Abstract
Background:
Cesarean section is a major operation that can be the predictor of postoperative pain and discomfort and, therefore, providing the effective postoperative analgesia is an important factor to facilitate sooner movement of the patient, better care of infants. The aim of this study was to determine the preventive effect of ilioinguinal nerve block on pain after cesarean section.
Materials and Methods:
In a randomized clinical trial study, 80 female candidates for cesarean section under general anesthesia were selected and divided into two groups. In the first group, ilioinguinal nerve was blocked and in the control group, ilioinguinal nerve block was not done. Finally, postoperative pain was compared between the two groups.
Results:
The mean pain intensity at 6 and 24 h after operation had no significant difference between two groups but in the rest of the times, it was different between two groups. Furthermore, in sitting position, except for 6 h, the pain intensity at the rest of the time had a significant difference between two groups. The pain intensity in 12 h after operation had a significant difference while in 24 h after operation; there was no difference between two groups. Doing repeated measures, ANOVA also indicated that the process of changes in the pain intensity in three positions of rest, sitting and walking had no significant difference up to 24 h after operation (P < 0.001).
Conclusion:
Control of pain after cesarean as one of the most common factors for abdominal surgery will lead to decrease the staying of the patient in hospital, reduce morbidity and lower use of narcotics and analgesics after surgery.
Keywords: Cesarean, ilioinguinal nerve block, postoperative pain
INTRODUCTION
According to the definition of International Association for the Study of Pain, pain is an unpleasant feeling, an unpleasant sensory and emotional experience associated with actual or potential tissue damage or described in terms of such damage and also, a protective mechanism to inform the body for the occurrence of the damage.[1]
The most important postoperative pain complications include respiratory dysfunction in shallow and rapid breathing and as a result, pulmonary atelectasis, cardiovascular complications and increasing the risk of ischemic heart and myocardial infarction, increasing the risk of deep vein thrombosis and pulmonary embolism as a result of postoperative immobility, gastrointestinal complications such as nausea and vomiting and ileus, the urinary system complications such as urinary retention from decreasing bladder activity, psychological complications such as stress and anxiety and finally, the length of hospitalization.[2]
Cesarean section is a major operation that can be the predictor of postoperative pain and discomfort and, therefore, providing the effective postoperative analgesia is an important factor to facilitate sooner movement of the patient, better care of infants (including breast feeding, relationship of mother–infant) and preventing postoperative complications.[3] Proper analgesic regimen should be chosen with minimal side-effects for the mother and her child. In general, for controlling the postoperative pain, there are various methods including narcotic patient controlled analgesia in spinal and epidurals cryoanalgesia method, nonsteroidal anti-inflammatory drug, local anesthetic techniques, glucocorticoids and ilioinguinal nerve block[4] so far, several studies have been done on the rate of the effect of each of these methods in reducing pain after cesarean and different results have been obtained from these studies.
Today, ilioinguinal nerve block is considered more due to safety than other methods and the lack of systemic complications, while like other methods of local anesthesia, the method has an intravenous injection and may cause severe systemic toxicity. Meanwhile, if there is a coagulopathy, the possibility of the incidence of hematoma is higher in due to the perforation of blood vessels. Infection in the injection site is also another complication of this method.[5] So far, in conducted studies, anesthesia drugs of bupivacaine, ropivacaine and lidocaine have been used for the mentioned nerves block, and various results have been obtained.[6]
The side complications of these drugs generally depend on the dosage; high plasma concentration resulted from unwanted entrance of the drug in vessel; reduction of the patient's tolerance; personal incompatibility or extreme sensitivity. Meanwhile, the rate of unwanted complications depends on the site of injection too.[7] In general, results from other studies have reported various rate and severity of postoperative complications and on using this drug in ilioinguinal nerve block, few studies have so far been done and therefore, the present study have been conducted with the aim of determining the preventive effect of ilioinguinal nerve block on pain after cesarean section in mothers referring to Alzahra and Beheshti Hospitals for elective cesarean section. There are a few studies in this field, which have been reached the different results.
For example: In the study done by Sakalli et al.’ in 2010’ with injecting 10cc ropivacaine 0/5% for ilioinguinal nerve block to 30 patient and 10cc normal saline to 30 patient in the control group no significant difference was observed in pain level and using narcotic in two groups.[3] Furthermore, in their study, Werawatganon and Charuluxanun concluded that the pain level and receiving narcotic in the group under preventive ilioinguinal nerve block with bupivacaine have been less than that in the control group.[8]
MATERIALS AND METHODS
This study is a randomized double-blind clinical trial conducted in Alzahra and Beheshti University Hospital, Isfahan in 2012. The study population consisted of pregnant women undergoing cesarean in the above-mentioned centers.
Inclusion criteria were women undergoing cesarean with general anesthesia, class American Society of Anesthesiologists = I and II, consent to participating in the study, lack of previous allergy to local anesthetics or narcotics, the lack of coagulation problems, lack of the history of considerable mental problems, chronic pain syndrome, lack of long-term use of analgesic, lack of recent use of opioids and lack of suffering from diabetes mellitus 1 and 2. Furthermore, it was appointed if changing the type of intraoperative anesthesia (due to prolonging the operation or failure of anesthesia) or impossibility of assessing the postoperative pain due to the several reasons such as death, patients should be excluded from the study.
Using the formula of estimating the sample size for comparing the means and considering confidence level of 95%, test power of 80% and variance of visual analogue scale (VAS) in the studied patients, the sample size required in the study was estimated about 1.1 according to the previous studies and the minimal significant difference between two groups considered equal to 0.8 was estimated as 40 cases in each group.
The method was in the way that 80 female candidates for cesarean section under general anesthesia were selected and divided into two groups with 40 individuals in the method of randomly allocation (one among).
Both groups received the same fluid therapy and anesthesia method and all patients were kept NPO for 8 h and during this time, according to Act 1, 2 and 4, the fluid therapy used fluid was 1.3 * 2.3. Before the induction of anesthesia, 500 mL ringer lactate was injected to all patients. General anesthesia was performed on all patients and after surgery and before sewing fascia, in the intervention group, approximately 2 cm inward and above point of anterior superior iliac spine was marked, by a needle A22G, was entered into skin and was injected after piercing external fascia oblique 1.6 from 10cc bupivacaine 5% after negative aspiration test. Then the needle was entered more to the extent that the resistance between the internal muscles of oblique and transverse is eliminated. At this stage, 1.6 of anesthetic solution was again injected and then, the needle was withdrawn and by changing the needle 15° inward and then outward, the process was repeated in a fan-shaped pattern. This process was also repeated on the opposite side, and 20cc anesthetic solution was totally injected on both sides. In the control group, ilioinguinal nerve block was not done. At the end, patients’ operation was extubated and they were transferred to the recovery room. It has shown the anatomy and nerve block method in Figures 1–4.
Figure 1.
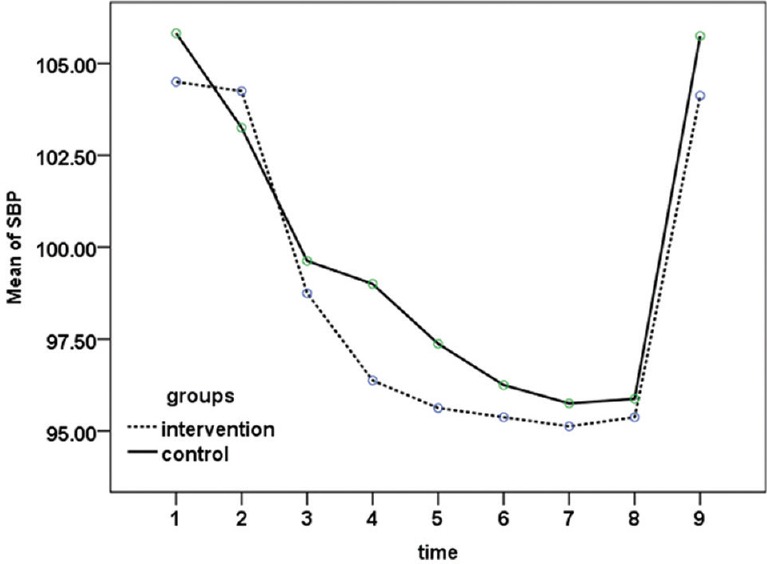
Mean of systolic blood pressure from arriving to the recovery room up to 24 h after doing operation in both groups (P = 0.34)
Figure 4.
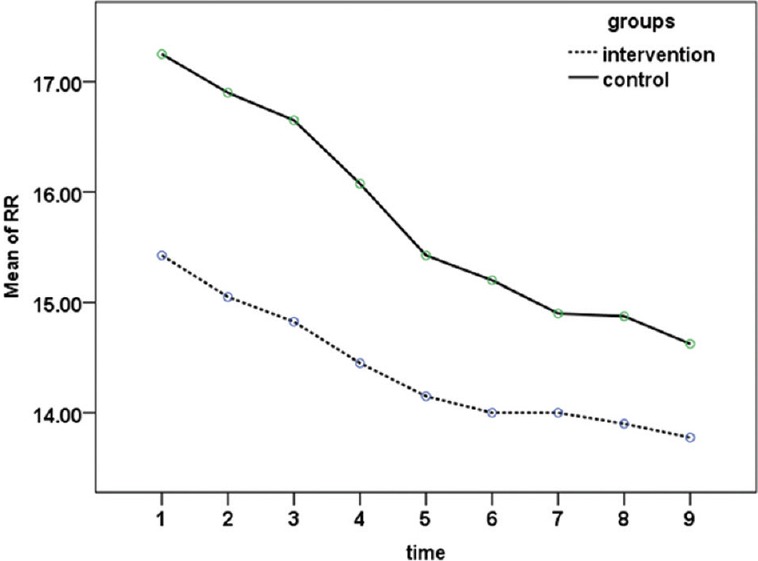
Mean of m respiratory rate from arriving to the recovery room up to 24 h after doing operation in both groups (P < 0.001)
Figure 2.
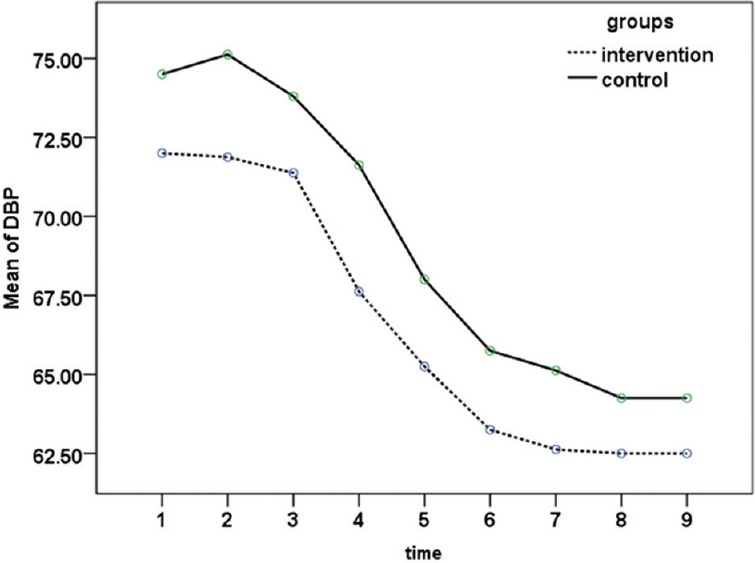
Mean of systolic blood pressure from arriving the recovery room up to 24 h after doing operation in both groups (P = 0.008)
Figure 3.
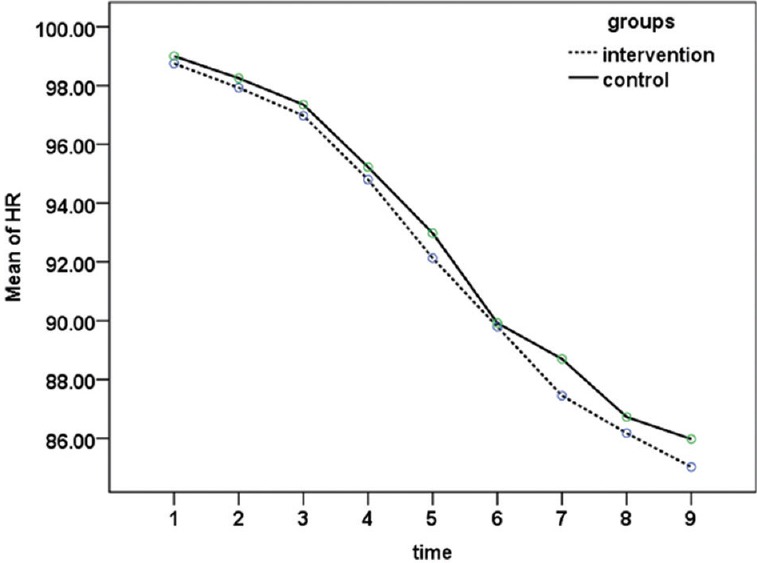
Mean of heart rate from arriving to the recovery room up to 24 h after doing operation in both groups (P = 0.37)
Patients and personnel involved in the data collection were not informed on the group type of patients and all patients received routine postoperative nursing care and when they achieved conditions of discharge from the recovery room, they entered into the ward. Hemodynamic parameters of the patients, including systolic and diastolic blood pressure, heart rate and respiratory rate of arrival to the recovery room at 15 and 30 min and 1, 2, 4, 6, 12 and 24 h after operation were monitored and recorded.
To estimate the pain intensity in VAS method, the necessary training were given to all patients before starting the investigation and they were asked to show their pain on a ruler graduated 10 cm (0: No pain feels, 10: The most intensive pain experienced).
Whenever a patient considered analgesia as insufficient and called anesthesiologist and if based on the VSA criteria, the patient's pain intensity was over 3; pethidine bolus was injected for the patient. The existence of nausea or vomiting was investigated at 0-1-2-4-6-12 and 24 h after cesarean, and whenever a patient complained for nausea or vomiting, 0.15 mg/kg dose of metoclopramide bolus was injected.
The study data were entered into a computer program and analyzed by SPSS software version 22 (Chicago, Illinois: SPSS Inc). Statistical tests used to analyze data included ANOVA with repeated measures, Student's t-test and Chi-square test.
RESULTS
In this study, 80 patients were selected and randomly divided into two intervention and control groups. The mean age of patients in two groups was 27.8 ± 2.7 and 27.2 ± 4.9 years, respectively, and according to t-test, there was no significant difference between two groups (P = 0.45). The mean changes in the hemodynamic parameters of patients in two groups arrival to the recovery room up to 24 h after doing operation in both studied groups has been shown in Figures 1–4. According to ANOVA with repeated observations, in both groups, changes in systolic blood pressure and heart rate were not significantly different, while the mean changes in diastolic blood pressure and respiratory rate was significant in both groups (P < 0.05).
The mean and standard deviation (SD) of postoperative pain intensity in two studied groups at rest and in sitting and walking positions have been shown in Table 1.
Table 1.
Mean±SD of postoperative pain at rest and in sitting and walking positions
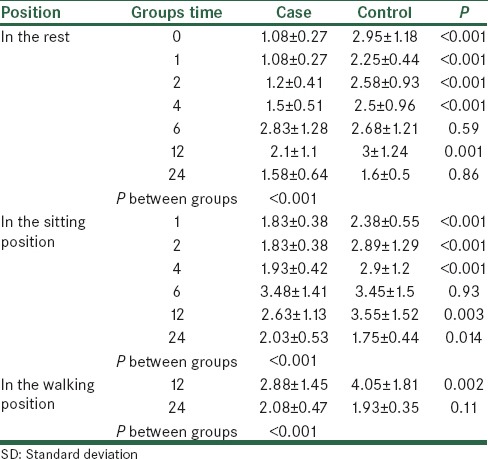
According to the t-test, at rest position, the mean pain intensity at 6 and 24 h after operation had no significant difference between two groups but in the rest of the times, it was different between two groups. Furthermore, in sitting a position, except for 6 h, the pain intensity at the rest of the time had a significant difference between two groups. The pain intensity in 12 h after operation had a significant difference while in 24 h after operation, there was no difference between two groups. Doing repeated measures, ANOVA also indicated that the process of changes in the pain intensity in three positions of rest, sitting and walking had no significant difference up to 24 h after operation (P < 0.001). The process of changes in the pain intensity has been shown in Figures 5–7.
Figure 5.
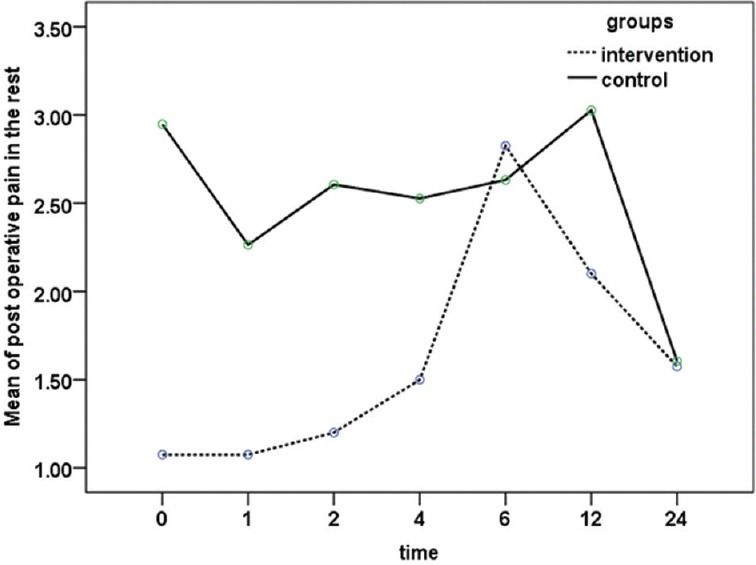
Mean of pain intensity at rest mode arrival to the recovery room to 24 h after doing operation in both groups (P < 0.001)
Figure 7.
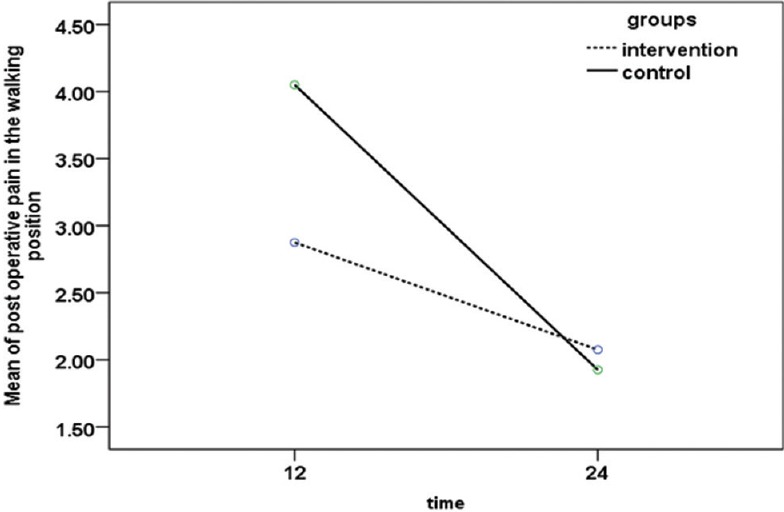
Mean of pain intensity in walking mode in 12 and 24 h after doing operation in both groups (P < 0.001)
Figure 6.
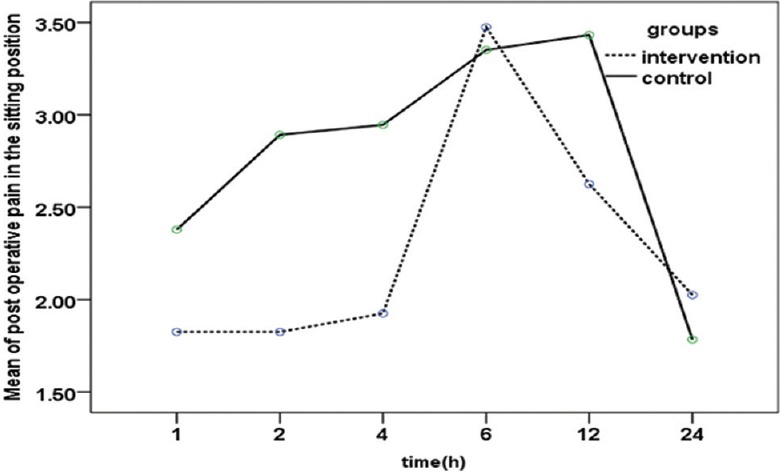
Mean of pain intensity in sitting mode from 1 h after the admission in the ward to 24 h after doing operation in both groups (P < 0.001)
In Table 2, the frequency distribution of using narcotic from arriving to the recovery room to 24 h after operation has been shown in both groups. According to Chi-square and Fisher's exact tests, except for 6 and 24 h, the frequency distribution using narcotic was different at the rest times and in the control group, it was significantly higher [Figure 8]. Notably, the amount of using narcotic was 25 mg in 2 cases and 50 mg in other cases per patient.
Table 2.
The frequency percentage using narcotic up to 24 h after operation in both groups
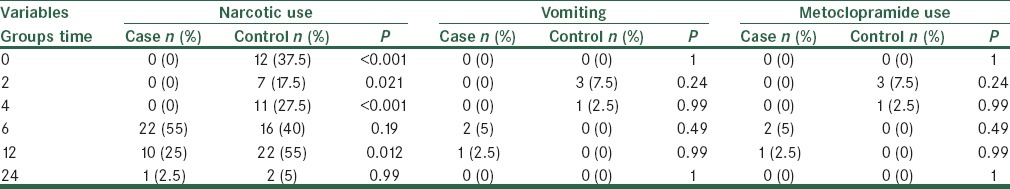
Figure 8.
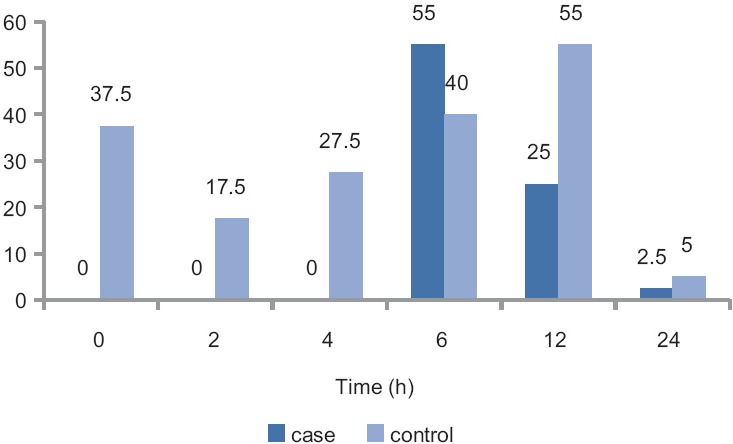
The frequency percentage of arrival of narcotic use to the recovery room to 24 h after doing operation in both groups
In the mentioned table, the frequency distribution of the incidence of nausea up to 24 h after the operation and using metoclopramide in both groups has been shown. Based on Fisher's exact test, no significant difference was observed between two groups. Also according to results of this study the mean ± SD of first time to receiving narcotic in the intervention and control groups was 7.65 ± 2.03 and 3.43 ± 2.76, respectively, and according to Student's t-test, there is a statistically difference between the two groups was seen (P < 0.001) [Figure 9].
Figure 9.
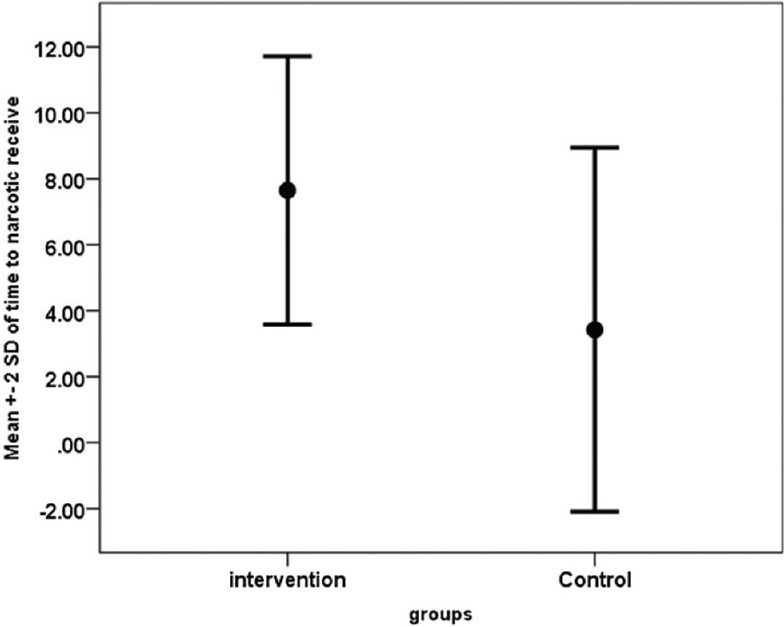
Mean of time to narcotic receiving in both groups
DISCUSSION AND CONCLUSION
The overall objective of this study was to determine the preventive effect of ilioinguinal nerve block on reducing postoperative pain in patients undergoing cesarean with general anesthesia. The age distribution had no significant difference between intervention and control groups and thus, the confounding effect of age was neutralized in the study and the obtained results have been likely due to the effect of intervention type in the patients.
Investigating the hemodynamic parameters in the two groups showed that patients in both groups had no significant difference in terms of systolic blood pressure and heart rate while patients undergoing intervention injection had lower mean of diastolic blood pressure and respiratory rate compared with the control group; however, no incidence of hypotension (decrease of over 20%) or Apnea were observed in the patients.
Evaluation of the pain intensity up to 24 h after operation in patients in both groups indicated that patients undergoing ilioinguinal nerve block had totally less pain intensity that there is this difference in all positions of rest, sitting and walking and correspondingly, the rate of using narcotic for controlling the pain was significantly lower except for 24 h in the rest of the times the patients in the intervention group. There are some similar studies with different results about the effect of this nerve block. For example, in the study by John et al. investigating the preventive effect of ilioinguinal nerve block and iliohypogastric on pain after cesarean in 50 women undergoing cesarean with general anesthesia, the injection of 1.5 mg bupivacaine has caused to decrease the intensity of postoperative pain and rate of using narcotics after cesarean.[4] However, in the study done by Dahl et al., examining injecting 10cc bupivacaine 0.5% for ilioinguinal nerve block to 30 patients and 10cc normal saline to 30 patients in the control group undergoing cesarean after anesthesia, no significant difference was observed in the pain level and using narcotic between two groups.[6] Furthermore, in their study, Werawatganon and Charuluxanun concluded that the pain level and receiving narcotic in the group under preventive ilioinguinal nerve block with bupivacaine have been less than that in the control group.[8]
Studying the postoperative complications showed that the incidence of nausea in both groups had no significant difference and using metoclopramide was not different too. In the study by Vallejo et al., the mentioned nerve block has not caused to a significant decrease in pain and using narcotic after cesarean. In this study 10cc ropivacaine 0/5% for ilioinguinal nerve block was injected to 30 patients and 10cc normal saline to 30 patients in the control group.[9] Most probably, different results in the similar studies are due to incorrect injection for ilioinguinal nerve block. Hence, accuracy during procedure is very important. Regarding the side-effects of narcotics (such as meperidine and pentazocine (Helman, Germany), which are widely used in our country) including the gastric complications, confusion, probably transferred to breast milk and leading to ill effect on neonates nutrition and their mothers relation it is suggested to do inguinal nerve block, which is a simple and safe method by gynecologists to control the post cesarean pain and increase the need to narcotics resulted to low the costs. Therefore, the overall conclusion obtained from the present study and other similar studies is that in addition to reducing pain in patients, control of pain after cesarean as one of the most common factors for abdominal surgery will lead to decrease the staying of the patient in hospital, reduce morbidity and lower use of narcotics and analgesics after surgery.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Farragher RA, Laffey JG. 2006. Postoperative Management; an Evidence-Based Guide to Practice; pp. 225–38. [Google Scholar]
- 2.Wolfson A, Lee AJ, Wong RP, Arheart KL, Penning DH. Bilateral multi-injection iliohypogastric-ilioinguinal nerve block in conjunction with neuraxial morphine is superior to neuraxial morphine alone for postcesarean analgesia. J Clin Anesth. 2012;24:298–303. doi: 10.1016/j.jclinane.2011.09.007. [DOI] [PubMed] [Google Scholar]
- 3.Sakalli M, Ceyhan A, Uysal HY, Yazici I, Basar H. The efficacy of ilioinguinal and iliohypogastric nerve block for postoperative pain after caesarean section. J Res Med Sci. 2010;15:6–13. [PMC free article] [PubMed] [Google Scholar]
- 4.McDonnell JG, O’Donnell B, Curley G, Heffernan A, Power C, Laffey JG. The analgesic efficacy of transversus abdominis plane block after abdominal surgery: A prospective randomized controlled trial. Anesth Analg. 2007;104:193–7. doi: 10.1213/01.ane.0000250223.49963.0f. [DOI] [PubMed] [Google Scholar]
- 5.O’Donnell BD, McDonnell JG, McShane AJ. The transversus abdominis plane (TAP) block in open retropubic prostatectomy. Reg Anesth Pain Med. 2006;31:91. doi: 10.1016/j.rapm.2005.10.006. [DOI] [PubMed] [Google Scholar]
- 6.Dahl JB, Jeppesen IS, Jørgensen H, Wetterslev J, Møiniche S. Intraoperative and postoperative analgesic efficacy and adverse effects of intrathecal opioids in patients undergoing cesarean section with spinal anesthesia: A qualitative and quantitative systematic review of randomized controlled trials. Anesthesiology. 1999;91:1919–27. doi: 10.1097/00000542-199912000-00045. [DOI] [PubMed] [Google Scholar]
- 7.Sweetman SC. London: Phamaceutical Press; 2007. Martindale: The Complete Drug Reference; pp. 1690–713. [Google Scholar]
- 8.Werawatganon T, Charuluxanun S. Patient controlled intravenous opioid analgesia versus continuous epidural analgesia for pain after intra-abdominal surgery. Cochrane Database Syst Rev. 2005 doi: 10.1002/14651858.CD004088.pub2. DOI: 10.1002/14651858.CD004088.pub2:CD004088. [DOI] [PubMed] [Google Scholar]
- 9.Vallejo MC, Steen TL, Cobb BT, Phelps AL, Pomerantz JM, Orebaugh SL, et al. Efficacy of the bilateral ilioinguinal-iliohypogastric block with intrathecal morphine for postoperative cesarean delivery analgesia. Scientific World Journal 2012. 2012 doi: 10.1100/2012/107316. 107316. [DOI] [PMC free article] [PubMed] [Google Scholar]


