Abstract
The present study aims to investigate the relationship of NF-κB p65 and PTEN protein with chemotherapy resistance in ovarian cancer by measuring their expression in primary epithelial ovarian cancer, and to explore the correlation of the expression of these two proteins with ovarian carcinoma and their clinical significance. Ovarian cancer patients (n = 161) were divided into two groups: sensitive group (n = 82) and resistant group (n = 79). Expression of NF-κB p65 and PTEN protein in the ovarian cancer tissues was determined using immunohistochemistry to assess the relationship and correlation between the expression levels of these two proteins and chemotherapy resistance of ovarian carcinoma. The Cox model was used to analyze the independent risk factors associated with ovarian cancer prognosis. The expression of NF-κB p65 in the sensitive group (68.29%) was lower than that of the resistant group (94.94%). In contrast, the expression of PTEN protein in the sensitive group (50.00%) was higher than that of the resistant group (17.72%). Expression of NF-κB p65 was negatively correlated with that of PTEN protein in ovarian cancer tissue (rs = -0.246, P = 0.002). Expression of NF-κB p65 or PTEN protein and surgical stage of ovarian cancer were independent risk factors associated with chemoresistance (all P < 0.05). Low expression of PTEN and high expression of NF-κB are significant risk factors for chemotherapy resistance of ovarian cancer patients.
Keywords: PTEN, NF-κB, immunohistochemistry, chemoresistance, ovarian epithelial cancer
Introduction
As one of the three most commonly occurring malignant tumors of female genitalia, the incidence rate of ovarian cancer is only second to cervical cancer and endometrial cancer, but its mortality rate ranks first [1]. Ovarian cancer is mainly treated by cytoreductive surgery combined with platinum-based chemotherapy. Chemotherapy has become an important part of ovarian cancer treatment, with cisplatin terminating the growth of tumor cells through inhibition of DNA replication and transcription. However, resistance against platinum-based drugs develops easily [2,3], which limits its therapeutic effects, and leads to poor prognosis of ovarian cancer; the 5-year survival rate is approximately 30%. Therefore, chemotherapy resistance has become an urgent problem for ovarian cancer treatment that needs to be solved.
The occurrence of tumor and chemo-resistance involves a variety of cellular events and physiological processes, including failed gene regulation and abnormal signal pathway as leading causes of malignant transformation of cells, which can result in uncontrolled cell proliferation, tumor occurrence and chemoresistance. The PI3K/AKt pathway is an important signal transduction pathway in cells and is activated in a variety of tumor cells. Activation of downstream NF-κB transcription factors can significantly increase the proliferation of tumor cells, decrease the apoptosis and autophagy of tumor cells, promote neovascularization in tumor cells and enhance the local invasion and distant metastasis of tumor cells [4-6]. Recent studies have found that changes in the NF-κB signaling pathway also play an important role in the chemoresistance of tumor cells [7,8]. The phosphatase and tension homolog deleted on chromosome ten (PTEN) gene is the first tumor suppressor gene found in humans with protein phosphatase and lipid phosphatase bispecific activity, which mainly inhibits tumor growth by suppressing the dephosphorylation of the PI3K/AKt signaling pathway. PTEN also plays an important role in regulation of the cell cycle and induction of cell apoptosis and autophagy, involving angiogenesis and transduction of multiple signaling pathways of cells [9-12]. Deletion and mutation of the PTEN gene is found in many human tumors [13], and deletion, mutation or inactivation of its expression product promotes the occurrence and development of various tumors [14]. Recent studies have also suggested that deletion of the PTEN gene may be involved in the formation of drug-resistant tumors [15,16].
The expression of NF-κB p65 and PTEN protein in primary epithelial ovarian carcinoma was measured using immunohistochemistry to evaluate the relationship and correlation of the expression of these two proteins and chemotherapy resistance in ovarian cancer. The role of NF-κB and PTEN in the chemotherapy resistance of ovarian cancer was revealed in order to explore the mechanism of chemoresistance in ovarian cancer and seek solutions to overcome such resistance, which bears great significance for the improvement of the survival rate of ovarian cancer patients.
Material and methods
Clinical samples
This study was approved by the Research Ethics Committee of the Shengjing Hospital Affiliated to China Medical University. Written informed consent was obtained from all of the patients. Tumor tissue was obtained during operation. All specimens were collected in full accordance with the ethical and legal standards. The ovarian cancer tissue samples were collected from 161 patients who received cytoreductive surgery at Shengjing Hospital of China Medical University between May 2006 and September 2012. The average age of the patients was 51 years (19-73 years). Only patients with complete clinical pathological data and follow-up data were included. All cases were primary cancer with no preoperative chemotherapy, and were divided into the sensitive group (82 cases) and resistant group (79 cases) according to clinical data. The expression levels of NF-κB p65 and PTEN protein in ovarian cancer tissue were detected using immunohistochemistry, and their relationship and correlation with chemotherapy resistance in ovarian cancer were explored. The pathological types included serous carcinoma (100 cases), mucinous carcinoma (11 cases), clear cell carcinoma (19 cases), poorly differentiated adenocarcinoma (20 cases), and 11 cases of other carcinoma endometrioid carcinoma (8 cases), transitional cell carcinoma (1 case) and mixed cell carcinoma (2 cases). Among the 161 patients, there were stage I-II (73 cases) and stage III-IV (88 cases) based on surgical pathology staging according to the International Federation of Gynecology and Obstetrics (FIGO). Based on pathological classification, there were well-differentiated (15 cases), moderately differentiated (54 cases), poorly differentiated (73 cases), and unknown (19 cases).
The patients were divided, according to NCCN guidelines, into a resistant or sensitive group. Patients in the resistant group exhibited clinical remission at an early stage of chemotherapy, with recurrence at late stage of chemotherapy or within 6 months after chemotherapy; recurrence 6-12 months after chemotherapy was defined as partial sensitivity; and recurrence beyond 12 months after chemotherapy was defined as drug sensitivity. The main clinical features of recurrent ovarian cancer include: (1) persistent increase of CA125, (2) mass found during gynecological examination, (3) tumor found during imaging examination, (4) ascites and (5) intestinal obstruction with unknown causes.
Immunohistochemical analysis
Four slices were prepared for each ovarian cancer tissue specimen, and expression levels of NF-κB p65 and PTEN protein were detected using the immunohistochemical streptavidin peroxidase connection (SP) method. The tissues were fixed in 4% formaldehyde and embedded in paraffin, with consecutive 5 μm slices obtained from the same section. The slices were dewaxed by xylene, followed by gradient hydration with ethanol, and then processed in 3% hydrogen peroxide solution for 30 min to block endogenous peroxidase activity. Slices were finally rinsed with phosphate buffer saline (PBS) for 3 min three times. Antigen retrieval was conducted with citrate buffer solution, which was then cooled to room temperature, and rinsed with PBS solution for 3 min three times. The slices were then incubated in 5% normal goat serum for 30 min to block the non-specific binding sites. After removal of the serum, 50 μl diluted NF-κB p65 primary antigen (Abcam) or PTEN primary antigen (Abcam) was added to the slices, which were then placed in a humidity chamber overnight at 4°C. The samples were rinsed with PBS, followed by addition of 50 μl goat anti-rabbit IgG secondary antigen, and then placed in a wet box and incubated for 30 min at 37°C. After addition of 50 μl streptavidin biotin peroxidase, samples were returned to the wet box and incubated for another 30 min at 37°C. Fifty microliters of newly prepared DAB solution was added and coloration was monitored under a microscope. The reaction was terminated by rinsing with tap water, followed by nuclear staining with hematoxylin. Samples were then dehydrated with gradient ethanol, followed by transparentizing by xylene. The samples were then fixed in neutral resin. For each batch of experiments, tissue slices from the sensitive group and resistant group were chosen, along with both negative and positive controls. For the negative control, PBS was used instead of primary antibody, while breast cancer tissue was used as the positive control.
A semi-quantitative approach was employed for the result determination. Cells with brownish-yellow staining observed in the cytoplasm and cell nucleus were considered positive. According to the staining intensity, no color, light yellow, brownish-yellow and brown were labeled as 0, 1, 2 and 3, respectively. The percentage of stained cells was the average value of five consecutive fields under 400 power for each slice. The score for the percentage of positive cells < 5% was 0, and 1 for 5-25%, 2 for 26-50%, 3 for 51-75%, and 4 for > 75%. The final result was calculated as the mean of the product of two scores of five fields: 2 or below was considered negative (-), 3-4 was considered weakly positive (+), 5-8 was considered moderately positive (++), and 9-12 was considered strongly positive (+++). To control for errors, two observers reviewed each sample slice separately.
Statistical analysis
SPSS19.0 software was employed for statistical analysis. The categorical data were analyzed using a Chi-square (χ2) test, while the continuous data were analyzed using a t-test Multivariate logistic regression analysis was used to analyze the relevant factors of chemoresistance, with the degree of closeness assessed using Spearman’s rank correlation coefficient. Furthermore, the Cox model was used to analyze the relationship with the prognosis. P < 0.05 was considered statistically significant.
Results
Expression of NF-κB p65 and PTEN protein in ovarian cancer sensitive group and resistant group
In the ovarian cancer tissues, NF-κB p65 was mainly expressed in the nucleus and cytoplasm, the positive rate of NF-κB p65 in the sensitive group (65.45) is significantly lower than the resistant group (94.94%). PTEN is mainly expressed in the cytoplasm, with occasionally stained nuclei observed, the positive rate of the PTEN in the sensitive group (50.00%) is significantly higher than the resistant group (17.72%) (Figure 1).
Figure 1.
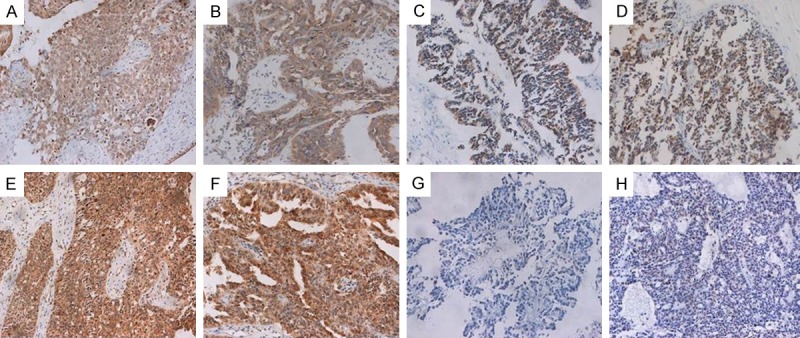
Representative photographs of NF-κB p65 and PTEN protein in primary epithelial ovarian carcinoma. A, B: NF-κB p65 expression in the sensitive group. C, D: PTEN expression in the sensitive group. E, F: NF-κB p65 expression in the resistant group; G, H: PTEN expression in the resistant group. All images are magnified 200×.
Correlation between NF-κB and PTEN expression in ovarian cancer tissues
In 161 cases of ovarian cancer tissues, Spearman rank correlation test demonstrated a negative correlation between the NF-κB p65 and PTEN expression (rs = -0.246, P = 0.002) (Figure 2; Table 1).
Figure 2.
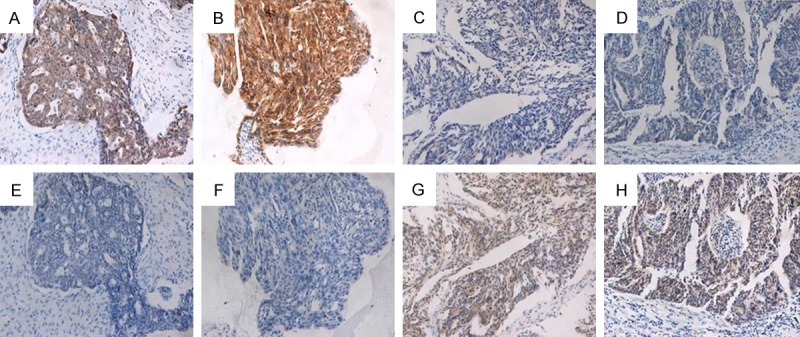
Representative photographs NF-κB p65 expression and PTEN expression in the consecutive sections. A-D: NF-κB p65 expression in ovarian cancer tissues; E-H: PTEN expression in the same tissue of A-D.
Table 1.
Correlation between NF-κB p65 and PTEN expression in ovarian cancer tissues
| N | NF-κB p65 | ||||
|---|---|---|---|---|---|
|
|
|||||
| - | + | ++ | +++ | ||
| PTEN | |||||
| - | 107 | 13 | 19 | 53 | 22 |
| + | 41 | 9 | 4 | 23 | 5 |
| ++ | 5 | 3 | 2 | 0 | 0 |
| +++ | 8 | 5 | 1 | 2 | 0 |
| N | 161 | 30 | 26 | 78 | 27 |
Univariate analysis of chemoresistance in ovarian cancer
Univariate analysis of the chemoresistance -related factors in both the sensitive and resistant groups showed statistically significant differences in surgical stage and lymph node metastasis between the two groups (P < 0.05). No statistical significance in age, histological grade and pathological types was demonstrated between the two groups (P > 0.05) (Table 2).
Table 2.
Univariate analysis of chemoresistance in ovarian cancer
| Groups | Total cases | Sensitive group | Resistant group | P | ||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Cases | Rate (%) | Cases | Rate (%) | |||
| Age (years) | ||||||
| ≤ 51 | 78 | 45 | 54.88 | 33 | 41.77 | 0.096 |
| > 51 | 83 | 37 | 45.12 | 46 | 58.23 | |
| Surgical stage | ||||||
| I-II | 73 | 57 | 69.51 | 16 | 20.25 | < 0.001 |
| III-IV | 88 | 25 | 30.49 | 63 | 79.75 | |
| Pathological grade | ||||||
| G1 | 73 | 32 | 39.02 | 41 | 51.90 | 0.198 |
| G2 | 54 | 29 | 35.37 | 25 | 31.65 | |
| G3 | 15 | 11 | 13.41 | 4 | 5.06 | |
| Unknown | 19 | 10 | 12.20 | 9 | 11.39 | |
| Histological type | ||||||
| Serous adenocarcinoma | 100 | 45 | 54.88 | 55 | 69.62 | 0.141 |
| Mucinous adenocarcinoma | 11 | 5 | 6.10 | 6 | 7.60 | |
| Clear cell carcinoma | 19 | 10 | 12.20 | 9 | 11.39 | |
| Poorly differentiated carcinoma | 20 | 15 | 18.29 | 5 | 6.33 | |
| Others | 11 | 7 | 8.53 | 4 | 5.06 | |
| Lymph node metastasis | ||||||
| Yes | 23 | 9 | 10.98 | 14 | 17.72 | 0.001 |
| No | 93 | 59 | 71.95 | 34 | 43.04 | |
| Unknown | 45 | 14 | 17.07 | 31 | 39.24 | |
Multivariate analysis of chemoresistance in ovarian cancer
The surgical stage of the ovarian cancer patients, the positive expression of NF-κB p65 and PTEN protein, and occurrence of lymph node metastasis were used as dependent variables in the multivariate logistic regression analysis. The results suggested that the surgical stage, NF-κB and PTEN were independent risk factors that closely associated with the chemoresistance of ovarian cancer (P < 0.05) (Table 3).
Table 3.
Multivariate analysis of ovarian cancer chemoresistance
| Factors | β-value | SE | Wald χ2 | sig | Exp (β) | 95% CI for Exp (β) | |
|---|---|---|---|---|---|---|---|
|
| |||||||
| lower limit | upper limit | ||||||
| NF-κB p65 | 1.296 | 0.634 | 4.18 | 0.041 | 3.655 | 1.055 | 12.66 |
| PTEN | -1.387 | 0.432 | 10.313 | 0.001 | 0.25 | 0.107 | 0.582 |
| Surgical stage | 1.793 | 0.424 | 17.838 | < 0.001 | 6.005 | 2.614 | 13.799 |
Prognosis analysis
The Cox model was used to carry out univariate and multivariate analysis of the factors that affect the prognosis of ovarian cancer. The results showed that NF-κB, surgical stage and groups were independent risk factors associated with ovarian cancer prognosis (P < 0.05) (Table 4).
Table 4.
Cox model analysis of the prognosis of ovarian cancer patients
| β-value | SE | Wald χ2 | sig | Exp (β) | 95% CI for Exp (β) | ||
|---|---|---|---|---|---|---|---|
|
| |||||||
| lower limit | upper limit | ||||||
| Univariate analysis | |||||||
| Age | 0.549 | 0.241 | 5.188 | 0.023 | 1.732 | 1.080 | 2.779 |
| Surgical stage | 2.047 | 0.308 | 44.257 | < 0.001 | 7.748 | 4.239 | 14.163 |
| Pathological grade | -0.258 | 0.191 | 1.822 | 0.177 | 0.773 | 0.531 | 1.124 |
| Histological type | -0.176 | 0.098 | 3.226 | 0.072 | 0.839 | 0.692 | 1.016 |
| Lymph node metastasis | 0.462 | 0.125 | 13.659 | < 0.001 | 1.587 | 1.242 | 2.027 |
| NF-κB p65 | 2.050 | 0.490 | 17.525 | < 0.001 | 7.765 | 2.974 | 20.271 |
| PTEN | -0.756 | 0.278 | 7.378 | 0.007 | 0.470 | 0.272 | 0.810 |
| Groups | 3.565 | 0.470 | 57.465 | < 0.001 | 35.348 | 14.061 | 88.857 |
| Multivariate analysis | |||||||
| Age | -0.061 | 0.263 | 0.053 | 0.817 | 0.941 | 0.563 | 1.575 |
| Surgical stage | 0.837 | 0.365 | 5.265 | 0.022 | 2.310 | 1.130 | 4.721 |
| Lymph node metastasis | 0.094 | 0.141 | 0.445 | 0.505 | 1.099 | 0.833 | 1.448 |
| NF-κB p65 | 1.193 | 0.567 | 4.431 | 0.035 | 3.296 | 1.086 | 10.006 |
| PTEN | 0.556 | 0.311 | 3.199 | 0.074 | 1.744 | 0.948 | 3.210 |
| Groups | 3.316 | 0.517 | 41.138 | < 0.001 | 27.562 | 10.004 | 75.934 |
All 161 cases of ovarian cancer were followed up (up to December 2014), with a survival time of 7-85 months (mean: 42 months). The results of Kaplan-Meier analysis and log-rank tests showed that the survival rates of patients in the sensitive group, patients with surgical stage of I-II, no lymph node metastasis, positive expression of PTEN and negative expression of NF-κB were significantly higher than those in the resistant group, with surgical stage of III-IV, lymph node metastasis, negative expression of PTEN and positive expression of NF-κB. When the pathological grading and pathological types were used as the grouping criteria, there was no significant difference in survival rates between the groups (P > 0.05) (Figure 3).
Figure 3.
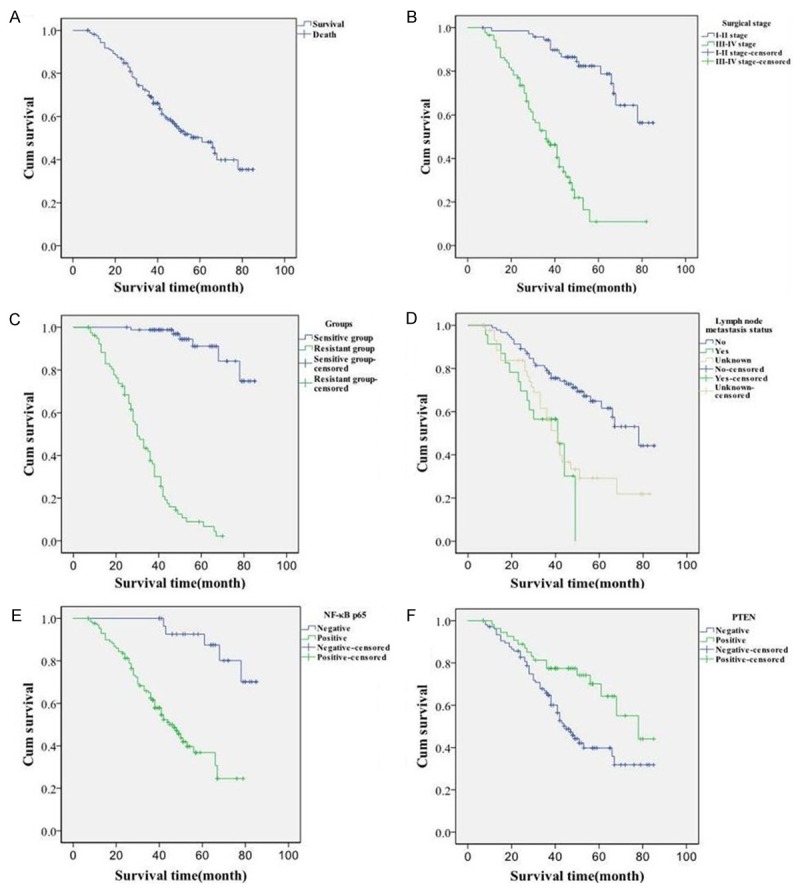
Prognosis analysis of the studied cohort. A: Survival curves of 161 patients with ovarian cancer, B-D: The survival curves of patients with surgical stage, grouping, presence of lymph node metastasis as grouping criteria, respectively; E, F: The survival curves of patients with positive or negative expression of NF-κB p65 and PTEN.
Discussion
Nuclear transcription factor κB (nuclear factor-κB, NF-κB) is an important multifunctional transcription factor, with a wide range of biological activities. Upon activation, NF-κB promotes the transcription of cellular factors, adhesion molecules, chemokines, etc. The NF-κB/Rel family consists of five subunits, c-Rel NF-κB1 (p50/p105), NF-κB2 (p52/p100), RelA (p65) and ReIB, and the most common dimer of NF-κB is the p50-p65 dimer. In the resting state, the p50-p65 dimer usually directly binds with its inhibitor IκB to form an inactive trimmer, which is present in the cytoplasm of almost all cells. When subjected to stimulation by external factors, NF-κB firstly dissociates with IκB, exposing its nuclear localization sequence. The p50-p65 dimer then rapidly translocates from the cytoplasm to the nucleus, and binds with its targeting sequence on the DNA, so as to regulate the transcription of the related gene [17]. Therefore, the expression of p65 can reflect the activity of NF-κB, and the expression of nuclear NF-κB protein can be considered a marker of NF-κB activation. NF-κB is the key in various transduction pathways, and is involved in the genetic regulation of various physiological and pathological processes, including immunity, inflammation, the occurrence and development of tumors, cell proliferation, apoptosis and autophagy, and angiogenesis. Studies have shown high expression of NF-κB in various malignant tumors, such as pancreatic cancer, breast cancer, colon cancer, and gastric cancer [18-21]. The activation of NF-κB plays an important role in increasing the proliferation of tumor cells, reducing apoptosis and autophagy of tumor cells, promoting the formation of new blood vessels within the tumor, enhancing the local invasion and distant metastasis of tumor cells, and promoting chemotherapy chemoresistance of tumor cells. The role of NF-κB in tumors may be related to the following aspects: (1) through upregulation of cyclin D1 transcription and regulation of the cell cycle, NF-κB promotes cell proliferation, eventually leading to malignant transformation, and canceration of the cells [22]; (2) NF-κB regulates the transcription of inhibitors of apoptosis proteins (IAP), anti-apoptotic gene Bcl-2, Bcl-XL, XIAP, etc., and inhibits cell apoptosis [23,24]; (3) by affecting the transcription of the autophagy-related gene Beclin-1/Bcl-2, NF-κB regulates autophagy [6]; (4) consistent activation of NF-κB could promote the abnormally high expression of important factors of angiogenesis, vascular endothelial growth factor (VEGF), IL-6 and IL-8, promoting angiogenesis in tumor tissues and the growth of tumors [25]; (5) in promoting the invasion and expansion of tumors, NF-κB not only regulates the expression of various chemotactic factors, which promotes cell migration, but also promotes the expression of matrix metalloproteinases (MMP) and urokinase plasminogen activator (u-PA), which facilitates invasion and metastasis of tumor cells [26]. Furthermore, recent studies have found that NF-κB also plays an important role in the development of tumor cell chemoresistance [7,8]. Many studies have found high expression of NF-κB in drug-resistant cancer cells. Eichholtz-Wirth H et al [27] found that the expression of NF-κB in the cervical carcinoma drug-resistant cell line Hela/B was higher than that in the sensitive cell line both at baseline and after cisplatin induction. The study by Mabuchi et al [28] showed that, in ovarian cancer cell lines, blocking NF-κB activation by its inhibitor SN50 promotes the apoptosis of ovarian cancer cells, enhances the sensitivity of cancer cells to cisplatin chemotherapy, and improves the efficacy of chemotherapy. The present study found that, among ovarian cancer patients, the positive expression rate of NF-κB in the resistant group was higher than that in the sensitive group. Univariate and multivariate analysis showed that NF-κB was an independent risk factor associated with chemotherapy chemoresistance in ovarian cancer, which, for the first time, demonstrated that NF-κB plays an important role in chemoresistance in ovarian carcinoma at the histological level. In addition, the survival rates of patients with positive expression of NF-κB in ovarian cancer tissues were lower than that of patients with negative expression of NF-κB. COX model analysis showed that NF-κB was an independent risk factor for chemoresistance in ovarian cancer.
PTEN is a tumor-suppressing gene with bispecific activity towards phosphatase and lipid phosphatase. Many studies have found that PTEN may be involved in the conduction of multiple signaling pathways, regulation of cell cycle, apoptosis and autophagy, cell adhesion and migration, be involved in angiogenesis and also play an important role in the transduction of multiple signaling pathways in cells. Studies have demonstrated genetic mutation and abnormal expression of PTEN in glioma, breast cancer, prostate cancer and other tumors, which play an important role in the occurrence and development of these tumors [29]. On the other hand, the expression level of PTEN in normal ovarian tissue, benign ovarian tumor, borderline ovarian tumors and ovarian cancer gradually decreased [30,31], indicating that down-regulation of PTEN may be involved in the occurrence and development of ovarian cancer. A number of in vitro studies showed that gene alterations of PTEN may be involved in the development of chemoresistance in tumors. Selvendiran et al found that the chemotherapeutic drug EF24 sensitizes cells to chemotherapy by upregulating PTEN protein expression in ovarian cancer cells [32]. Wu et al increased the PTEN protein expression in a cisplatin-resistant C13K ovarian cancer cell line by in vitro liposomal transfection of the PTEN gene, and the resultant cell lines showed higher sensitivity towards cisplatin compared with the cells transfected with empty plasmid [33]. The in vitro cancer cell study by Yan et al [34] demonstrated that PTEN protein can make the cisplatin-resistant ovarian cancer cell lines OV20028, CI3* and A2780 sensitive to chemotherapy by upregulating the expression of P53, rather than through inhibiting the activation of Akt protein. Compared with the primary ovarian cancer cell line OVCAR-3, the expression level of PTEN in drug-resistant ovarian cancer cell line OVCAR-3/CDDP was lower, which may lead to activation of classic PI3K/Akt apoptosis-inhibiting signaling pathways and the cisplatin resistance. Our previous study demonstrated decreased PTEN and BECN1 expression in ovarian cancer cells [35], with even more significant decrease in the drug-resistant ovarian cancer cells, suggesting that the low expression of PTEN was related to the chemoresistance of ovarian cancer. Improvement of chemoresistance in ovarian cancer may be related to decreasing autophagic activity, and PTEN may be involved in the process of autophagy to inhibit tumor growth. To further confirm the correlation between PTEN and chemotherapy resistance in human ovarian carcinoma, the expression of PTEN protein in cancer tissues of patients in the sensitive and resistant groups was determined. The positive expression rate of PTEN protein in the resistant group was significantly lower than that of the sensitive group. Moreover, PTEN was confirmed to be an independent risk factor of the chemoresistance in ovarian cancer through univariate and multivariate analysis, which, on the basis of previous research, proved for the first time that the absence of PTEN protein might be associated with the chemoresistance of ovarian cancer at the histological level. The functional mechanism of PTEN in the occurrence and development of ovarian cancer may be: (1) it is a classical cytokine that inhibits PI3K/AKT signaling transport with dual specificity towards phosphatase, which can decrease the PIP3 level by promoting dephosphorylation of PIP3 to form PIP2, thereby blocking the PI3K/AKT pathway, inducing cell cycle arrest at the G1 phase, promoting cell apoptosis and autophagy, and affecting the occurrence and development of tumor and chemoresistance [36]; (2) by suppressing the activation of ERK, phosphorylation of downstream SH2, activation of Ras, and phosphorylation of insulin receptor-1, PTEN inhibited the PTEN/ERK/MARK pathway, cell growth and differentiation [37]; (3) through its protein phosphatase activity, PTEN dephosphorylated the focal adhesion kinase and promoted phosphorylation of P130Cas to inhibit the migration and invasion of tumor cells [38]; (4) by controlling the invasiveness of cancer cells via stabilization of the cadherin-ring/beta adhesion junction complex, thereby playing a part in its anti-cancer role [39].
The study by Gustin et al [40] found that PTEN can inhibit the function of phosphatidylinositol-3-hydroxyl kinase, reduce the activation of serine/threonine protein kinase (Akt) and IκB kinase complex (IκB kinase, complex, IκK) by tumor necrosis factor (TNF), and inhibit the DNA binding and transcription of NF-κB. Another study [41] showed that PTEN can directly inhibit the transcription activating activity of NF-κB p65 to suppress cell proliferation and transcription of the anti-apoptosis gene, which inhibits cell proliferation and promotes cell apoptosis. Our study demonstrated that the positive expression rate of PTEN in the sensitive group was significantly higher than that in the resistant group. On the contrary, the positive expression of NF-κB p65 in the sensitive group was significantly lower than that in the resistant group. Both NF-κB and PTEN were independent risk factors for chemotherapy resistance in ovarian cancer, the expression levels of which in ovarian carcinoma were negatively correlated. Therefore, the down-regulation of PTEN may directly or indirectly activate NF-κB p65 involvement in the occurrence and development of the chemoresistance mechanism in ovarian cancer, which can both be used as predictors of multichemoresistance in ovarian carcinoma.
Acknowledgements
This work is financially supported by the National Natural Science Foundation of China (81372486).
Disclosure of conflict of interest
None.
References
- 1.Furukawa S, Soeda S, Kiko Y, Suzuki O, Hashimoto Y, Watanabe T, Nishiyama H, Tasaki K, Hojo H, Abe M, Fujimori K. MCP-1 promotes invasion and adhesion of human ovarian cancer cells. Anticancer Res. 2013;33:4785–90. [PubMed] [Google Scholar]
- 2.Lee S, Choi EJ, Jin C, Kim DH. Activation of PI3K/Akt pathway by PTEN reduction and PIK3CA mRNA amplification contributes to cisplatin resistance in an ovarian cancer cell line. Gynecol Oncol. 2005;97:26–34. doi: 10.1016/j.ygyno.2004.11.051. [DOI] [PubMed] [Google Scholar]
- 3.Yunos NM, Mutalip SS, Jauri MH, Yu JQ, Huq F. Anti-proliferative and pro-apoptotic effects from sequenced combinations of andrographolide and cisplatin on ovarian cancer cell lines. Anticancer Res. 2013;33:4365–71. [PubMed] [Google Scholar]
- 4.Morishita N, Tsukahara H, Chayama K, Ishida T, Washio K, Miyamura T, Yamashita N, Oda M, Morishima T. Activation of Akt is associated with poor prognosis and chemotherapeutic resistance in pediatric B-precursor acute lymphoblastic leukemia. Pediatr Blood Cancer. 2012;59:83–9. doi: 10.1002/pbc.24034. [DOI] [PubMed] [Google Scholar]
- 5.Karin M, Cao Y, Greten FR, Li ZW. NF-kappaB in cancer: from innocent bystander to major culprit. Nat Rev Cancer. 2002;2:301–10. doi: 10.1038/nrc780. [DOI] [PubMed] [Google Scholar]
- 6.Djavaheri-Mergny M, Amelotti M, Mathieu J, Besançon F, Bauvy C, Souquère S, Pierron G, Codogno P. NF-kappaB activation represses tumor necrosis factor-alpha-induced autophagy. J Biol Chem. 2006;281:30373–82. doi: 10.1074/jbc.M602097200. [DOI] [PubMed] [Google Scholar]
- 7.Montagut C, Tusquets I, Ferrer B, Corominas JM, Bellosillo B, Campas C, Suarez M, Fabregat X, Campo E, Gascon P, Serrano S, Fernandez PL, Rovira A, Albanell J. Activation of nuclear factor-kappa B is linked to resistance to neoadjuvant chemotherapy in breast cancer patients. Endocr Relat Cancer. 2006;13:607–16. doi: 10.1677/erc.1.01171. [DOI] [PubMed] [Google Scholar]
- 8.Holcomb B, Yip-Schneider M, Schmidt CM. The role of nuclear factor kappaB in pancreatic cancer and the clinical applications of targeted therapy. Pancreas. 2008;36:225–35. doi: 10.1097/MPA.0b013e31815b3207. [DOI] [PubMed] [Google Scholar]
- 9.Gil A, Andres-Pons A, Fernandez E, Valiente M, Torres J, Cervera J, Pulido R. Nuclear localization of PTEN by a Ran-dependent mechanism enhances apoptosis: Involvement of an N-terminal nuclear localization domain and multiple nuclear exclusion motifs. Mol Biol Cell. 2006;17:4002–13. doi: 10.1091/mbc.E06-05-0380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tang Y, Eng C. PTEN autoregulates its expression by stabilization of p53 in a phosphatase-independent manner. Cancer Res. 2006;66:736–42. doi: 10.1158/0008-5472.CAN-05-1557. [DOI] [PubMed] [Google Scholar]
- 11.Ogier-Denis E, Codogno P. Autophagy: a barrier or an adaptive response to cancer. Biochim Biophys Acta. 2003;1603:113–28. doi: 10.1016/s0304-419x(03)00004-0. [DOI] [PubMed] [Google Scholar]
- 12.Gozuacik D, Kimchi A. Autophagy as a cell death and tumor suppressor mechanism. Oncogene. 2004;23:2891–906. doi: 10.1038/sj.onc.1207521. [DOI] [PubMed] [Google Scholar]
- 13.Maehama T, Dixon JE. PTEN: a tumour suppressor that functions as a phospholipid phosphatase. Trends Cell Biol. 1999;9:125–8. doi: 10.1016/s0962-8924(99)01519-6. [DOI] [PubMed] [Google Scholar]
- 14.Mutter GL, Lin MC, Fitzgerald JT, Kum JB, Baak JP, Lees JA, Weng LP, Eng C. Altered PTEN expression as a diagnostic marker for the earliest endometrial precancers. J Natl Cancer Inst. 2000;92:924–30. doi: 10.1093/jnci/92.11.924. [DOI] [PubMed] [Google Scholar]
- 15.Song MS, Salmena L, Pandolfi PP. The functions and regulation of the PTEN tumour suppressor. Nat Rev Mol Cell Biol. 2012;13:283–96. doi: 10.1038/nrm3330. [DOI] [PubMed] [Google Scholar]
- 16.Zhuang HQ, Wang J, Yuan ZY, Zhao LJ, Wang P, Wang CL. The drug-resistance to gefitinib in PTEN low expression cancer cells is reversed by irradiation in vitro. J Exp Clin Cancer Res. 2009;28:123. doi: 10.1186/1756-9966-28-123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Siebenlist U, Franzoso G, Brown K. Structure, regulation and function of NF-kappa B. Annu Rev Cell Biol. 1994;10:405–55. doi: 10.1146/annurev.cb.10.110194.002201. [DOI] [PubMed] [Google Scholar]
- 18.Liu A, Chen H, Tong H, Ye S, Qiu M, Wang Z, Tan W, Liu J, Lin S. Emodin potentiates the antitumor effects of gemcitabine in pancreatic cancer cells via inhibition of nuclear factor-kappaB. Mol Med Rep. 2011;4:221–7. doi: 10.3892/mmr.2011.414. [DOI] [PubMed] [Google Scholar]
- 19.Ko HS, Lee HJ, Kim SH, Lee EO. Piceatannol suppresses breast cancer cell invasion through the inhibition of MMP-9: involvement of PI3K/AKT and NF-kappaB pathways. J Agric Food Chem. 2012;60:4083–9. doi: 10.1021/jf205171g. [DOI] [PubMed] [Google Scholar]
- 20.Kojima M, Morisaki T, Sasaki N, Nakano K, Mibu R, Tanaka M, Katano M. Increased nuclear factor-kB activation in human colorectal carcinoma and its correlation with tumor progression. Anticancer Res. 2004;24:675–81. [PubMed] [Google Scholar]
- 21.Sasaki N, Morisaki T, Hashizume K, Yao T, Tsuneyoshi M, Noshiro H, Nakamura K, Yamanaka T, Uchiyama A, Tanaka M, Katano M. Nuclear factor-kappaB p65 (RelA) transcription factor is constitutively activated in human gastric carcinoma tissue. Clin Cancer Res. 2001;7:4136–42. [PubMed] [Google Scholar]
- 22.Guttridge DC, Albanese C, Reuther JY, Pestell RG, Baldwin AS Jr. NF-kappaB controls cell growth and differentiation through transcriptional regulation of cyclin D1. Mol Cell Biol. 1999;19:5785–99. doi: 10.1128/mcb.19.8.5785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pommier Y, Sordet O, Antony S, Hayward RL, Kohn KW. Apoptosis defects and chemotherapy resistance: molecular interaction maps and networks. Oncogene. 2004;23:2934–49. doi: 10.1038/sj.onc.1207515. [DOI] [PubMed] [Google Scholar]
- 24.Takada Y, Kobayashi Y, Aggarwal BB. Evodiamine abolishes constitutive and inducible NF-kappaB activation by inhibiting IkappaBalpha kinase activation, thereby suppressing NF-kappaB-regulated antiapoptotic and metastatic gene expression, up-regulating apoptosis, and inhibiting invasion. J Biol Chem. 2005;280:17203–12. doi: 10.1074/jbc.M500077200. [DOI] [PubMed] [Google Scholar]
- 25.Pahl HL. Activators and target genes of Rel/NF-kappaB transcription factors. Oncogene. 1999;18:6853–66. doi: 10.1038/sj.onc.1203239. [DOI] [PubMed] [Google Scholar]
- 26.Trusolino L, Comoglio PM. Scatter-factor and semaphorin receptors: cell signalling for invasive growth. Nat Rev Cancer. 2002;2:289–300. doi: 10.1038/nrc779. [DOI] [PubMed] [Google Scholar]
- 27.Eichholtz-Wirth H, Sagan D. IkappaB/NF-kappaB mediated cisplatin resistance in HeLa cells after low-dose gamma-irradiation is associated with altered SODD expression. Apoptosis. 2000;5:255–63. doi: 10.1023/a:1009656513307. [DOI] [PubMed] [Google Scholar]
- 28.Mabuchi S, Ohmichi M, Nishio Y, Hayasaka T, Kimura A, Ohta T, Saito M, Kawagoe J, Takahashi K, Yada-Hashimoto N, Sakata M, Motoyama T, Kurachi H, Tasaka K, Murata Y. Inhibition of NFkappaB increases the efficacy of cisplatin in in vitro and in vivo ovarian cancer models. J Biol Chem. 2004;279:23477–85. doi: 10.1074/jbc.M313709200. [DOI] [PubMed] [Google Scholar]
- 29.Li J, Yen C, Liaw D, Podsypanina K, Bose S, Wang SI, Puc J, Miliaresis C, Rodgers L, McCombie R, Bigner SH, Giovanella BC, Ittmann M, Tycko B, Hibshoosh H, Wigler MH, Parsons R. PTEN, a putative protein tyrosine phosphatase gene mutated in human brain, breast, and prostate cancer. Science. 1997;275:1943–7. doi: 10.1126/science.275.5308.1943. [DOI] [PubMed] [Google Scholar]
- 30.Laudanski P, Kowalczuk O, Klasa-Mazurkiewicz D, Milczek T, Rysak-Luberowicz D, Garbowicz M, Baranowski W, Charkiewicz R, Szamatowicz J, Chyczewski L. Selective gene expression profiling of mTOR-associated tumor suppressor and oncogenes in ovarian cancer. Folia Histochem Cytobiol. 2011;49:317–24. doi: 10.5603/fhc.2011.0044. [DOI] [PubMed] [Google Scholar]
- 31.Skirnisdottir I, Seidal T. Prognostic impact of concomitant p53 and PTEN on outcome in early stage (FIGO I-II) epithelial ovarian cancer. Int J Gynecol Cancer. 2011;21:1024–31. doi: 10.1097/IGC.0b013e31821dc906. [DOI] [PubMed] [Google Scholar]
- 32.Selvendiran K, Tong L, Vishwanath S, Bratasz A, Trigg NJ, Kutala VK, Hideg K, Kuppusamy P. EF24 induces G2/M arrest and apoptosis in cisplatin-resistant human ovarian cancer cells by increasing PTEN expression. J Biol Chem. 2007;282:28609–18. doi: 10.1074/jbc.M703796200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wu HJ, Wu HT, Weng DH, Xing H, Lu YP, Ma D. Reversal of chemoresistance in human ovarian cancer cells by wild-type PTEN gene and its mechanisms. Zhonghua Fu Chan Ke Za Zhi. 2007;42:612–6. [PubMed] [Google Scholar]
- 34.Yan X, Fraser M, Qiu Q, Tsang BK. Over-expression of PTEN sensitizes human ovarian cancer cells to cisplatin-induced apoptosis in a p53-dependent manner. Gynecol Oncol. 2006;102:348–55. doi: 10.1016/j.ygyno.2005.12.033. [DOI] [PubMed] [Google Scholar]
- 35.Ying H, Qu D, Liu C, Liu C, Ying T, Lv J, Jin S, Xu H. Chemoresistance is associated with Beclin-1 and PTEN expression in epithelial ovarian cancers. Oncol Lett. 2015;9:1759–1763. doi: 10.3892/ol.2015.2950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bouali S, Chretien AS, Ramacci C, Rouyer M, Becuwe P, Merlin JL. PTEN expression controls cellular response to cetuximab by mediating PI3K/AKT and RAS/RAF/MAPK downstream signaling in KRAS wild-type, hormone refractory prostate cancer cells. Oncol Rep. 2009;21:731–5. [PubMed] [Google Scholar]
- 37.Gu J, Tamura M, Yamada KM. Tumor suppressor PTEN inhibits integrin- and growth factor-mediated mitogen-activated protein (MAP) kinase signaling pathways. J Cell Biol. 1998;143:1375–83. doi: 10.1083/jcb.143.5.1375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Diao L, Chen YG. PTEN, a general negative regulator of cyclin D expression. Cell Res. 2007;17:291–2. doi: 10.1038/cr.2007.24. [DOI] [PubMed] [Google Scholar]
- 39.Kotelevets L, van Hengel J, Bruyneel E, Mareel M, van Roy F, Chastre E. Implication of the MAGI-1b/PTEN signalosome in stabilization of adherens junctions and suppression of invasiveness. FASEB J. 2005;19:115–7. doi: 10.1096/fj.04-1942fje. [DOI] [PubMed] [Google Scholar]
- 40.Gustin JA, Maehama T, Dixon JE, Donner DB. The PTEN tumor suppressor protein inhibits tumor necrosis factor-induced nuclear factor kappa B activity. J Biol Chem. 2001;276:27740–4. doi: 10.1074/jbc.M102559200. [DOI] [PubMed] [Google Scholar]
- 41.Mayo MW, Madrid LV, Westerheide SD, Jones DR, Yuan XJ, Baldwin AS Jr, Whang YE. PTEN blocks tumor necrosis factor-induced NF-kappa B-dependent transcription by inhibiting the transactivation potential of the p65 subunit. J Biol Chem. 2002;277:11116–25. doi: 10.1074/jbc.M108670200. [DOI] [PubMed] [Google Scholar]


