Abstract
Purpose/Background
Assessment of postural sway with force plates can be affected by type of measurement and various clinical parameters such as age and activity level of the individual person. For this reason, variability is detected in postural reactions of healthy subjects without balance impairment. Test‐retest reliability of postural sway in adolescent athletes has been measured using a force plate and additional test‐retest studies have been suggested for subjects of different age groups with different activity levels. Therefore, the purpose of this research was to assess test‐retest reliability of Tetrax® Static Posturography in young adults with low physical activity level, and examine the relationship between posturography results and low activity level.
Methods
Young adults older than 18 years of age were included in the study. Demographic characteristics of the cases were recorded including age, weight, height, body mass index (BMI, kg/m2) and dominant extremity. Number of falls in the previous six months, lower body endurance (sit to stand test) and single‐leg eyes closed stance test were recorded. Activity level of participants was determined according to the International Physical Activity Questionnaire (IPAQ). Posturographic evaluation of all volunteers was completed using the Tetrax® Interactive Postural Balance System (Sunlight Medical Ltd, Israel). Fall risk and general stability index (SI) calculated by the Tetrax® were recorded. Following the first test, measurements were repeated 24 to 48 hours later for reliability purposes.
Results
Sixty‐five subjects (28 male, 37 female; mean age 22.2 ± 1.1 years, mean BMI 22.6 ± 3.3 kg/m2) were evaluated. All participants were classified as minimally active according to mean IPAQ score (1042.1 ± 517.7 [231 – 2826] MET‐ minutes per week). ICC scores between the first and second tests for fall index and total stability index were excellent (ICC2,1=0.858, 0.850, respectively). Fall risk determined by using the Tetrax® device was negatively correlated with lower body endurance (p=0.001, r=‐0.446), vigorous activity score (p=0.011, ‐0.312) and total activity score (p=0.029, r=‐0.271), and positively correlated with single leg stance score (p=0.001, r=0.606). There was a weak correlation between fall risk history and the fall risk determined by using Tetrax® device (p=0.04, r=0.255). There were no correlations between fall risk and height, weight, and BMI (p>0.05).
Conclusions
The results demonstrated the high test‐retest reliability of Tetrax® interactive balance system in young healthy adults with low physical activity level. Future studies are needed to determine the effectiveness of increasing physical activity level on postural control.
Level of Evidence
III
Keywords: Balance, physical activity level, static posturography
INTRODUCTION
Postural stability requires complex integration of multiple inputs from the vestibular, visual, and somoto‐sensory organs in the central and peripheral nervous systems. Adults with high postural sway and diminished postural control fall more frequently and due to these falls may have a higher fracture risk than subjects with good postural control. Falls resulting in fracture or other musculoskeletal injury have personal, economic, and social consequences along with immobilization and morbidity.1‐4 Although postural stability disorders are diagnosed more frequently in the older population, higher fall risk and fracture incidence have been reported in the literature that examines young adults with poor postural stability and excessive postural sway.4‐6 In addition, more than 97 % of most frequently encountered upper extremity fractures in young adults have been reported to occur due to falls.5 Diagnosis of postural disorders, prevention of falls, and rehabilitation of postural stability are all important issues in decreasing health expenses.
Several methods are used for evaluation of postural control in clinical practice including static and dynamic posturography.7 Static or dynamic computerized posturography gives quantitative data while evaluating the vestibular, visual and somoto‐sensory systems. Therefore, sensitivity and specificity of this evaluation method is higher than the other methods in terms of diagnosis of specific organ systems causing postural stability disorders.8 On the other hand, static computerized posturography has an advantage of shorter evaluation period and less expensive equipment compared to dynamic computerized posturography devices.7 However, intrinsic variability of the body's center of pressure (COP), age of the patient, and equipment used in testing are all variables affecting reliability and validity of this method for obtaining quantitative measurements.7,9
It has been reported that type of the measurement, age of the patient, comorbidities, and difficulty levels of balance tasks all affect posturography results.10 For this reason, variability in results of posturography measurements are seen in the postural reactions of healthy subjects without balance impairment. This variability results in unreliable outcomes, and there is limited and inconclusive research available regarding the test‐retest reliability of posturography devices.10‐12 Therefore, it has been suggested that while evaluating test‐retest reliability, homogenous groups of subjects in specific age groups should be utilized in studies to decrease inter‐subject variability in balance reactions.13‐15
Test‐retest reliability of postural sway evaluation measured with force plates in adolescent athletes has been reported and further test‐retest studies have been suggested for different age groups and for subjects with a variety of activity levels.16 The Tetrax® Interactive Static Posturography System (Tetrax°) (Sunlight Medical Ltd, Israel) has been used to measure postural stability in several previous studies evaluating different age groups and various patient populations.17‐21 However, to the authors' knowledge, the Tetrax° device has not been tested for reliability in young adults with low physical activity level. Therefore, the purpose of this research was to assess test‐retest reliability of Tetrax® Static Posturography in young adults with low physical activity level, and examine the relationship between posturography results and low activity level.
MATERIALS AND METHODS
Young adults older than 18 years of age who were minimally physical active as defined by the International Physical Activity Questionnaire (IPAQ) were included in the study.22 The IPAQ short version was used to define daily activity levels and frequency of activities of the subjects. The questionnaire includes information about vigorous physical activity duration (soccer, basketball, aerobic, fast bicycling, weight lifting, heavy labor, etc.), moderate physical activity duration (light weight laboring, moderate bicycling, traditional dancing, dancing, bowling, table tennis, etc), duration of daily walking, and duration of daily sitting in minutes. Total physical activity score as a basal metabolic equivalent (Metabolic Equivalent Task‐MET minutes per week) can be calculated according to the data obtained from IPAQ. Total physical activity score of participants was classified as inactive (less than 600 MET minutes per week), minimally active (between 600 to 3000 MET minutes per week), and active (more than 3000 MET minutes per week) according to recommendations in the IPAQ.22
Exclusion criteria included history of inflammatory disease, inner ear disorder impairing postural stability, history or current complaint of vertigo or dizziness, marked visual impairment, orthopedic disability or history of surgery related to lower limbs, neurological disorders and peripheral neuropathy, and athletic participation in sports (participation in any type of sports, including recreational exercise at least 4 days/week). Ethical approval was obtained from ethical committee of Pamukkale University Medical Faculty.
Volunteers who met the aforementioned inclusion/exclusion criteria were enrolled in the study. Demographic and anthropometric characteristics of the subjects were recorded including age, weight, height, body mass index (BMI) in kg/m2, occupation, and dominant extremity. Number of falls in the prior six months was recorded. A fall was defined as an unintentional episode of a fall to the ground.23 Falls which were the result of fainting, dizziness, loss of consciousness, sustaining a violent blow, or other overwhelming external factor were excluded. Sleep quality of the subjects were also recorded using Sleep Quality Numeric Rating Scale that assesses the quality of sleep in the previous 24 hours on a numeric rating scale ranging from 0 (best possible sleep) to 10 (worst possible sleep).24
Functional status of the participants was evaluated with lower body endurance (sit to stand test) and single‐limb eyes closed stance test.25 Lower‐body endurance was tested with the subject sitting on a stable chair with the seat height of approximately 43 cm with arms crossed over the chest, and then asked to perform as many sit to stand repetitions as possible in 30 seconds. Total number of stands executed was used as the test value. Higher values indicate better lower body endurance.25
For the single limb stance test, participants were asked to stand as long as possible on their extended dominant leg with eyes closed. During this test, the knee of the non‐dominant side was fully flexed and fixed on gluteal region by ipsilateral hand. When the subject lost balance, he or she was allowed to touch contralateral foot to the ground. Loss of balance was defined as the touch of contralateral foot to the ground. The number of balance losses in 30 seconds was recorded, therefore higher values indicated worse results.26 After each break, the same position was repeated until the 30 seconds session was completed for the single limb stance test.
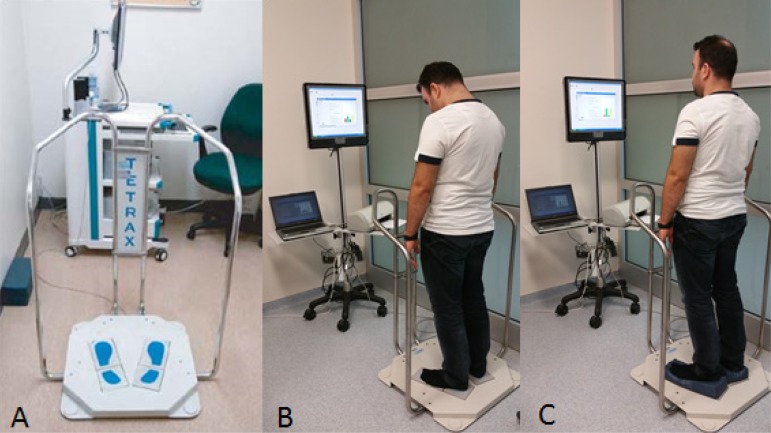
Postural control assessment was performed before functional tests in order to prevent the possibility of fatigue. Posturographic evaluation was performed with the Tetrax°. This system involves evaluation of static postural balance by recording vertical pressure fluctuations in four different power plates when the subject is standing barefoot on the device with the arms freely hanging next to the body. Hand pieces are present on both sides of the device that allows subjects to use these metal bars for stability when needed. The Tetrax° has a computer and dedicated software system, from which all the data were obtained. (Figure 1) Input from the plates is integrated and processed by a computer. Subjects were instructed to begin by placing their feet side by side on lined places of plates in shape of feet, not to speak and move during task. Measurements are made in eight different conditions, each with the same technique, sequence, and directions (each position takes about 40 seconds): (i) head straight, eyes open, on hard ground; (ii) head straight, eyes closed, on hard ground; (iii) head straight, eyes open, on soft ground (foam under feet); (iv) head straight, eyes closed, on soft ground; (v) head turned to the right, eyes closed, on hard ground; (vi) head turned to the left, eyes closed on hard ground; (vii) neck fully extended, eyes closed, on hard ground; and (viii) neck fully flexed, eyes closed, on hard ground. Vestibular, visual and somoto‐sensorial inputs are recorded in each of the eight different positions to evaluate static postural balance and fall risk.20
Figure 1.
Static posturography device and two positions of eight different positions shown as examples. A, Tetrax® static posturography device (Sunlight Medical, Israel). B, Neck fully flexed, eyes closed, on hard ground. C, Head straight, eyes open, on soft ground (foam under feet)
Measurements were performed at the same time period during the day (around 11:00 am). Following the first test, measurements are repeated 24 to 48 hours later. For each subject, fall risk and general stability index (SI) as calculated by the Tetrax° were recorded. Higher stability index and fall risk shows poorer postural performance. Fall risk obtained from the Tetrax° is a numerical value in between 0 and 100 (low fall risk, 0‐35; moderate fall risk, 36‐57; high fall risk, 58‐100).20
Data were analyzed with Statistical Package for Social Sciences software (SPSS Version 17, Chicago, IL, USA). Descriptive statistics (including mean ± standard deviation, frequency, and percentage) were calculated. Intra‐class correlation coefficient (ICC with the confidence interval 95%) was used to examine test‐retest reliability of postural balance data from the device. ICC score in the range of 0.00‐0.49 was considered poor, 0.50‐0.74 moderate and 0.75‐1.00 excellent reliability.27 Spearman correlation analysis was used to examine the correlation between fall risk and clinical variables. Statistical significance was set at p < 0.05. An a priori power analysis revealed that 65 subjects should be included in the study for 80 % power (D=0.015, β = 20, α = 0.05).
RESULTS
Sixty‐five subjects (28 male, 37 female; mean age 22.2 ± 1.1 years, mean height 1.70 ± 0.1 meters, mean weight 65.9 ± 13.4 kg, mean BMI 22.6 ± 3.3) were included in the study. In 56 (86.2%) of the subjects, dominant extremity was right side. Mean total physical activity score of the subjects was 1042.1 ± 517.7 (MET‐minutes per week) and mean sitting duration was 661.8 ± 105.5 (minute per day). Demographic and clinical characteristics of the patients are summarized in Table 1.
Table 1.
Demographic, clinical and posturographic data of the subjects
| N = 65 | Mean ± Standard Deviation (Min‐Max) |
|---|---|
| Age (years) | 22.2 ± 1.1 (20 ‐ 25) |
| Height (meters) | 1.70 ± 0.1 (1.55 ‐ 1.94) |
| Weight (kg) | 65.9 ± 13.4 (43 ‐ 95) |
| Body Mass Index (kg/m2) | 22.6 ± 3.3 (16.2 ‐ 31.9) |
| Sleep Quality in previous 24 hours | 3.1 ± 1.9 (0 ‐ 10) |
| Fall number in previous 6 months | 0.1 ± 0.3 (0 ‐ 2) |
| Sit to stand test (Number.of stands/30 sec.) | 18.9 ± 3.4 (14 ‐ 28) |
| Single limb stance test (Number of balance losses/30 sec.) | 1.4 ± 1.4 (0 ‐ 5) |
| Vigorous physical actvitiy (MET‐min/week) | 113.2 ± 266.0 (0‐1140) |
| Moderate physical activity (MET‐ min/ week) | 126.5 ± 224.6 (0‐720) |
| Walking activity (MET‐ min/week) | 802.4 ± 418.2 (231‐2772) |
| Total physical activity (MET‐ minutes per week) | 1042.1 ± 517.7 (231‐2826) |
| Sitting duration (min/day) | 661.8 ± 105.5 (480‐900) |
MET = Metabolic Equivalent Task
ICC's between first and second tests for fall index (0.858) and total stability index (0.850) were excellent. ICC values of first and second measurements for fall index, total SI, and ICC values of stability index of eight different positions of the subjects are presented in Table 2.
Table 2.
Fall index ansd stability index values of cases in first and second posturographic tests
| N = 65 | First Postrurography | Second Posturography | p | ICC, (min‐max) |
|---|---|---|---|---|
| Fall Index | 47.9 ± 26.6 (2‐100) | 48.6 ± 25.5 (6‐100) | 0.001 | 0.858 (0.768‐0.914) |
| Total Stability Index | 185.3 ± 46.7 (108.4‐341.2) | 180.7 ± 45.0 (107.0‐362.7) | 0.001 | 0.850 (0.755‐0.909) |
| NO SI |
18.8 ± 6.3 (10.4‐37.5) | 17.9 ± 5.1 (10.8‐38.6) | 0.001 | 0.746 (0.583‐0.845) |
| NC SI |
22.2 ± 6.1 (13.1‐40.9) | 21.4 ± 5.6 (13‐41) | 0.001 | 0.818 (0.702‐0.889) |
| PO SI |
19.1 ± 4.6 (12.7‐34.7) | 19.2 ± 6.3 (8.4‐54.4) | 0.006 | 0.470 (0.132‐0.677) |
| PC SI |
26.9 ± 5.4 (17.1‐41.7) | 26.3 ± 7.3 (16.3‐50.2) | 0.001 | 0.740 (0.574‐0.841) |
| HR SI |
23.9 ± 6.1 (13.4‐42.5) | 24.1 ± 6.8 (11.2‐57.4) | 0.001 | 0.832 (0.724‐0.897) |
| HL SI |
23.3 ± 7.2 (9.4‐54.2) | 24.3 ± 9.7 (11.5‐80.7) | 0.001 | 0.679 (0.474‐0.804) |
| HB SI |
24.7 ± 7.8 (12.7‐46.6) | 24.9 ± 8.0 (11.2‐54.4) | 0.001 | 0.863 (0.775‐0.916) |
| HF SI |
23.6 ± 7.4 (12.2‐51.1) | 22.4 ± 6.6 (7.9‐39.8) | 0.001 | 0.864 (0.777‐0.917) |
NO = Head straight, eyes open, on hard ground; NC = Head straight, eyes closed, on hard ground;
PO,=Head straight, eyes open, on soft ground; PC = Head straight, eyes closed, on soft ground;
HR = Head turned to right, eyes closed, on hard ground; HL = Head turned to left, eyes closed, on hard ground;
HB = Servical extension, eyes closed, on hard ground; HF=Cervical flexion, eyes closed, on hard ground.
SI = Stability index; higher values indicate worse postural stability.
ICC = Intraclass correlation coefficient.
Relationships between fall risk obtained from posturographic evaluation and clinical parameters are summarized on Table 3. Fall risk determined by using Tetrax® device in minimaly active young adults was weakly negatively correlated with lower body endurance (p=0.001, r=‐0.446), vigorous activity score (p=0.011, ‐0.312) and total activity score (p=0.029, r=‐0.271), and moderately positively correlated with single limb stance score (p=0.001, r=0.606). There was a weak correlation between fall risk history and the fall risk determined by using Tetrax® device (p=0.04, r=0.255). There were no correlations between fall risk and height, weight, and BMI (p>0.05).
Table 3.
Relationships between fall risk and clinical parameters.
| N = 65 | p | r |
|---|---|---|
| Fall Risk – Age | 0.663 | 0.055 |
| Fall Risk – Height | 0.424 | 0.101 |
| Fall Risk – Weight | 0.551 | −0.075 |
| Fall Risk – Body Mass Index | 0.193 | −0.163 |
| Fall Risk – Sleep Quality | 0.874 | −0.020 |
| Fall Risk – Number of falls in last 6 months | 0.113 | 0.199 |
| Fall Risk – Previous Fall history | 0.040* | 0.255 |
| Fall Risk – Sit to stand test | 0.001* | −0.446 |
| Fall Risk – One leg stance | 0.001* | 0.606 |
| Fall Risk – Vigorous activity score | 0.011* | −0.312 |
| Fall Risk – Moderate activity score | 0.199 | 0.162 |
| Fall Risk – Walking score | 0.074 | −0.223 |
| Fall Risk – Total Physical activity score | 0.029* | −0.271 |
| Fall Risk – Daily sitting duration | 0.157 | −0.178 |
p<0.05
DISCUSSION
The most important finding of this study is that test‐retest reliability of Tetrax® Static Posturography System is high for output values for fall risk and stability index in young adults with low physical activity level. According to the results of this study, as the lower body endurance, vigorous activity score, and total activity score increase, Tetrax® measured fall risk decreases. Additionally, significant positive correlation was detected between score of single limb stance (number of balance losses in 30 seconds) and Tetrax® measured fall risk, indicating that greater losses of balance occur there is a greater fall risk.
In previous studies, postural control has been evaluated with force plates, and validity of test‐retest reliability in young athletes has been reported.16 However, test‐retest reliability of Tetrax® static posturography system in young adults with low physical activity level has not been previously investigated. Test‐retest reliability of postural stability scores with Tetrax® has been demonstrated with no learning effect in older women and autistic children.20,21 Similarly, there was no significant difference between the first and second evaluation of fall risk with Tetrax® in young adults with low physical activity level. This supports the theory that learning effect does not influence the results in this system. Fall risk determined by using Tetrax® device in sedentary young adults was weakly negatively correlated with lower body endurance, vigorous activity score and total activity score. In addition, only a weak correlation between fall risk and number of falls at last six months existed in healthy young adults with low activity in our study. The weak correlation between number of falls in the previous six months and fall risk may be attributed to the low population size that reported falls in the previous six months in this group of subjects. Therefore, investigation of the effects of increasing physical activity level on fall risk in young adults in further prospective randomized studies using this reliable assessment method will provide additional results, which could assist in planning rehabilitation programs for prevention of fall risk.
In addition to specific vestibular or central disorders causing postural stability disturbances, visual problems and other sensorimotor problems due to aging have been described as resulting in deterioration of balance.18,28 However, there was no correlation between fall risk and age of the subjects in our study. Strict exclusion criteria, and homogenous distribution of the young adults in terms of age might have resulted in this finding. Larger groups with more heterogeneous distribution of age of the subjects in future studies will allow for evaluation of the correlation between fall risk and age.
Postural stability of healthy subjects before and after a 24‐hour sleepless period was evaluated in a previous study, and it was reported that fatigue due to sleeplessness might affect the postural stability.29 Therefore, all of the current subjects were evaluated at almost the same time of day, in order to minimalize the potential effect of sleeplessness. The mean sleep quality of the subjects in the current study was approximately 3 (0=best possible sleep, 10=worst possible sleep). No relationship was detected between sleep quality and fall risk. This is likely due to homogenous distribution of the subjects in terms the overall good sleep quality experienced by the whole group.
One of the limitations of the current study is that data for fall frequency was recorded according to subjects' recall over the prior six months. Another limitation of the current study is that since the study population consisted of only young (20‐25 years of age) healthy adults with sedentary life styles, the results cannot be generalized to other age groups and patients with balance disorders or to more active young adults. Repeating the study in wider and heterogeneous group of patients will provide more detailed information about fall risk in different age groups and in specific disorders.
CONCLUSIONS
This results of this study demonstrate the high test‐retest reliability of Tetrax® interactive balance system for testing postural stability in young healthy adults with low physical activity levels. Correlations between performance measures related to endurance, activity level, and postural stability and fall risk exist.
REFERENCES
- 1.Tinetti ME. Clinical practice. Preventing falls in elderly persons. N Engl J Med. 2003;348(1):42–9. [DOI] [PubMed] [Google Scholar]
- 2.Cumming RG Salkeld G Thomas M Szonyi G. Prospective study of the impact offear of falling on activities of daily living, SF‐36 scores, and nursing homeadmission. J Gerontol A BiolSci Med Sci. 2000;55(5):299–305. [DOI] [PubMed] [Google Scholar]
- 3.Stel VS Smit JH Pluijm SM Lips P. Consequences of falling in older men and womenand risk factors for health service use and functional decline. Age Aging. 2004;33(1):58–65. [DOI] [PubMed] [Google Scholar]
- 4.ONeill TW Marsden D Adams JE Silman AJ. Risk factors, falls, and fracture of the distal forearm in Manchester, UK. J Epidemiol Community Health. 1996;50(3):288–292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Goulding A Jones IE Taylor RW Piggot JM Taylor D. Dynamic and static tests of balance and postural sway in boys: effects of previous wrist bone fractures and high adiposity. Gait Posture. 2003;17(2):136‐41. [DOI] [PubMed] [Google Scholar]
- 6.Visser JE Carpenter MG van der Kooij H Bloem BR. The clinical utility of posturography. Clin Neurophysiol. 2008;119(11):2424‐36. [DOI] [PubMed] [Google Scholar]
- 7.Barozzi S1 Socci M Soi D Di Berardino F Fabio G Forti S Gasbarre AM Brambilla D Cesarani A. Reliability of postural control measures in children and young adolescents. Eur Arch Otorhinolaryngol. 2014;271(7):2069‐77. [DOI] [PubMed] [Google Scholar]
- 8.Tomaz A Ganança MM Garcia AP Kessler N Caovilla HH. Postural control in underachieving students. Braz J Otorhinolaryngol. 2014;80(2):105‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Baker CP Newstead AH Mossberg KA Nicodemus CL. Reliability of static standing balance in nondisabled children: comparison of two methods of measurement. Pediatr Rehabil. 1998;2(1):15–20 [DOI] [PubMed] [Google Scholar]
- 10.Geurts AC Nienhuis B Mulder TW. Intrasubject variability of selected forceplatformparameters in the quantification of postural control. Arch Phys Med Rehabil. 1993;74(11):1144–50. [PubMed] [Google Scholar]
- 11.Benvenuti F Mecacci R Gineprari I Bandinelli S Benvenuti E Ferrucci L, et al. Kinematic characteristics of standing disequilibrium: reliability and validity of aposturographic protocol. Arch Phys Med Rehabil. 1999;80(3):278–87. [DOI] [PubMed] [Google Scholar]
- 12.Helbostad JL Askim T Moe‐Nilssen R. Short‐term repeatability of body sway duringquiet standing in people with hemiparesis and in frail older adults. Arch Phys Med Rehabil. 2004;85(6):993–9. [DOI] [PubMed] [Google Scholar]
- 13.Ledin T Odkvist LM Vrethem M Moller C. Dynamic posturography in assessment of polyneuropathic disease. J Vestib Re.s 1990;1(2):123–8. [PubMed] [Google Scholar]
- 14.Baloh RW Fife TD Zwerling L Socotch T Jacobson K Bell T, et al. Comparison ofstatic and dynamic posturography in young and older normal people. J Am Geriatr Soc. 1994;42(4):405–12. [DOI] [PubMed] [Google Scholar]
- 15.Allum JH Carpenter MG Honegger F Adkin AL Bloem BR. Age‐dependent variationsin the directional sensitivity of balance corrections and compensatory armmovements in man. J Physiol. 2002;542:643–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Quatman‐Yates CC Lee A Hugentobler JA Kurowski BG Myer GD Riley MA. Test‐retest consistency of a posturalsway assessment protocol for adolescent athletes measured with a force plate. Int J Sports Phys Ther. 2013;8(6):741‐8. [PMC free article] [PubMed] [Google Scholar]
- 17.Dıraçog˘lu D Cihan C I˙s¸sever H Aydın R. Postural performance in patients with cervical radiculopathy. Turkish J Physc Ther Rehab. 2009;55(4):153‐7. [Google Scholar]
- 18.Oppenheim U Kohen‐Raz R Alex D Kohen‐Raz A Azarya M. Postural characteristics of diabetic neuropathy. Diabetes Care. 1999;22(2):328‐32. [DOI] [PubMed] [Google Scholar]
- 19.Akkaya N Akkaya S Atalay NS Acar M Catalbas N Sahin F. Assessment of the relationship between postural stability and sleep quality in patients with fibromyalgia. Clin Rheumatol. 2013;32(3):325‐31. [DOI] [PubMed] [Google Scholar]
- 20.Kohen‐Raz R, Application of tetra‐ataxiametric posturography in clinical and developmental diagnosis. Percept Mot Skills. 1991;73(2): 635–656. [DOI] [PubMed] [Google Scholar]
- 21.Schwesig R Kluttig A Leuchte S Becker S Schmidt H Esperer HD. The impact of different sports on posture regulation. Sportverletz Sportschaden. 2009. ;23(3):148‐54. [DOI] [PubMed] [Google Scholar]
- 22.Hagstromer M Oja P Sjostrom M. The International Physical Activity Questionnaire (IPAQ): a study of concurrent and construct validity. Public Health Nutr, 2006;9(6):755‐62. [DOI] [PubMed] [Google Scholar]
- 23.Tinetti ME Speechley M Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988; 319(26):1701‐7. [DOI] [PubMed] [Google Scholar]
- 24.Martin S Chandran A Zografos L Zlateva G. Evaluation of the impact of fibromyalgia on patients' sleep and the content validity of two sleep scales. Health and Quality of Life Outcomes. 2009;7:64‐70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lord SR Murray SM Chapman K Munro B Tiedemann A. Sit to stand performance depends on sensation speed, balance, and psychological status in addition to strength in older people. J Gerontol A BiolSci Med Sci. 2002; 57(8): M539‐43 [DOI] [PubMed] [Google Scholar]
- 26.Tomas‐Carus P Gusi N Hakinken A Hakinken K Raimundo A Ortega‐Alonso A. Improvements of muscle strength predicted benefits in HRQOL and postural balance in women with fibromyalgia: an 8‐month randomized controlled trial. Rheumatology (Oxford). 2009;48(9):1147‐51. [DOI] [PubMed] [Google Scholar]
- 27.Portney LG Watkins MP. Foundations of clinical research: applications to practice. Appleton & Lange, East Norwalk. 1993, pp 53‐67. [Google Scholar]
- 28.Schwartz S Segal O Barkana Y Schwesig R Avni I Morad Y. The effect of cataract surgery on postural control. Invest Ophthalmol Vis Sci. 2005;46(3):920‐4. [DOI] [PubMed] [Google Scholar]
- 29.Ma J Yao YJ Ma RM Li JQ Wang T Li XJ, et al. (2009) Effects of sleep deprivation on human postural control, subjective fatigue assessment and psychomotor performance. J Int Med Res. 37(5):1311‐20 [DOI] [PubMed] [Google Scholar]