Abstract
We compared the prevalence of respiratory disease in former and current US coal miners using chest radiographs and lung functions collected from 2009 to 2013 among miners of the Appalachian and Interior US coalfields. We calculated prevalence ratios (PRs) of pneumoconiosis and impaired lung function. Significantly higher prevalences of pneumoconiosis (PR = 1.5; 95% confidence interval = 1.2, 2.0) and impaired lung function were observed among former miners compared with active miners. Former miners continue to suffer negative health effects from occupational coal mine dust exposure. The respiratory health of active and former miners is a global concern because international coal production is projected to increase for decades to come.
The term coal mine dust lung disease recently has been used to describe the spectrum of respiratory conditions, including pneumoconiosis, associated with chronic coal mine dust exposure.1 Coal mine dust lung disease can progress or manifest after a miner has left a job that exposed him or her to dust.2,3 Between the 1970s and 1990s, the prevalence of pneumoconiosis and progressive massive fibrosis declined precipitously. However, starting in 1999, this trend reversed with increases in both forms of the disease.4,5
Since 1970, active, but not former, underground miners in the United States have been eligible for periodic chest radiograph screening through the National Institute for Occupational Safety and Health’s (NIOSH) Coal Workers’ Health Surveillance Program. The severity of coal mine dust lung disease among former miners is not well understood. We surveyed former miners to determine the prevalence of pneumoconiosis and lung function impairment, comparing findings to those of active miners.
METHODS
Between 2012 and 2013, NIOSH’s Enhanced Coal Workers’ Health Surveillance Program mobile surveillance unit traveled to coal mining regions in Alabama, Illinois, Indiana, Kentucky, Pennsylvania, Virginia, and West Virginia and offered chest radiographs and lung function testing (spirometry) to active and former coal miners, as previously described by Blackley et al.6 A comparison group of active underground coal miners who participated in the regular Coal Workers’ Health Surveillance Program and in the Enhanced Coal Workers’ Health Surveillance Program during 2009 to 2013 was assembled. Both programs collected work histories, demographics, and smoking status (never, current, former). Spirometry was available only for Enhanced Coal Workers’ Health Surveillance Program participants.
We included only miners with 10 years or more of mining tenure in the analyses. We performed modified Poisson regression analysis using SAS version 9.3 (SAS Institute, Cary, NC) PROC GENMOD procedure with a robust error variance procedure7 to estimate prevalence ratios8 comparing disease among former miners with disease among active miners, adjusting for potentially confounding factors.
RESULTS
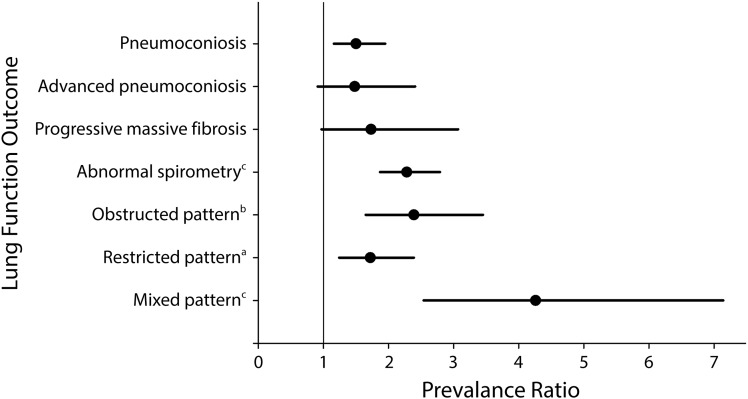
After controlling for mining tenure, being a former miner was associated with a significantly higher prevalence of pneumoconiosis (prevalence ratio = 1.50; 95% confidence interval [CI] = 1.16, 1.95; Figure 1). After controlling for mining tenure, smoking, and body mass index (BMI; defined as weight in kilograms divided by height in meters squared), being a former miner was associated with a significantly higher prevalence of abnormal spirometry (prevalence ratio = 2.28; 95% CI = 1.87, 2.79) and mixed pattern impairment (prevalence ratio = 4.26; 95% CI = 2.54, 7.14).
FIGURE 1—
Prevalence ratio estimates comparing coal mine dust lung disease in former miners with disease in active miners: United States, 2009 to 2013.
Note. Prevalence ratio estimates are represented by the closed circle with a solid line representing corresponding 95% confidence intervals. All estimates were derived while controlling for mining tenure. In addition to mining tenure, the confounders body mass index (BMI; defined as weight in kilograms divided by the square of height in meters) and ever smoker were controlled for depending on the lung function outcome of interest:
aBMI.
bEver smoker.
cBMI and ever smoker.
Former miners had higher prevalence of obstructive impairment when controlling for mining tenure and smoking (prevalence ratio = 2.39; 95% CI = 1.65, 3.45) and a higher prevalence of restrictive impairment when adjusting for mining tenure and BMI (prevalence ratio = 1.72; 95% CI = 1.24, 2.39).
DISCUSSION
Despite the cessation of exposure to coal mine dust for a median 14 years, former miners had significantly higher prevalence of pneumoconiosis and lung function impairment (all patterns) when compared with active miners. Lung function impairment is associated with cumulative exposure to coal mine dust regardless of the presence or absence of radiographic pneumoconiosis.9 Increased prevalence of impaired lung function is important clinically, because previous studies of coal miners found an association between decreased lung function and increased incidence of self-reported respiratory symptoms, diagnosis of respiratory disease, and greater risk of mortality from cardiovascular disease and chronic obstructive pulmonary disease.10
The consequences of exposure to respirable coal mine dust among miners are well established. Control technologies and best practice guidance are readily available to prevent these consequences, yet we continue to identify and document coal mine dust lung disease in active and former miners. Given the resurgence of pneumoconiosis in the United States since 1999, with the most prominent increases occurring in central Appalachia,4,11 and the decline in numbers of active miners,12 we unfortunately anticipate that the prevalence of coal mine dust lung disease will increase in former miners in the coming years.
Acknowledgments
The authors would like to thank David Blackley, DrPH, Robert Cohen, MD, and Mei Lin Wang, MD, for helpful feedback during the preparation of the brief and the staff of the Coal Workers’ Health Surveillance Program.
Human Participant Protection
The Coal Workers Health Surveillance Program has a nonresearch designation and is exempt from human subjects review board approval (NIOSH:11-DRDS-NR03) as a surveillance activity. All participants provided written informed consent.
References
- 1.Petsonk EL, Rose C, Cohen R. Coal mine dust lung disease: New lessons from old exposure. Am J Respir Crit Care Med. 2013;187(11):1178–1185. doi: 10.1164/rccm.201301-0042CI. [DOI] [PubMed] [Google Scholar]
- 2.Dimich-Ward H, Bates DV. Reanalysis of a longitudinal study of pulmonary function in coal miners in Lorraine, France. Am J Ind Med. 1994;25(5):613–623. doi: 10.1002/ajim.4700250502. [DOI] [PubMed] [Google Scholar]
- 3.Kimura K, Ohtsuka Y, Kaji H et al. Progression of pneumoconiosis in coal miners after cessation of dust exposure: a longitudinal study based on periodic chest x-ray examinations in Hokkaido, Japan. Intern Med. 2010;49(18):1949–1956. doi: 10.2169/internalmedicine.49.2990. [DOI] [PubMed] [Google Scholar]
- 4.Blackley DJ, Halldin CN, Laney AS. Resurgence of a debilitating and entirely preventable respiratory disease among working coal miners. Am J Respir Crit Care Med. 2014;190(6):708–709. doi: 10.1164/rccm.201407-1286LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Laney AS, Weissman DN. Respiratory diseases caused by coal mine dust. J Occup Environ Med. 2014;56(suppl 10):S18–S22. doi: 10.1097/JOM.0000000000000260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Blackley DJ, Halldin CN, Wang ML, Laney AS. Small mine size is associated with lung function abnormality and pneumoconiosis among underground coal miners in Kentucky, Virginia and West Virginia. Occup Environ Med. 2014;71(10):690–694. doi: 10.1136/oemed-2014-102224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–706. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 8.Deddens JA, Petersen MR. Approaches for estimating prevalence ratios. Occup Environ Med. 2008;65(7):501–506. doi: 10.1136/oem.2007.034777. 481. [DOI] [PubMed] [Google Scholar]
- 9.Attfield MD, Hodous TK. Pulmonary function of US coal miners related to dust exposure estimates. Am Rev Respir Dis. 1992;145(3):605–609. doi: 10.1164/ajrccm/145.3.605. [DOI] [PubMed] [Google Scholar]
- 10.Beeckman LA, Wang ML, Petsonk EL, Wagner GR. Rapid declines in FEV1 and subsequent respiratory symptoms, illnesses, and mortality in coal miners in the United States. Am J Respir Crit Care Med. 2001;163(3 pt 1):633–639. doi: 10.1164/ajrccm.163.3.2008084. [DOI] [PubMed] [Google Scholar]
- 11.Antao VC, Petsonk EL, Sokolow LZ et al. Rapidly progressive coal workers’ pneumoconiosis in the United States: geographic clustering and other factors. Occup Environ Med. 2005;62(10):670–674. doi: 10.1136/oem.2004.019679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.US Department of Labor, Mine Safety and Health Administration. Number of injuries, injury-incidence rates, average number of employees, employee-hours, and production by type of coal mined and work location: 2009–2013. 2013. Available at: http://www.msha.gov/ACCINJ/ALLCOAL.HTM. Accessed August 31, 2015.