Abstract
We determined the extent to which adolescents who have never used tobacco try e-cigarettes. Data on the prevalence and correlates of e-cigarette use among 482 179 California middle and high school students are from the 2013–2014 California Healthy Kids Survey.
Overall, 24.4% had ever used e-cigarettes (13.4% have never used tobacco and 11.0% have used tobacco), and 12.9% were current e-cigarette users (5.9% have never used tobacco). Among those who have never used tobacco, males and older students were more likely to use e-cigarettes than females and younger students. Hispanics (odds ratio [OR] = 1.60; confidence interval [CI] = 1.53, 1.67) and those of other races (OR = 1.24; CI = 1.19, 1.29) were more likely than Whites to have ever used e-cigarettes, but only among those who had never used smokeless tobacco and never smoked a whole cigarette.
E-cigarette use is very prevalent among California students who have never smoked tobacco, especially among Hispanic and other race students, males, and older students.
Electronic cigarettes (e-cigarettes) are now the most common tobacco product used by US adolescents.1 E-cigarettes are not currently federally regulated, so relevant policymaking is left to states and localities. Although 40 states have laws prohibiting the sale of e-cigarettes to minors,2 few regulate retailer licensing or public use. Restrictions on e-cigarettes help support tobacco-free norms, because smoke- and vapor-free policies result in diminishing the social acceptability of smoking and vaping.3,4 California, for instance, is currently considering a bill (SB-140) that would recast and broaden the definition of “tobacco product” in current law to include e-cigarettes. Policymakers need empirical evidence about the extent and correlates of adolescents’ e-cigarette use to help them decide how to regulate e-cigarettes.
There are many unanswered questions about e-cigarettes.5,6 Scholars debate whether e-cigarette use among youths encourages conventional cigarette smoking or reflects experimentation with multiple tobacco products,7,8 but a recent longitudinal study finds that e-cigarette users were more likely than were nonusers to report initiation of tobacco use at 1-year follow-up.9 Regardless of whether it’s a gateway to combustible tobacco use, vaping may expose users to toxicants and nicotine (even some that are labeled as having no nicotine), the tobacco-derived addictive substance in conventional cigarettes10–13; however, more studies are needed to understand e-cigarette liquid content, consistency, and labeling concordance.14 For 97% of e-cigarette users, nicotine exposure is a concern; only 3% of e-cigarettes contain no nicotine.15 Because e-cigarettes are relatively new, the long-term health effects of use are unknown. In the meantime, however, youth consumption has increased rapidly in the absence of effective regulation.1
An important question for policymakers is whether youths who have never used other tobacco products use e-cigarettes. Considering the high probability of nicotine and toxicant exposure and the potentially serious health implications,16–18 the precautionary principle suggests that policymakers should treat e-cigarette use as less safe than no use of any tobacco product. By decreasing e-cigarette accessibility and social acceptability, regulation may discourage use, particularly among nonsmoking youths. Youth e-cigarette users are likely to be cigarette smokers, male, older, and White (although evidence on racial and ethnic differences is sparse)1,19; however, the sociodemographic correlates of e-cigarette use among nonsmokers are unknown and may differ from tobacco users.
We examined the prevalence and correlates of e-cigarette use among a diverse sample of California middle and high school students to address the following questions: (1) What is the prevalence of e-cigarette use compared with other tobacco products? (2) To what extent do youths who have never used other tobacco products use e-cigarettes? and (3) What are the sociodemographic correlates of e-cigarette use among those who have never used tobacco products? This information will help public health practitioners define target groups for prevention efforts and will help policymakers assess the need for e-cigarette regulation.
METHODS
Data are from the 2013–2014 California Healthy Kids Survey, which was administered to middle and high school students throughout California and was designed to represent school district populations. Participation was voluntary, anonymous, and confidential, and parental consent was obtained. The analytic sample size was n = 482 179. Participants were asked about ever (at least once in their lifetime) and current (past 30 days) use of e-cigarettes and other tobacco (smokeless tobacco and conventional cigarettes). We coded ever use for each product as 1 for those responding 1 or more times, and 0 for those reporting zero times. We defined current use for each product as using a product on 1 or more days during the past 30 days.
We used descriptive statistics to assess the prevalence of e-cigarette and other tobacco use and multivariable binomial logistic regressions, conducted separately for tobacco users and nonusers, to predict e-cigarette ever use and current use. Covariates included race/ethnicity, gender, age, and highest level of parents’ education. We used a fully interacted model to test for statistically significant differences by tobacco use status.
RESULTS
Nearly one quarter (24.4%) of California students had ever used e-cigarettes, and 12.9% were current e-cigarette users, compared with 15.6% who had ever used and 7.8% who currently used smokeless tobacco or smoked conventional cigarettes (Figure A, available as a supplement to the online version of this article at http://www.ajph.org). Of both ever and current e-cigarette users, the majority had never smoked cigarettes or used smokeless tobacco.
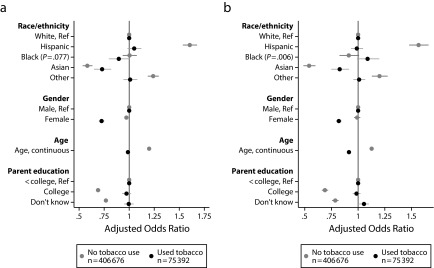
Controlling for sociodemographics (Figure 1a), Hispanics (odds ratio [OR] = 1.60; confidence interval [CI] = 1.53, 1.67) and those of other races (OR = 1.24; CI = 1.19, 1.29) who had never used smokeless tobacco and never smoked a whole cigarette were more likely to ever use e-cigarettes than were Whites. Asians were less likely than Whites to have ever used e-cigarettes, regardless of whether they were tobacco users. Girls’ odds of e-cigarette ever use were 3% lower than boys’ odds among tobacco nonusers (OR = 0.97; CI = 0.95, 0.99; P < .01), whereas among tobacco users girls had 27% lower odds than boys (OR = 0.73; CI = 0.69, 0.75; P < .001). Older age was associated with higher odds of ever use, and higher parental educational attainment with lower odds of ever use, particularly among tobacco nonusers. Results are largely equivalent for current use (Figure 1b).
FIGURE 1—
Correlates of e-cigarette use among tobacco users and nonusers by (a) ever use and (b) current use: California Healthy Kids Survey, 2013–2014.
Note. Separate logistic regressions for tobacco users and nonusers predicting e-cigarette ever use (vs never used) and current use (vs no past 30-day use). Bars indicate 95% confidence intervals. All differences between odds ratios for tobacco users and nonusers are statistically significant at α = .001 unless otherwise noted (2-tailed test).
DISCUSSION
Our results provide empirical evidence on e-cigarette use among California middle and high school students, particularly those who do not use other tobacco products. These estimates will help policymakers who are considering e-cigarette regulation (e.g., public use bans, retailer restrictions) and will be useful as a baseline with which to compare e-cigarette use among California adolescents if SB140 is implemented, which would subject e-cigarettes to the same regulations as other tobacco products.
Several findings are particularly policy relevant: (1) nearly one quarter of our California sample had ever used e-cigarettes (the most popular tobacco product), compared with approximately 11.9% of high school students nationally20; (2) more than 50.0% (nearly 60 000 students in the sample) of those who had used e-cigarettes had never smoked conventional cigarettes—much higher than national estimates; and (3) Hispanic students who had never smoked or used smokeless tobacco were more likely than were non-Hispanic Whites to use e-cigarettes, contrary to earlier national trends.21,22 Policies that decrease adolescent e-cigarette access are a first step. Considering that the regulation of youth access is not always sufficient to deter use,23 comprehensive prevention programs targeting groups that are at higher risk for e-cigarette use (older adolescents, Hispanics, males) are also needed.
With little current regulation on licensing, marketing, or use, e-cigarette use has contributed to an increased prevalence of aggregate tobacco product use among high school students nationally (in 2009, prevalence of current use of any tobacco was 23.9% and in 2014 it was 24.6%), moving us further away from the Healthy People 2020 goal of 21.0%.24 Because of California’s lower rates of youth smoking nationally, it is concerning that its total tobacco use prevalence was higher than the national estimate.
Although this survey was not designed to be representative of all California youths, it is the largest recent state data set on e-cigarette use in this population. Moreover, estimates are consistent with smaller California studies and other estimates.8,25 Because measures are cross-sectional, it is unknown whether e-cigarette use leads to smoking or vice versa. Nevertheless, the key issue of whether e-cigarette marketing recruits nonsmoking students is clear: under current conditions of minimal federal or state regulation, many middle and high school students who have never used conventional cigarettes or smokeless tobacco use e-cigarettes.
Acknowledgments
D. R. T. was supported by the Tobacco-Related Disease Research Program, University of California, Office of the President (grant 23RT-0016). W. J. M. was supported in part by the National Institutes of Health (grant 1P50HL105188#6094).
The authors gratefully acknowledge the helpful comments of Christopher Marcum and the anonymous reviewers.
Human Participant Protection
The Chapman University institutional review board deemed this study exempt because we obtained data from secondary sources.
References
- 1.Centers for Disease Control and Prevention. Tobacco use among middle and high school students—United States, 2011–2014. MMWR Morb Mortal Wkly Rep. 2015;64(14):381–385. [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. State laws prohibiting sales to minors and indoor use of electronic nicotine delivery systems—United States, November 2014. MMWR Morb Mortal Wkly Rep. 2014;63(49):1145–1150. [PMC free article] [PubMed] [Google Scholar]
- 3.US Department of Health and Human Services. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. 2014. Atlanta, GA. [Google Scholar]
- 4.Duke JC, Lee YO, Kim AE et al. Exposure to electronic cigarette television advertisements among youth and young adults. Pediatrics. 2014;134(1):e29–e36. doi: 10.1542/peds.2014-0269. [DOI] [PubMed] [Google Scholar]
- 5.Grana R, Benowitz N, Glantz SA. E-cigarettes: a scientific review. Circulation. 2014;129(19):1972–1986. doi: 10.1161/CIRCULATIONAHA.114.007667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Etter JF. E-cigarettes: methodological and ideological issues and research priorities. BMC Med. 2015;13:32. doi: 10.1186/s12916-014-0264-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Delnevo CD, Bover Manderski MT, Giovino GA. Youth tobacco use and electronic cigarettes. JAMA Pediatr. 2014;168(8):775–776. doi: 10.1001/jamapediatrics.2014.733. [DOI] [PubMed] [Google Scholar]
- 8.Dutra LM, Glantz SA. Electronic cigarettes and conventional cigarette use among US adolescents: a cross-sectional study. JAMA Pediatr. 2014;168(7):610–617. doi: 10.1001/jamapediatrics.2013.5488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Leventhal AM, Strong DR, Kirkpatrick MG et al. Association of electronic cigarette use with initiation of combustible tobacco product smoking in early adolescence. JAMA. 2015;314(7):700–707. doi: 10.1001/jama.2015.8950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goniewicz ML, Knysak J, Gawron M et al. Levels of selected carcinogens and toxicants in vapour from electronic cigarettes. Tob Control. 2014;23(2):133–139. doi: 10.1136/tobaccocontrol-2012-050859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Trehy ML, Ye W, Hadwiger ME et al. Analysis of electronic cigarette cartridges, refill solutions, and smoke for nicotine and nicotine related impurities. J Liq Chromatogr Relat Technol. 2011;34(14):1442–1458. [Google Scholar]
- 12.Goniewicz ML, Kuma T, Gawron M, Knysak J, Kosmider L. Nicotine levels in electronic cigarettes. Nicotine Tob Res. 2013;15(1):158–166. doi: 10.1093/ntr/nts103. [DOI] [PubMed] [Google Scholar]
- 13.Schober W, Szendrei K, Matzen W et al. Use of electronic cigarettes (e-cigarettes) impairs indoor air quality and increases FeNO levels of e-cigarette consumers. Int J Hyg Environ Health. 2014;217(6):628–637. doi: 10.1016/j.ijheh.2013.11.003. [DOI] [PubMed] [Google Scholar]
- 14.Orr MS.Electronic cigarettes in the USA: a summary of available toxicology data and suggestions for the future Tob Control 201423suppl 2ii18–ii22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Etter JF, Bullen C. Electronic cigarette: users profile, utilization, satisfaction and perceived efficacy. Addiction. 2011;106(11):2017–2028. doi: 10.1111/j.1360-0443.2011.03505.x. [DOI] [PubMed] [Google Scholar]
- 16.Suter MA, Mastrobattista J, Sachs M, Aagaard K. Is there evidence for potential harm of electronic cigarette use in pregnancy? Birth Defects Res A Clin Mol Teratol. 2015;103(3):186–195. doi: 10.1002/bdra.23333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schraufnagel DE. Electronic cigarettes: vulnerability of youth. Pediatr Allergy Immunol Pulmonol. 2015;28(1):2–6. doi: 10.1089/ped.2015.0490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.England LJ, Bunnell RE, Pechacek TF, Tong VT, McAfee TA. Nicotine and the developing human: a neglected element in the electronic cigarette debate. Am J Prev Med. 2015;49(2):286–293. doi: 10.1016/j.amepre.2015.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Carroll Chapman SL, Wu L-T. E-cigarette prevalence and correlates of use among adolescents versus adults: a review and comparison. J Psychiatr Res. 2014;54:43–54. doi: 10.1016/j.jpsychires.2014.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention. Tobacco use among middle and high school students—United States, 2013. MMWR Morb Mortal Wkly Rep. 2014;63(45):1021–1026. [PMC free article] [PubMed] [Google Scholar]
- 21.Camenga DR, Delmerico J, Kong G et al. Trends in use of electronic nicotine delivery systems by adolescents. Addict Behav. 2014;39(1):338–340. doi: 10.1016/j.addbeh.2013.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pepper JK, Reiter PL, McRee A-L, Cameron LD, Gilkey MB, Brewer NT. Adolescent Males’ Awareness of and Willingness to Try Electronic Cigarettes. J Adolesc Health. 2013;52(2):144–150. doi: 10.1016/j.jadohealth.2012.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Richardson L, Hemsing N, Greaves L et al. Preventing smoking in young people: a systematic review of the impact of access interventions. Int J Environ Res Public Health. 2009;6(4):1485–1514. doi: 10.3390/ijerph6041485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.US Department of Health and Human Services. Healthy People 2020. 2015. Washington, DC. [DOI] [PubMed] [Google Scholar]
- 25.Al-Delaimy WK, Myers MG, Leas EC, Strong DR, Hofstetter CR. E-cigarette use in the past and quitting behavior in the future: a population-based study. Am J Public Health. 2015;105(6):1213–1219. doi: 10.2105/AJPH.2014.302482. [DOI] [PMC free article] [PubMed] [Google Scholar]