Abstract
Objectives. We examined independent and synergistic effects of school and neighborhood environments on preadolescent body mass index (BMI) to determine why obesity rates nearly double during preadolescence.
Methods. Physical measures and health surveys from fifth and sixth graders in 12 randomly selected schools in New Haven, Connecticut, in 2009 were matched to student sociodemographics and school- and residential census tract–level data, for a total of 811 urban preadolescents. Key independent variables included school connectedness, neighborhood social ties, and school and neighborhood socioeconomic status. We estimated cross-classified random-effects hierarchical linear models to examine associations between key school and neighborhood characteristics with student BMI.
Results. Greater average connectedness felt by students to their school was significantly associated with lower BMI. This association was stronger among students living in neighborhoods with higher concentrations of affluent neighbors.
Conclusions. How schools engage and support students may affect obesity rates preferentially in higher-income neighborhoods. Further research should explore the associations between multiple environments to which children are exposed and obesity-related behaviors and outcomes. This understanding of the multiple social–spatial contexts that children occupy has potential to inform comprehensive and sustainable child obesity prevention efforts.
Approximately 17% of the children in the United States aged 2 to 19 years are obese.1 Obesity has both short- and long-term health consequences through adulthood.2–5 A vast field of research has struggled to identify factors contributing to this epidemic that are most amenable to change. Recent research has used ecological frameworks to explore risks for childhood obesity at multiple levels,6 including school7 and neighborhood8 contexts, yet few studies have explored these contexts simultaneously.9–11 Despite the fact that obesity rates nearly double during preadolescence,12 few studies have explored contextual effects specific to this age group.13
NEIGHBORHOODS AND PREADOLESCENT OBESITY
Residential neighborhood factors influence childhood development and well-being.14 As has been found among adults,15 lower neighborhood socioeconomic status (SES) has been associated with childhood obesity and related behaviors such as diet and exercise.16–18 Among adults, this association may relate to factors such as access to healthy food and places to exercise,15 neighborhood safety,19 the existence of neighborhood social ties or cohesion,20–22 and health norms among social networks.23,24 Among children, however, and particularly among preadolescent children, the evidence is much more limited.
Most studies among preadolescent children have focused on characteristics of the neighborhood-built environment that influence diet, exercise, and body mass index (BMI; defined as weight in kilograms divided by the square of height in meters). Studies among younger children have found that proximity to convenience stores and fast food outlets is associated with higher body weight11,25,26 and unhealthy food intake,26 whereas proximity to supermarkets and produce markets is associated with lower body weight.11,26,27 One study found that rates of preadolescent physical activity were associated with greater perceived access to parks, playgrounds, and gyms, and more neighborhood social ties, but not to perceptions of neighborhood safety.28 Another study of girls aged 9 to 10 years found that living in high-income areas was associated with less sedentary activity,29 suggesting that levels of neighborhood advantage, and not just disadvantage, also may be associated with the risk of childhood obesity. Finally, the only social environment inquiries among preadolescent children have focused on peer social ties and networks, showing that physically active middle school students are more likely to have physically active friends.30 However, these social ties were not specifically tied to the neighborhood context.
SCHOOLS AND PREADOLESCENT OBESITY
Obesity rates also differ significantly by school. Although a recent review found insufficient evidence to suggest a relation between the internal school physical environment and child obesity,31 a promising area of research focuses on the internal school psychosocial environment. Our own prior study modeling school differences in BMI found that students attending schools with a more positive school climate, characterized by supportive and caring educators who care about students’ learning and well-being, had lower average BMI compared with students in schools with less positive school climate.32
School connectedness is a component of school climate and refers to the sense of attachment and loyalty students have to their school.33 This construct is similar to neighborhood social cohesion.34 Although this literature is new, research has shown a protective association of school connectedness with lower risk of chronic illnesses,35 fewer depression and anxiety symptoms,36 fewer risk-taking behaviors,37 fewer bullying incidents,38 and lower odds of smoking.39
NEIGHBORHOODS VS SCHOOLS AND PREADOLESCENT OBESITY
Given that children spend substantial time at both school and home, it is important to consider the cumulative or interactive effects of school and neighborhood environments on child obesity-related health behaviors and weight. Although several studies have described interactions between school and neighborhood characteristics on a variety of outcomes, we found only 3 studies that examined the simultaneous associations of school and neighborhood contexts on obesity-related outcomes among preadolescents.
Of these studies, 1 found no significant association between school and home food environments on diet or BMI.9 However, this study was limited to publicly available retailer data and self-reported BMI. A second study explored associations of home and school neighborhood environments with physical activity levels and found that attributes of each context were uniquely associated with overall activity levels.10 The authors argued that youths spend time in multiple contexts, so examining only 1 environment underestimates the environmental determinants of physical activity. However, this study included preadolescents and adolescents in the same sample and did not examine differences in age groups. A third study found that among 9- to 10-year-old girls who walked or biked to school, fat mass index was lower among those who lived in neighborhoods with healthy food outlets and higher among those with more access to unhealthy outlets on their route to school and surrounding their school.11 Nevertheless, this study was conducted in rural United Kingdom and is thus likely not generalizable to urban US preadolescents.
CURRENT INVESTIGATION
In this study, we explored the independent and interactive associations of neighborhood and school socioeconomic and social contexts with BMI among an urban sample of preadolescents, above and beyond known differences by individual-level factors such as SES and race/ethnicity. We hypothesized that BMI would be associated with characteristics of each environment independently and that positive (or negative) attributes of each would interact and be associated with lower (or higher) BMI.
We conducted this study in New Haven, Connecticut, a city of approximately 130 000 that experiences persistent socioeconomic and health disparities.40,41 The city school district is largely an interdistrict school choice system, meaning that students do not always attend school in their residential neighborhood nor necessarily live in the same neighborhood as their school friends. New Haven is therefore an ideal place to explore the unique role of school and neighborhood social–spatial contexts on disparities in obesity.
METHODS
Data for this study were drawn from the Community Interventions for Health study, a longitudinal, school-stratified study of preadolescent students from 12 randomly selected schools (kindergarten through eighth grade) in New Haven. Detailed study procedures are described elsewhere.42,43 All fifth- and sixth-grade students (n = 1312) were invited to participate in the study. Response rate for the survey was 83% (n = 1094). Parental consent included opt-out forms sent home with each student. On the day data were collected, students were allowed to opt out of the survey or physical measures data collection.
We collected student data in fall 2009 and included both health surveys and physical measurements. Surveys containing 55 items that assessed health, health behaviors, and neighborhood health environments were administered online in computer laboratories during computer classes. Trained research staff read the survey aloud while children confidentially responded online, with assistance given as needed. We used data from 9 of these items in the current analysis, including diet, exercise, and neighborhood social ties.
Trained research staff collected physical measurements in a private area during gym class. Height and weight were measured according to the World Health Organization Expanded STEPS protocol.44 A standardized stadiometer (Charder Electronic Co, Ltd, Taichung City, Taiwan) and electronic flat scale (Seca Co, Hamburg, Germany) were used to measure height to the nearest half-centimeter and weight to the nearest tenth of a kilogram.
Supplementary data came from several sources. Student sociodemographic characteristics were extracted from records updated annually and provided by our school district partners. These were merged with survey and physical measures via student identification number.
Neighborhood-level data were drawn from the US census or aggregated from student records. Census tracts were used to approximate neighborhoods in this study, as tracts in New Haven are closely aligned with locally derived neighborhood boundaries.45 We used ArcGIS software (Esri, Redlands, CA) to geocode and link student addresses to 2000 US Census data by census tract identifiers (FIPS codes).
School-level data came from the 2009 to 2010 School Learning Environment survey, an independent district-wide survey conducted annually by the Connecticut Department of Education that collects data directly from each of the study school’s students, teachers, and parents. This survey includes questions on academic expectations, school communication, student engagement, safety and respect, and collaboration.
Analytic Sample
Of the 1094 total students who took the health survey, we were unable to include 283 in this study because of absence on the day of the physical data collection, missing address for geocoding, or other missing study variable data. Therefore, the final analytic sample for this investigation included the 811 students with complete data. Because this sample represents only 74% of the survey respondents, we ran a sensitivity analysis on those excluded by comparing them with those included on all final model variables, and we controlled for clustering due to school-based sampling. The only significant differences were that excluded students were more likely to be of higher SES according to our single measure of eligibility for reduced-price or free lunch program (odds ratio [OR] = 2.03; P < .01) and reported slightly more social ties in their neighborhoods (mean = 3.3 vs 3.0, respectively; P = .01) compared with those who were included in the analyses. We thus controlled for these 2 variables in all analyses.
The analytic sample of neighborhoods included 25 of the 29 total census tracts in New Haven in which the student sample was represented. The tracts contained between 6 and 85 students (mean = 32). The school sample included the 12 randomly selected kindergarten through eighth-grade study schools.
Student Body Mass Index
We used measured student heights and weights to calculate BMI for each child, which we then converted to BMI percentile based on age- and gender-adjusted Centers for Disease Control and Prevention growth charts.46
Neighborhood Social and Socioeconomic Environment
Neighborhood social ties.
Students answered 3 survey items to assess neighborhood social ties: (1) “How many of the grown-ups in your neighborhood do you know?”; (2) “How many of the kids and teens do you know?”; and (3) “Now think about your closest friends; do any of them live in your neighborhood?” (adapted from Los Angeles Family and Neighborhood Survey).47 Ordinal responses, ranging from 0 (knows none) to 5 (knows most), were averaged to create a mean scale of peer and intergenerational ties. The mean scale was aggregated to the neighborhood level as an indicator of neighborhood-level social environment.
Concentrated affluence.
We created a factor-weighted scale to capture the upper extreme of the socioeconomic spectrum to measure the relative affluence of a neighborhood. The argument for examining affluence as its own construct is that as poverty has become more geographically concentrated, so have neighborhoods characterized by higher educational attainment, income levels, and occupations.34 US census variable indicators of concentrated affluence included percentage of residents aged 25 years or older with a college education, percentage of households with high income (> $75 000/year), and percentage of residents who are executives or professionals.34
Concentrated disadvantage.
We created another factor-weighted scale to measure the opposite end of the socioeconomic spectrum defined by 4 tract-level census characteristics: percentage living below the poverty line, percentage receiving public assistance, percentage of female-headed families with children, and percentage who were unemployed.34 The use of a multidimensional cluster of neighborhood traits provides a more comprehensive perspective on the social ecology of neighborhoods than does the use of a poverty measure alone.48 We simultaneously modeled both ends of the socioeconomic continuum to determine their relative importance.49
School Social and Socioeconomic Environment
School connectedness.
Our measure of school connectedness was based on Resnick’s School Connectedness Scale50 and was created from a subset of 5 items from the school district’s School Learning Environment survey that was collected from only the student respondents. The 5 survey items were
“I feel safe in this school,”
“There is at least 1 adult in this school that knows me well,”
“Overall, I feel good about this school,”
“I feel welcomed in my school,” and
“I am treated fairly in this school.”
All items were collected on a response scale from 1 (strongly disagree) to 5 (strongly agree) and combined into an additive scale with total scores ranging from 5 to 25 (Cronbach α = 0.94).
School socioeconomic status.
The percentage of students who qualify for the free or reduced-price school lunch program was our best available measure of students’ family SES. Although not an ideal measure,51 it is used frequently in student studies because of its universal access in school settings.52
Student-Level Control Variables
Fruit and vegetable intake.
We asked students how many days per week they usually eat fruits and vegetables and their usual number of servings per day.48 We calculated average daily fruit and vegetable consumption to classify them as meeting or not meeting current dietary guidelines (US Department of Agriculture Center for Nutrition Policy and Promotion),53 a benchmark for healthy dietary behaviors.
Physical activity.
We used 2 items to create a dichotomous variable of students who meet current US guidelines for children of 60 minutes of exercise per day54: “In the past week, how many days did you exercise for at least 30 minutes (e.g., walking, playing, sports, gym/PE class)” (adapted from Patrick et al.55) and (2) “How long do you usually exercise on these days?”
Neighborhood social ties.
The individual-level mean scale score of neighborhood social ties was used as a control variable to ensure that the neighborhood aggregate scale truly represented social ties among all students in the neighborhood, above and beyond what any individual student reported.
Sociodemographic control variables.
Individual-level demographic controls included age, race/ethnicity, gender, and individual-level qualification for free or reduced-price school lunch program (yes/no). Tract-level controls included percentage of residents who were Black or Latino, drawn from US census data. School-level controls included the percentage of Black and Latino students, drawn from state data.
Statistical Analysis
We estimated cross-classified random-effects hierarchical linear models, in which students were simultaneously nested within schools and neighborhoods, to examine associations and interactions between key school and neighborhood characteristics and student BMI, above and beyond control variables. We estimated multilevel regression models with PROC MIXED in SAS version 9.3 (SAS Institute, Cary, NC) and used maximum likelihood estimation method to calculate model parameters.
To make interpretation of the model more meaningful, the social ties scale score was centered around the grand mean, and continuous neighborhood- and school-level predictor variables were centered around neighborhood- and school-level group means, respectively.56
RESULTS
Table 1 presents means and SDs or frequencies and percentages for all individual-, school-, and neighborhood-level variables included in analyses. The mean BMI percentile indicates that, on average, the students in this sample had higher BMIs than 72% of their peers nationally, indicating an above-average risk of overweight and obesity. The students in our sample were predominantly Black and Latino, were from low-income families, and reported diet and exercise behaviors well below national recommendations.
TABLE 1—
Sample Description, 25 Census Tracts, and 12 Schools: Community Interventions for Health Study, Student Module, New Haven, Connecticut, 2009
| Variable | No. (%) or Mean ±SDa |
| Student-level variables (n = 811) | |
| BMI percentile | 71.8 ±29.52 |
| BMI z score | 0.81 ±1.17 |
| Latino | 392 (48.3) |
| Black | 327 (40.3) |
| White/other | 92 (11.3) |
| Eligible for free or reduced-price lunch | 734 (90.5) |
| Meets 2010 dietary guidelines for fruit and vegetable intake | 26 ±3.21 |
| Exercises 1 h each day | 176 (21.7) |
| Neighborhood social ties (0–5) | 3.00 ±1.32 |
| Neighborhood-level variables (n = 25) | |
| % Latino | 24.84 ±18.52 |
| % Black | 39.36 ±19.84 |
| Concentrated affluence | 23.99 ±14.12 |
| Concentrated disadvantage | 17.26 ±6.99 |
| Aggregated neighborhood social ties (0–5) | 3.05 ±0.05 |
| School-level variables (n = 12) | |
| % Latino | 46.92 ±28.88 |
| % Black | 37.43 ±24.30 |
| % eligible for free or reduced-price lunch | 82.70 ±9.71 |
| School Connectedness Scale (5–25) | 19.34 ±1.51 |
Note. BMI = body mass index.
Mean ±SD for continuous variables and No. (%) for categorical variables.
Table 2 presents results from the cross-classified random-effects model that examined the unique and interactive associations of neighborhood- and school-level variables with individual student BMI percentiles, while controlling for individual-, neighborhood-, and school-level sociodemographic variables. We found a significant association between school connectedness and BMI percentile (B = −2.31; 95% confidence interval [CI] = −4.43, −0.20; P = .03), such that individual students’ BMI percentile decreased by approximately 2.3 percentage points for each 1-unit increase in the school connectedness scale for students from a neighborhood with concentrated affluence at the mean. This was true even when holding dietary and exercise behaviors and sociodemographic risk factors constant. Neighborhood-level social ties, concentrated affluence, and concentrated disadvantage indices had no significant main effects on BMI. However, explorations of interactive effects identified a significant interaction between concentrated affluence and school connectedness (B = −0.15; 95% CI = −0.30, −0.01; P = .03); the decrease in BMI percentile as school connectedness increased was larger as neighborhood concentrated affluence increased.
TABLE 2—
Cross-Classified Random-Effects Model Predicting Body Mass Index Percentile: Community Interventions for Health Study, Student Module, New Haven, Connecticut, 2009
| Variable | B (95% CI) | SE |
| Student-level variables (n = 811) | ||
| Latino | 11.25** (3.29, 19.22) | 4.06 |
| Black | 12.63** (4.51, 20.75) | 4.14 |
| Eligible for free or reduced-price lunch | −2.33 (−10.78, 6.13) | 4.31 |
| Meets 2010 dietary guidelines for fruit and vegetable intake | −8.87 (−20.20, 2.45) | 5.77 |
| Exercises 1 h each day | −1.91 (−6.89, 3.06) | 2.53 |
| Neighborhood social ties scale (0–5)a | −2.65** (−4.28, −1.02) | 0.83 |
| Neighborhood-level variables (n = 25)b | ||
| % Latino | 0.22 (−0.08, 0.52) | 0.15 |
| % Black | 0.03 (−0.19, 0.25) | 0.11 |
| Concentrated affluence | 0.00 (−0.35, 0.35) | 0.18 |
| Concentrated disadvantage | −0.11 (−0.97, 0.74) | 0.43 |
| Aggregated neighborhood social ties (0–5) | 6.53 (−2.57, 15.64) | 4.64 |
| School-level variables (n = 12)c | ||
| % Latino | −0.04 (−0.34, 0.27) | 0.16 |
| % Black | −0.10 (−0.39, 0.20) | 0.15 |
| % eligible for free or reduced-price lunch | −0.15 (−0.69, 0.38) | 0.27 |
| School Connectedness Scale (5–25) | −2.31* (−4.43, −0.20) | 1.08 |
| Interaction: concentrated affluence × School Connectedness Scale | −0.15* (−0.30, −0.01) | 0.07 |
| Intercept | 70.93*** (57.54, 84.32) | 5.66 |
Note. CI = confidence interval.
Continuous, individual-level independent variables were centered about the grand mean.
Continuous neighborhood-level independent variables were centered about the neighborhood-level mean.
Continuous school-level independent variables were centered about the school-level mean.
*P < .05; **P < .01; ***P < .001.
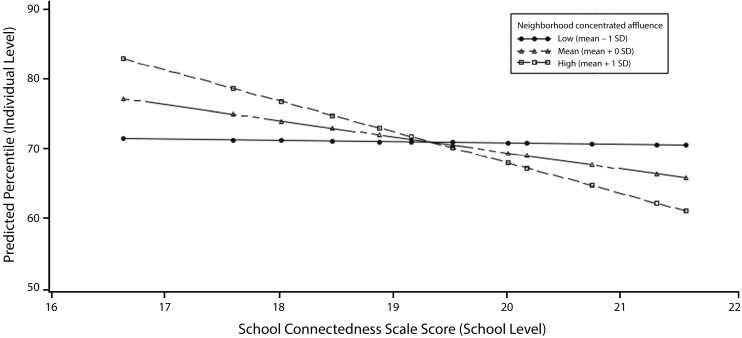
Figure 1 presents predicted values for the BMI percentile across the range of School Connectedness Scale scores at 3 different levels of neighborhood concentrated affluence, with other covariates fixed at their averages and other cofactors fixed at 0. Figure 1 shows that the association of school connectedness with BMI percentile is stronger as neighborhood affluence increases. The slope is steepest for students living in a neighborhood at 1 SD above the mean level of affluence. The slope is comparatively less steep for students living in a neighborhood at the mean level of affluence and is almost flat (suggesting no association) for students living in a neighborhood 1 SD below the mean affluence level. The interaction between school connectedness and neighborhood disadvantage was nonsignificant and therefore was not included in the model.
FIGURE 1—
Association of body mass index percentile with school connectedness in urban preadolescents, by level of neighborhood concentrated affluence: New Haven, Connecticut, 2009.
Note. Displayed are predicted values for the body mass index percentile across the range of School Connectedness Scale scores at 3 different levels of Neighborhood Concentrated Affluence, with other covariates fixed at their averages and other cofactors fixed at 0; predictions are based on a cross-classified random effects model.
DISCUSSION
Our results indicate that higher school connectedness is associated with lower BMIs. Despite no direct association of neighborhood affluence with BMI, the association of school connectedness and BMI was much stronger among children living in more affluent neighborhoods than among children from less affluent neighborhoods. Neighborhood disadvantage had no direct association with BMI and did not interact with school connectedness.
Our study adds healthier BMI to the list of positive health outcomes previously associated with school connectedness. In our sample of students, a 1-unit increase in the school connectedness scale equated to a 33% reduction of obesity (≥ 95th BMI percentile) and a 17% reduction of overweight (≥ 85th and < 95th BMI percentile) for students from a neighborhood with concentrated affluence at the mean. These findings are consistent with evidence that school connectedness is a protective factor for child behavioral, cognitive, and achievement outcomes.14 Similar to the neighborhood social cohesion literature,34 schools in which students feel supported and socially connected may foster healthier social norms, such as the social acceptability of fruit and vegetable consumption, physical activity, or a lower average BMI.57 However, there was no association among students living in poorer neighborhoods. Students from more disadvantaged neighborhoods may experience stressors in their home or neighborhood environments, such as food insecurity or exposure to community violence, that make a positive school environment or school connectedness less relevant for their weight or related health behaviors.58–60 Conversely, students living in neighborhoods with more affluent neighbors had a stronger negative association between school climate and BMI. More affluent neighborhoods may confer benefits of healthier social norms or improved access to healthy foods, allowing students to better leverage the advantages of a positive school climate to maintain healthier behaviors.8,61
Limitations and Strengths
This study had several limitations. We were limited by our single individual-level family SES variable and had no other family-level data with which to more precisely model family socioeconomic environment as separate from neighborhood factors. This was partly because of our inability to survey parents and guardians as a result of school district wishes. Future research should collect data from parents and students to get a better assessment of family SES and neighborhood environments. We lacked the sample size and statistical power to include more school- and neighborhood-level explanatory variables. Finally, our data were cross-sectional, and therefore, caution must be taken when interpreting our findings. We cannot draw conclusions about the direction of effects or examine the mechanisms through which neighborhood affluence influences the relation between school connectedness and BMI.
Despite these limitations, a strength of this study was working with our school district partners to link primary student health data to existing student and school data; this novel method minimized data collection burden on the schools and maximized utility of existing data. This cross-sectional exploration of school connectedness, neighborhood affluence, and BMI is a critical step to understanding how school and neighborhood environments interact to affect preadolescent obesity.
Future research must explore the longitudinal effect of positive changes in school connectedness on student BMI as well as the dynamic nature of student exposures to schools and neighborhoods and associated social ties and interactions over time. Such research would allow tests of causality, directionality, and potential mechanisms of action. Additional research into the School Connectedness Scale and related school climate scales is also important to explore different dimensions of school connectedness and how they relate to obesity and other health behaviors and outcomes in different samples.
Our results extend previous research by examining objectively measured preadolescent BMI in relation to school connectedness and neighborhood affluence and by modeling individual, school, and neighborhood effects independently and simultaneously.
Conclusions
Our findings indicate that both neighborhood and school environments are important for understanding and addressing child obesity. For maximum effect of obesity prevention programs, we must discuss multicontextual programs that build on the realities and complexities of the contexts to which children are exposed. Research and prevention efforts on child obesity must include all aspects of children’s lives—their neighborhood, their school, and the health habits that are developed and reinforced in each setting. Our study suggests that schools that engage and support their students may play a positive role in student weight and thus should continue to be explored as a potential factor in efforts to curb the obesity epidemic. However, our results indicate that well-intentioned school climate interventions may benefit only students from higher-income neighborhoods if broader social inequalities persist.
Further research is needed that explores the simultaneous and interactive associations between the multiple environments to which children are exposed and a variety of obesity-related behaviors and outcomes. This more complex understanding of the multiple social–spatial contexts that children occupy holds great potential to inform comprehensive and sustainable child obesity prevention efforts.
Acknowledgments
Funding for this study came from the Aetna Foundation. Support for the baseline data collection came from the Patrick and Catherine Weldon Donaghue Medical Research Foundation.
This research was conducted in affiliation with Community Interventions for Health, Oxford Health Alliance, Oxford, England.
We are grateful to our partnership with the New Haven Public Schools and would like to acknowledge district leadership, the students who participated in the study, and the principals, teachers, and school wellness facilitators at each of the 12 Community Interventions for Health study schools. We would also like to thank Rebecca Joyce for help cleaning census data for this study.
Human Participant Protection
This study was reviewed and approved by the Yale University Human Subjects Committee and the New Haven Public School District.
References
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999-2010. JAMA. 2012;307(5):483–490. doi: 10.1001/jama.2012.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA. 2013;309(1):71–82. doi: 10.1001/jama.2012.113905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Singh AS, Mulder C, Twisk JWR, Van Mechelen W, Chinapaw MJM. Tracking of childhood overweight into adulthood: a systematic review of the literature. Obes Rev. 2008;9(5):474–488. doi: 10.1111/j.1467-789X.2008.00475.x. [DOI] [PubMed] [Google Scholar]
- 4.Owen CG, Whincup PH, Orfei L et al. Is body mass index before middle age related to coronary heart disease risk in later life? Evidence from observational studies. Int J Obes (Lond) 2009;33(8):866–877. doi: 10.1038/ijo.2009.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Freedman DS, Mei Z, Srinivasan SR, Berenson GS, Dietz WH. Cardiovascular risk factors and excess adiposity among overweight children and adolescents: the Bogalusa Heart Study. J Pediatr. 2007;150(1):12–17. doi: 10.1016/j.jpeds.2006.08.042. e2. [DOI] [PubMed] [Google Scholar]
- 6.Egger G, Swinburn B. An “ecological” approach to the obesity pandemic. BMJ. 1997;315(7106):477–480. doi: 10.1136/bmj.315.7106.477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.O’Malley PM, Johnston LD, Delva J, Bachman JG, Schulenberg JE. Variation in obesity among American secondary school students by school and school characteristics. Am J Prev Med. 2007;33(4, suppl):S187–S194. doi: 10.1016/j.amepre.2007.07.001. [DOI] [PubMed] [Google Scholar]
- 8.Sallis JF, Glanz K. The role of built environments in physical activity, eating, and obesity in childhood. Future Child. 2006;16(1):89–108. doi: 10.1353/foc.2006.0009. [DOI] [PubMed] [Google Scholar]
- 9.An R, Sturm R. School and residential neighborhood food environment and diet among California youth. Am J Prev Med. 2012;42(2):129–135. doi: 10.1016/j.amepre.2011.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Millstein RA, Strobel J, Kerr J et al. Home, school, and neighborhood environment factors and youth physical activity. Pediatr Exerc Sci. 2011;23(4):487–503. doi: 10.1123/pes.23.4.487. [DOI] [PubMed] [Google Scholar]
- 11.Harrison F, Jones AP, van Sluijs EMF, Cassidy A, Bentham G, Griffin SJ. Environmental correlates of adiposity in 9-10 year old children: considering home and school neighbourhoods and routes to school. Soc Sci Med. 2011;72(9):1411–1419. doi: 10.1016/j.socscimed.2011.02.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.National Institute of Diabetes and Digestive and Kidney Diseases. Overweight and obesity statistics. Available at: http://www.niddk.nih.gov/health-information/health-statistics/Pages/overweight-obesity-statistics.aspx#a. Accessed September 23, 2015.
- 13.Schuster MA, Elliott MN, Kanouse DE et al. Racial and ethnic health disparities among fifth-graders in three cities. N Engl J Med. 2012;367(8):735–745. doi: 10.1056/NEJMsa1114353. [DOI] [PubMed] [Google Scholar]
- 14.Leventhal T, Brooks-Gunn J. The neighborhoods they live in: the effects of neighborhood residence on child and adolescent outcomes. Psychol Bull. 2000;126(2):309–337. doi: 10.1037/0033-2909.126.2.309. [DOI] [PubMed] [Google Scholar]
- 15.Lovasi GS, Hutson MA, Guerra M, Neckerman KM. Built environments and obesity in disadvantaged populations. Epidemiol Rev. 2009;31:7–20. doi: 10.1093/epirev/mxp005. [DOI] [PubMed] [Google Scholar]
- 16.Kimbro RT, Denney JT. Neighborhood context and racial/ethnic differences in young children’s obesity: structural barriers to interventions. Soc Sci Med. 2013;95:97–105. doi: 10.1016/j.socscimed.2012.09.032. [DOI] [PubMed] [Google Scholar]
- 17.Grow HM, Cook AJ, Arterburn DE, Saelens BE, Drewnowski A, Lozano P. Child obesity associated with social disadvantage of children’s neighborhoods. Soc Sci Med. 2010;71(3):584–591. doi: 10.1016/j.socscimed.2010.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Singh GK, Siahpush M, Kogan MD. Neighborhood socioeconomic conditions, built environments, and childhood obesity. Health Aff (Millwood) 2010;29(3):503–512. doi: 10.1377/hlthaff.2009.0730. [DOI] [PubMed] [Google Scholar]
- 19.Burdette HL, Wadden TA, Whitaker RC. Neighborhood safety, collective efficacy, and obesity in women with young children. Obesity (Silver Spring) 2006;14(3):518–525. doi: 10.1038/oby.2006.67. [DOI] [PubMed] [Google Scholar]
- 20.Moore K, Diez Roux AV, Auchincloss A et al. Home and work neighbourhood environments in relation to body mass index: the Multi-Ethnic Study of Atherosclerosis (MESA) J Epidemiol Community Health. 2013;67(10):846–853. doi: 10.1136/jech-2013-202682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Duncan M, Mummery K. Psychosocial and environmental factors associated with physical activity among city dwellers in regional Queensland. Prev Med. 2005;40(4):363–372. doi: 10.1016/j.ypmed.2004.06.017. [DOI] [PubMed] [Google Scholar]
- 22.Kim D, Subramanian SV, Gortmaker SL, Kawachi I. US state- and county-level social capital in relation to obesity and physical inactivity: a multilevel, multivariable analysis. Soc Sci Med. 2006;63(4):1045–1059. doi: 10.1016/j.socscimed.2006.02.017. [DOI] [PubMed] [Google Scholar]
- 23.Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. N Engl J Med. 2007;357(4):370–379. doi: 10.1056/NEJMsa066082. [DOI] [PubMed] [Google Scholar]
- 24.Tamers SL, Okechukwu C, Allen J et al. Are social relationships a healthy influence on obesogenic behaviors among racially/ethnically diverse and socio-economically disadvantaged residents? Prev Med. 2013;56(1):70–74. doi: 10.1016/j.ypmed.2012.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Galvez MP, Pearl M, Yen IH. Childhood obesity and the built environment. Curr Opin Pediatr. 2010;22(2):202–207. doi: 10.1097/MOP.0b013e328336eb6f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jennings A, Welch A, Jones AP et al. Local food outlets, weight status, and dietary intake: associations in children aged 9-10 years. Am J Prev Med. 2011;40(4):405–410. doi: 10.1016/j.amepre.2010.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Saelens BE, Sallis JF, Frank LD et al. Obesogenic neighborhood environments, child and parent obesity: the Neighborhood Impact on Kids study. Am J Prev Med. 2012;42(5):e57–e64. doi: 10.1016/j.amepre.2012.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Carroll-Scott A, Gilstad-Hayden K, Rosenthal L et al. Disentangling neighborhood contextual associations with child body mass index, diet, and physical activity: the role of built, socioeconomic, and social environments. Soc Sci Med. 2013;95:106–114. doi: 10.1016/j.socscimed.2013.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.MacLeod KE, Gee GC, Crawford P, Wang MC. Neighbourhood environment as a predictor of television watching among girls. J Epidemiol Community Health. 2008;62(4):288–292. doi: 10.1136/jech.2007.061424. [DOI] [PubMed] [Google Scholar]
- 30.Voorhees CC, Murray D, Welk G et al. The role of peer social network factors and physical activity in adolescent girls. Am J Health Behav. 2005;29(2):183–190. doi: 10.5993/ajhb.29.2.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Williams AJ, Wyatt KM, Hurst AJ, Williams CA. A systematic review of associations between the primary school built environment and childhood overweight and obesity. Health Place. 2012;18(3):504–514. doi: 10.1016/j.healthplace.2012.02.004. [DOI] [PubMed] [Google Scholar]
- 32.Gilstad-Hayden K, Carroll-Scott A, Rosenthal L, Peters SM, McCaslin C, Ickovics JR. Positive school climate is associated with lower body mass index percentile among urban preadolescents. J Sch Health. 2014;84(8):502–506. doi: 10.1111/josh.12177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Centers for Disease Control and Prevention. School Connectedness: Strategies for Increasing Protective Factors Among Youth. Atlanta, GA: US Department of Health and Human Services; 2009. Available at: http://www.cdc.gov/healthyyouth/protective/pdf/connectedness.pdf. Accessed March 29, 2014. [Google Scholar]
- 34.Sampson RJ, Morenoff JD, Earls F. Beyond social capital: spatial dynamics of collective efficacy for children. Am Sociol Rev. 1999;64(5):633–660. [Google Scholar]
- 35.Svavarsdottir EK. Connectedness, belonging and feelings about school among healthy and chronically ill Icelandic schoolchildren. Scand J Caring Sci. 2008;22(3):463–471. doi: 10.1111/j.1471-6712.2007.00553.x. [DOI] [PubMed] [Google Scholar]
- 36.Langille D, Rasic D, Kisely S, Flowerdew G, Cobbett S. Protective associations of school connectedness with risk of depression in Nova Scotia adolescents. Can J Psychiatry. 2012;57(12):759–764. doi: 10.1177/070674371205701208. [DOI] [PubMed] [Google Scholar]
- 37.Chapman RL, Buckley L, Sheehan MC, Shochet IM, Romaniuk M. The impact of school connectedness on violent behavior, transport risk-taking behavior, and associated injuries in adolescence. J Sch Psychol. 2011;49(4):399–410. doi: 10.1016/j.jsp.2011.04.004. [DOI] [PubMed] [Google Scholar]
- 38.Wilson D. The interface of school climate and school connectedness and relationships with aggression and victimization. J Sch Health. 2004;74(7):293–299. doi: 10.1111/j.1746-1561.2004.tb08286.x. [DOI] [PubMed] [Google Scholar]
- 39.Azagba S, Asbridge M. School connectedness and susceptibility to smoking among adolescents in Canada. Nicotine Tob Res. 2013;15(8):1458–1463. doi: 10.1093/ntr/nts340. [DOI] [PubMed] [Google Scholar]
- 40.Dillon C. 1 in 4 live in poverty in New Haven. Yale Daily News. October 5, 2010. Available at: http://yaledailynews.com/blog/2010/10/05/1-in-4-live-in-poverty-in-new-haven. Accessed February 3, 2015.
- 41.Yousey-Hindes KM, Hadler JL. Neighborhood socioeconomic status and influenza hospitalizations among children: New Haven County, Connecticut, 2003-2010. Am J Public Health. 2011;101(9):1785–1789. doi: 10.2105/AJPH.2011.300224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ickovics JR, Carroll-Scott A, Peters SM, Schwartz M, Gilstad-Hayden K, McCaslin C. Health and academic achievement: cumulative effects of health assets on standardized test scores among urban youth in the United States. J Sch Health. 2014;84(1):40–48. doi: 10.1111/josh.12117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Duffany KO, Finegood DT, Matthews D et al. Community Interventions for Health (CIH): a novel approach to tackling the worldwide epidemic of chronic diseases. CVD Prev Control. 2011;6(2):47–56. [Google Scholar]
- 44.STEPS Manual. Geneva, Switzerland: World Health Organization; 2008. Available at: http://www.who.int/chp/steps/manual/en. Accessed March 1, 2014. [Google Scholar]
- 45. DataHaven. 2012 New Haven neighborhood profiles. 2012. Available at: http://www.ctdatahaven.org/neighborhoodprofiles.php. Accessed February 1, 2014.
- 46.Kuczmarski RJ, Ogden CL, Guo SS et al. 2000 CDC Growth Charts for the United States: methods and development. Vital Health Stat 11. 2002;(246):1–190. [PubMed] [Google Scholar]
- 47.Sastry N, Ghosh-Dastidar B, Adams J, Pebley AR. The design of a multilevel survey of children, families, and communities: the Los Angeles Family and Neighborhood Survey. Soc Sci Res. 2006;35(4):1000–1024. [Google Scholar]
- 48.Elliott DS, Wilson WJ, Huizinga D, Sampson RJ, Elliott A, Rankin B. The effects of neighborhood disadvantage on adolescent development. J Res Crime Delinq. 1996;33(4):389–426. [Google Scholar]
- 49.Pebley AR, Sastry N. Concentrated Poverty vs. Concentrated Affluence: Effects on Neighborhood Social Environments and Children’s Outcomes. Santa Monica, CA: RAND Labor & Population; 2003. [Google Scholar]
- 50.Resnick MD, Bearman PS, Blum RW et al. Protecting adolescents from harm: findings from the National Longitudinal Study on Adolescent Health. JAMA. 1997;278(10):823–832. doi: 10.1001/jama.278.10.823. [DOI] [PubMed] [Google Scholar]
- 51.Harwell M, LeBeau B. Student eligibility for a free lunch as an SES measure in education research. Educ Res. 2010;39(2):120–131. [Google Scholar]
- 52.National Center for Education Statistics. The Nation’s Report Card: Trial Urban District Assessment Mathematics 2011: Executive Summary. Washington, DC: US Department of Education; 2011. Available at: http://nces.ed.gov/nationsreportcard/pubs/dst2011/2012452.asp. Accessed March 31, 2014. [Google Scholar]
- 53.US Department of Agriculture and US Department of Health and Human Services. Dietary Guidelines for Americans, 2010. Washington, DC: US Government Printing Office; 2010. [Google Scholar]
- 54.US Department of Health and Human Services. 2008 Physical Activity Guidelines for Americans. Washington, DC: US Department of Health and Human Services; 2008. [Google Scholar]
- 55.Patrick K, Sallis JF, Long BJ, Calfas KJ, Wooten WJ, Health G. A new tool for encouraging activity: Project PACE. Phys Sportsmed. 1994;22(11):45–55. doi: 10.1080/00913847.1994.11947706. [DOI] [PubMed] [Google Scholar]
- 56.Raudenbush SW, Bryk AS. Hierarchical Linear Models: Applications and Data Analysis. Thousand Oaks, CA: Sage Publications; 2002. [Google Scholar]
- 57.Wang Y, Xue H, Chen HJ, Igusa T. Examining social norm impacts on obesity and eating behaviors among US school children based on agent-based model. BMC Public Health. 2014;14:923. doi: 10.1186/1471-2458-14-923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Dubow EF, Edwards S, Ippolito MF. Life stressors, neighborhood disadvantage, and resources: a focus on inner-city children’s adjustment. J Clin Child Psychol. 1997;26(2):130–144. doi: 10.1207/s15374424jccp2602_2. [DOI] [PubMed] [Google Scholar]
- 59.Quinn K, Kaufman JS, Siddiqi A, Yeatts KB. Parent perceptions of neighborhood stressors are associated with general health and child respiratory health among low-income, urban families. J Asthma. 2010;47(3):281–289. doi: 10.3109/02770901003605324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Haines RJ. Smoking cessation was difficult for adolescents because of daily life stressors and the need for major lifestyle changes. Evid Based Nurs. 2008;11(1):27. doi: 10.1136/ebn.11.1.27. [DOI] [PubMed] [Google Scholar]
- 61.Wang Y, Xue H, Chen H, Igusa T. Examining social norm impacts on obesity and eating behaviors among US school children based on agent-based model. BMC Public Health. 2014;14:923. doi: 10.1186/1471-2458-14-923. [DOI] [PMC free article] [PubMed] [Google Scholar]