Abstract
Background:
We aimed to identify risk factors associated with chronic low back pain (C-LBP) in Syria.
Materials and Methods:
We conducted the study in a busy outpatient neurology clinic in Damascus city from October 2011 to August 2012. We enrolled all eligible adults presenting with C-LBP along with those who denied any back pain as a controls. We considered C-LBP any LBP lasting over 3 months. We developed our own questionnaire. A clinical nurse interviewed each person and filled in the results.
Results:
We had a total of 911 subjects; 513 patients and 398 controls. We found that C-LBP increased with age. Having a sibling with C-LBP was a strong predictor of C-LBP. In women obesity, but not overweight, was a risk factor. Number of children was a risk factor for mothers. Higher level of education decreased the chance of C-LBP in women. Sedentary job increased the risk of C-LBP.
Conclusion:
This study sheds some light on risk factors for C-LBP in our population and might help find possible preventive measures.
Keywords: Family history, low back pain, obesity, waist circumference, waist to hip ratio
INTRODUCTION
Chronic low back pain (C-LBP) is a common complaint in neurology practices. It has a tremendous cost in sick-leave, management and pain and suffering.[1,2] The estimated annual prevalence is 10–13%.[3,4] C-LBP is estimated to be about 20% of all patients we see in the location of this study. The risk factors continue to be disputed.
Previous studies have yielded inconclusive results concerning the association between LBP and body mass index (BMI).[5,6,7] Other possible risk factors were studied; waist circumference (WC),[8,9,10] hip circumference (HC),[8] waist to hip ratio (WHR),[8,9,11,12] smoking,[2,8,13,14,15] hypertension,[4] diabetes mellitus,[4,14] marital status,[14,16] exercise,[2,16,17] depression,[4,14,18] anxiety,[14,18] and family history of LBP.[19,20] Inverse relationship was reported between education level and LBP.[13,21,22,23] Previous studies have also explored the association between LBP and work related factors such as lifting heavy objects,[16,20,24,25] bending,[24,25] and prolonged standing.[25]
To our knowledge, no previous study was carried out in Syria. Our objective is to clarify some of these risk factors in our population. We aim also to explore the effect of number of pregnancies and children particularly in a community where a high number is very common.[4]
MATERIALS AND METHODS
We conducted the study on C-LBP in adults (age 18-year-old and above) in a busy outpatient neurology clinic between October 2011 and August 2012. C-LBP was defined as any LBP lasting more than 3 months.[3,19,26]
Inclusion criteria
Patients who presented with C-LBP
Adults over the age of 18 years.
Exclusion criteria
Cancer, trauma or known vertebral fractures
Work-compensation claim or pending litigation related to the medical problem.
Informed consent was obtained from all those who agreed to participate, which complied with the principles outlined in Declaration of Helsinki (59th WMA General Assembly, Seoul, Korea, October 2008).
A questionnaire was filled by a nurse trained to interview each person. She filled in their answers and took their study required anthropomorphic measurements [Table S1]. WC was measured midway between the lower rib margin and the superior border of the iliac crest using a tape measure while the participant was standing with feet together and breathing gently.[27] We divided WC into groups (≤80, 81–90, 91–100, >100). HC was measured in centimeters. The measuring tape was placed around the maximum circumference of the buttocks in horizontal position.[28] We divided HC into groups (≤100, 101–110, 111–120, >120). We divided BMI in groups (<25 kg\m2, 25–29.99 overweight, ≥30 obese) and WHR in groups (≤0.8, >0.8, and ≤ 0.9, >0.9).
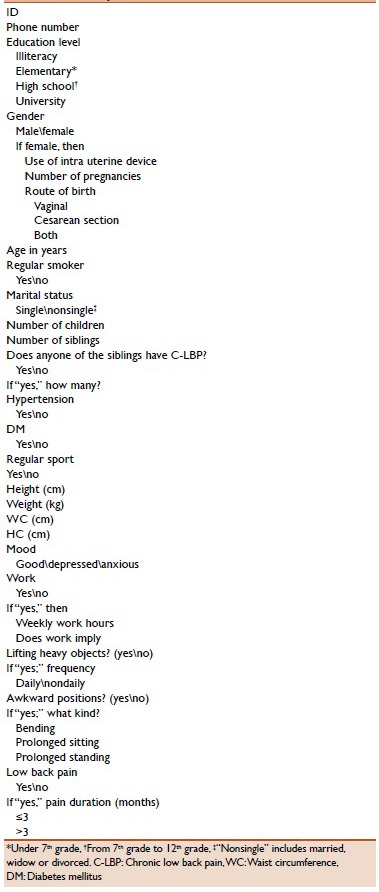
Table S1.
Supplementary material. Questionnaire for our C-LBP study
We had a total of 952 subjects who agreed to participate in the study. There were 398 control subjects and 554 C-LBP patients of whom 41 patients were excluded for not meeting inclusion criteria.
Control subjects are those who denied having any back pain at any time. We took our controls from family members or friends escorting patients with symptoms unrelated to back pain such as migraine, Parkinson's disease, stroke, and multiple sclerosis.
We divided participants into age groups; 18–30, 31–40, 41–50, 51–60, 61–70, and >70 years old. We categorized level of education as follows: Illiteracy, elementary (under 7th grade), high school (from 7th grade to 12th grade), and university (above high school). We asked about current smoking as a habit without specification of the amount. We took marital status as single and non-single (married, divorced, widow). We grouped subjects according to the number of their children: 1–3, 4–6 and >6 children. Patients with diabetes mellitus and systemic hypertension were categorized by their presence or absence. We inquired about the regular physical activity, but we did not inquire about type, duration or consistency. We asked if the patient has had anxiety or depression regardless of the onset of C-LBP. When asked about prolonged sitting or standing at work; we did not specify number of hours but asked if it was most of the time during work. We divided number of pregnancies into groups; 1–3, 4–6 and >6 pregnancies. Regarding the family history of LBP, we asked only about siblings. We thought this would provide more accurate and reliable information since we have many large families locally.
Statistical analysis
We tested factors associated with C-LBP in a univariate logistic regression model. In a next step, we tested all statistically significant variables from the univariate testing in a multiple logistic regression model. Descriptive statistics of frequencies and percentages were used to describe the variables. Odds ratios (OR) and corresponding 95% confidence intervals (95% CI) were used to analyze the data. The level of P < 0.05 was considered as a cut-off value for significance, and all P values were two-sided. The statistical package for Social Sciences, version 21.0 (SPSS Inc., Chicago, IL, USA) was used for all calculations.
RESULTS
A total of 911 subjects answered the questionnaire and met our inclusion criteria. There were 379 women and 134 men in the case group, and 263 women and 135 men in the control group. Subjects with C-LBP were more likely to be females. The largest number (105 women and 37 men) of those with C-LBP were between 41 and 50 years old [Figure 1].
Figure 1.
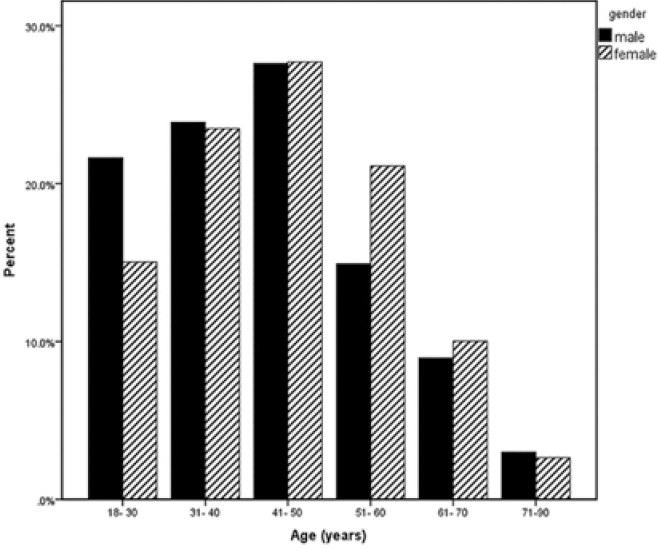
Percentages of chronic low back pain patients in different age groups with regard to total male and female patients separately (n = 134 males, 379 females)
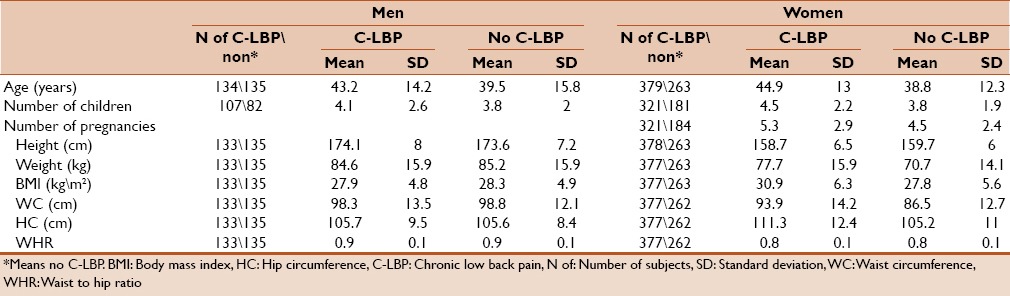
Table 1 presents means and standard deviations for some factors associated with C-LBP which are: Age, children number, pregnancies number, height, weight, BMI, WC, HC, and WHR. These variables are presented in men and women separately with\without C-LBP.
Table 1.
Means and SDs for some factors associated with C-LBP in men and women
Obesity (BMI ≥ 30) was found in 31.9% in control men and 30.4% in control women. We found 164 smokers (18%) in the whole group. Illiteracy was found in 46 (5%) subjects. Few women had more than 12 children.
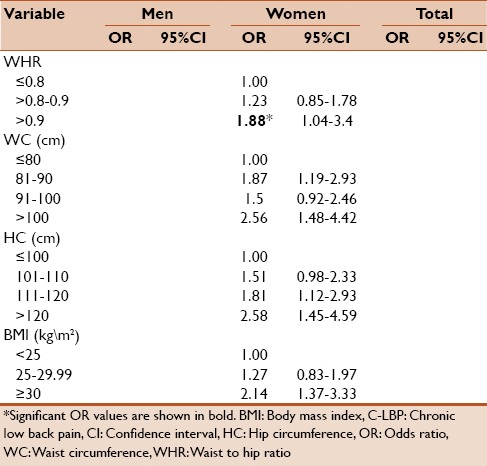
Table 2 presents OR (including 95% CI) as univariate analysis for education level, number of children, number of pregnancies, route of delivery, marital status, intra-uterine device use, and smoking in men and women separately. Table 3 presents OR (including 95% CI) as univariate analysis for BMI, WHR, WC, HC, hypertension, diabetes mellitus, regular sport, and family history in men and women separately. Table 4 presents OR (including 95% CI) as univariate analysis for work-hours per week, lifting heavy objects, bending, prolonged sitting, prolonged standing, and mood. Then we adjusted the significant results for age by using multiple logistic regressions [Tables 5 and 6].
Table 2.
Relative frequencies of men and women with and without C-LBP and factors associated with C-LBP tested by univariate logistic regression model
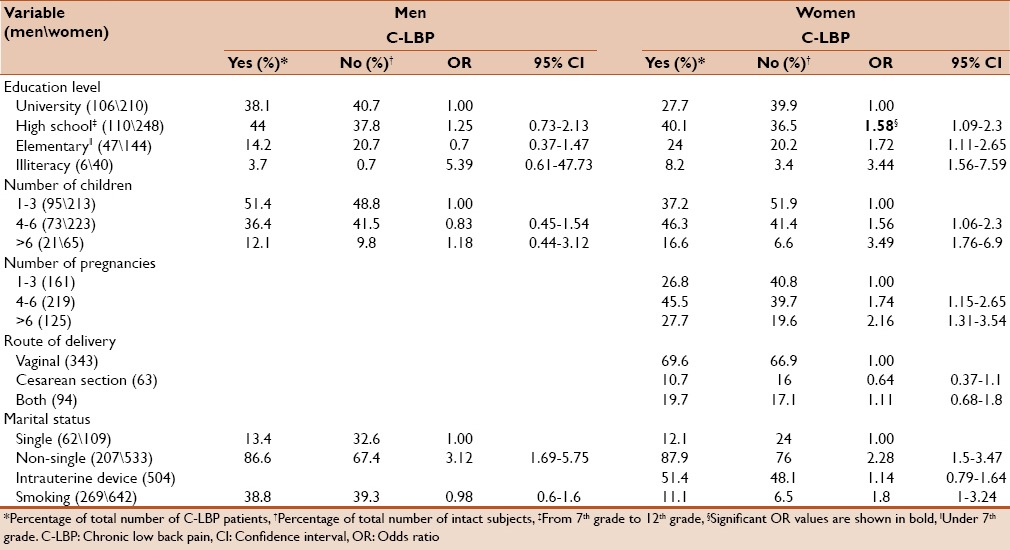
Table 3.
Relative frequencies of men and women with and without C-LBP and factors associated with C-LBP tested by univariate logistic regression model
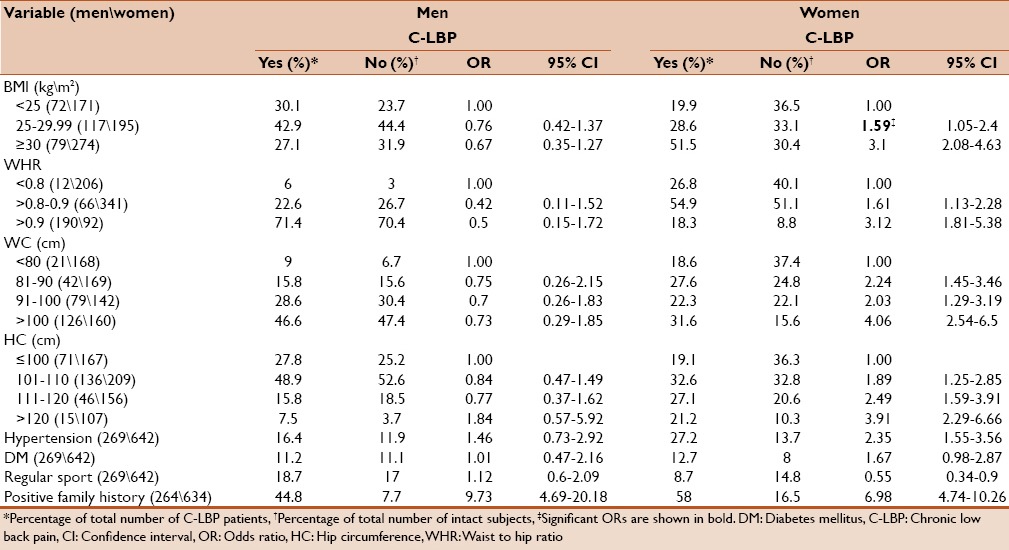
Table 4.
Relative frequencies of people with and without C-LBP and factors associated with C-LBP tested by univariate logistic regression model
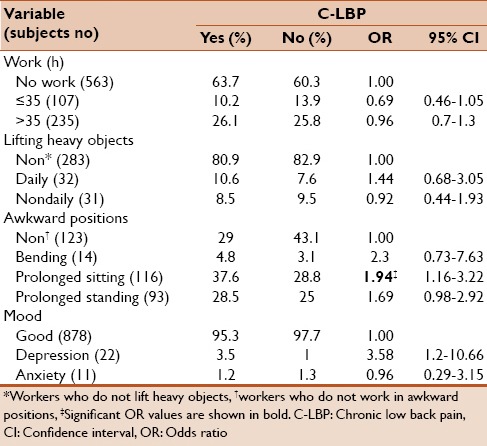
Table 5.
Risk factors for C-LBP tested in a multiple logistic regression model (adjusted for age)
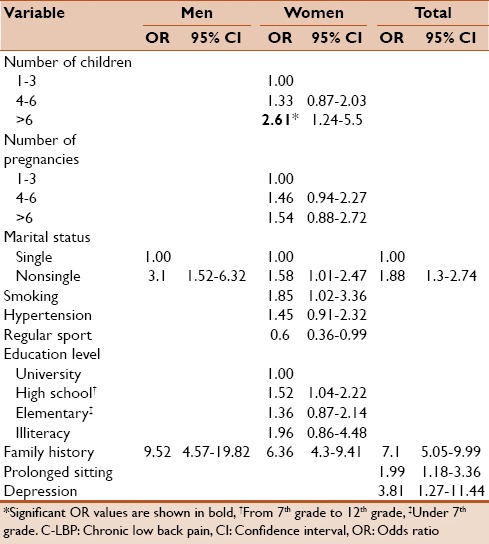
Table 6.
Risk factors for C-LBP tested in a multiple logistic regression model (adjusted for age)
We found positive family history in 26.5% of men and 41% of women. It was significantly associated with C-LBP in both men and women; the OR was 9.73 with (95% CI: 4.69–20.18), P < 0.001 in men and 6.98 with (95% CI: 4.74–10.26), P < 0.001 in women. This strong association remained significant after adjustment for age; (OR = 9.52, 95% CI: 4.57–19.82), P < 0.001, (OR = 6.36, 95% CI: 4.3, 9.41), P < 0.001 for men and women, respectively.
DISCUSSION
To our knowledge, this is the first study to be conducted about C-LBP in Syria. We found a higher rate of C-LBP in women as found in other studies.[13,14,16,29]
Regarding the family history of LBP, the very high rate of another sibling with LBP might suggest hereditary/congenital susceptibility to C-LBP. Only limited literature is available about this issue.[19,20] Should this hold true in future studies, it would have many implications including a preemptive early risk-management approach.
Based on increasing mechanical force on the person's back, we expected to find a linear correlation with weight in our patients. However, we found significant correlation only in obese women similar to a few studies.[2,8,9,30] While some previous studies reported a positive association to increasing BMI,[4,6,13,14,23,31] others did not.[11,32,33]
We found that higher HC, WC, and WHR increased the risk of C-LBP in women but not in men. Previous studies found this association of higher WC[8,10] and WHR[2,8,9,12] with LBP only in women, while a positive association of higher HC was reported in both men and women in another study.[8] This is in contrast with the cardiovascular risk where a thinner waist and a larger hip are protective.[34] A Chinese study by Yip et al.[11] found an inverse relation of WHR to LBP.
Cigarette smoking is generally reported to be a weak risk factor for LBP.[15] Many studies have shown this risk;[2,8,14,16,19] some have reported this in women,[13] and some have not.[4,22,33] In our study, it has showed a weak association with C-LBP only in women.
We found non-single status to be associated with C-LBP in both men and women, which is similar to other studies.[14,16] Diabetes mellitus and hypertension were not associated with C-LBP, which is consistent with Altinel et al.,[4] but not another study.[18]
Regular physical activity appeared as a protective factor from C-LBP similar to another study.[16] However, in our study this was only true for women. We found a positive association between depression and C-LBP similar to some studies[4,14] and in contrast to another one.[18]
We have many families with large number of children in our community and it is not uncommon to see families with >6 children. We, therefore, asked about number of children and pregnancies, a factor hardly studied previously. We did find a correlation with number of children in female patients. However, we cannot isolate the burden of raising the children as a superimposed factor due to the fact that the study is performed in a community where mothers carry this responsibility while men work outside earning a living. Higher number of pregnancies was not associated with C-LBP in our study while a Turkish study by Altinel et al.[4] found the contrary.
Several studies reported an inverse relationship of education level to LBP.[13,21,22,23] It can be speculated that higher education decreases risk due to less demanding work and better back-hygiene and habits in daily activities, but it is difficult to explain why it is helpful only in females. We can explain the lack of risk of illiteracy in men by having very few cases (6 cases) in this group.
Work related factors as working-hours per week, heavy weight lifting, bending, and prolonged standing showed no significant correlation with C-LBP in our study, which is surprising since other studies showed the contrary.[24,25] We did not evaluate the role of chores among women most of whom were housewives. Their risks include harmful positions such as bending, lifting children and prolonged standing. In our questionnaire, those who worked inside were labeled as nonworkers. This issue clearly needs to be addressed in future studies.
Finally, this study has several limitations; we do not have a confirmed etiology for the pain in our patients in the study. Nonetheless, all of them fit our definition of C-LBP. Lack of work-up in many patients is mainly due to financial reason and available resources. Most of our patients did not have medical insurance. Accordingly, it is not uncommon for our patients to be lost to follow-up. Furthermore, we cannot comment on treatment since we do not have full work up and/or follow-up on all the patients. Despite the limitation of specific etiology of C-LBP, we have interesting findings in regards to many risk factors studied.
CONCLUSION
This study shows some of the factors associated with C-LBP and should be helpful in directing effort for prevention. In women we found obesity (P = 0.001), increased WC (P = 0.001 for WC > 100 cm), increased HC (P = 0.001 for HC > 120 cm), higher WHR (P = 0.37 for WHR > 0.9), lower level of education (P = 0.31), having more than 6 children (P = 0.012), and smoking (P = 0.45) to be associated with C-LBP. We found that positive family history had a high level of significant association with C-LBP in both men and women (P < 0.001). Furthermore, being non-single (P = 0.001) and prolonged sitting at work (P = 0.01) were important risk factors for C-LBP.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors thank Rania Tawil for conducting the interviews with the patients.
REFERENCES
- 1.Brooks PM. The burden of musculoskeletal disease – A global perspective. Clin Rheumatol. 2006;25:778–81. doi: 10.1007/s10067-006-0240-3. [DOI] [PubMed] [Google Scholar]
- 2.Hemingway H, Shipley M, Stansfeld S, Shannon H, Frank J, Brunner E, et al. Are risk factors for atherothrombotic disease associated with back pain sickness absence? The Whitehall II Study. J Epidemiol Community Health. 1999;53:197–203. doi: 10.1136/jech.53.4.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Freburger JK, Holmes GM, Agans RP, Jackman AM, Darter JD, Wallace AS, et al. The rising prevalence of chronic low back pain. Arch Intern Med. 2009;169:251–8. doi: 10.1001/archinternmed.2008.543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Altinel L, Köse KC, Ergan V, Isik C, Aksoy Y, Ozdemir A, et al. The prevalence of low back pain and risk factors among adult population in Afyon region, Turkey. Acta Orthop Traumatol Turc. 2008;42:328–33. doi: 10.3944/aott.2008.328. [DOI] [PubMed] [Google Scholar]
- 5.Mirtz TA, Greene L. Is obesity a risk factor for low back pain? An example of using the evidence to answer a clinical question. Chiropr Osteopat. 2005;13:2. doi: 10.1186/1746-1340-13-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Leboeuf-Yde C. Body weight and low back pain. A systematic literature review of 56 journal articles reporting on 65 epidemiologic studies. Spine (Phila Pa 1976) 2000;25:226–37. doi: 10.1097/00007632-200001150-00015. [DOI] [PubMed] [Google Scholar]
- 7.Garzillo MJ, Garzillo TA. Does obesity cause low back pain? J Manipulative Physiol Ther. 1994;17:601–4. [PubMed] [Google Scholar]
- 8.Shiri R, Solovieva S, Husgafvel-Pursiainen K, Taimela S, Saarikoski LA, Huupponen R, et al. The association between obesity and the prevalence of low back pain in young adults: The Cardiovascular Risk in Young Finns Study. Am J Epidemiol. 2008;167:1110–9. doi: 10.1093/aje/kwn007. [DOI] [PubMed] [Google Scholar]
- 9.Han TS, Schouten JS, Lean ME, Seidell JC. The prevalence of low back pain and associations with body fatness, fat distribution and height. Int J Obes Relat Metab Disord. 1997;21:600–7. doi: 10.1038/sj.ijo.0800448. [DOI] [PubMed] [Google Scholar]
- 10.Lean ME, Han TS, Seidell JC. Impairment of health and quality of life in people with large waist circumference. Lancet. 1998;351:853–6. doi: 10.1016/s0140-6736(97)10004-6. [DOI] [PubMed] [Google Scholar]
- 11.Yip YB, Ho SC, Chan SG. Tall stature, overweight and the prevalence of low back pain in Chinese middle-aged women. Int J Obes Relat Metab Disord. 2001;25:887–92. doi: 10.1038/sj.ijo.0801557. [DOI] [PubMed] [Google Scholar]
- 12.Toda Y, Segal N, Toda T, Morimoto T, Ogawa R. Lean body mass and body fat distribution in participants with chronic low back pain. Arch Intern Med. 2000;160:3265–9. doi: 10.1001/archinte.160.21.3265. [DOI] [PubMed] [Google Scholar]
- 13.Björck-van Dijken C, Fjellman-Wiklund A, Hildingsson C. Low back pain, lifestyle factors and physical activity: A population based-study. J Rehabil Med. 2008;40:864–9. doi: 10.2340/16501977-0273. [DOI] [PubMed] [Google Scholar]
- 14.Strine TW, Hootman JM. US national prevalence and correlates of low back and neck pain among adults. Arthritis Rheum. 2007;57:656–65. doi: 10.1002/art.22684. [DOI] [PubMed] [Google Scholar]
- 15.Leboeuf-Yde C. Smoking and low back pain. A systematic literature review of 41 journal articles reporting 47 epidemiologic studies. Spine (Phila Pa 1976) 1999;24:1463–70. doi: 10.1097/00007632-199907150-00012. [DOI] [PubMed] [Google Scholar]
- 16.Bejia I, Younes M, Jamila HB, Khalfallah T, Ben Salem K, Touzi M, et al. Prevalence and factors associated to low back pain among hospital staff. Joint Bone Spine. 2005;72:254–9. doi: 10.1016/j.jbspin.2004.06.001. [DOI] [PubMed] [Google Scholar]
- 17.Khruakhorn S, Sritipsukho P, Siripakarn Y, Vachalathiti R. Prevalence and risk factors of low back pain among the university staff. J Med Assoc Thai. 2010;93(Suppl 7):S142–8. [PubMed] [Google Scholar]
- 18.Gilchrist IC. Psychiatric and social factors related to low-back pain in general practice. Rheumatol Rehabil. 1976;15:101–7. doi: 10.1093/rheumatology/15.2.101. [DOI] [PubMed] [Google Scholar]
- 19.Fujii T, Matsudaira K. Prevalence of low back pain and factors associated with chronic disabling back pain in Japan. Eur Spine J. 2013;22:432–8. doi: 10.1007/s00586-012-2439-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Matsui H, Maeda A, Tsuji H, Naruse Y. Risk indicators of low back pain among workers in Japan. Association of familial and physical factors with low back pain. Spine (Phila Pa 1976) 1997;22:1242–7. doi: 10.1097/00007632-199706010-00014. [DOI] [PubMed] [Google Scholar]
- 21.Latza U, Kohlmann T, Deck R, Raspe H. Influence of occupational factors on the relation between socioeconomic status and self-reported back pain in a population-based sample of German adults with back pain. Spine (Phila Pa 1976) 2000;25:1390–7. doi: 10.1097/00007632-200006010-00011. [DOI] [PubMed] [Google Scholar]
- 22.Lindell O, Johansson SE, Strender LE. Living conditions, including life style, in primary-care patients with nonacute, nonspecific spinal pain compared with a population-based sample: A cross-sectional study. Clin Epidemiol. 2010;2:261–71. doi: 10.2147/CLEP.S14761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bener A, Alwash R, Gaber T, Lovasz G. Obesity and low back pain. Coll Antropol. 2003;27:95–104. [PubMed] [Google Scholar]
- 24.Sanya AO, Omokhodion FO, Ogwumlke OO. Risk factors for low back pain among hospital workers in Ibadan, Oyo state, Nigeria. J Nigeria Soc Physiother. 2005;15:31–4. [Google Scholar]
- 25.Lu JL. Risk factors for low back pain among Filipino manufacturing workers and their anthropometric measurements. Appl Occup Environ Hyg. 2003;18:170–6. doi: 10.1080/10473220301349. [DOI] [PubMed] [Google Scholar]
- 26.Rozenberg S. Chronic low back pain: Definition and treatment. Rev Prat. 2008:265–72. [PubMed] [Google Scholar]
- 27.Janwantanakul P, Pensri P, Moolkay P, Jiamjarasrangsi W. Development of a risk score for low back pain in office workers – A cross-sectional study. BMC Musculoskelet Disord. 2011;12:23. doi: 10.1186/1471-2474-12-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Parker ED, Pereira MA, Stevens J, Folsom AR. Association of hip circumference with incident diabetes and coronary heart disease: The Atherosclerosis Risk in Communities study. Am J Epidemiol. 2009;169:837–47. doi: 10.1093/aje/kwn395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Andersson GB. Epidemiological features of chronic low-back pain. Lancet. 1999;354:581–5. doi: 10.1016/S0140-6736(99)01312-4. [DOI] [PubMed] [Google Scholar]
- 30.Lake JK, Power C, Cole TJ. Back pain and obesity in the 1958 British birth cohort. cause or effect? J Clin Epidemiol. 2000;53:245–50. doi: 10.1016/s0895-4356(99)00155-9. [DOI] [PubMed] [Google Scholar]
- 31.Shiri R, Karppinen J, Leino-Arjas P, Solovieva S, Viikari-Juntura E. The association between obesity and low back pain: A meta-analysis. Am J Epidemiol. 2010;171:135–54. doi: 10.1093/aje/kwp356. [DOI] [PubMed] [Google Scholar]
- 32.Kujala UM, Taimela S, Viljanen T, Jutila H, Viitasalo JT, Videman T, et al. Physical loading and performance as predictors of back pain in healthy adults. A 5-year prospective study. Eur J Appl Physiol Occup Physiol. 1996;73:452–8. doi: 10.1007/BF00334423. [DOI] [PubMed] [Google Scholar]
- 33.Tiwari RR, Saha A. An epidemiological study of low back pain among oil drilling workers in India. Toxicol Ind Health. 2014;30:60–3. doi: 10.1177/0748233712451771. [DOI] [PubMed] [Google Scholar]
- 34.Seidell JC, Pérusse L, Després JP, Bouchard C. Waist and hip circumferences have independent and opposite effects on cardiovascular disease risk factors: The Quebec Family Study. Am J Clin Nutr. 2001;74:315–21. doi: 10.1093/ajcn/74.3.315. [DOI] [PubMed] [Google Scholar]


