Abstract
Background
Many U.S. adults have multiple behavioral risk factors, and effective, scalable interventions are needed to promote population-level health. In the health care setting, interventions are often provided in print, although accessible to nearly everyone, are brief (e.g., pamphlets), are not interactive, and can require some logistics around distribution. Web-based interventions offer more interactivity but may not be accessible to all. Healthy Directions 2 was a primary care–based cluster randomized controlled trial designed to improve five behavioral cancer risk factors among a diverse sample of adults (n = 2,440) in metropolitan Boston. Intervention materials were available via print or the web.
Purpose
To (a) describe the Healthy Directions 2 study design and (b) identify baseline factors associated with whether participants opted for print or web-based materials.
Methods
Hierarchical regression models corrected for clustering by physician were built to examine factors associated with choice of intervention modality.
Results
At baseline, just 4.0% of participants met all behavioral recommendations. Nearly equivalent numbers of intervention participants opted for print and web-based materials (44.6% vs. 55.4%). Participants choosing web-based materials were younger, and reported having a better financial status, better perceived health, greater computer comfort, and more frequent Internet use (p < .05) than those opting for print. In addition, Whites were more likely to pick web-based material than Black participants.
Conclusions
Interventions addressing multiple behaviors are needed in the primary care setting, but they should be available in web and print formats as nearly equal number of participants chose each option, and there are significant differences in the population groups using each modality.
Keywords: computer-based health education, health promotion, multiple risk behaviors, multiple risk factor interventions, print intervention
Leading causes of morbidity and mortality among adults living in the United States adults are influenced by multiple behavioral risk factors, such as physical inactivity, unhealthful diet, and smoking, which often occur together (Berrigan, Dodd, Troiano, Krebs-Smith, & Barbash, 2003; Fine, Philogene, Gramling, Coups, & Sinha, 2004; Reeves & Rafferty, 2005). As a result, there is increasing emphasis on addressing multiple behavioral risk factors. There has recently been work to develop effective multiple behavioral risk interventions, although largely conducted in or through workplaces (Emmons, 1997; Emmons et al., 2003; Emmons, Linnan, Shadel, Marcus, & Abrams, 1999; Harley et al., 2010; Prochaska et al., 2008; Sorensen, Emmons, et al., 2003; Sorensen, Stoddard, et al., 2003; Sorensen et al., 2010) or with specific chronic disease populations (Eakin et al., 2007; Toobert et al., 2007; Toobert et al., 2011; Toobert, Strycker, Barrera, & Glasgow, 2010). However, the health care setting provides an important venue to intervene on multiple risk behaviors at the population level, and feasible strategies are needed to help providers address all of a patient’s risk behaviors simultaneously (Hyman, Pavlik, Taylor, Goodrick, & Moye, 2007; Orleans, 2004; Pronk, Peek, & Goldstein, 2004). Although some studies have been undertaken in Australia (Parekh, Vandelanotte, King, & Boyle, 2012a, 2012b), there is a need to understand the extent to which patients in the United States present to the primary care setting with multiple risk behaviors.
Furthermore, it is important to develop interventions for multiple risk behaviors that are scalable and sustainable in the primary care setting. The Patient Protection and Affordable Care Act calls for engaging patients in their health care (Honoré et al., 2011; Koh & Sebelius, 2010) and behavior change interventions must be well used if they are to lead to population-level health improvement. That means that developed interventions and intervention strategies need to be responsive to the needs of recipients. Yet, in the health care setting, interventions are often developed for the least interactive strategy (e.g., print) that is available to everyone, although it is likely that intervention recipients will include individuals with computer and Internet access as well as those without access. Print interventions are often brief (e.g., pamphlets), not interactive, and require planning around the logistics of distribution. Web-based interventions offer more interactivity but may not be accessible to all patients. Designing and implementing interventions that allow individuals to use their preferred or best resources available to them, and not be limited by what is available to the entire population, may promote greater intervention engagement and ultimately greater population change. Research is needed to determine what factors are associated with preferred intervention modality (web vs. print) as this may maximize participants’ engagement with the intervention as well as intervention reach.
Healthy Directions 1 (HD1) was a multiple risk behavior change intervention implemented in a primary care setting that was developed for adults living in low-income, multiethnic neighborhoods. HD1 led to significant improvement across multiple cancer risk behaviors (Emmons et al., 2003; Emmons, Stoddard, et al., 2005; Sorensen et al., 2005), but the intervention included an in-person counseling session plus four follow-up telephone sessions, which are difficult to sustain in the primary care setting. Healthy Directions 2 (HD2) evaluates an adaptation of HD1 designed to promote health at the population level by maximizing reach, while maintaining intervention effectiveness. HD2 was developed in two modalities, web or print, and participants selected their preferred intervention modality when enrolling in the study. The purpose of this article is to describe the HD2 study design and to use cross-sectional analyses to examine factors associated with participants’ choice of intervention modality.
Method
Study Design
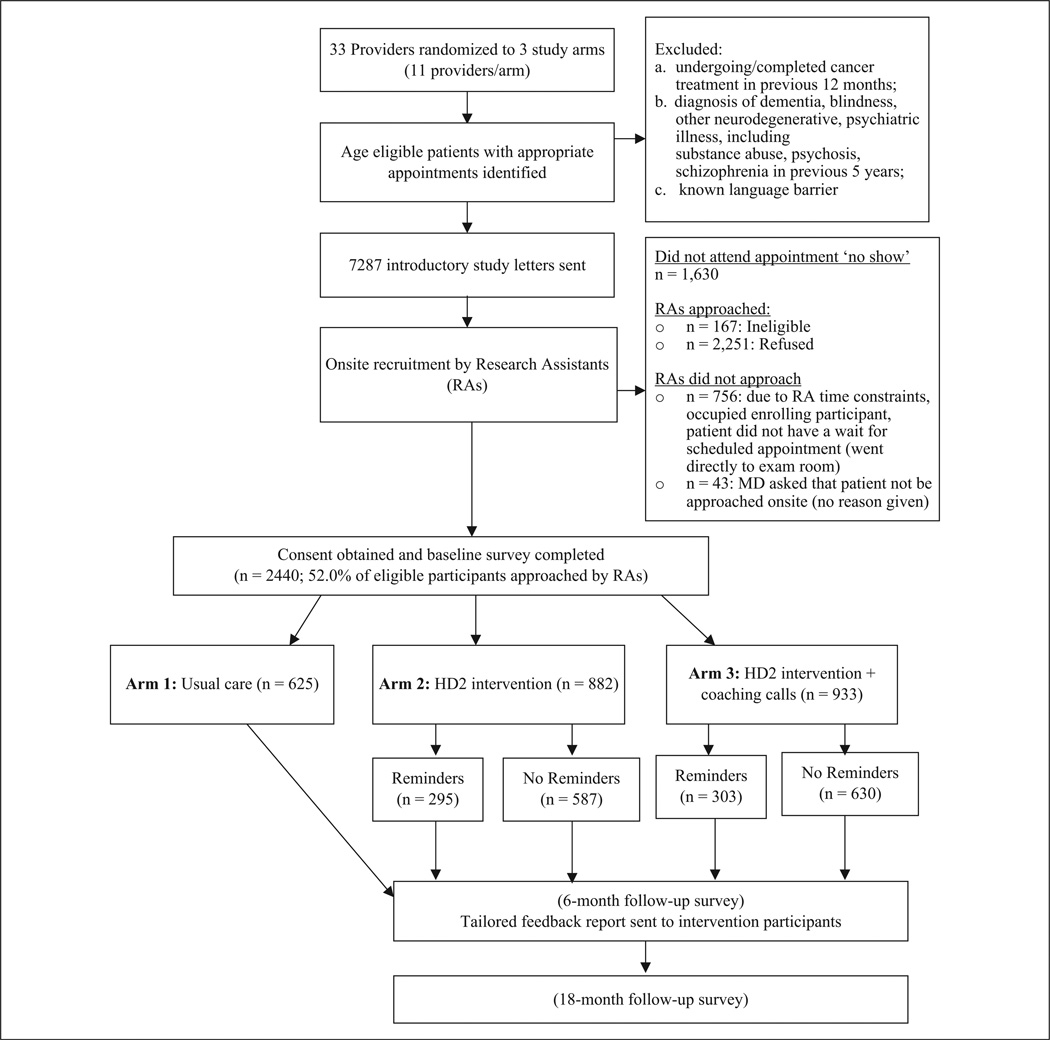
HD2 is a cluster randomized control trial conducted in two health centers in metropolitan Boston of a community-based managed care practice organization. Randomization occurred at the primary care provider level with providers (n = 33) being randomized to (a) usual care, (b) HD2 intervention delivered in web or print format, or (c) HD2 intervention materials plus two coaching calls (see Figure 1). HD2 addressed multiple behaviors simultaneously (physical activity, fruit and vegetable intake, red meat consumption, multivitamin use, smoking). All participating providers, regardless of randomization, were given a brief training on study protocols and messages.
Figure 1.
Health Directions 2 (HD2) study design.
Study Participants and Recruitment
Eligibility requirements included (a) being aged 18+; (b) being able to read English; (c) not having a diagnosis of dementia, blindness, neurodegenerative, or psychiatric illness (previous 5 years); and (d) not undergoing cancer treatment (previous 12 months).
HD2 research staff sent potentially eligible patients a study introduction letter with “opt out” information. When checking in for a well visit or chronic disease management appointment, clinic reception staff provided patients with study-related information. HD2 staff then approached patients and confirmed eligibility and interest, obtained informed consent, and distributed the self-administered baseline survey. To assist in behavior change efforts, participants in the two intervention arms received a pedometer to track steps and a bottle of multivitamins. About half (52%, n = 2,440) of the patients approached consented to enrolled in the study; enrollees received a $5 gift card. The study was approved by the Institutional Review Board at Harvard Pilgrim Healthcare.
Intervention Conditions
Usual care
Usual care participants received the current standard of care offered by their providers, and publicly available pamphlets from health agencies (e.g., American Cancer Society), addressing the targeted behaviors.
HD2 intervention
The intervention was guided by the social contextual framework (Sorensen, Emmons, et al., 2003), and focused on influences at multiple levels (individual, interpersonal, and community; McLeroy, Bibeau, Steckler, & Glanz, 1988). Intervention components were selected for their ability to motivate and maintain behavior change, and for potential sustainability, and included (a) provider endorsement, (b) intervention materials (web or print), (c) two tailored feedback reports, (d) materials for one’s social network, and (e) links to key community-based resources.
Providers verbally endorsed study participation and intervention targets using a brief script (<30 seconds) at the appointment when the participant enrolled in the study. Immediately on enrolling in the study, participants selected their preferred modality for the intervention materials. The content of the web and print intervention materials were similar, and emphasized changing multiple behaviors simultaneously. Participants were encouraged to work on changing all needed behaviors, and measurable behavioral goals for the targeted behaviors were provided: take a multivitamin daily, walk 10,000 steps/day, eat 5+ servings of fruits and vegetable/day, eat ≤3 servings of red meat/week, and quit smoking.
Intervention participants received two tailored feedback reports (after enrollment and the 6-month survey). All reports were tailored, which is associated with greater behavior change (Broekhuizen, Kroeze, van Poppel, Oenema, & Brug, 2012; Krebs, Prochaska, & Rossi, 2010; Noar, Benac, & Harris, 2007). Reports were signed electronically by participant’s provider, and used survey data to provide feedback on the targeted health behaviors by comparing participants’ behaviors with current behavioral recommendations. The second report also reported and provided feedback on the participants’ changes in behavior from baseline to 6-month follow-up.
As interpersonal and community-level factors support behavior change (McLeroy et al., 1988), participants received a print booklet that included the web address for the HD2 social support website for family and members of their social network, and a community resource guide. The social network materials provided information about supporting the participant’s behavior change efforts, whereas the community resource guide provided information about community resources to facilitate physical activity, healthful eating, and smoking cessation.
HD2 intervention plus coaching
Participants in this arm received all of the previously described intervention components plus two coaching calls from graduate-level health coaches trained in motivational interviewing (Miller & Rollnick, 2002). Calls took place shortly after enrollment and again 4 weeks later. The brief calls, designed to last between 5 and 10 minutes, were meant to increase use of and engagement with the intervention.
The HD2 study design makes it possible to determine the comparative effectiveness of the self-guided intervention versus the coached intervention on reducing multiple risk factors simultaneously compared with usual care. This study was not designed to examine the intervention components separately, but rather its impact as a whole.
Data Collection
Participants completed a brief (~5 minutes), self-administered baseline survey that provided data for intervention tailoring. Follow-up survey data were collected at 6 months and 18 months post-baseline. This article examines baseline data only (collected in 2009).
Measures
Outcome measure
The outcome measure for this article is participants’ selected intervention modality (web or print), among participants in the two intervention arms.
Sociodemographic characteristics
We assessed race/ethnicity, education, marital/partner status, and participants’ perceived financial status of their household (range: comfortable with some extra to cannot make ends meet). Age, sex, and primary care provider were obtained from the electronic medical record.
Health status
We assessed self-perceived health status using the one-item assessment from the Medical Outcomes Study Short-Form (Ware & Sherbourne, 1992). We used self-reported height and weight to calculate body mass index (BMI; kg/m2) and weight status.
Health behaviors
Physical activity was assessed using four questions from Centers for Disease Control and Prevention’s (CDC, n.d.) Behavioral Risk Factor Surveillance Survey that assessed moderate (brisk walking, biking, or anything that causes small increases in breathing or heart rate) and vigorous activity (running, aerobics, or anything else that causes large increases in breathing or heart rate; Estabrooks, Bradshaw, Dzewaltowski, & Smith-Ray, 2008; Macera et al., 2001). We summed reported minutes of moderate and vigorous physical activity into a total number of weekly minutes, and then dichotomized the variable as to whether a person met the current recommendation of 150+ minutes of moderate activity or 60+ minutes of vigorous activity or the equivalent per week (U.S. Department of Health and Human Services, 2008).
Fruit and vegetable intake was assessed using the “5 A Day for Better Health” tool, a seven-item instrument covering different types of fruit and vegetable items with predetermined frequencies of intake (Serdula et al., 1993). We calculated total daily servings of fruits and vegetables (excluding fried potatoes and French fries), with 5+ servings/ day being the daily recommended intake (U.S. Department of Agriculture, U.S. Department of Health and Human Services, 2005).
Red meat intake was assessed with an abbreviated form of a semiquantitative Food Frequency Questionnaire (Willett et al., 1985). Responses were recoded to equivalent servings per week and summed to obtain total servings per week. Results were then dichotomized, with <3 serving/week being the recommendation (U.S. Department of Agriculture, U.S. Department of Health and Human Services, 2005).
Multivitamin intake was assessed by asking respondents how many days per week, on average, they took a multivitamin (Emmons, McBride, et al., 2005). Participants were classified as meeting the recommendation if they reported taking a multivitamin at least 6 days per week.
Smoking was assessed using the Behavioral Risk Factor Surveillance Survey Tobacco use module, which assesses lifetime and current smoking (CDC, n.d.). Nonsmokers were classified as meeting smoking guidelines.
Multiple risk behavior score
A multiple risk behavior score (MRB score) was calculated with participants given 1 point for each behavioral recommendation they did not meet (range: 0 = no risk to 5 = all risk behaviors). The MRB score detects improvement in any or all behaviors, and recognizes that everyone may not need to improve all behaviors. When calculating the MRB score, participants with incomplete data for a measured behavior were classified as not meeting the recommendation for that behavior (n = 61).
Psychosocial and contextual factors
We assessed participants’ self-efficacy to do 3+ of the targeted behaviors over the next 6 months (range: not at all confident to extremely confident) using a measure developed from our previous work (Emmons, McBride, et al., 2005). We also assessed level of social resources for chronic illnesses management and healthful behaviors at the interpersonal (friends and family), neighborhood, and organizational levels using sub-scales from the Chronic Illness Resources Survey. Subscales were measured by three items on a 5-point scale (range: not at all to very often), which we used to calculate an average score (range: 0–4) with higher scores being indicative of greater support (Glasgow, Strycker, Toobert, & Eakin, 2000; Glasgow, Toobert, Barrera, & Strycker, 2005). We determined how comfortable participants were using computers (range: very uncomfortable to very comfortable) and frequency of Internet use (The Health Information National Trends Survey [HINTS]: http://hints.cancer.gov/).
Data Analysis
Data were analyzed using a cluster design with provider being the primary sampling unit (cluster) and study subject as the secondary sampling unit. Due to the cluster design, data were weighted to the provider’s panel size. We first calculated descriptive statistics for key variables to describe the entire study sample (weighted sample size = 49,415).
To examine factors associated with participants’ choice of intervention modality, we limited analyses to intervention participants (weighted sample size = 32,691). We examined the correlation between age, education, and perceived health status and computer comfort and frequency of Internet. We then conducted bivariate analyses to examine the associations between participants’ sociodemographic characteristics, health status and health behaviors, psychosocial and contextual factors and chosen modality. Variables significant at p < .05 in these analyses were included in building regression models that examined selected intervention modality. We built models sequentially with the first model including only the sociodemographic variables. After this we added to the model each of the computer-related variables, comfort with computers, and frequency of Internet use both individually and together. Last, we added the other predictor variables that were significant in the initial bivariate analyses. All analyses were conducted using SUDAAN 9.01 and SAS 9.3 statistical software accounting for the cluster design.
Results
Participants
Sociodemographic characteristics
Of the 2,440 participants (weighted sample = 49,415) who completed the baseline survey, 53.9% were White, 27.0% were Black, and 8.8% were Hispanic/Latino; the majority were female (65.8%). The mean age was 49.4 years (SD = 15), and when assessing household financial situation, 24.5% reported being unable to make ends meet or having to cut back (see Table 1).
Table 1.
Description of the Healthy Directions 2 Sample (Weighted Sample = 49,415), Boston, Massachusetts.a
| Sociodemographic characteristics | Mean (SD) or percentage |
|---|---|
| Age (years) | 49.4 (15) |
| Female (male = ref) |
65.8 |
| Race/ethnicity | |
| White | 53.9 |
| Black | 27.0 |
| Hispanic/Latino | 8.8 |
| Other (includes multiracial, Asian) | 8.3 |
| Education | |
| <High school | 3.7 |
| High school graduate/GED | 12.1 |
| Some college/2-year degree | 23.6 |
| ≥College degree | 59.1 |
| Married/partnered | 62.0 |
| Household’s financial status | |
| Comfortable with some extras | 44.1 |
| Enough, no extras | 28.4 |
| Have to cut back | 19.4 |
| Cannot make ends meet | 5.1 |
| Health status | |
| Perceived health | |
| Excellent/very good | 51.0 |
| Good | 35.3 |
| Fair/poor | 12.3 |
| Weight status (body mass index) | |
| Healthy weight/underweight (25.0 kg/m2) |
33.3 |
| Overweight (25.0–29.9 kg/m2) | 32.2 |
| Obese (≥30 kg/m2) | 31.1 |
| Behaviors | |
| Physical activityb | 68.4 |
| Fruits and vegetablesc | 20.2 |
| Red meatd | 53.4 |
| Multivitamine | 29.7 |
| Not smoking | 87.5 |
| Multiple risk behavior scoref | |
| 0 (met all 5 recommendations) | 4.0 |
| 1 (met 4 recommendations) | 17.3 |
| 2 (met 3 recommendations) | 31.4 |
| 3 (met 2 recommendations) | 32.6 |
| 4 (met 1 recommendation) | 13.0 |
| 5 (met none of the recommendations) |
1.8 |
| Contextual and psychosocial factors | |
| Self-efficacy to do 3+ targeted behaviors | |
| Not at all confident | 3.1 |
| A little confident | 7.2 |
| Somewhat confident | 18.0 |
| Very confident | 25.2 |
| Extremely confident | 31.0 |
| Not trying/thinking of doing in next 6 months |
1.7 |
| Comfort level with computers | |
| Very uncomfortable | 11.8 |
| Uncomfortable | 6.1 |
| Comfortable | 26.0 |
| Very comfortable | 54.0 |
| Frequency of Internet use | |
| Never | 7.5 |
| 1–3 times a month | 4.3 |
| Once a week | 3.0 |
| 2–4 times/week | 11.0 |
| Social resourcesg | |
| Interpersonal supports | 1.2 (0.02) |
| Neighborhood supports | 1.4 (0.02) |
| Organizational supports | 0.7 (0.02) |
Percent totals may not add up to 100 because of missing values and/ or rounding.
150+ minutes of moderate physical activity or equivalent of vigorous activity (or combination of the two).
5+ servings/day.
≤3 servings/week.
Taking multivitamin 6 or 7 days/week.
Participants with incomplete data for a behavior were classified as not meeting the recommendation for that behavior (n = 61).
Range 0–4.
p < .05.
p < .01.
Health status
About half of participants rated their health as being excellent/very good (51.0%). Using self-reported data, two thirds of the sample had a BMI ≥ 25 kg/m2.
Health behaviors
Most participants did not meet the recommendations for all behaviors; only 4.0% had an MRB score of 0, indicating that they met all the behavioral recommendations. Nearly half (47.4%) met two or fewer recommendations, and 14.8% met one or none of the recommendations.
Psychosocial and contextual factors
Many participants (56.1%) were extremely confident or very confident that they could meet the recommendations for 3+ of the targeted behaviors within the next 6 months. Participants reported fewer social resources at the organizational level than at the interpersonal level (family and friends) or neighborhood level. Most participants (81.6%) reported being comfortable/very uncomfortable using computers.
Choice of intervention modality
Among intervention participants, slightly more than half (55.4%) elected to receive the intervention materials via the web, whereas 44.6% selected print.
Factors Associated With Selection of Intervention Modality
Correlations
Age, education, and perceived health status were correlated (p < .01) with both computer-related variables (computer comfort, frequency of Internet use); older adults and those who perceived their health status as being poorer reported being less comfortable with computers and using the Internet less often, whereas those with greater educational attainment reported being more comfortable with computers and using the Internet more frequently.
Bivariate analyses
With the exception of marital/partner status, the MRB score, and meeting the recommendations for the individual health behaviors, all the examined variables were associated with selection of intervention modality (p < .05, see Table 2).
Table 2.
Bivariate Associations and the Hierarchal Regression Models Predicting Preference for Web-Based (vs. Print) Materials as the Intervention Modality in the Healthy Directions 2 Study, Boston, Massachusetts (Weighted Sample = 32,691).
| Bivariate analyses |
Sociodemographics + computer comfort |
Sociodemographics + Internet use |
Final model |
|
|---|---|---|---|---|
| OR [95% CI] | OR [95% CI] | OR [95% CI] | OR [95% CI] | |
| Age (years) | 0.96 [0.95, 0.97]** | 0.96 [0.95, 0.97]** | 0.96 [0.95, 0.97]** | 0.96 [0.95, 0.97]** |
| Female (male = Ref) | 0.74 [0.57, 0.96]* | 0.80 [0.60, 1.08] | 0.81 [0.61, 1.08] | 0.81 [0.60, 1.10]* |
| Race/ethnicity (White = Ref) | ||||
| Black | 0.42 [0.33, 0.53]** | 0.61 [0.43, 0.88] | 0.67 [0.49, 0.92] | 0.68 [0.48, 0.96] |
| Hispanic/Latino | 0.70 [0.53, 0.93] | 0.76 [0.48, 1.22] | 0.74 [0.46. 1.19] | 0.77 [0.46, 1.26] |
| Othera | 0.81 [0.59. 1.11] | 0.62 [0.40, 0.96] | 0.63 [0.41, 0.96] | 0.65 [0.42, 1.01] |
| Education | ||||
| <High school (HS) | 0.25 [0.13, 0.48]** | 0.55 [0.28, 1.07] | 1.30 [1.02, 1.65] | 0.98 [0.48, 1.98] |
| HS graduate/GED | 0.49 [0.37, 0.65]** | 0.64 [0.44, 0.93] | 0.86 [0.43, 1.70] | 0.76 [0.50, 1.16] |
| Some college/2-year degree | 1.0 (Ref) | 1.0 (Ref) | 0.70 [0.47, 1.08] | 1.0 (Ref) |
| ≥College degree | 2.06 [1.69, 2.50]** | 1.41 [1.14, 1.76]** | 1.30 [1.02, 1.65]** | 1.24 [1.01, 1.52]* |
| Married/partnered (yes = Ref) | 0.83 [0.68, 1.02] | |||
| Household’s financial status | ||||
| Comfortable, some extras | 1.65 [1.31, 2.07]** | 1.38 [1.08. 1.76]** | 1.31 [1.00, 1.71]** | 1.31 [1.02, 1.69]** |
| Enough, no extras | 1.24 [0.95, 1.63]* | 1.15 [0.81, 1.63] | 1.19 [0.85. 1.66] | 1.19 [0.84, 1.69] |
| Have to cut back | 1.0 (Ref) | 1.0 (Ref) | 1.0 (Ref) | 1.0 (Ref) |
| Cannot make ends meet | 0.52 [0.32, 0.83]** | 0.67 [0.36, 1.24]* | 0.70 [0.39. 1.26] | 0.68 [0.35, 1.33] |
| Health status | ||||
| Perceived health | ||||
| Excellent/very good | 1.74 [1.47. 2.06]** | 1.41 [1.07, 1.85] | 1.57 [1.21, 2.04]** | 1.43 [1.07. 1.91]* |
| Good | 1.0 (Ref) | 1.0 (Ref) | 1.0 (Ref) | 1.0 (Ref) |
| Fair/poor | 0.82 [0.60, 1.11]** | 0.94 [0.67, 1.33] | 1.0 [0.76, 1.58] | 1.02 [0.70, 1.49] |
| Weight status | ||||
| Healthy weight /underweightb | 1.52 [1.30, 1.76]** | 0.81 [0.61, 1.09] | 0.70 [0.53, 0.93]** | 0.77 [0.57, 1.05] |
| Overweightc | 1.42 [1.11, 1.82] | 0.96 [0.64, 1.42] | 0.86 [0.60. 1.22] | 0.90 [0.61, 1.34] |
| Obesed | 1.0 (Ref) | 1.0 (Ref) | 1.0 (Ref) | 1.0 (Ref) |
| Behaviors (met recommendations = Ref) | ||||
| Physical activitye | 0.97 [0.81, 1.16] | |||
| Fruits and vegetablesf | 0.98 [0.80, 1.21] | |||
| Red meatg | 0.88 [0.69, 1.12] | |||
| Multivitaminh | 1.16 [0.96, 1.40] | |||
| Not smoking | 1.07 [0.91, 1.26] | |||
| Multiple risk behavior scorei | ||||
| 0 (met 5 recommendations) | 0.99 [057, 1.73] | |||
| 1 (met 4 recommendations) | 1.06 [0.60, 1.88] | |||
| 2 (met 3 recommendations) | 1/17 [0.64. 2.13] | |||
| 3 (met 2 recommendations) | 0.99 [0.55, 1.79] | |||
| 4 (met 1 recommendation) | 1.06 [0.58, 1.94] | |||
| 5 (met 0 recommendations) | 1.0 (Ref) | |||
| Contextual and psychosocial factors | ||||
| Self-efficacy for 3+ behaviors | ||||
| Not at all confident | 0.51 [0.22, 1.20] | |||
| A little confident | 0.71 [0.43, 1.17] | |||
| Somewhat confident | 1.11 [0.78, 1.57] | |||
| Very confident | 1.0 (Ref) | |||
| Extremely confident | 1.12 [0.83, 1.49] | |||
| Not trying/thinking of doing in next 6 months |
0.30 [0.13, 0.66]* | |||
| Comfort with computers | ||||
| Very uncomfortable | 1.0 (Ref) | 1.0 (Ref) | 1.0 (Ref) | |
| Uncomfortable | 0.13 [0.06, 0.28]** | 0.17 [0.07, 0.41]** | 0.28 [0.11, 0.75]** | |
| Comfortable | 0.91 [0.67, 1.24] | 0.80 [0.55, 1.16] | 0.69 [0.45, 1.05] | |
| Very comfortable | 4.55 [3.40, 6.09]** | 2.63 [1.83, 3.77]** | 1.89 [1.22, 2.92]** | |
| Frequency of Internet use | ||||
| Never | 0.11 [0,04, 0.29]** | 10.27 [0.10, 0.70]** | ||
| 1–3 times a month | 0.43 [0.22, 0.83]* | 0.25 [0.10, 0.68]** | 0.52 [0.22, 1.20]* | |
| Once a week | 1.0 (Ref) | 0.45 [0.22, 0.93]** | 1.0 (Ref) | |
| 2–4 times/week | 1.9 3 [1.09, 3.41]** | 1.0 (Ref) | 1.67 [0.89. 3.16]** | |
| 5+ times/week | 6.89 [4.48. 10.60]** | 1.80 [1.01, 3.20]** | 2.73 [1.61, 4.63]** | |
| Social resourcesj | 4.55 [3.00, 7.00]** | |||
| Interpersonal supports | 1.20 [1.09, 1.33]** | |||
| Neighborhood supports | 1.24 [1.10, 1.40]** | |||
| Organizational supports | 1.25 [1.11, 1.42]** | |||
Note. OR = odds ratio; CI = confidence interval; Ref = reference.
Other includes Asian and multiracial.
Healthy weight/underweight ≤ 25.0 kg/m2.
Overweight: Body mass index = 25.0–29.9 kg/m2.
Obese: Body mass index ≥30.0 kg/m2.
150+ minutes/week of moderate physical activity or equivalent of vigorous activity (or combination of the two).
5+ servings/day.
≤3 servings/week.
Taking multivitamin 6 or 7 days/week.
Participants with incomplete data were classified as not meeting the behavioral recommendation (n = 61).
Range = 0–4.
p < .05.
p < .01.
Hierarchal multivariable analyses
In the initial model with only the sociodemographic variables, age, race/ethnicity, education, perceived health status, weight status, and perceived household financial status, were associated with selected intervention modality (p < .05). When the frequency of Internet use measure was added to the model, all variables remained significant (see Table 2). However, when the model included the sociodemographics and the computer comfort variable, weight status was no longer significant. When both computer-related variables (frequency of Internet use, computer comfort) were added to the model, age, race/ethnicity, perceived health status, perceived household financial status, frequency of Internet use, and computer comfort were associated with selected intervention modality (p < .05). In this model, compared to those who selected print materials, participants who elected to receive web-based materials were more likely to be younger, White, and perceive the financial status of their household as being better. In addition, participants who were most comfortable using computers and accessed the Internet more frequently selected web-based materials. The other predictor variables that were significant in the initial bivariates (the Chronic Illness Resources Survey subscales, self-efficacy to do 3+ behaviors) were added to the model, and the association remained between age, perceived financial status of household, computer comfort, frequency of Internet use, and selection of intervention modality (p < .05), although neither the Chronic Illness Resources Survey subscales nor the self-efficacy measure were significant (data not shown). After building all models, we examined the model fit statistics of each model and determined that the model that included just the sociodemographics variables and both computer-related variables had the best fit. Thus, this became our final model.
Discussion
The health care setting provides an important venue to address multiple risk behaviors simultaneously among a wide range of patients. Results of this study clearly indicate that there is a need for multiple health behavior interventions that can be easily implemented in the health care setting. Nearly half of participants met two or fewer behavioral recommendations, and only 4.0% of participants met all behavioral recommendations. This is a significant issue for primary care, as these behaviors likely drive the multimorbidities that are increasingly seen in this setting (Anderson, 2010; Weiss, Boyd, Yu, Wolff, & Leff, 2007). Although not conducted in the primary care setting, other studies examining multiple behavioral risk factors have found comparable rates of multiple risk behaviors (Emmons et al., 2003; Emmons, McBride, et al., 2005; Emmons, Stoddard, et al., 2005; Ford, Bergmann, Boeing, Li, & Capewell, 2012; Keller, Maddock, Hannover, Thyrian, & Basler, 2008; Reeves & Rafferty, 2005; Troost, Rafferty, Luo, & Reeves, 2012). Allowing patients to self-select their preferred intervention modality may promote intervention engagement (Greaney et al., 2009) and increase the impact of interventions. To our knowledge, HD2 is one of the first studies that provided participants with the opportunity to select their preferred intervention modality. Other intervention studies have used both print and interactive interventions (web, CD-ROM), but participants were randomized to intervention modality (Kroeze, Oenema, Campbell, & Brug, 2008; Marcus et al., 2007; Marshall, Leslie, Bauman, Marcus, & Owen, 2003; Pekmezi et al., 2010). The use of web-based interventions for behavior change is increasing, as these interventions have the potential for a wide reach (Bennett & Glasgow, 2009), and, once a critical threshold of users has been reached, web-based interventions can be more cost-effective than print interventions (Lewis, Williams, Neighbors, Jakicic, & Marcus, 2010). Nonetheless, despite increasing web access, results of this study indicate that interventions implemented in the primary care setting should make health promotion materials available via print and web, as almost half of the participants elected to receive print materials.
Few of the variables that were significantly associated with intervention choice in the bivariate analyses were significant in the final model. It is interesting that participants’ behavioral profiles did not predict preferred modality, as we had hypothesized that those with the most risk behaviors may prefer the interactivity available in web-based materials. Our final model determined that individuals who elected to receive print materials were older, less educated, and in poorer health status and more likely to be Black than those who chose web-based materials. Results of this study indicate that interventions implemented in the health care setting should be available in print- and web-based formats, as limiting interventions to web-based formats could exclude populations with heavy disease burdens (e.g., less educated, older, poorer health status) whereas limiting interventions to print may reduce intervention engagement among younger participants.
The health care setting is an important venue to address behavior change, yet the gap between research and practice is large (Lenfant, 2003). Intervention studies conducted in this setting under ideal circumstances are likely contributing to this gap, as they may be too costly or labor intensive to be implemented in the “real world.” An important step for dissemination is for intervention studies to include realistic alternative treatment comparisons (Tunis, Stryer, & Clancy, 2003). HD2 does this, as it was designed to compare different intervention approaches that are both sustainable and scalable, and to address key implementation challenges.
This study has limitations that should be noted; enrollment was limited to patients with the ability to read and write English and the majority of them were well educated and financially comfortable. These factors may limit generalizability. However, participants were from a large urban primary care practice, and were quite diverse.
Implications for Practice
In this diverse sample of adults from an urban health center, we found that only 4.0% met the recommendations for all five health behaviors, highlighting the need for multiple behavior change interventions. Nearly half of the participants opted for print materials, both print- and web-based intervention materials should be available in the health care setting. Our finding that older participants preferred print materials and that younger people wanted web-based materials is not surprising but does confirm that behavior change materials should be made available in both print and electronic formats, such as interactive websites. Using only web-based format may exclude more vulnerable, needy, and higher risk subsets of the population, individuals often in most need of such interventions whereas using print-based materials may limit intervention engagement among younger participants.
Acknowledgment
We thank Harvard Vanguard Medical Associates for the opportunity to conduct our research in their clinical sites. We would like to thank the HD2 staff: Louisa Bloomstein, Joanne Chin, Lindsay ElShazly, Emma Issenberg, Fatima Shahzad, Kim Skeete, Kristie Usher, and Val Varner. We also would like to thank Martha Zorn for her statistical support.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article:
This work was supported by the National Institutes of Health (NIH Grant Nos. R01 CA123228, 1K05 CA124415).
Footnotes
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Anderson G. Chronic care: Making the case for ongoing care. Princeton, NJ: Robert Wood Johnson Foundation; 2010. Retrieved from http://www.rwjf.org/content/dam/web-assets/2010/01/chronic-care. [Google Scholar]
- Bennett GG, Glasgow RE. The delivery of public health interventions via the Internet: Actualizing their potential. Annual Review of Public Health. 2009;30:273–292. doi: 10.1146/annurev.publhealth.031308.100235. [DOI] [PubMed] [Google Scholar]
- Berrigan D, Dodd K, Troiano RP, Krebs-Smith SM, Barbash RB. Patterns of health behavior in U.S. adults. Preventive Medicine. 2003;36:615–623. doi: 10.1016/s0091-7435(02)00067-1. [DOI] [PubMed] [Google Scholar]
- Broekhuizen K, Kroeze W, van Poppel MN, Oenema A, Brug J. A systematic review of randomized controlled trials on the effectiveness of computer-tailored physical activity and dietary behavior promotion programs: An update. Annals of Behavioral Medicine. 2012;44:259–286. doi: 10.1007/s12160-012-9384-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System Survey Questionnaire. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; (n.d.) [Google Scholar]
- Eakin EG, Bull SS, Riley KM, Reeves MM, McLaughlin P, Gutierrez S. Resources for health: A primary-care-based diet and physical activity intervention targeting urban Latinos with multiple chronic conditions. Health Psychology. 2007;26:392–400. doi: 10.1037/0278-6133.26.4.392. [DOI] [PubMed] [Google Scholar]
- Emmons KM. Maximizing cancer risk reduction efforts: Addressing multiple risk factors simultaneously. Cancer Causes & Control. 1997;8(Suppl. 1):S31–S34. [PubMed] [Google Scholar]
- Emmons KM, Linnan LA, Shadel WG, Marcus B, Abrams DB. The Working Healthy Project: A worksite health-promotion trial targeting physical activity, diet, and smoking. Journal of Occupational and Environmental Medicine. 1999;41:545–555. doi: 10.1097/00043764-199907000-00003. [DOI] [PubMed] [Google Scholar]
- Emmons KM, McBride CM, Puleo E, Pollak KI, Clipp E, Kuntz K, Fletcher R. Project PREVENT: A randomized trial to reduce multiple behavioral risk factors for colon cancer. Cancer Epidemiology, Biomarkers & Prevention. 2005;14:1453–1459. doi: 10.1158/1055-9965.EPI-04-0620. [DOI] [PubMed] [Google Scholar]
- Emmons KM, Stoddard AM, Fletcher R, Gutheil C, Suarez EG, Lobb R, Bigby JA. Cancer prevention among working class, multiethnic adults: Results of the Healthy Directions-Health Centers study. American Journal of Public Health. 2005;95:1200–1205. doi: 10.2105/AJPH.2004.038695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emmons KM, Stoddard AM, Gutheil C, Suarez EG, Lobb R, Fletcher R. Cancer prevention for working class, multiethnic populations through health centers: The healthy directions study. Cancer Causes & Control. 2003;14:727–737. doi: 10.1023/a:1026375408862. [DOI] [PubMed] [Google Scholar]
- Estabrooks PA, Bradshaw M, Dzewaltowski DA, Smith-Ray RL. Determining the impact of Walk Kansas: Applying a team-building approach to community physical activity promotion. Annals of Behavioral Medicine. 2008;36:1–12. doi: 10.1007/s12160-008-9040-0. [DOI] [PubMed] [Google Scholar]
- Ford ES, Bergmann MM, Boeing H, Li C, Capewell S. Healthy lifestyle behaviors and all-cause mortality among adults in the United States. Preventive Medicine. 2012;55:23–27. doi: 10.1016/j.ypmed.2012.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fine LJ, Philogene GS, Gramling R, Coups EJ, Sinha S. Prevalence of multiple chronic disease risk factors. 2001 National Health Interview Survey. American Journal of Preventive Medicine. 2004;27(2 Suppl.):18–24. doi: 10.1016/j.amepre.2004.04.017. [DOI] [PubMed] [Google Scholar]
- Glasgow RE, Strycker LA, Toobert DJ, Eakin E. A social-ecologic approach to assessing support for disease self-management: The Chronic Illness Resources Survey. Journal of Behavioral Medicine. 2000;23:559–583. doi: 10.1023/a:1005507603901. [DOI] [PubMed] [Google Scholar]
- Glasgow RE, Toobert DJ, Barrera M, Jr, Strycker LA. The Chronic Illness Resources Survey: Cross-validation and sensitivity to intervention. Health Education Research. 2005;20:402–409. doi: 10.1093/her/cyg140. [DOI] [PubMed] [Google Scholar]
- Greaney ML, Quintiliani LM, Warner ET, King DD, Emmons KM, Colditz GA, Bennett GG. Weight management among patients at community health centers: The “Be Fit, Be Well” Study. Obesity and Weight Management. 2009;5:222–228. [Google Scholar]
- Harley AE, Devine CM, Beard B, Stoddard AM, Hunt MK, Sorensen G. Multiple health behavior changes in a cancer prevention intervention for construction workers, 2001–2003. Preventing Chronic Disease. 2010;7:A55. [PMC free article] [PubMed] [Google Scholar]
- Honoré PA, Wright D, Berwick DM, Clancy CM, Lee P, Nowinski J, Koh HK. Creating a framework for getting quality into the public health system. Health Affairs (Millwood) 2011;30:737–745. doi: 10.1377/hlthaff.2011.0129. [DOI] [PubMed] [Google Scholar]
- Hyman DJ, Pavlik VN, Taylor WC, Goodrick GK, Moye L. Simultaneous vs sequential counseling for multiple behavior change. Archives of Internal Medicine. 2007;167:1152–1158. doi: 10.1001/archinte.167.11.1152. [DOI] [PubMed] [Google Scholar]
- Keller S, Maddock JE, Hannover W, Thyrian JR, Basler HD. Multiple health risk behaviors in German first year university students. Preventive Medicine. 2008;46:189–195. doi: 10.1016/j.ypmed.2007.09.008. [DOI] [PubMed] [Google Scholar]
- Koh HK, Sebelius KG. Promoting prevention through the Affordable Care Act. New England Journal Medicine. 2010;363:1296–1299. doi: 10.1056/NEJMp1008560. [DOI] [PubMed] [Google Scholar]
- Krebs P, Prochaska JO, Rossi JS. A meta-analysis of computer-tailored interventions for health behavior change. Preventive Medicine. 2010;51:214–221. doi: 10.1016/j.ypmed.2010.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroeze W, Oenema A, Campbell M, Brug J. The efficacy of web-based and print-delivered computer-tailored interventions to reduce fat intake: Results of a randomized, controlled trial. Journal of Nutrition Education and Behavior. 2008;40:226–236. doi: 10.1016/j.jneb.2007.09.008. [DOI] [PubMed] [Google Scholar]
- Lenfant C. Shattuck lecture—clinical research to clinical practice—lost in translation? New England Journal of Medicine. 2003;349:868–874. doi: 10.1056/NEJMsa035507. [DOI] [PubMed] [Google Scholar]
- Lewis BA, Williams DM, Neighbors CJ, Jakicic JM, Marcus BH. Cost analysis of Internet vs. print interventions for physical activity promotion. Psychology of Sport and Exercise. 2010;11:246–249. doi: 10.1016/j.psychsport.2009.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macera CA, Ham SA, Jones DA, Kimsey CD, Ainsworth BE, Neff LJ. Limitations on the use of a single screening question to measure sedentary behavior. American Journal of Public Health. 2001;91:2010–2012. doi: 10.2105/ajph.91.12.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcus BH, Lewis BA, Williams DM, Whiteley JA, Albrecht AE, Jakicic JM, Bock BC. Step into Motion: A randomized trial examining the relative efficacy of Internet vs. print-based physical activity interventions. Contemporary Clinical Trials. 2007;28:737–747. doi: 10.1016/j.cct.2007.04.003. [DOI] [PubMed] [Google Scholar]
- Marshall AL, Leslie ER, Bauman AE, Marcus BH, Owen N. Print versus website physical activity programs: A randomized trial. American Journal of Preventive Medicine. 2003;25:88–94. doi: 10.1016/s0749-3797(03)00111-9. [DOI] [PubMed] [Google Scholar]
- McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Education Quarterly. 1988;15:351–377. doi: 10.1177/109019818801500401. [DOI] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Preparing people for change. 2nd ed. New York, NY: Guilford Press; 2002. [Google Scholar]
- Noar SM, Benac CN, Harris MS. Does tailoring matter? Meta-analytic review of tailored print health behavior change interventions. Psychological Bulletin. 2007;133:673–693. doi: 10.1037/0033-2909.133.4.673. [DOI] [PubMed] [Google Scholar]
- Orleans CT. Addressing multiple behavioral health risks in primary care. Broadening the focus of health behavior change research and practice. American Journal of Preventive Medicine. 2004;27(2 Suppl.):1–3. doi: 10.1016/j.amepre.2004.05.001. [DOI] [PubMed] [Google Scholar]
- Parekh S, Vandelanotte C, King D, Boyle FM. Design and baseline characteristics of the 10 Small Steps Study: A randomised controlled trial of an intervention to promote healthy behaviour using a lifestyle score and personalised feedback. BMC Public Health. 2012a;12:179. doi: 10.1186/1471-2458-12-179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parekh S, Vandelanotte C, King D, Boyle FM. Improving diet, physical activity and other lifestyle behaviours using computer-tailored advice in general practice: A randomised controlled trial. International Journal of Behavioral Nutrition and Physical Activity. 2012b;9:108. doi: 10.1186/1479-5868-9-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pekmezi DW, Williams DM, Dunsiger S, Jennings EG, Lewis BA, Jakicic JM, Marcus BH. Feasibility of using computer-tailored and Internet-based interventions to promote physical activity in underserved populations. Telemedicine Journal and e- Health. 2010;16:498–503. doi: 10.1089/tmj.2009.0135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prochaska JO, Butterworth S, Redding CA, Burden V, Perrin N, Leo M, Prochaska JM. Initial efficacy of MI, TTM tailoring and HRI’s with multiple behaviors for employee health promotion. Preventive Medicine. 2008;46:226–231. doi: 10.1016/j.ypmed.2007.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pronk NP, Peek CJ, Goldstein MG. Addressing multiple behavioral risk factors in primary care. A synthesis of current knowledge and stakeholder dialogue sessions. American Journal of Preventive Medicine. 2004;27(2 Suppl.):4–17. doi: 10.1016/j.amepre.2004.04.024. [DOI] [PubMed] [Google Scholar]
- Reeves MJ, Rafferty AP. Healthy lifestyle characteristics among adults in the United States, 2000. Archives of Internal Medicine. 2005;165:854–857. doi: 10.1001/archinte.165.8.854. [DOI] [PubMed] [Google Scholar]
- Serdula M, Coates R, Byers T, Mokdad A, Jewell S, Chavez N, Block G. Evaluation of a brief telephone questionnaire to estimate fruit and vegetable consumption in diverse study populations. Epidemiology. 1993;4:455–463. doi: 10.1097/00001648-199309000-00012. [DOI] [PubMed] [Google Scholar]
- Sorensen G, Barbeau E, Stoddard AM, Hunt MK, Kaphingst K, Wallace L. Promoting behavior change among working-class, multiethnic workers: Results of the Healthy Directions—small business study. American Journal of Public Health. 2005;95:1389–1395. doi: 10.2105/AJPH.2004.038745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorensen G, Emmons K, Hunt MK, Barbeau E, Goldman R, Peterson K, Berkman L. Model for incorporating social context in health behavior interventions: Applications for cancer prevention for working-class, multiethnic populations. Preventive Medicine. 2003;37:188–197. doi: 10.1016/s0091-7435(03)00111-7. [DOI] [PubMed] [Google Scholar]
- Sorensen G, Stoddard AM, LaMontagne AD, Emmons K, Hunt MK, Youngstrom R, Christiani DC. A comprehensive worksite cancer prevention intervention: Behavior change results from a randomized controlled trial (United States) Journal of Public Health Policy. 2003;24:5–25. [PubMed] [Google Scholar]
- Sorensen G, Stoddard A, Quintiliani L, Ebbeling C, Nagler E, Yang M, Wallace L. Tobacco use cessation and weight management among motor freight workers: Results of the gear up for health study. Cancer Causes & Control. 2010;21:2113–2122. doi: 10.1007/s10552-010-9630-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toobert DJ, Glasgow RE, Strycker LA, Barrera M, Jr, Ritzwoller DP, Weidner G. Long-term effects of the Mediterranean lifestyle program: A randomized clinical trial for postmenopausal women with type 2 diabetes. International Journal of Behavioral Nutrition and Physical Activity. 2007;4:1. doi: 10.1186/1479-5868-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toobert DJ, Strycker LA, Barrera M, Glasgow RE. Seven-year follow-up of a multiple-health-behavior diabetes intervention. American Journal of Health Behavior. 2010;34:680–694. doi: 10.5993/ajhb.34.6.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toobert DJ, Strycker LA, Barrera M, Jr, Osuna D, King DK, Glasgow RE. Outcomes from a multiple risk factor diabetes self-management trial for Latinas: !Viva Bien! Annals of Behavioral Medicine. 2011;41:310–323. doi: 10.1007/s12160-010-9256-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troost JP, Rafferty AP, Luo Z, Reeves MJ. Temporal and regional trends in the prevalence of healthy lifestyle characteristics: United States, 1994–2007. American Journal of Public Health. 2012;102:1392–1398. doi: 10.2105/AJPH.2011.300326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tunis SR, Stryer DB, Clancy CM. Practical clinical trials: Increasing the value of clinical research for decision making in clinical and health policy. Journal of the American Medical Association. 2003;290:1624–1632. doi: 10.1001/jama.290.12.1624. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Agriculture, U.S. Department of Health and Human Services. Dietary guidelines for Americans, 2005. 6th ed. Washington, DC: Government Printing Office; 2005. [Google Scholar]
- U.S. Department of Health and Human Services. 2008 Physical Activity Guidelines for Americans. Washington, DC: Author; 2008. [Google Scholar]
- Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Medical Care. 1992;30:473–483. [PubMed] [Google Scholar]
- Weiss CO, Boyd CM, Yu Q, Wolff JL, Leff B. Patterns of prevalent major chronic disease among older adults in the United States. Journal of the American Medical Association. 2007;298:1160–1162. doi: 10.1001/jama.298.10.1160-b. [DOI] [PubMed] [Google Scholar]
- Willett WC, Sampson L, Stampfer MJ, Rosner B, Bain C, Witschi J, Speizer FE. Reproducibility and validity of a semiquantitative food frequency questionnaire. American Journal of Epidemiology. 1985;122:51–65. doi: 10.1093/oxfordjournals.aje.a114086. [DOI] [PubMed] [Google Scholar]