Abstract
Background
Major depressive disorder (MDD) is a common disorder that is often associated with suicide. We have recently suggested that elevation may play a role in regional variations in rates of suicide. We hypothesize that there is also a significant correlation between incidence of MDD and elevation of residence.
Methods
The substate estimates from the 2004 to 2006 National Surveys on Drug Use and Health (NSDUH) report from SAMHSA was used to extract substate level data related to percentages of people 18 years or older who experienced serious psychological distress or a major depressive episode in the past year. Mean elevation of each substate region was calculated by averaging the weighted elevations of its relevant counties. Average elevation for United States counties was calculated using the Shuttle Radar Topography Mission (SRTM) elevation dataset. Pearson correlation coefficients were computed to investigate the association between average substate elevation and rate of serious psychological distress or major depressive episode.
Results
There was a significant correlation between percentage of people experiencing serious psychological distress in the past year in a substate region and that substate region's mean elevation (r = 0.18; p = 0.0005), as well as between the percentage of people having at least one major depressive episode in the past year in a substate region and that substate region's mean elevation (r = 0.27; p < 0.0001).
Conclusions
Elevation appears to be a significant risk factor for MDD. Further studies are indicated to determine whether the increased incidence of depression with increased elevation may be due to the hypoxic effects on subjects with MDD.
Keywords: Major depressive disorder, Suicide, Altitude, Hypoxia, Depression, Elevation
1. Introduction
Major depressive disorder (MDD) is the mental disorder that most commonly leads to suicide (Kessler et al., 2005; World Health Organization, 2001). It is well known that rates of suicide, rates of MDD, and rates of mood disorders, in general, show regional variation (Weissman et al., 1996). Researchers have hypothesized that this variation is related to many different factors. Tempier et al. (2008) have suggested that the higher rates of depression seen in Australia compared to Canada, both countries with similar mental health policies, may result from the greater availability of alcohol in Australia. Likewise, a number of studies have associated variation in rates of mental health disorders, such as major depression, to differences in stigma associated with mental health disorders, public mental health knowledge, income, education level, marital status, unemployment, social class, living environment, sex and age (Bijl et al., 2003; Lewis and Booth, 1992; World Health Organization, 2001). A different perspective is presented in a 1998 study in which Joseph Hibbeln demonstrates that fish consumption and rates of depression are inversely correlated (p < 0.005) (Hibbeln, 1998). Hibbeln reports that countries with diets that are high in fish consumption, such as Japan, Taiwan and Korea, have lower rates of depression than countries with diets comparatively low in fish consumption, such as New Zealand, Canada, and West Germany.
Suicide is one of the top three causes of death worldwide for those 15–34 years of age (World Health Organization, 2001) and the eleventh leading cause of death in the United States (Centers for Disease Control and Prevention, 2005). The variation in rates of suicide worldwide is currently attributed to differences in gender, race, socioeconomic change, and access to drugs, alcohol and firearms (World Health Organization, 2001). In the United States, specifically, suicide rates are higher in the western region of country, even when adjusted for gender and race (Centers for Disease Control and Prevention, 1997). More recently we have suggested that elevation may play a role in regional variations in suicide rates (Haws et al., 2009). Haws et al. found a significant correlation between age, ethnicity, and sex adjusted suicide rate and the state's peak elevation (r = 0.62) as well as between adjusted suicide rate and the state's capital city elevation (r = 0.74) (Haws et al., 2009). Another recent study has demonstrated similarly significant positive correlations between age-adjusted suicide rate and elevation at a county level in the continental United States (r = 0.51) (Kim et al., in press). In addition, Kim et al. (in press) reported that elevation appears to be a more highly correlated with suicide than gun ownership or population density at a state level.
Since MDD and suicide are highly associated, we hypothesized that there would be a significant correlation between rates of major depression and elevation. Little data exists on the rates of mental health disorders for geographic regions smaller than states. However, the Substate Estimates from the 2004 to 2006 National Surveys on Drug Use and Health (NSDUH) report from the Substance Abuse and Mental Health Services Administration, Office of Applied Studies (SAMHSA, OAS) includes data on substance abuse and mental health from 203,870 responders in 345 substate regions making up all 50 states and the District of Columbia. The substate regions for each state are defined by SAMHSA and are divided by counties or census tracts (Substance Abuse and Mental Health Services Administration, 2008a). Two important measures reported for each substate region are: (1) the percent of people 18 years and older who have experienced serious psychological distress in the previous year and; (2) the percent of people who have experienced at least one episode of major depression in the previous year (Substance Abuse and Mental Health Services Administration, 2008b). Using the Shuttle Radar Topography Mission (National Geospatial-Intelligence Agency and National Aeronautics and Space Administration, 2000) elevation dataset along with the NSDUH data, we assessed the relationship between the above two measures for a substate region and that substate region's mean elevation.
2. Methods
2.1. Major depressive disorder data
The Substate Estimates from the 2004 to 2006 National Surveys on Drug Use and Health (NSDUH) report from SAMHSA was used to extract data related to percentages of people 18 years or older who experienced serious psychological distress in the past year as well as percentages of people 18 years or older having at least one major depressive episode in the past year. Data from all 50 states and the District of Columbia were evaluated at a substate level. The substate region definition for each state is defined by SAMHSA. Data were obtained by SAMHSA through the NSDUH questionnaire. Responders scoring 13 or greater on the K6 screening instrument for nonspecific psychological distress were determined to have experienced serious psychological distress in the last year. Responders were determined to have had a major depressive episode in the past year based on a NSDUH questionnaire module developed from the DSM-IV criteria for major depression (Substance Abuse and Mental Health Services Administration, 2008b).
2.2. Average elevation
Average elevation for United States counties was calculated using the Shuttle Radar Topography Mission (SRTM) elevation dataset (National Geospatial-Intelligence Agency and National Aeronautics and Space Administration, 2000). The SRTM dataset is a global scale digital topographic database of the Earth created in February of 2000. The approximately 0.1 km spatial resolution of this dataset allow accurate calculation of mean elevation of United States counties. However, the dataset does not include Alaska, Hawaii or the United States territories. Also, one county in Montana, one in Georgia and two counties in Virginia are not included in the SRTM dataset, and therefore, are not included in this analysis. The average elevation of each United States county (n = 3108) included in the SRTM dataset was calculated using zonal statistics in an ArcGIS/ArcInfo 9.3 environment. County outlines from the National Atlas of the United States: County Boundaries of the United States (National Atlas of the United States, 2001) were used to obtain the mean county elevation for each included county based on the SRTM mean elevation calculations for each square kilometer. Notably, the same method was used by Kim et al. (in press) to calculate US county elevation.
Substate regions, as defined by SAMHSA Office of Applied Studies, include multiple counties or census tracts in each state. SAMHSA data evaluated 345 substate regions, making up all 50 states and the District of Columbia (Substance Abuse and Mental Health Services Administration, 2008b). Mean elevation of each substate region was calculated by averaging the weighted elevations of its relevant counties. County elevation was weighted using its area within the substate region since several counties were in multiple substate regions.
2.3. Data analysis and statistics
Pearson correlation coefficients were computed to investigate the association between average substate elevation and rate of serious psychological distress as well as between average substate area elevation and rate of major depressive episode. Statistical significance was defined at an alpha level of 0.05 (two-tailed). R v2.10 (R Foundation for Statistical Computing, Vienna, Austria, http://www.R-project.org) was used for the computation.
3. Results
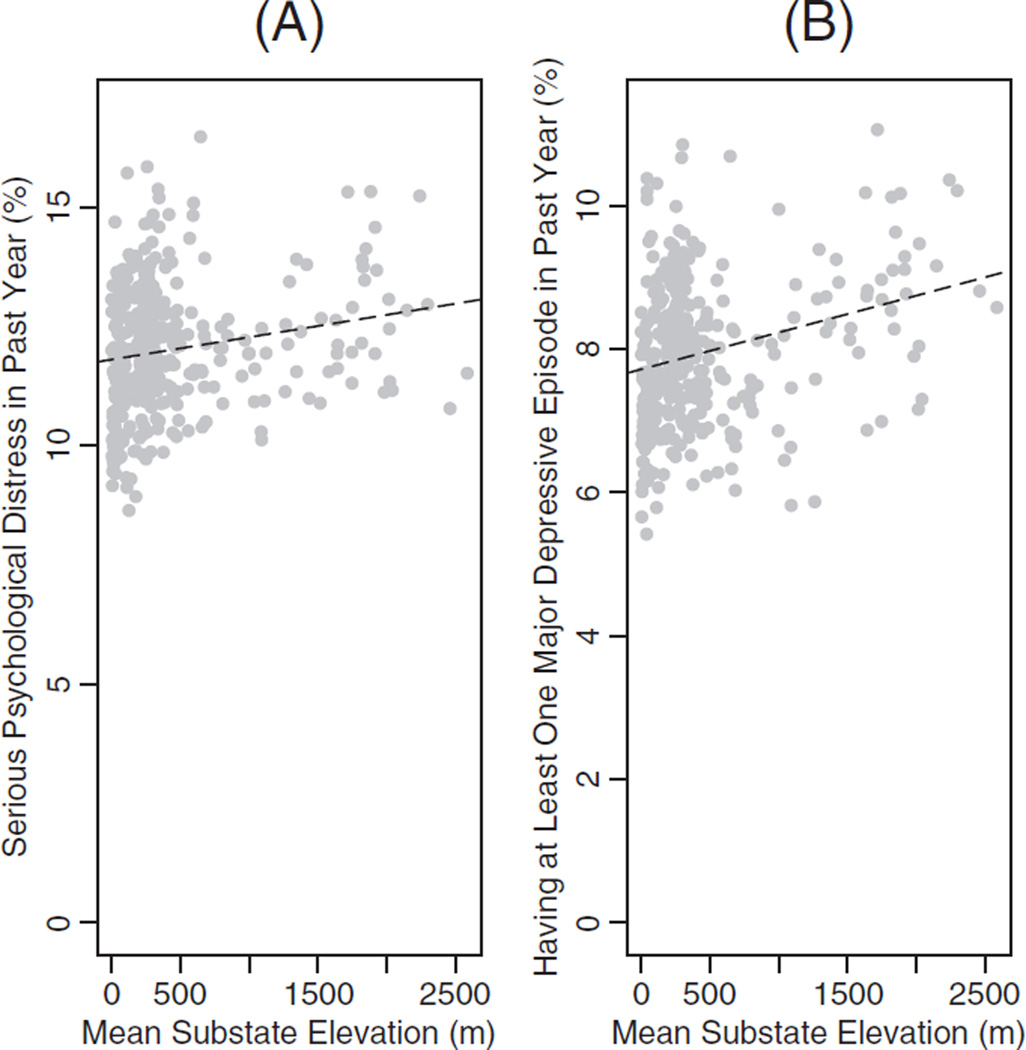
Fig. 1A shows a significant correlation between percentage of people experiencing serious psychological distress in the past year in a substate region and that substate region's mean elevation (r = 0.18; p = 0.0005). In addition, Fig. 1B also demonstrates a significant correlation between the percentage of people having at least one major depressive episode in the past year in a substate region and that substate region's mean elevation (r = 0.27; p < 0.0001).
Fig. 1.
(A) Serious Psychological Distress in Past Year (%) vs. Mean Substate Elevation (y = 0.0005× +11.81; r = 0.182; p = 0.0005). (B) Having at Least One Major Depressive Episode in Past Year (%) vs. Mean Substate Elevation (y = 0.0005× +7.716; r = 0.268; p < 0.0001).
4. Discussion
A significant correlation exists between the percentage of people who have experienced serious psychological distress in the past year in a substate region and that region's mean elevation. A similar relationship was demonstrated between the percentage of people who have experienced a major depressive episode in the last year in a substate region and that region's mean elevation. Haws et al. (2009) and Kim et al. (in press) have suggested that the observed increase in suicide with elevation is due to the effects of hypoxia on mood-disordered individuals. Our current research supports this hypothesis. One important observation, however, is that the increase in the rate of major depression with elevation demonstrated in this paper is small (e.g. a 13% increase from sea level to 2000 m) and cannot completely account for the larger increase in the rate of suicide with elevation at a county level (e.g. a 68.4% increase from sea level to 2000 m) (Kim et al., in press).
One possible explanation for this discrepancy is that depression at increased elevation may be more treatment refractory. Neuroimaging studies, such as those using Magnetic Resonance Spectroscopy (MRS), have convincingly demonstrated that MDD is associated with mitochondrial dysfunction (Forester et al., 2009; Iosifescu et al., 2008; Moore et al., 1997; Renshaw et al., 2001; Volz et al., 1998). More specifically, a growing body of research shows that MDD subjects have decreased beta nucleoside triphosphate (β-NTP) and increased levels of phosphocreatine (PCr) compared with healthy controls (Moore et al., 1997; Renshaw et al., 2001; Volz et al., 1998). Furthermore, successful treatment of MDD with antidepressants is associated with normalization in both NTP and PCr levels (Forester et al., 2009; Volz et al., 1998). Due to mitochondrial dysfunction, individuals with MDD may experience a worsening of symptoms with exposure to levels of hypoxia to which healthy individuals may easily be able to acclimate.
While relatively little research has been done on changes in brain chemistry associated with hypoxia, there have been studies examining the changes in heart tissue, which has similarly varied bioenergetic needs. A 31Phosphorus magnetic resonance spectroscopy (31P-MRS) study of heart tissue showed that concentration ratios of PCr/adenosine triphosphate (ATP) in Sherpas (elevation of residence of about 3400 m) were half that of people acclimated to 300 m (Hochachka et al., 1996). Interestingly, a 31P-MRS study by Renshaw et al. (2001) studied females with major depressive disorder and showed that β-NTP was about 21% lower in those who responded to fluoxetine treatment than those who did not. A more recent 31P-MRS study also showed decreased β-NTP in geriatric MDD subjects prior to treatment with sertraline (Forester et al., 2009). A study by Iosifescu et al. (2008) demonstrated that subjects with SSRI resistant depression that responded to adjunctive triiodothyronine treatment exhibited a trend towards higher baseline levels of PCr. β-NTP levels, which consist mostly of ATP, however, were similar in responders, nonresponders and controls. In other words, treatment responders demonstrated increased PCr/ATP ratios, the opposite of what is seen in the heart of those adapted to high elevations. Creatine supplementation has been shown to induce increased brain PCr/ATP ratios to the levels observed in individuals who are more likely to respond to antidepressant therapy (Lyoo et al., 2003). Creatine has also been shown to be effective in decreasing symptoms consistent with an animal model of depression in female rats (Allen et al., 2009) as well as in females with MDD who were treated with creatine as an adjunct to the SSRI escitalopram (Lyoo and Renshaw, Unpublished). If decreased brain PCr/ATP ratios are associated with life at increased elevations, elevation might therefore be associated with an increased rate of refractory depression.
Another possibility is that other disorders associated with suicide might also be increased with elevation. For example, bipolar disorder (BD) is also commonly associated with suicide (Tondo et al., 2003). Several studies have shown that BD is correlated with state-dependent changes in brain pH (Hamakawa et al., 2004; Kato et al., 1992, 1993; Kato et al., 1994). More specifically, Kato et al. (1992, 1993) demonstrated that brain pH is decreased in BD subjects in the euthymic state compared to healthy controls or BD subjects in a depressive ormanic state. Goldberg et al. (1992) used 31P-MRS to study brain pH in subjects prior to and after 7 days in a hypobaric chamber at a simulated elevation of 4267 m. After 1 week in the hypobaric chamber, the brain intracellular pH was unchanged from pre-hypoxic levels, but after return to sea level brain intracellular pH decreased significantly. This decrease in pH was still present 12 hours after return to sea level. Goldberg et al. were unable to measure brain pH at introduction to hypoxia or shortly thereafter, however, it is clear that changes in elevation do affect brain intracellular pH. An already decreased brain pH in patients with BD could exacerbate changes in brain pH due to elevation and potentially increase depressive symptoms and risk for suicide.
This study offers support for the hypothesis that the increase in the rate of suicide with elevation may be due to an increased incidence of depression, which may be related to the hypoxic effects on people with already compromised mitochondrial function. Unfortunately, we have not yet been able to obtain data that would allow us to explore the possible correlation between elevation and the incidence of bipolar disorder. However, an analysis of that sort could be important in illuminating a separate contributing factor to a previously demonstrated increase in rates of suicide with elevation. More research in this area could lead to effective adjunctive treatments for individuals with mood disorders living at increased elevations and may help to decrease symptoms and suicidality.
Acknowledgement
We would like to thank NIH Grant MH58681, VISN 19 MIRECC, and the Utah Science Technology and Research (USTAR) initiative for supporting this research.
Role of funding source
Funding for this study was provided by NIH Grant MH58681, the VISN 19 MIRECC, and the Utah Science Technology and Research (USTAR) initiative. The NIH, VISN 19 MIRECC and USTAR had no further role in this study, the writing of the report, or the decision to submit the paper for publication.
Perry F. Renshaw, M.D., Ph.D., M.B.A. is a consultant for Novartis, Roche and Kyowa Hakko. Dr. Renshaw also has research support from GlaxoSmithKline and Roche.
Footnotes
Conflict of interest statement
All other authors report no conflicts of interest.
References
- Allen PJ, D'Anci KE, Kanarek RB, Renshaw PF. Chronic creatine supplementation alters depression-like behavior in rodents in a sex-dependent manner. Neuropsychopharmacology. 2009;35:534–546. doi: 10.1038/npp.2009.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bijl RV, Graaf Rd, Hiripi E, Kessler RC, Kohn R, Offord DR, Ustun TB, Vicente B, Vollebergh WAM, Walters EE, Wittchen H-U. The prevalance of treated and untreated mental disorders in five countries. Health Aff. (Millwood) 2003;22:122–133. doi: 10.1377/hlthaff.22.3.122. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Regional variations in suicide rates - United States, 1990–1994. MMWR Weekly. 1997;46:789–793. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Web-based Injury Statistics Query and Reporting System (WISQARS) 2005 [Google Scholar]
- Forester BP, Harper DG, Jensen JE, Ravichandran C, Jordan B, Renshaw PF, Cohen BM. 31 Phosphorus Magenetic Resonance Spectroscopy study of tissue specific changes in high energy phosphates before and after sertraline treatment of geriatric depression. Int. J. Geriatr. Psychiatry. 2009;24:788–797. doi: 10.1002/gps.2230. [DOI] [PubMed] [Google Scholar]
- Goldberg SV, Schoene RB, Haynor D, Trimble B, Swenson ER, Morrison JB, Banister EJ. Brain tissue pH and ventilatory acclimatization to high altitude. J. Appl. Physiol. 1992;72:58–63. doi: 10.1152/jappl.1992.72.1.58. [DOI] [PubMed] [Google Scholar]
- Hamakawa H, Murashita J, Yamada N, Inubushi T, Kato N, Kato T. Reduced intracellular pH in the basal ganglia and whole brain measured by 31P-MRS in bipolar disorder. Psychiatr. Clin. Neuros. 2004;58:82–88. doi: 10.1111/j.1440-1819.2004.01197.x. [DOI] [PubMed] [Google Scholar]
- Haws CA, Gray DB, Yurgelun-Todd DA, Moskos M, Meyer LJ, Renshaw PF. The possible effect of altitude on regional variation in suicide rates. Med. Hypotheses. 2009;73:587–590. doi: 10.1016/j.mehy.2009.05.040. [DOI] [PubMed] [Google Scholar]
- Hibbeln JR. Fish consumption and major depression. Lancet. 1998;351:1213. doi: 10.1016/S0140-6736(05)79168-6. [DOI] [PubMed] [Google Scholar]
- Hochachka PW, Clark CM, Holden JE, Stanley C, Ugurbil K, Menon RS. 31P magnetic resonance spectroscopy of the Sherpa heart: a phosphocreatine / adenosin triphosphate signature of metabolic defence against hypobaric hypoxia. Proc. Natl Acad. Sci. USA. 1996;93:1215–1220. doi: 10.1073/pnas.93.3.1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iosifescu DV, Bolo NR, Nierenberg AA, Jensen JE, Fava M, Renshaw PF. Brain bioenergetics and response to triiodothyronine augmentation in major depressive disorder. Biol. Psychiatry. 2008;63:1127–1134. doi: 10.1016/j.biopsych.2007.11.020. [DOI] [PubMed] [Google Scholar]
- Kato T, Takahashi S, Shioiri T, Inubushi T. Brain phosphorus metabolism in depressive disordres detected by phosphorus-31 magnetic resonance spectroscopy. J. Affect. Disord. 1992;26:223–230. doi: 10.1016/0165-0327(92)90099-r. [DOI] [PubMed] [Google Scholar]
- Kato T, Takahashi S, Shioiri T, Inubushi T. Alterations in brain phosphorus metabolism in bipolar disorder detected by in vivo 31P and 7Li magnetic resonance spectroscopy. J. Affect. Disord. 1993;27:53–59. doi: 10.1016/0165-0327(93)90097-4. [DOI] [PubMed] [Google Scholar]
- Kato T, Takahashi S, Shioiri T, Murashita J, Hamakawa H, Inubushi T. Reduction of brain phosphocreatine in bipolar II disorder detected by phosphorus-31 magnetic resonance spectroscopy. J. Affect. Disord. 1994;31:125–133. doi: 10.1016/0165-0327(94)90116-3. [DOI] [PubMed] [Google Scholar]
- Kessler R, Chiu W, Demler O, Walters E. Prevalence, severity, and comorbidity of twelve-month DSM-IV disorders in the National Comorbidity Survey Replication (NCS-R) Arch. Gen. Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim N, Mickelson JB, Brenner BE, Haws CA, Yurgelun-Todd DA, Renshaw PF. Altitude, Gun Ownership, Rural Areas, and Suicide. Am J Psychiatry. doi: 10.1176/appi.ajp.2010.10020289. in press. (Epub ahead of print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis G, Booth M. Regional differences in mental health in Great Britain. J. Epidemiol. Commun. H. 1992;46:608–611. doi: 10.1136/jech.46.6.608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyoo IK, Renshaw PF. A pilot study on the efficacy and safety of oral creatine supplementation in females with MDD. Unpublished. [Google Scholar]
- Lyoo IK, Kong SW, Sung SM, Hirashima F, Parow A, Hennen J, Cohen BM, Renshaw PF. Multinuclear magnetic resonance spectroscopy of high-energy phosphate metabolites in human brain following oral choline supplementation of creatine-monohydrate. Psychiatry Res. 2003;123:87–100. doi: 10.1016/s0925-4927(03)00046-5. [DOI] [PubMed] [Google Scholar]
- Moore CM, Christensen JD, Lafer B, Fava M, Renshaw PF. Lower levels of nucleoside triphosphate in the basal ganglia of depressed subjects: a phosphorus-31 magnetic resonance spectroscopy study. Am. J. Psychiatry. 1997;154:116–118. doi: 10.1176/ajp.154.1.116. [DOI] [PubMed] [Google Scholar]
- National Atlas of the United States. County Boundaries of the United States. 2001 [Google Scholar]
- National Geospatial-Intelligence Agency, National Aeronautics and Space Administration. Shutte Radar Topography Mission (STRM) Dataset. Souix Falls, SD: United States Geological Survey; 2000. [Google Scholar]
- Renshaw PF, Parow AM, Hirashima F, Ke Y, Moore CM, Frederick Bd, Fava M, Hennen J, Cohen BM. Multinuclear magnetic resonance spectroscopy studies of brain purines in major depression. Am. J. Psychiatry. 2001;158:2048–2055. doi: 10.1176/appi.ajp.158.12.2048. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration, Office of Applied Statistics. Section D: Substate Region Definitions. Rockville, MD: 2008a. [Google Scholar]
- Substance Abuse and Mental Health Services Administration, Office of Applied Statistics. Substate estimate from the 2004–2006 National Surveys on Drug Use and Health. Rockville, MD: 2008b. [Google Scholar]
- Tempier R, Meadows GN, Vasiliadis H-M, Mosier KE, Lesage A, Stiller A, Graham A, Lepnurm M. Mental disorders and mental health care in Canada and Australia: comparative epidemiological findings. Soc. Psychiatry Psychiatr. Epidemiol. 2008;44:63–72. doi: 10.1007/s00127-008-0409-y. [DOI] [PubMed] [Google Scholar]
- Tondo L, Isacsson G, Baldessarini RJ. Suicidal behaviour in bipolar disorder. CNS Drugs. 2003;17:491–511. doi: 10.2165/00023210-200317070-00003. [DOI] [PubMed] [Google Scholar]
- Volz H-P, Rzanny R, Riehemann S, May S, Hegewald H, Preussler B, Hubner G, Kaiser WA, Sauer H. 31P magnetic resonance spectroscopy in the frontal lobe of major depressed patients. Eur. Arch. Psychiatry Clin. Neurosci. 1998;248:289–295. doi: 10.1007/s004060050052. [DOI] [PubMed] [Google Scholar]
- Weissman M, Bland R, Canino G, Faravelli C, Greenwald S, Hwu H, Joyce P, Karam E, Lee C, Lellouch J, Lepine J, Newman S, Rubio-Stipec M, Wells J, Wickramaratne P, Wittchen H, Yeh E. Cross-national epidemiology of major depression and bipolar disorder. JAMA. 1996;276:292–299. [PubMed] [Google Scholar]
- World Health Organization. The World Health Report 2001: Mental Health: new understanding, new hope. World Health Organization; 2001. [DOI] [PubMed] [Google Scholar]