Abstract
Aim
Rapid maxillary expansion (RME) splits the midpalatal suture to correct maxillary transverse discrepancies and increase the arch perimeter. The goal of this paper is to evaluate the immediate effects of RME with Hyrax appliances on the dentoalveolar complex using cone beam computed tomography (CBCT).
Methods
Twenty-eight patients (19 females and 9 males) requiring maxillary expansion therapy were included (mean age, 14.1 years; range, 13 to 20 years). CBCT images were taken at T1 (before maxillary expansion) and T2 (immediately after expansion) as part of clinical records. Maxillary arch width, posterior segment angulation, and buccal bone thickness at the level of the first premolar and first molar were evaluated. Paired t tests determined statistical significance (P < .05).
Results
The mean ± SD amount of expansion achieved was 4.7788 ± 2.8474 mm for the maxillary premolars and 4.6943 ± 3.2198 mm for the molars. Significant tipping of the palatal roots of the maxillary right and left premolars as well as that for the maxillary left molar was observed. When present, the thickness of the buccal plate decreased on all observed roots.
Conclusion
There is a significant increase in interpremolar and intermolar distance with RME. The increase in root angulation suggests that the movement is more tipping than translation. The thickness of the buccal plate decreases immediately after RME. Therefore, the level of inflammation should be closely monitored to avoid periodontal destruction. There is a need to define standardized reference planes and comparable methodology to achieve compatible results among studies.
Keywords: CBCT, dentoalveolar, maxillary expansion
Rapid maxillary expansion (RME) is used in orthodontics to correct transverse and arch length discrepancies of the maxillary arch.1,2 The most predictable results are typically achieved in the late mixed or early permanent dentitions, when patients are in their prepubertal peak, before the
 complete fusion of the midpalatal suture.3 Ideally, RME would result in a maximal amount of skeletal expansion compared to dental tipping. However, when RME appliances are anchored to the teeth, the dental effects supersede the skeletal changes.4 These effects include the appearance of a midline diastema; an increase in the intermolar width, usually followed by mandibular molar uprighting; buccal tipping; and extrusion of the maxillary molars.2,4–7 The dental effects of RME have traditionally been evaluated on plaster casts and on frontal and lateral cephalograms.8,9 To overcome the errors related to the two-dimensional (2D) representation of 3D structures, new studies use CBCT technology to evaluate expansion effects.10–12 CBCT allows a 3D reconstruction of the teeth and jaw with a significantly reduced radiation dosage and scanning time compared to conventional computed tomography (CT).13 CBCT has been reported to render a 1:1 ratio result,14 and given the adequate settings and software, it is capable of measuring alveolar bone height to an accuracy of approximately 0.6 mm.15 The aim of this study was to evaluate the immediate effects of RME on maxillary arch width, posterior segment angulation, and buccal bone thickness using CBCTs.
complete fusion of the midpalatal suture.3 Ideally, RME would result in a maximal amount of skeletal expansion compared to dental tipping. However, when RME appliances are anchored to the teeth, the dental effects supersede the skeletal changes.4 These effects include the appearance of a midline diastema; an increase in the intermolar width, usually followed by mandibular molar uprighting; buccal tipping; and extrusion of the maxillary molars.2,4–7 The dental effects of RME have traditionally been evaluated on plaster casts and on frontal and lateral cephalograms.8,9 To overcome the errors related to the two-dimensional (2D) representation of 3D structures, new studies use CBCT technology to evaluate expansion effects.10–12 CBCT allows a 3D reconstruction of the teeth and jaw with a significantly reduced radiation dosage and scanning time compared to conventional computed tomography (CT).13 CBCT has been reported to render a 1:1 ratio result,14 and given the adequate settings and software, it is capable of measuring alveolar bone height to an accuracy of approximately 0.6 mm.15 The aim of this study was to evaluate the immediate effects of RME on maxillary arch width, posterior segment angulation, and buccal bone thickness using CBCTs.
METHODS
Twenty-eight patients (19 females and 9 males) requiring maxillary expansion therapy as part of their comprehensive orthodontic treatment were included in this study. All treatment was started after July 2007 at the University of Texas Health Science Center Houston Dental Branch. The study protocol was approved by the Institutional Review Board of University of Texas Health Science Center, Houston, Texas. The mean age of patients was 14.1 years (range, 13 to 20 years). Inclusion criteria were a need for RME as determined by an experienced orthodontist, a need for fixed orthodontic treatment, aged between 10 and 20 years, adequate CBCT records, and signed informed consent.
Exclusion criteria were craniofacial anomalies, undergoing surgically assisted RME, having orthodontic appliances prior to the start of maxillary expansion, and noncompliant patients.
Each patient had CBCT images taken prior to orthodontic treatment (T1) and after the completion of maxillary expansion activation (T2) using Hyrax appliances. Patients were instructed to turn the screw once a day until an adequate amount of clinical expansion had been reached.
Imaging device
Cone beam images were acquired using the Sirona Galileos System (Sirona Dental Systems). This machine features a 14-second cycle in 220 degrees, which results in 200 individual exposures. Volume dimensions of 15 × 15 × 15 cm3 capture an image at a high level of detail. The voxel size is 0.15 to 0.30 mm, and the grayscale is 12 bit. Image reconstruction time is approximately 4.5 minutes. The technology also allows for small-region close-up views at double the detail without an additional scan.
Image manipulation
The images were evaluated using the Sidexis software (Sirona). With this software, it is possible to view the different cuts at increasing magnifications for better accuracy. To evaluate the immediate dental and alveolar changes following RME, linear (mm) and angular measurements (degrees) were taken at T1 and T2.
Dental effects
Two-dimensional coronal images were created perpendicular to the midsagittal plane to measure the amount of dental expansion at the level of the maxillary first molars and premolars (Fig 1).
Intermolar distance: measured between the mesiolingual cusp tip of the maxillary left first molar and the mesiolingual cusp tip of the maxillary right first molar.
Interpremolar distance: measured from the lingual cusp tip of the maxillary left first premolar to the lingual cusp tip of the maxillary right first premolar.
Molar angulation: measure of the angle created between a line parallel to the palatal root of each of the maxillary first molars and the mandibular occlusal plane.
Premolar angulation: measure of the angle created between a line parallel to the palatal root of each of the maxillary first premolar and the mandibular occlusal plane.
Fig 1.

Example of the measurements on a T1 slice. Blue line, assessement of buccal plate thickness; yellow lines, intermolar distance; pink angle, molar angulation relative to the mandibular occlusal plane.
Alveolar effects
The alveolar effects of expansion were evaluated based on the following criteria.
Presence or absence of buccal bone: Similar 2D coronal sections were used to determine the presence or absence of buccal bone at T1 and T2 on the root surfaces of the mesiobuccal root of the maxillary left and right first molars, the distobuccal root of the maxillary left and right first molars, and the buccal root of the maxillary left and right first premolars. The cuts were taken at the junction between the cervical and middle root thirds from the center of the root canal to the outer surface of the buccal plate. The presence of buccal bone was graded 0, and the absence of buccal bone was graded 1.
Buccal plate thickness: This was measured at T1 and T2 at the junction between the cervical and middle root thirds from the center of the root canal to the outer surface of the buccal plate at the following locations: mesiobuccal root of the maxillary left and right first molars, the distobuccal root of the maxillary left and right first molars, and the buccal root of the maxillary left and right first premolars. Bone thickness was determined by subtracting the T2 from the T1 measurement.
Statistical analysis
T1 and T2 data were imported to the SAS/STAT (SAS) software for statistical analysis. Means and standard deviations were calculated for each parameter. Paired t tests were performed to determine statistical significance. P < .05 was used for all statistical analyses.
To test intraexaminer reliability, 10 patient records at T1 and T2 were randomly selected and all measurements repeated. Intraclass correlation coefficients (ICCs) were calculated.
RESULTS
All 28 patients were included in the molar measurements. However, four patients were excluded from the premolar measurements because of premolar extractions (two patients), lack of eruption (one patient), and scatter at the premolar region on the T2 CBCT (one patient). Therefore, 24 patients had premolar measurements taken. Table 1 presents the premolar measurements at T1 and T2. Table 2 presents the molar measurements at T1 and T2. The statistical comparisons between T1 and T2 are reported in Table 3 for the premolars and Table 4 for the molars. ICC was greater than 0.9 with a mean 95% confidence interval (CI) of 1.00.
Table 1.
Mean ± SD premolar measurements at T1 and T2
| Measurement | Site | n | Mean ± SD |
|---|---|---|---|
| Buccal plate measurement | UR4-T1 | 24 | 3.2725 ± 0.5859 |
| UR4-T2 | 24 | 2.9196 ± 0.6519 | |
| UL4-T1 | 24 | 3.3716 ± 0.7307 | |
| UL4-T2 | 24 | 2.9350 ± 0.6826 | |
| Interpremolar distance | U4-T1 | 24 | 27.6592 ± 3.3799 |
| U4-T2 | 24 | 32.4379 ± 2.8890 | |
| Root angulation | UR4_ang-T1 | 24 | 83.1916 ± 9.5498 |
| UR4_ang-T2 | 24 | 77.4541 ± 8.7466 | |
| UL4_ang-T1 | 24 | 89.9875 ± 11.0456 | |
| UL4_ang-T2 | 24 | 82.3500 ± 9.3493 |
SD, standard deviation; UR4, maxillary right first premolar; UL4, maxillary left first premolar; T1, before expansion; T2, postexpansion; U4, interpremolar measurement; ang, palatal angular measurement.
Table 2.
Mean ± SD molar measurements at T1 and T2
| Site | n | Mean ± SD | |
|---|---|---|---|
| Buccal plate measurement | MB_UR6-T1 | 28 | 4.5232 ± 0.6954 |
| MB_UR6-T2 | 28 | 3.8050 ± 0.9247 | |
| DB_UR6-T1 | 28 | 4.2979 ± 0.8568 | |
| DB_UR6-T2 | 28 | 3.5300 ± 0.8953 | |
| MB_UL6-T1 | 28 | 4.6761 ± 0.9101 | |
| MB_UL6-T2 | 28 | 3.8364 ± 0.8549 | |
| DB_UL6-T1 | 28 | 4.6193 ± 0.8866 | |
| DB_UL6-T2 | 28 | 3.8896 ± 1.0889 | |
| Intermolar distance | U6-T1 | 28 | 37.2136 ± 4.1284 |
| U6-T2 | 28 | 41.9079 ± 1.9799 | |
| Root angulation | UR6_ang-T1 | 28 | 67.0643 ± 4.6343 |
| UR6_ang-T2 | 28 | 68.2321 ± 5.1505 | |
| UL6_ang-T1 | 28 | 70.1679 ± 68.2429 | |
| UL6_ang-T2 | 28 | 5.3753 ± 3.5161 |
SD, standard deviation; UR6, maxillary right first molar; UL6, maxillary left first molar; T1, before expansion; T2, postexpansion; MB, mesiobuccal root; DB, distobuccal root; U6, intermolar measurement; ang, palatal angular measurement.
Table 3.
Premolar differences between T1 and T2
| Paired differences |
||||||
|---|---|---|---|---|---|---|
| 95% CI |
||||||
| Mean | SD | Lower | Upper | P value | ||
| Buccal plate thickness | UR4-T1–UR4-T2 | 0.3529 | 0.3807 | 0.2006 | 0.5052 | * |
| UL4-T1–UL4-T2 | 0.4367 | 0.4885 | 0.2413 | 0.6321 | * | |
| Expansion | U4-T1–U4-T2 | 4.7788 | 2.8474 | 3.6396 | 5.918 | * |
| Root angulation | UR4_ang-T1–UR4_ang-T2 | 5.7375 | 7.6307 | 2.6847 | 8.7903 | * |
| UL4_ang-T1–UL4_ang-T2 | 7.6375 | 8.4893 | 4.2412 | 11.0338 | * | |
significant; SD, standard deviation; CI, confidence interval; UR4, maxillary right first premolar; UL4, maxillary left first premolar; T1, before expansion; T2, postexpansion; U4, interpremolar measurement; ang, palatal angular measurement.
Table 4.
Molar differences between T1 and T2
| Paired differences |
||||||
|---|---|---|---|---|---|---|
| 95% CI |
||||||
| Mean | SD | Lower | Upper | P value | ||
| Buccal plate thickness | MB_UR6-T1–MB_UR6-T2 | 0.7182 | 0.8055 | 0.4199 | 1.0165 | * |
| DB_UR6-T1–DB_UR6-T2 | 0.7679 | 0.5993 | 0.5460 | 0.9898 | * | |
| MB_UL6-T1–MB_UL6-T2 | 0.8396 | 0.5043 | 0.6528 | 1.0264 | * | |
| DB_UL6-T1–DB_UL6-T2 | 0.7296 | 0.5753 | 0.5166 | 0.9426 | * | |
| Expansion | U6-T1–U6-T2 | 4.6943 | 3.2198 | 3.5017 | 5.8869 | * |
| Root angulation | UR6-T1–UR6-T2 | 1.1679 | 4.9314 | −0.6587 | 2.9945 | NS |
| UL6-T1–UL6-T2 | −1.9250 | 4.5942 | −3.6267 | −0.2233 | * | |
significant; NS, not significant; SD, standard deviation; CI, confidence interval; UR6, maxillary right first molar; UL6, maxillary left first molar; T1, before expansion; T2, postexpansion; U6, interpremolar measurement; ang, palatal angular measurement.
Dental effects
The mean amount of expansion achieved was 4.7788 ± 2.8474 mm for the maxillary premolars and 4.6943 ± 3.2198 mm for the molars. Tipping of the palatal roots of the maxillary right and left premolars as well as that for the maxillary left molar increased significantly (P < .05). The angulation of the maxillary right molar root did not change significantly.
Alveolar effects
The absence of the buccal plate at the premolar and molar levels is reported in Table 5. The number of patients where the bone was not observed increased after RME. Five patients did not have an observable buccal plate on both mesio- and distobuccal roots on the maxillary right molar and presented a similar situation on the left molar (Fig 2). Six patients did not have bone on either premolar buccal root after expansion. When present, the thickness of the buccal plate decreased on all observed roots, as reported in Tables 3 and 4 (P < .05).
Table 5.
Summary of the number of teeth/patients with no visible buccal alveolar bone at T1 and T2
| n = 24 |
n = 28 |
|||||
|---|---|---|---|---|---|---|
| UR4 | UL4 | MB_UR6 | DB_UR6 | MB_UL6 | DB_UL6 | |
| T1 | 2 | 2 | 0 | 0 | 2 | 0 |
| T2 | 10 | 11 | 7 | 8 | 9 | 6 |
| T2 loss on both roots | 7 | 5 | 6 | |||
The bottom row represents the number of patients where the buccal bone was not detected on both premolars at T2 or on both roots of each molar at T2. T1, before expansion; T2, postexpansion; UR4, maxillary right first premolar; UL4, maxillary left first premolar; UR6, maxillary right first molar; UL6, maxillary left first molar; MB, mesiobuccal root; DB, distobuccal root.
Fig 2.
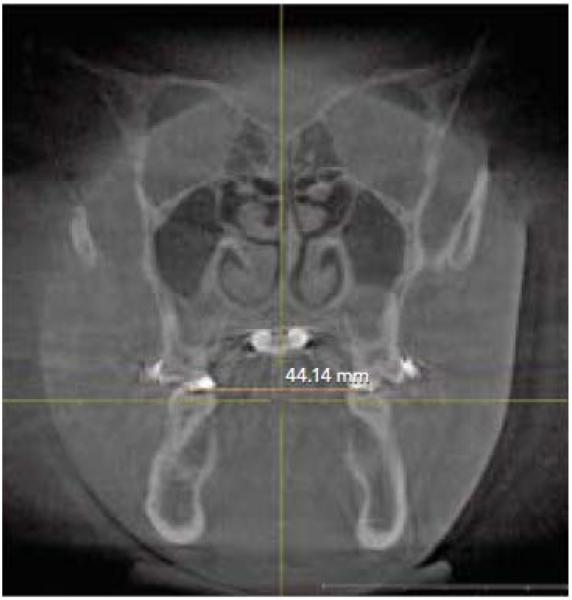
Example of a T2 slice. The intermolar distance is shown. Note the inability to observe the buccal plate in the postexpansion CBCT image.
DISCUSSION
The present study aimed to evaluate the immediate effects of RME on maxillary arch width, posterior segment angulation, and buccal bone thickness using CBCT.
Dental effects
There was a significant increase in the intermolar and interpremolar widths between T1 and T2. These results are similar to those published in two recent studies.
Lagravére et al12 measured the width change between the pulp chamber centers of first molars and premolars at T1 and T2. When using a tooth-anchored maxillary expansion device, they found a mean expansion increase of 5.51 ± 1.79 mm at the molar level and 3.99 ± 1.92 mm at the premolar level. The second study by Ballanti et al16 used a butterfly type of expander that was anchored only on the first molars. The distance between the palatal cusp tips of the first permanent molars was measured immediately before and 6 months after expansion. They found a mean expansion of 6.1 mm (P < .001). Even though both studies used tooth-anchored expansion devices, each found a statistically significant increase in intermolar width. The difference in measurements can be explained by the diverse methodologies of each study.
The molar inclination was also measured in the present paper by measuring the angle formed between a line parallel to the palatal root of each of the maxillary first molars and first premolars and the mandibular occlusal plane. This plane was selected because it is not immediately affected by the maxillary expansion. The rationale is that since the mandibular plane is constant, a change in angulation of the molar/premolar palatal root would indicate tipping, whereas no change would indicate translation. This approach eliminates the need to measure the interapex distance to assess the type of tooth movement. Our results showed a significant tipping of the palatal roots of the maxillary right and left premolars as well as that of the maxillary left molar. These results are less important than those observed by Christie et al.11 In their study, a bonded palatal expander was used. The angle between the lateral limits of the nasal cavity and the line that joins the apices of the first molar palatal root to the tip of the mesiobuccal cusps, as seen on a frontal cut, was measured to evaluate molar tipping. Their results indicate a difference in angulation of 6.22 ± 2.5 degrees for the right molars and 5.6 ± 2.6 degrees for the left molars. Another study12 assessed tipping at the apex level by measuring the angles formed between the line that joins the center of the pulp chambers and the mesiobuccal apices of the right and left molars and the tips on the mesial pulp horns and the buccal apices of the right and left premolars. When a tooth-borne expansion appliance was utilized, the amount of tipping achieved immediately after expansion was greater at the molar than at the premolar level, which is the opposite of our results. In both cases, the numbers are not comparable because of a different reference plane. Furthermore, the fact that the angulation of the maxillary right molar root did not change significantly in our study might point toward the need for a nondental reference plane that would allow better visualization of the changes. Therefore, a standardized methodology should be applied to be able to monitor the changes that occur after a specific orthodontic mechanotherapy.
Periodontal changes in the present study were evaluated at baseline by assessing the presence or absence of buccal alveolar bone and by measuring the thickness of the buccal plate at the first premolar and molar levels. Our results indicate a decrease in buccal bone thickness at the premolar and molar levels, with a more predominant thinning at the premolar level. This result is consistant with previous findings.12,16 Garib et al17 used axial sections parallel to the palatal plane at the level of the furcation of the right maxillary first molar to evaluate the thickness of the buccal bone after expansion with a Hyrax appliance. Their results corroborate ours in that buccal resorption appeared on the appliance supporting teeth, with the first premolars presenting the largest resorption. The number of teeth with no visible bone at T2 increased. This conclusion can be anticipated since the RME pushes the anchor teeth buccally. Moreover, it corresponds to previously published results and indicates that the thicker the initial buccal bone is, the less risk of fenestration/dehiscence exists.
CONCLUSION
Within the limitations of this study, the following conclusions can be made on the immediate effects of RME:
There is a significant tipping of the crowns with RME.
There is a significant increase of root angulation on the first premolars and the left first molar relative to the mandibular occlusal plane, suggesting that the movement is more tipping than translation.
The thickness of the buccal plate decreases immediately after RME. Therefore, the level of inflammation should be closely monitored to avoid periodontal destruction.
There is a need to define standardized reference planes and comparable methodology to achieve compatible results among studies.
REFERENCES
- 1.Bishara SE, Staley RN. Maxillary expansion: Clinical implications. Am J Orthod Dentofacial Orthop. 1987;91:3–14. doi: 10.1016/0889-5406(87)90202-2. [DOI] [PubMed] [Google Scholar]
- 2.Haas A. Rapid expansion of the maxillary dental arch and cavity by opening the midpalatal suture. Angle Orthod. 1961;31:73–90. [Google Scholar]
- 3.Baccetti T, Franchi L, Cameron CG, McNamara JA., Jr Treatment timing for rapid maxillary expansion. Angle Orthod. 2001;71:343–350. doi: 10.1043/0003-3219(2001)071<0343:TTFRME>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 4.Haas AJ. The treatment of maxillary deficiency by opening the midpalatal suture. Angle Orthod. 1965;35:200–217. doi: 10.1043/0003-3219(1965)035<0200:TTOMDB>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 5.Davis WM, Kronman JH. Anatomical changes induced by splitting of the midpalatal suture. Angle Orthod. 1969;39:126–132. doi: 10.1043/0003-3219(1969)039<0126:ACIBSO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 6.Garib DG, Henriques JF, Janson G, Freitas MR, Coelho RA. Rapid maxillary expansion—Tooth tissue-borne versus tooth-borne expanders: A computed tomography evaluation of dentoskeletal effects. Angle Orthod. 2005;75:548–557. doi: 10.1043/0003-3219(2005)75[548:RMETVT]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 7.Lagravère MO, Heo G, Major PW, Flores-Mir C. Meta-analysis of immediate changes with rapid maxillary expansion treatment. J Am Dent Assoc. 2006;137:44–53. doi: 10.14219/jada.archive.2006.0020. [DOI] [PubMed] [Google Scholar]
- 8.Major PW, Johnson DE, Hesse KL, Glover KE. Landmark identification error in posterior anterior cephalometrics. Angle Orthod. 1994;64:447–454. doi: 10.1043/0003-3219(1994)064<0447:LIEIPA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 9.Lagravère MO, Major PW, Flores-Mir C. Long-term dental arch changes after rapid maxillary expansion treatment: A systematic review. Angle Orthod. 2005;75:155–161. doi: 10.1043/0003-3219(2005)075<0151:LDACAR>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 10.Rungcharassaeng K, Caruso JM, Kan JYK, Kim J, Taylor G. Factors affecting buccal bone changes of maxillary posterior teeth after rapid maxillary expansion. Am J Orthod Dentofacial Orthop. 2007;132:428, e1–e8. doi: 10.1016/j.ajodo.2007.02.052. [DOI] [PubMed] [Google Scholar]
- 11.Christie KF, Boucher N, Chung CH. Effects of bonded rapid palatal expansion on the transverse dimensions of the maxilla: A cone-beam computed tomography study. Am J Orthod Dentofacial Orthop. 2010;137(suppl):S79–85. doi: 10.1016/j.ajodo.2008.11.024. [DOI] [PubMed] [Google Scholar]
- 12.Lagravère MO, Carey J, Heo G, Toogood RW, Major PW. Transverse, vertical, and anteroposterior changes from bone-anchored maxillary expansion vs traditional rapid maxillary expansion: A randomized clinical trial. Am J Orthod Dentofacial Orthop. 2010;137:304, e1–e12. doi: 10.1016/j.ajodo.2009.09.016. [DOI] [PubMed] [Google Scholar]
- 13.Kau CH, Richmond S, Palomo JM, Hans MG. Three-dimensional cone beam computerized tomography in orthodontics. J Orthod. 2005;32:282–293. doi: 10.1179/146531205225021285. [DOI] [PubMed] [Google Scholar]
- 14.Lagravère MO, Carey J, Toogood RW, Major PW. Three-dimensional accuracy of measurements made with software on cone-beam computed tomography images. Am J Orthod Dentofacial Orthop. 2008;134:112–116. doi: 10.1016/j.ajodo.2006.08.024. [DOI] [PubMed] [Google Scholar]
- 15.Leung C, Palomo L, Griffith R, Hans MG. Accuracy and reliability of cone-beam computed tomography for measuring alveolar bone height and detecting bony dehiscences and fenestrations. Am J Orthod Dentofacial Orthop. 2010;137(suppl):S109–119. doi: 10.1016/j.ajodo.2009.07.013. [DOI] [PubMed] [Google Scholar]
- 16.Ballanti F, Lione R, Fanucci E, Franchi L, Baccetti T, Cozza P. Immediate and postretention effects of rapid maxillary expansion investigated by computed tomography in growing patients. Angle Orthod. 2009;79:24–29. doi: 10.2319/012008-35.1. [DOI] [PubMed] [Google Scholar]
- 17.Garib DG, Henriques JF, Janson G, de Freitas MR, Fernandes AY. Periodontal effects of rapid maxillary expansion with tooth-tissue-borne and tooth-borne expanders: A computed tomography evaluation. Am J Orthod Dentofacial Orthop. 2006;129:749–758. doi: 10.1016/j.ajodo.2006.02.021. [DOI] [PubMed] [Google Scholar]


