Abstract
Wandering spleen is a rare condition, characterized by a mobile spleen that is attached only by an elongated vascular pedicle, allowing it to migrate to any part of the abdomen or pelvis. Mesenteroaxial gastric volvulus usually occurs in children and may be associated with wandering spleen. Both entities result from abnormal laxity or absence of the peritoneal attachments due to abnormal fusion of the peritoneal mesenteries. Pancreatic volvulus is a very rare anomaly, with only a few isolated case reports described in association with wandering spleen. Anomalous right sided descending and sigmoid colon is a very rare entity and its association with wandering spleen has not been previously reported. We report a case of wandering spleen associated with mesenteroaxial gastric volvulus, pancreatic volvulus and rightward shift of the splenic flexure of the colon and right sided descending and sigmoid colon in a young female.
Keywords: Wandering spleen, Ectopic spleen, Gastric volvulus, Pancreatic volvulus, Colon, Computed tomography
CASE REPORT
A 22-year-old woman, previously asymptomatic, with history of mental retardation and epilepsy was admitted to the Emergency Department for abdominal pain and vomiting. The family history was unremarkable.
The physical examination revealed a marked abdominal distension with diffuse tenderness but without signs of peritoneal irritation. Vital signs and laboratory tests showed no remarkable abnormalities.
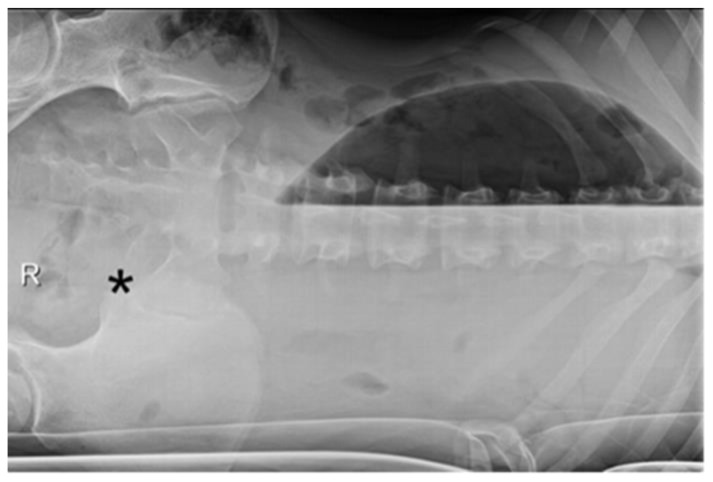
Plain abdominal radiography showed severe gastric distension, empty splenic fossa and a large mass in the right iliac fossa (Fig. 1) moveable in the left lateral decubitus projection (Fig. 2).
Figure 1.
A 22-year-old female with wandering spleen, gastric and pancreatic volvulus and right-sided descending colon.
FINDINGS: Plain abdominal film shows a severe gastric distension (black asterisk), an empty splenic fossa and a mass in the right iliac fossa (white asterisk).
TECHNIQUE: Supine abdominal plain film.
Figure 2.
A 22-year-old female with wandering spleen, gastric and pancreatic volvulus and right-sided descending colon.
FINDINGS: Plain abdominal film demonstrates a moveable mass in the left iliac fossa (black asterisk).
TECHNIQUE: Left lateral decubitus abdominal film.
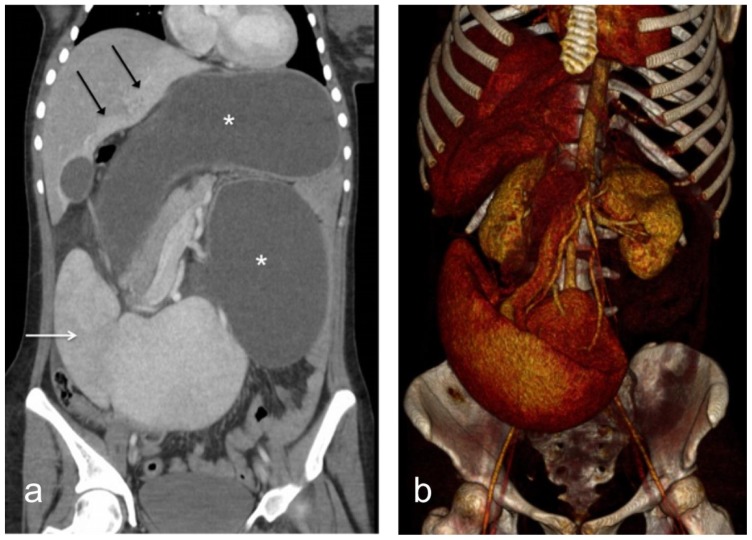
Contrast-enhanced computed tomography (CT) demonstrated severe gastric dilatation with the pylorus lying at the level of the gastroesophageal junction due to mesenteroaxial volvulus (Fig. 3). An enlarged spleen with poor enhancement of the upper pole was located in the right iliac fossa (Fig. 3). A pancreatic volvulus (Fig. 4) and an anomalous rightward shift of the splenic flexure of the colon and right sided descending and sigmoid colon were also seen. (Fig. 5). The splenic vessels were forming a twist leading to enlarged splenic vein secondary to congestion. The liver showed peripheral enhanced areas reflecting increased arterial blood flow due to a reduced portal venous flow (Fig. 3).
Figure 3.
A 22-year-old female with wandering spleen, gastric and pancreatic volvulus and right-sided descending colon.
FINDINGS: Coronal contrast-enhanced CT in portal venous phase (a) demonstrates a large spleen in the right iliac fossa with a perfusion defect in the upper pole (white arrow), a hyper-enhanced area of increased blood flow in the liver (black arrows) and a gastric and pancreatic volvulus (white asterisks). (b) 3D volume rendering image showing the spleen displaced into the right iliac fossa, the torsion of the splenic vessels and the pancreatic volvulus.
TECHNIQUE: Axial contrast-enhanced CT. LightSpeed GE Medical Systems, kVp 120, mA 600, 5 mm slice thickness, Pitch 1.375:1, 100 cc of Ultravist 300 IV, in portovenous phase.
Figure 4.
A 22-year-old female with wandering spleen, gastric and pancreatic volvulus and right-sided descending colon.
FINDINGS: Axial post contrast CT scan in the portal venous phase showing the pancreatic volvulus (white arrow), markedly gastric distension and the absence of descending colon on the left flank.
TECHNIQUE: Axial post contrast CT scan in the portal venous phase. LightSpeed GE Medical Systems, kVp 120, mA 600, 5 mm slice thickness, Pitch 1.375:1, 100 cc of Ultravist 300 IV, in portovenous phase.
Figure 5.
A 22-year-old female with wandering spleen, gastric and pancreatic volvulus and right-sided descending colon.
FINDINGS: Coronal contrast-enhanced CT in portal venous phase demonstrates a right-sided transverse and descending colon (white arrows).
TECHNIQUE: Coronal post contrast CT scan in the portal venous phase LightSpeed GE Medical Systems, kVp 120, mA 600, 5 mm slice thickness, Pitch 1.375:1, 100 cc of Ultravist 300 IV, in portovenous phase.
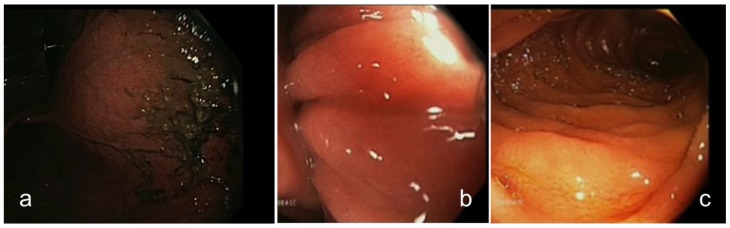
An urgent upper gastrointestinal endoscopy was performed. Mild erosions in the distal esophagus and a huge distension of the stomach that required the aspiration of approximately 4 liters of liquid with fecaloid aspect (Fig. 6), and a pre-pyloric retraction with secondary volvulation. An endoscopic devolvulation was subsequently performed, with resolution of the gastric volvulus.
Figure 6.
A 22-year-old female with wandering spleen, gastric and pancreatic volvulus and right-sided descending colon.
FINDINGS: Upper gastrointestinal endoscopy showing the distended stomach during the aspiration of liquid with fecaloid aspect (a), the torsioned pylorus (b) and the normal distal duodenum after devolvulation (c).
TECHNIQUE: Flexible upper gastrointestinal endoscopy.
After endoscopic devolvulation, plain abdominal radiography confirmed the return of the spleen to its normal position (Fig. 7). The patient was discharged on seventh day remaining asymptomatic.
Figure 7.
A 22-year-old female with wandering spleen, gastric and pancreatic volvulus and right-sided descending colon.
FINDINGS: Abdominal plain film after endoscopic devolvulation shows the return of the spleen and transverse colon to a normal position (white asterisk) and resolution of the gastric volvulus. Note also the right-sided descending colon (white arrow).
TECHNIQUE: Supine abdominal plain film.
DISCUSSION
Wandering spleen
Etiology & demographics
Wandering spleen is a rare condition accounting for less than 0.2% of splenectomies [1,2]. It has two peaks of incidence in children aged less than 10 years and in women of childbearing age [3,4].
This anomaly is characterized by an abnormal localization of the spleen within the abdominal and pelvic cavity due to hyperlaxity, underdevelopment or even absence of splenic suspensory ligaments [1,5].
Both congenital and acquired causes of wandering spleen have been previously described [1,6]. The congenital hypothesis is an anomalous development of the dorsal mesogastrium, which does not fuse with the posterior peritoneum, leading to the absence or abnormal development of one or more of the gastrosplenic, splenorenal and phrenocolic ligaments [3,4]. These ligaments hold the spleen in its normal position and attach it to adjacent viscera. The absence of the splenorenal ligament makes the pancreas not completely retroperitoneal, with its tail localized within the splenic hilum [6]. Acquired anomalies, such as splenomegaly, weakness of the abdominal wall, multiple pregnancies and hormonal changes, have been associated with this entity, explaining its higher incidence among women of reproductive age [4,6]. Both congenital and acquired conditions result in a mobile spleen with predisposition to torsion [2]. An unusual association with gastric and pancreatic volvulus have been described [6].
Clinical & Imaging findings
The clinical presentation of wandering spleen is highly variable, ranging from asymptomatic patients to recurrent episodes of abdominal pain and acute abdomen due to complete torsion and splenic infarction [2,4].
Imaging plays a major role in establishing the diagnosis. Plain abdominal radiography findings include the absence of splenic silhouette in the splenic fossa, small bowel loops occupying the left upper quadrant, elevation of the left kidney and a well-circumscribed abdominal mass. US can demonstrate the absence of splenic tissue in its normal position. The echotexture can be normal, heterogeneous or hypoechoic if complete infarction. Doppler sonography can be useful to evaluate the blood flow in the parenchyma and in the splenic vessels. [7]. CT confirms the abnormal position of the spleen at the mid-abdomen, pelvis or more rarely at the right iliac fossa. Often, the spleen is rotated, more commonly counter-clockwise, and usually has vascular congestion signs, so that it may be also increased in size [3]. The “whirl sign” of the splenic pedicle is highly specific and characteristic for splenic torsion and has been described in cases with pancreatic tail involvement, some of them associated with acute pancreatitis [1,2]. Other features of vascular compromise and splenic infarctions include poor enhancement of splenic parenchyma, hyperattenuating pedicle on unenhanced CT due to acute thrombosis, or peripheral enhancement of splenic parenchyma (“pseudocapsule sign”) attributed to chronic ischemia and secondary perisplenic collateral circulation [3,4,8].
Treatment & Prognosis
Surgery is the treatment of choice of wandering spleen. Splenopexy to reduce the risk of torsion and infarction is recommended when a viable wandering spleen is found in the operating room and in the absence of splenic pathology. Splenectomy should be reserved for patients with massive splenic infarction or splenic pathology [4,9].
Gastric volvulus
Etiology & Demographics
Gastric volvulus is an uncommon entity in adults characterized by an abnormal rotation of the stomach of more than 180° around one of its axis. It is thought to be secondary to hyperlaxity or absence of gastric ligaments. In fact, both gastric volvulus and wandering spleen share a common mechanism, the abnormality of intraperitoneal visceral ligaments [10].
There are described 3 types of gastric volvulus according to the axis of rotation: organoaxial, mesenteroaxial and combination. Organoaxial volvulus is the most common form accounting for approximately 60% of cases, being more frequent in adults. Mesenteroaxial volvulus is the least common gastric volvulus, usually occurs in children and may be associated with wandering spleen, diaphragmatic defects, congenital bands, intestinal malrotation and gastric outlet obstruction [9,10]. It is characterized by rotation around the transgastric axis (a line connecting the middle of the lesser curvature with the middle of the greater curvature).
Clinical & Imaging findings
Clinical presentation may vary between an acute abdominal emergency and recurrent volvulus [11]. Acute gastric presentation consists of severe epigastric pain with distension, vomiting followed by violent, non-productive retching and difficulty or inability to pass a nasogastric tube into the stomach (Brochardt’s triad).
The diagnosis of this entity can be often difficult. A delayed or misleading diagnosis may have serious consequences (strangulation, perforation, hemorrhage, ischemia, gastric necrosis) with high rates of mortality (30–50%) [12,13].
In mesenteroaxial volvulus, supine radiograph shows gastric distension with air, while in the organoaxial type, the greater curvature appears above the lesser [9].
On CT scan, mesenteroaxial volvulus is characterized by an abnormal position of pyloroduodenal junction rotated from right to left at the level of a lower gastroesophageal junction and a distended stomach secondary to gastric outlet obstruction [10,11,12].
Treatment & Prognosis
The treatment of gastric volvulus has changed during recent years. After diagnosis, surgery should be considered, especially for acute volvulus given the high risk of immediate complications. In some cases, endoscopic decompression and reduction could be performed [11,13,14,15].
Pancreatic volvulus
Pancreatic volvulus is another unusual entity and its association with wandering spleen has been reported in only a few cases [5,6,16]. Our patient presented a wandering spleen associated with mesenteroaxial gastric volvulus, pancreatic volvulus and right sided descending and sigmoid colon. To our knowledge, this association has not been previously reported.
In summary, an abnormal development of peritoneal ligaments and fascia during the fetal development of dorsal mesogastrium may explain most of these associated anomalies. In our case, we think that the absence of phrenosplenic, phrenocolic and splenorenal ligaments allows the spleen to be mobile and drop into the right iliac fossa. The absence of retro-pancreatic and left retro-colic fasciae leads to a pancreas tail not completely retroperitoneal and a left colon moveable. Then the fall of the spleen would cause the gastric and pancreatic volvulus and folded the splenic flexure and descending colon to the right side by traction trough the gastrosplenic, pancreaticosplenic, splenocolic ligaments that may be present.
TEACHING POINT
Wandering spleen is a rare condition due to laxity or abnormal developmental of the peritoneal ligaments surrounding and supporting the spleen resulting in a hypermoveable spleen. These anomalies may also lead to hypermobility of the adjacent viscerae (stomach, pancreas or colon ) depending on which ligaments are absent and which present.
Table 1.
Summary table of wandering spleen
| Etiology | Congenital or acquired hyperlaxity of the peritoneal splenic ligaments. |
| Incidence | < 0.2% of splenectomies. |
| Gender ratio | Male > Female in children. Female > male in adults. |
| Age predilection | Children aged < 10 years. Women of childbearing age. |
| Risk factors | Trauma, splenomegaly, multiple pregnancies. |
| Treatment | Splenopexy or Splenectomy if infarcted. |
| Prognosis | Good if prompt diagnosis. |
| Complications | Torsion, infarction, splenic vein thrombosis, gastric volvulus, pancreatic volvulus, gastrointestinal obstruction. |
| Imaging findings | X-ray:
|
Table 2.
Differential diagnosis table of wandering spleen and gastric volvulus
| Differential diagnosis | X-Ray | CT |
|---|---|---|
| Wandering spleen |
|
|
| Gastric outlet obstruction with secondary volvulus |
|
|
| Internal hernia involving the stomach |
|
|
ABBREVIATIONS
- CT
Computed Tomography
- MRI
Magnetic Resonance Imaging
- US
Ultrasonography
REFERENCES
- 1.Raissaki M, Prassopoulos P, Daskalogiannaki M, Magkanas E, Gourtsoyiannis N. Acute abdomen due to torsion of wandering spleen: CT diagnosis. European radiology. 1998;8(8):1409–12. doi: 10.1007/s003300050562. [DOI] [PubMed] [Google Scholar]
- 2.Ben Ely A, Zissin R, Copel L, Vasserman M, Hertz M, Gottlieb P, et al. The wandering spleen: CT findings and possible pitfalls in diagnosis. Clinical radiology. 2006;61(11):954–8. doi: 10.1016/j.crad.2006.06.007. [DOI] [PubMed] [Google Scholar]
- 3.Liu HT, Lau KK. Wandering spleen: an unusual association with gastric volvulus. AJR American journal of roentgenology. 2007;188(4):W328–30. doi: 10.2214/AJR.05.0672. [DOI] [PubMed] [Google Scholar]
- 4.Priyadarshi RN, Anand U, Kumar B, Prakash V. Torsion in wandering spleen: CT demonstration of whirl sign. Abdominal imaging. 2013;38(4):835–8. doi: 10.1007/s00261-012-9944-9. [DOI] [PubMed] [Google Scholar]
- 5.Gorsi U, Bhatia A, Gupta R, Bharathi S, Khandelwal N. Pancreatic volvulus with wandering spleen and gastric volvulus: an unusual triad for acute abdomen in a surgical emergency. Saudi journal of gastroenterology : official journal of the Saudi Gastroenterology Association. 2014;20(3):195–8. doi: 10.4103/1319-3767.133026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sheflin JR, Lee CM, Kretchmar KA. Torsion of wandering spleen and distal pancreas. AJR American journal of roentgenology. 1984;142(1):100–1. doi: 10.2214/ajr.142.1.100. [DOI] [PubMed] [Google Scholar]
- 7.Danaci M, Belet U, Yalin T, Polat V, Nurol S, Selcuk MB. Power Doppler sonographic diagnosis of torsion in a wandering spleen. Journal of clinical ultrasound : JCU. 2000;28(5):246–8. doi: 10.1002/(sici)1097-0096(200006)28:5<246::aid-jcu6>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 8.Swischuk LE, Williams JB, John SD. Torsion of wandering spleen: the whorled appearance of the splenic pedicle on CT. Pediatric radiology. 1993;23(6):476–7. doi: 10.1007/BF02012458. [DOI] [PubMed] [Google Scholar]
- 9.Uc A, Kao SC, Sanders KD, Lawrence J. Gastric volvulus and wandering spleen. The American journal of gastroenterology. 1998;93(7):1146–8. doi: 10.1111/j.1572-0241.1998.00349.x. [DOI] [PubMed] [Google Scholar]
- 10.Lee NK, Kim S, Jeon TY, Kim HS, Kim DH, Seo HI, et al. Complications of congenital and developmental abnormalities of the gastrointestinal tract in adolescents and adults: evaluation with multimodality imaging. Radiographics : a review publication of the Radiological Society of North America, Inc. 2010;30(6):1489–507. doi: 10.1148/rg.306105504. [DOI] [PubMed] [Google Scholar]
- 11.Rashid F, Thangarajah T, Mulvey D, Larvin M, Iftikhar SY. A review article on gastric volvulus: a challenge to diagnosis and management. International journal of surgery. 2010;8(1):18–24. doi: 10.1016/j.ijsu.2009.11.002. [DOI] [PubMed] [Google Scholar]
- 12.Millet I, Orliac C, Alili C, Guillon F, Taourel P. Computed tomography findings of acute gastric volvulus. European radiology. 2014;24(12):3115–22. doi: 10.1007/s00330-014-3319-2. [DOI] [PubMed] [Google Scholar]
- 13.Wasselle JA, Norman J. Acute gastric volvulus: pathogenesis, diagnosis, and treatment. The American journal of gastroenterology. 1993;88(10):1780–4. [PubMed] [Google Scholar]
- 14.Jeong SH, Ha CY, Lee YJ, Choi SK, Hong SC, Jung EJ, et al. Acute gastric volvulus treated with laparoscopic reduction and percutaneous endoscopic gastrostomy. Journal of the Korean Surgical Society. 2013;85(1):47–50. doi: 10.4174/jkss.2013.85.1.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kilincalp S, Akinci H, Coban S. Successful treatment of acute gastric volvulus by emergency endoscopic reduction in a patient with cerebral palsy. Endoscopy. 2014;46(Suppl 1):UCTN:E375–6. doi: 10.1055/s-0034-1377350.. [DOI] [PubMed] [Google Scholar]
- 16.Aswani Y, Anandpara KM, Hira P. Wandering spleen with torsion causing pancreatic volvulus and associated intrathoracic gastric volvulus. An unusual triad and cause of acute abdominal pain. JOP : Journal of the pancreas. 2015;16(1):78–80. doi: 10.6092/1590-8577/2905. [DOI] [PubMed] [Google Scholar]