site of involvement (6 cases), followed by the femur (1 cases) and the ankle (1 cases). Pathological examination showed 2 cases of a well-differentiated squamous cell carcinoma with bone invasion and 6 cases of invasive squamous cell carcinoma. None of the patients had metastatic lesions (Table 1). The amputations were performed in all patients except one patient who refused the treatment. We performed a hip exarticulation in the case with femur osteomyelitis (Patient 2) and a below-knee amputation (BKA) in 6 cases located in tibia (Patient 3, 4, 5, 6, 7 and 8). The patients performed hip disarticulation can walk with the help of a cane. The rest amputee patients achieved a positive results with an artificial limb; they experienced no residual pain and were ambulatory without crutches. The amputee patients did not show local recurrence or metastatic dissemination over a period of 5 years (Table 2).
Table 1.
Clinical and radiological features
| Patients | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|
| Sex | male | male | female | female | male | male | male | male |
| Age | 51 | 61 | 52 | 66 | 45 | 53 | 52 | 58 |
| Initial lesion | Post-traumatic chronic osteitis | Post-traumatic chronic osteitis | Chronic osteomyelitis | Chronic osteomyelitis | Post-traumatic chronic osteitis | Post-traumatic chronic osteitis | Post-traumatic chronic osteitis | Post-traumatic chronic osteitis |
| Location | Ankle | Femur | Tibia | Tibia | Tibia | Tibia | Tibia | Tibia |
| Cancerization delay (years) | 13 | 40 | 33 | 20 | 30 | 30 | 8 | 50 |
| Clinical symptoms | Pain; Skin ulceration; Sinus; Hyperosteogeny | Pain; Sinus | Pain; Purulent secretion | Pain; Purulent secretion | Pain; Purulent secretion | Pain; Purulent secretion | Pain; Abscesses; Skin peeling, scarring and lumpiness | Pain; Skin ulceration; Sinus; Hyperosteogeny |
| Lymph nodes | No | No | No | No | No | No | No | No |
| Radiology | Osteolysis | Osteolysis | Osteolysis | Osteolysis | Osteolysis | Osteolysis | Osteolysis | Osteolysis |
| Metastasis | No | No | No | No | No | No | No | No |
Table 2.
Histopathology, treatment and recurrence details of the patients
| Patients | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|
| Histopathology | Well Differentiated squamous cell carcinoma with bone invasion | Invasive squamous cell carcinoma | Well Differentiated squamous cell carcinoma with bone invasion | Invasive squamous cell carcinoma | Invasive squamous cell carcinoma | Invasive squamous cell carcinoma | Invasive squamous cell carcinoma | Invasive squamous cell carcinoma |
| Treatment | Amputation refused by patient | Hip exarticulation | BKA | BKA | BKA | BKA | BKA | BKA |
| Recurrence | Lost to follow-up | No recurrence | No recurrence | No recurrence | No recurrence | No recurrence | No recurrence | No recurrence |
BKA: Below-knee amputation.
Discussion
Squamous cell carcinoma is the most common type of malignant tumor deriving from chronic osteomyelitis [5-7]. The most frequently affected site is the tibia, followed by the femur. The upper limb is rarely affected. Accordingly, in six of eight cases a tibial localization was found. Beyond that, the presentation was variable; we could observe an extension or an unusual persistence of skin ulceration, an onset of a burgeoning mass of the fistulous orifice, a rapidly growing and disabling pain, a discharge with an unpleasant odor, sometimes containing blood or an increase in the size of the limb [8-12]. When the neoplasm invades the bone, there is either osteolytic erosion or a pathological fracture. In our series, we observed osteolysis in all patients, which indicates the infiltrative stage of the disease. Diagnosis is confirmed by biopsy at all suspicious wound sites [10,11]. The malignant transformation most often results in squamous cell carcinoma and much more rarely in fibrosarcoma, osteosarcoma, reticulosarcoma, malignant fibrous histiocytoma or angiosarcoma [3,13-17]. It begins at the skin or epithelial structure of the fistulous route and then invades the bone. We observed only squamous cell carcinoma in our series, the most frequent type in the literature. The occurrence of metastasis is limited to 15% of cases, always occurring within five years of diagnosis [18]. The presence of satellite nodes is common but often indicates a simple inflammatory reaction. None of our patients had metastases or palpable lymph nodes at the initial assessment.
Many experts accept amputation as the best treatment option for carcinomatous transformations of chronic bone infections [9-12]. Avoiding amputation, wide resections can result in local recurrence, which could require delayed amputation with worse outcome [19]. All our patients were in the advanced stage, with bone invasion in all patients and active bone infection, associated with a large skin defect in all patients. Amputation was chosen because in these advanced cases, the limb-preserving treatment is very complex and often does not provide a complete recovery without recurrence. Amputation allows a faster rehabilitation and safer recovery. The prognosis is generally better for well differentiated squamous cell carcinoma than for other differentiated histological types. The existence of lymphatic node involvement or visceral metastasis lowers the 5-year survival rate to 35-50% [9,11,12].
Mankin et al [20] performed a study in 1982 to evaluate the hazards of 329 biopsies of primarily malignant musculoskeletal tumors, including bone and soft tissue. The results demonstrated troubling rates of errors in diagnosis and technique, resulting in complications and poor patient care. The same group of investigators replicated this study 10 years later and found similar results. A recent study in 2011 reported seven cases of chronic osteomyelitis related squamous cell carcinoma between 1993 and 2005 [21]. The patients had an average age of 55 years (ranged from 38 to 71 years), with a male predominance (6 men, 1 woman). The mean time between the occurrence of the skin lesions and the diagnosis of malignant degeneration was 25 years (ranged from 9 to 40 years). The carcinoma resulted from tibia osteomyelitis in 4 cases, femur in 2 cases and humerus in one case. The pathological examination showed five cases of a well differentiated squamous cell carcinoma with bone invasion, and two cases of invasive squamous cell carcinoma. The treatment consisted of amputation in all but one patient, who refused the amputation. The six amputees did not suffer from local recurrence or metastatic dissemination over a period of five years. In our series, the good prognosis was due to the pathological type of the tumors, the efficient and definitive treatment, and the absence of malignant lymph nodes and metastasis.
Carcinomatous degeneration after chronic osteomyelitis is a rare and late complication. It should be considered even years after the development of chronic osteomyelitis. The most suggestive signs are the persistence of a foul smelling fistula and the ulceration. Biopsy is the most trusted method for diagnosis. Treatment depends on the stage of the disease: in the early stage, limb saving surgery can be performed, but in the advanced stages with bone invasion and large skin defects, amputation is necessary. The aim of this series was to show the gravity of the disease and highlight the fact that it can occur many years after the onset of osteomyelitis. The most effective prevention of carcinomatous degeneration is the use of local fasciocutaneous flaps for skin coverage to prevent chronic wounds which is a breeding ground for carcinomatous degeneration (Figure 6).
Figure 6.
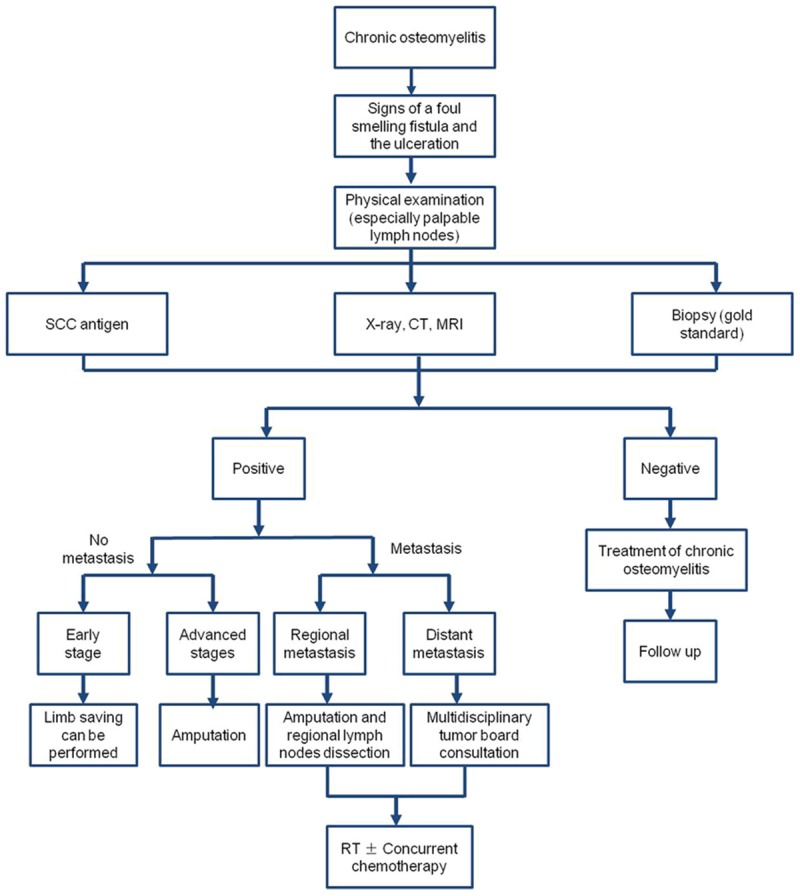
Diagnosis and treatment algorithm for suspicion of carcinomatous transformation of osteomyelitis.
Conclusion
Squamous cell carcinoma following the chronic osteomyelitis is a rare lesion found in the lower extremity. Ulceration with an atypical presentation and a long duration should raise clinical suspicion and a biopsy should be performed to exclude underlying malignancy. Ideally, the definitive procedure should be performed by the surgeon who obtained the biopsy. Amputation appears to be an effective treatment method in squamous carcinoma secondary to chronic osteomyelitis.
Acknowledgements
This research was supported by grants from the National Natural Science Foundation of China (No. 81300964 and No. 81301556), the China Postdoctoral Science Foundation (No. 2013M531611 and No. 2014T70648) and the Natural Science Foundation of Shandong Province (No. ZR2011HM054).
Disclosure of conflict of interest
None.
References
- 1.McGrory JE, Pritchard DJ, Unni KK, Ilstrup D, Rowland CM. Malignant lesions arising in chronic osteomyelitis. Clin Orthop Relat Res. 1999;362:181–189. [PubMed] [Google Scholar]
- 2.Hawkins C. Cases of warty tumours in cicatrices. Med Chir Trans. 1835;19:19–34. doi: 10.1177/095952873501900104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bergstrahl EJ, Offord KP. Technical Report Series No. 37. Rochester (MN): Section of Biostatistics, Mayo Clinic; 1988. Conditional probabilities used in calculating cohort expected survival. [Google Scholar]
- 4.Selin ED, Fleming JL. Epidermoid carcinoma arising in chronic osteomyelitic foci. J Bone Joint Surg Am. 1963;45:827–838. [Google Scholar]
- 5.Blidi M, Gatefosse M, Barjonnet G, Bedoucha JS, Wajcner G. Epidermoid carcinoma complicating chronic osteomyelitis of the femur. Rev Rhum Engl Ed. 1996;63:62–4. [PubMed] [Google Scholar]
- 6.Goldberg DJ, Arbesfeld D. Squamous cell carcinoma arising in a site of chronic osteomyelitis. J Dermatol Surg Oncol. 1991;17:788–790. doi: 10.1111/j.1524-4725.1991.tb03261.x. [DOI] [PubMed] [Google Scholar]
- 7.Mabit C, Huc H, Setton D, Leboutet MJ, Arnaud JP, Pecout C. Epidermoid carcinoma arising in femoral osteitis. A case. Rev Chir Orthop Reparatrice Appar Mot. 1993;79:62–65. [PubMed] [Google Scholar]
- 8.Johnson LL, Kempson RL. Epidermoid carcinoma in chronic osteomyelitis: diagnostic problems and management: report of ten cases. J Bone Joint Surg Am. 1965;47:133–145. [PubMed] [Google Scholar]
- 9.Gebhart M, Fabeck L, Muller C. Malignant transformation of chronic osteomyelitis and its scar tissue: apropos of 3 cases. Acta Orthop Belg. 1993;59:327–332. [PubMed] [Google Scholar]
- 10.Sankaran-Kutty M, Corea JR, Ali MS, Kutty MK. Squamous cell carcinoma in chronic osteomyelitis. Report of a case and review of the literature. Clin Orthop Relat Res. 1985;198:264–267. [PubMed] [Google Scholar]
- 11.Saglik Y, Arikan M, Altay M, Yildiz Y. Squamous cell carcinoma arising in chronic osteomyelitis. Int Orthop. 2001;25:389–391. doi: 10.1007/s002640100280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mahfoud M. Traité de Traumatologie. Tome 2. Tétouan: Editions Cercos; 2006. pp. 402–404. [Google Scholar]
- 13.Akbarnia BA, Wirth CR, Colman N. Fibrosarcoma arising from chronic osteomyelitis. Case report and review of the literature. J Bone Joint Surg Am. 1976;58:123–125. [PubMed] [Google Scholar]
- 14.Denham RH, Dingley AF. Fibrosarcoma occurring in a draining sinus. J Bone Joint Surg Am. 1963;45:384–386. [Google Scholar]
- 15.Morris JM, Lucas DB. Fibrosarcoma within a sinus tract of chronic draining osteomyelitis. Case report and review of the literature. J Bone Joint Surg Am. 1964;46:853–857. [PubMed] [Google Scholar]
- 16.Waugh W. Fibro Sarcoma occurring in a chronic bone sinus. J Bone Joint Surg. 1952;34:642–646. doi: 10.1302/0301-620X.34B4.642. [DOI] [PubMed] [Google Scholar]
- 17.Zlowodzki M, Allen B, Schreibman KL, Vance RB, Kregor PJ. Malignant fibrous histiocytoma of bone arising in chronic osteomyelitis. Clin Orthop Relat Res. 2005;439:269–273. doi: 10.1097/01.blo.0000176556.12728.cd. [DOI] [PubMed] [Google Scholar]
- 18.Bereston ES, Ney C. Squamous cell carcinoma arising in a chronic osteomyelitic sinus tract with metastasis. Arch Surg. 1941;43:257–268. [Google Scholar]
- 19.Bauer T, David T, Rimareix F, Lortat-Jacob A. Marjolin’s ulcer in chronic osteomyelitis: seven cases and a review of the literature. Rev Chir Orthop Reparatrice Appar Mot. 2007;93:364–372. doi: 10.1016/s0035-1040(07)90205-6. [DOI] [PubMed] [Google Scholar]
- 20.Mankin HJ, Lange TA, Spainer SS. The hazards of biopsy in patients with malignant primary bone and soft tissue tumors. J Bone Joint Surg Am. 1982;64:1121–1127. [PubMed] [Google Scholar]
- 21.Alami M, Mahfoud M, El Bardouni A, Berrada MS, El Yaacoubi M. Squamous cell carcinoma arising from chronic osteomyelitis. Acta Orthop Traumatol Turc. 2011;45:144–148. doi: 10.3944/AOTT.2011.2537. [DOI] [PubMed] [Google Scholar]


