Abstract
The pattern of anatomical organization of the thoraco-abdominal visceral and vascular structures which is not the expected normal arrangement, is called as situs ambiguous or heterotaxy syndrome. Patients with heterotaxy syndrome exhibit a wide spectrum of anatomical variations involving thoraco-abdominal structures. We present here an incidental finding of heterotaxy syndrome associated with unique vascular anomalies in a 35 year old male patient evaluated initially for nephrolithiasis by ultrasonography, and intravenous pyelography. Further evaluation by multidetector row computed tomography showed bilateral bilobed lungs with hyparterial bronchi, cardiac apex to the left, five branches from left-sided aortic arch with retroesophageal right subclavian artery, interrupted inferior vena cava with azygos continuation, left renal vein continuing as hemiazygos vein and replaced common hepatic artery arising from the superior mesenteric artery. Other vascular anomalies include right internal iliac vein joining the left common iliac vein and precaval course of the single main right renal artery. Anomalies involving abdominal organs include right-sided stomach, midline liver, multiple splenules (polysplenia) in right upper quadrant of abdomen, short truncated pancreas, intestinal malrotation, inversion of superior mesenteric vessels and a preduodenal portal vein. To the best of our knowledge this is the first report of association of left renal vein continuing as hemiazygos vein, precaval right renal artery and anomalous branching pattern of aortic arch with heterotaxy syndrome.
Keywords: Heterotaxy syndrome, Polysplenia Syndrome, Situs ambiguous, Truncated pancreas, Interrupted inferior vena cava, Preduodenal portal vein, Intestinal malrotation
CASE REPORT
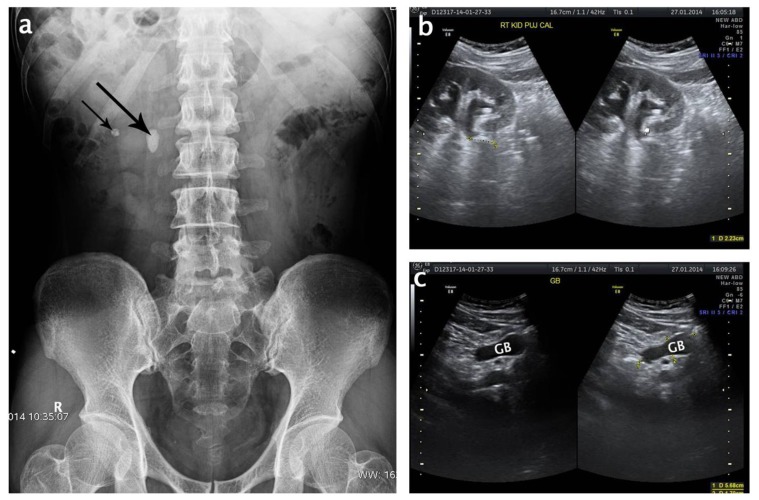
A 35 year old male was referred to our imaging center for the evaluation of suspected nephrolithiasis. Abdominal ultrasonography (USG) and Intravenous pyelography (IVP) revealed a large stone impacted at the pelviureteric junction (PUJ) and another small stone in the lower calyx of right kidney [Figure 1a,b]. Incidental observation of discordant position of gastric gas bubble on the right side in pyelogram and position of gall bladder in USG [Figure-1 c], prompted us for further evaluation of the patient by contrast enhanced computed tomography (CECT). Scanning was done from suprasternal notch to the level of pubic symphysis. A plethora of congenital anomalies involving thoraco-abdominal viscero- vascular structures were seen indicating the presence of heterotaxy polysplenia syndrome.
Figure 1.
A 35 year old male with heterotaxy polysplenia (left isomerism) syndrome. (a) - X-ray showing renal stones (black arrows) at PUJ and lower calyx of right kidney. Discordant position of gastric bubble was noted. (b and c)- USG images showing right kidney and gall bladder. Position of gall bladder was slightly to the left of midline. (Curvilinear 2.5 MHz probe; GE Voluson E8)
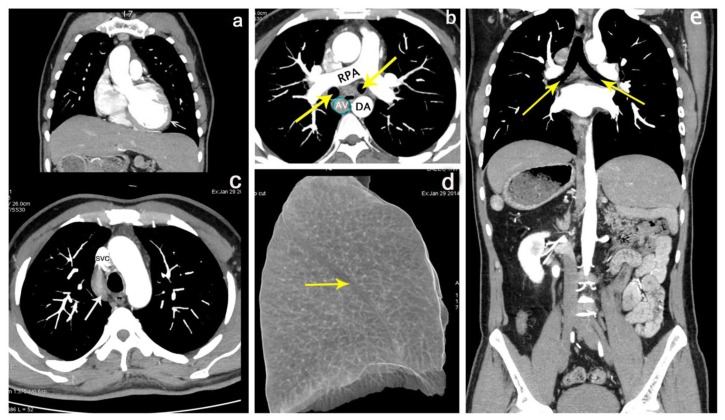
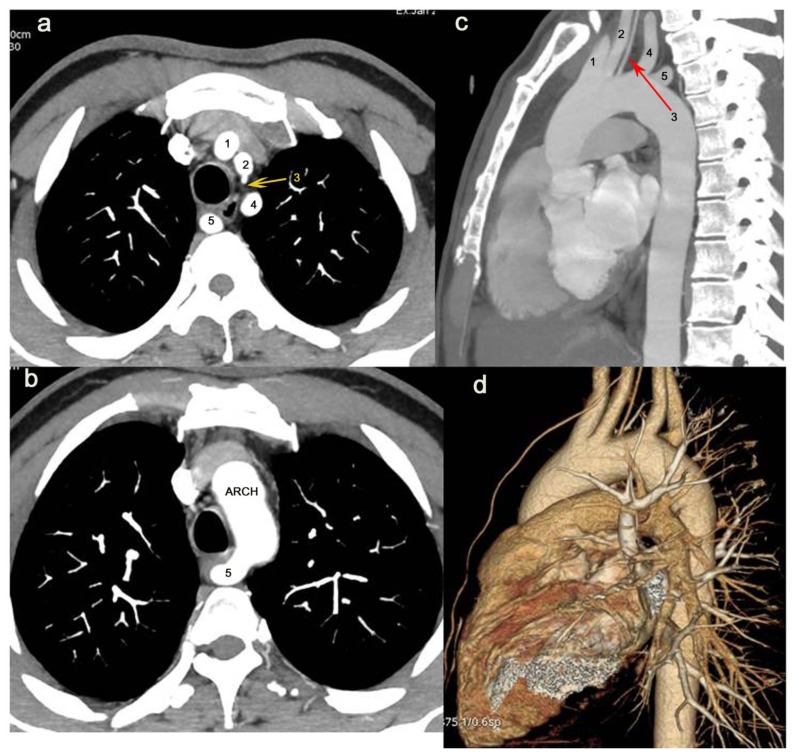
Cardiac shadow was normal with the apex pointing to the left suggesting levocardia [Figure 2a]. Transthoracic echocardiogram performed at a separate cardiology center was normal. No anomaly was observed in the cardiac chambers. Left sided arch of aorta gave rise to five branches, right common carotid, left common carotid, left vertebral, left subclavian and the retroesophageal right subclavian artery [Figure 3]. Right lung showed absence of horizontal (minor) fissure and presence of only two lobes [Figure 2d]. So the patient had bilateral bilobed lungs (thoracic left isomerism) with hyparterial bronchi [Figure 2b, 2e]. The azygos vein was dilated and appeared to be the continuation of inferior vena cava (IVC) [Figure 2b] and drained into superior vena cava [Figure 2c].
Figure 2.
A 35 year old male with heterotaxy polysplenia (left isomerism) syndrome. (a) - Coronal image of chest and abdomen showing normal situs of heart (levocardia) with the cardiac apex pointing to left (arrow). (b)- Axial image of the chest showing enlarged azygos vein ( AV- blue circle) and bilateral hyparterial bronchi (arrows) passing below their respective pulmonary arteries. RPA- right pulmonary artery; DA- descending aorta. (c) Axial image showing the azygos vein (arrow) arching over right lung root to join superior vena cava (SVC). The dilated azygos vein in the right paratracheal space may be mistaken for lymphadenopathy. (d) - VR image of the right lung showing only the major oblique fissure (arrow) and two lobes. (e) Coronal image showing hyparterial bronchi bilaterally passing below their respective pulmonary arteries (arrows). (Protocol: GE Optima 660, 64 channel, mAs 250, kV 120, slice thickness 0.625 mm; Contrast material: 85 ml Omnipaque 350 mg I/ml injected at a rate of 5 ml/s)
Figure 3.
A 35 year old male with heterotaxy polysplenia (left isomerism) syndrome (a and b) Axial images of chest; (c) Sagittal image and (d) VR image of heart showing five branches from left sided arch of aorta, right common carotid (1), left common carotid (2), left vertebral (3), left subclavian (4) and retroesophageal right subclavian artery (5) (Protocol: GE Optima 660, 64 channel, mAs 250, kV 120, slice thickness 0.625 mm; Contrast material: 85 ml Omnipaque 350 mg I/ml injected at a rate of 5 ml/s)
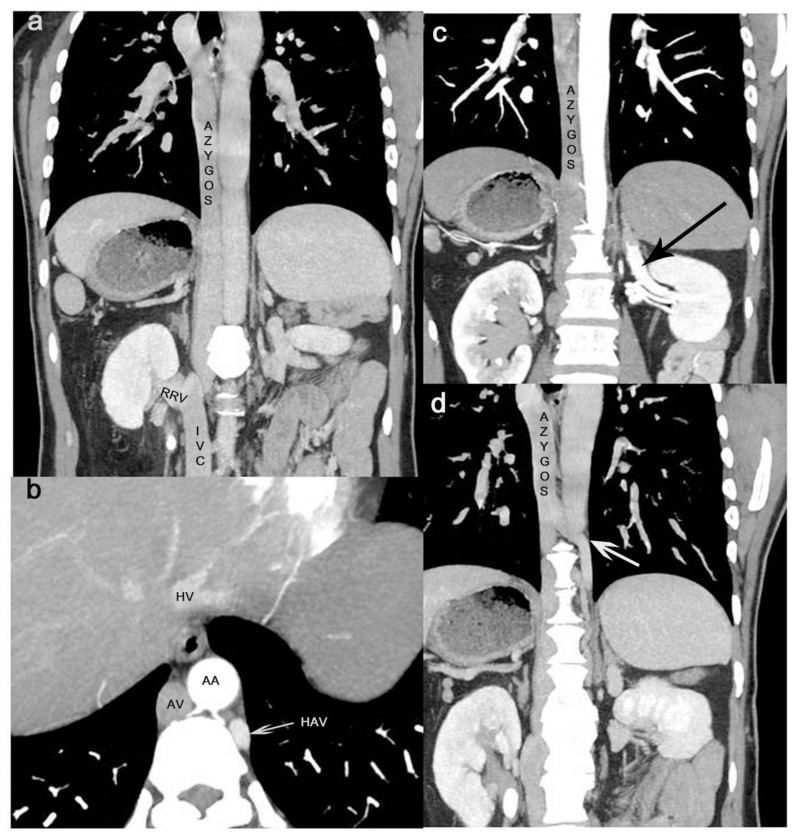
The infrarenal segment of the IVC was normally positioned and after receiving the right renal vein continued as azygos vein (Interrupted IVC with azygos continuation) passing into the retrocrural space [Figure 4a,b]. The left renal vein instead of joining the IVC entered the retrocrural space and continued as hemiazygos vein because the preaortic segment of the vein was absent [Figure 4b,c]. The hemiazygos vein crossed the midline in the posterior mediastinum and drained into azygos vein [Figure 4d]. After draining the hepatic veins, the suprahepatic segment of IVC opened into right atrium [Figure 8c]. Variant formation of IVC by the union of right external iliac vein and left common iliac vein was observed [Figure 5]. The right internal iliac vein crossed the midline and drained into left common iliac vein.
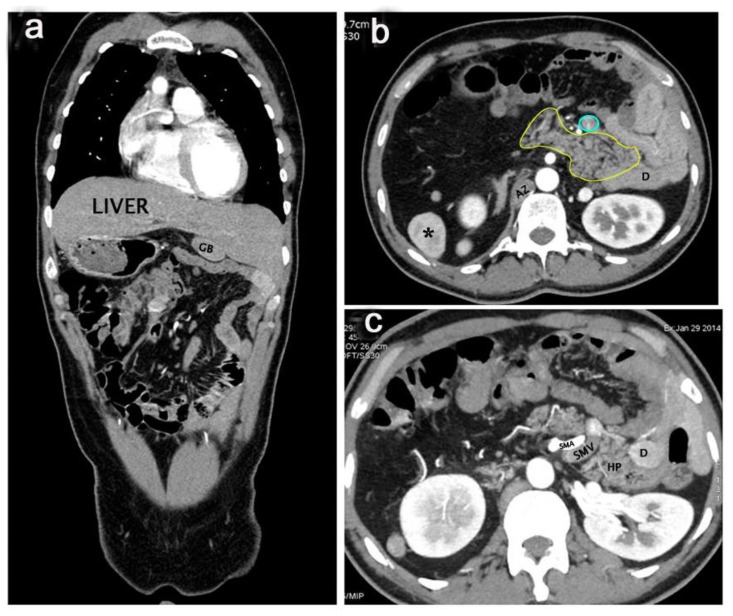
Figure 4.
A 35 year old male with heterotaxy polysplenia (left isomerism) syndrome (a) Coronal image showing the azygos continuation of interrupted inferior vena cava. IVC after receiving right renal vein (RRV) continue as azygos vein. (b) Axial image showing the retrocrural space with abdominal aorta (AA), azygos vein (AV), and hemiazygos vein (HAV). HV- hepatic vein. (c) Coronal image showing left renal vein (arrow) turning upwards and backwards to continue as hemiazygos vein. (d) Coronal image showing the hemiazygos vein crossing the midline (arrow) to drain into azygos vein. (Protocol: GE Optima 660, 64 channel, mAs 250, kV 120, slice thickness 0.625 mm; Contrast material: 85 ml Omnipaque 350 mg I/ml injected at a rate of 5 ml/s)
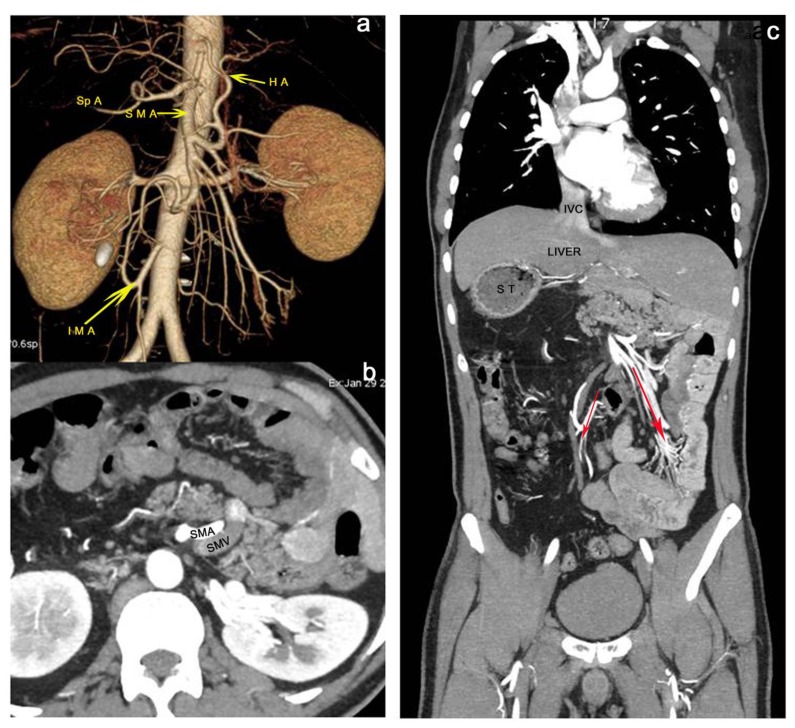
Figure 8.
35 year old male with heterotaxy polysplenia (left isomerism) syndrome (a) VR image showing the replaced common hepatic artery (HA) arising from the superior mesenteric artery (SMA). Splenic artery (SpA) is passing to the right side. Inferior mesenteric artery (IMA) is directed to the right.(b) Axial image showing the reversal of position of SMA and SMV. (c) Coronal image showing intestinal rotational anomaly with small bowel loops occupying the left side and the ileocaecal junction in the left iliac fossa to the left of midline. Ascending colon is present on the left side and descending colon on the right suggested by the direction of SMA (large arrow) and IMA (small arrow) (Protocol: GE Optima 660, 64 channel, mAs 250, kV 120, slice thickness 0.625 mm; Contrast material: 85 ml Omnipaque 350 mg I/ml injected at a rate of 5 ml/s)
Figure 5.
A 35 year old male with heterotaxy polysplenia (left isomerism) syndrome Coronal image of the pelvic region showing the formation of IVC by the union of right external iliac vein (4) with left common iliac vein (*). The left common iliac vein is formed by the union of left internal iliac (2) and left external iliac veins (3). Proximally it receives right internal iliac vein (1). (Protocol: GE Optima 660, 64 channel, mAs 250, kV 120, slice thickness 0.625 mm; Contrast material: 85 ml Omnipaque 350 mg I/ml injected at a rate of 5 ml/s)
The stomach was located in the right upper quadrant of abdomen with eight splenic masses (polysplenia) located along the greater curvature [Figure 6a,b]. The splenic artery originating from the celiac trunk, was seen directed towards the right side. The gall bladder was on the left side but closer to midline with a more or less symmetrical bridging liver [Figure 7a]. A replaced common hepatic artery (CHA) was taking origin from the superior mesenteric artery (SMA) [Figure 8 a]. A preduodenal portal vein (PDPV) was observed lying anterior to head of pancreas and duodenum [Figure 6a,b, 7b]. The pancreas was short and truncated with the agenesis of part of the body and the tail. The head of the pancreas was present on the left side within the reversed loop of duodenum [Figure 7b].
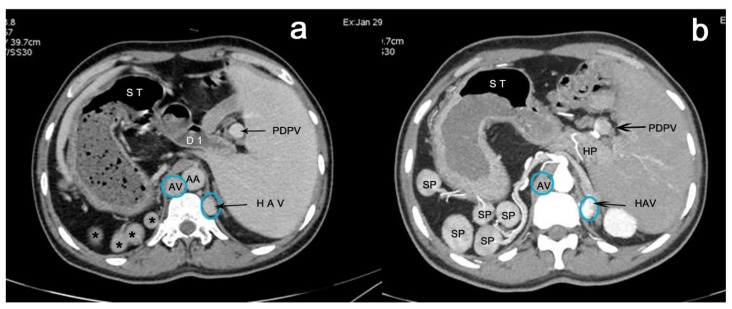
Figure 6.
35 year old male with heterotaxy polysplenia (left isomerism) syndrome (a) Axial image of upper abdomen showing right-sided stomach (ST) continuing towards left as superior duodenum (D1) which is related anteriorly to preduodenal portal vein (PDPV). Multiple splenules (*) related to greater curvature of stomach can be observed in the right upper quadrant. Dilated azygos vein(AV) and hemiazygos vein (HAV) (blue circles) in the retrocrural space lie on either side of the abdominal aorta (AA). (b) Axial image showing PDPV lying anterior to head of pancreas (HP) and five splenules (SP) in the right upper quadrant supplied by a tortuous splenic artery. (Protocol: GE Optima 660, 64 channel, mAs 250, kV 120, slice thickness 0.625 mm; Contrast material: 85 ml Omnipaque 350 mg I/ml injected at a rate of 5 ml/s)
Figure 7.
35 year old male with heterotaxy polysplenia (left isomerism) syndrome (a) Coronal image showing a bridging liver occupying both right and left hypochondrium and a gall bladder (GB) lying to the left of midline. (b) Axial image showing reversed loop of duodenum (D) concavity to the right occupied by pancreas (yellow outline). PDPV (blue circle). One splenule (*) is seen on the right side. A dilated Azygos (AZ) vein is seen to the right of spine. (c) Axial image showing Superior mesenteric vein (SMV) rotation sign. Note the SMV lying to the left of superior mesenteric artery (SMA) which is suggestive of intestinal malrotation. D- Descending duodenum; HP- Head of pancreas. (Protocol: GE Optima 660, 64 channel, mAs 250, kV 120, slice thickness 0.625 mm; Contrast material: 85 ml Omnipaque 350 mg I/ml injected at a rate of 5 ml/s)
The relationship of superior mesenteric vessels was reversed with the superior mesenteric vein (SMV) lying to the left of superior mesenteric artery [Figure 7c, 8b]. The small bowel loops were located on the left side in the upper abdomen and the ileocaecal junction located in the left iliac fossa to the left of midline with the SMA directed downwards and to the left. Ascending colon was situated on the left side and the descending colon on the right side with the inferior mesenteric artery directed downwards and to the right. The location of the bowel loops and the reversal of position of superior mesenteric vessels were suggestive of intestinal malrotation [Figure 8b,c]. No anomaly could be detected in the urogenital organs but the single main right renal artery had a precaval course crossing anterior to IVC to reach renal hilum [Figure 9].
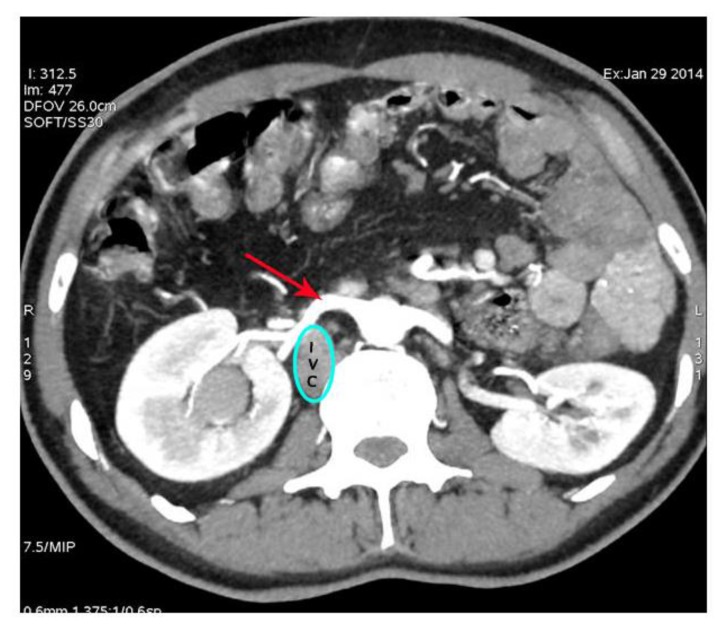
Figure 9.
35 year old male with heterotaxy polysplenia (left isomerism) syndrome Axial image showing the main right renal artery (arrow) passing in front of the IVC (blue circle) to reach the renal hilum - precaval right renal artery. (Protocol: GE Optima 660, 64 channel, mAs 250, kV 120, slice thickness 0.625 mm; Contrast material: 85 ml Omnipaque 350 mg I/ml injected at a rate of 5 ml/s)
DISCUSSION
Heterotaxy is defined as “an abnormality where the internal thoraco-abdominal organs demonstrate abnormal arrangement across the left- right axis of the body” [1,2]. Situs ambiguous is defined as “an abnormality in which there are components of both situs solitus (normal asymmetrical arrangement) and situs inversus (reversal or mirror-image of normal arrangement) in the same person and can be considered to be present when the thoraco-abdominal organs are not clearly lateralized”[1]. Therefore, all patients with heterotaxy can be considered to have situs ambiguous and all patients with situs ambiguous also have heterotaxy syndrome [2]. A confusing array of terms are still being used to classify the heterotaxy, which is generally classified into polysplenia (left isomerism) and asplenia (right isomerism) syndromes. Polysplenia is classically described as left isomerism or bilateral left handedness referring to duplication of left sided structures with bilateral bilobed lungs, bilateral hyparterial bronchi and bilateral pulmonary atria in addition to presence of multiple spleens [3,4]. In nearly 50 % – 90 % cases, polysplenia is associated with complex cardiac anomalies and only about 10% patients may reach adulthood without any complications [5].
Etiology & Demographics
The exact cause of heterotaxia polysplenia syndrome is unknown. Disruption of left-right axis determination during early embryonic development results in a wide variety of cardiac and extracardiac malformations that characterize the human heterotaxy syndrome. There is no single pathognomonic anomaly that characterizes this rare entity. Recent studies have shown that more than 80 genes are required for normal asymmetric left-right organ development. The genes which are implicated in left-right laterality determination and heterotaxy syndrome include, ZIC 3, NODAL, LEFTY 2, ACVR2B, CRYPTIC, CRELD-1, NKX2.5 and SHROOM 3 [6,7]. Microdeletion of Xq26 and mutations in some of these genes have been identified in patients with heterotaxy.
Left to right patterning is one of the most important embryological events for asymmetrical organs like heart, lungs and digestive system. Accurate sequential delivery and expression of precise genetic signals along the left-right axis is responsible for proper morphogenesis and positioning of the internal organs. Different organ systems may have separate left-right signaling systems and failure of normal coordination might have resulted in a set of abnormalities such as situs anomalies of abdominal organs associated with normally positioned heart.
Polysplenia is a rare heterotaxy disorder with a reported incidence of 1 per 250,000 live births [8]. Rose et al has reported that situs ambiguous has an incidence of 1 per 40,000 live births [9]. Abut et al has estimated the incidence of situs inversus to be 1 in 10000 live births and situs ambiguous to be 0.25 in 10000 live births [10]. Gatrad et al reported that the situs ambiguous is more common in a highly inbred community of Asian Muslims (1 in 2700) in comparison to English population (1 in 24000) [11]. Asians have a higher prevalence of heterotaxy syndrome [2]. Polysplenia syndrome is more common in females. It is difficult to calculate exact incidence of polysplenia in adults because of absence of severe congenital heart disease. Situs anomalies are detected incidentally in adults during imaging evaluation for unrelated conditions. Since there is no single pathognomonic anomaly that characterizes this rare entity, it is suggested that the wide spectrum of anomalies need to be described individually [12]. Table-1 and Table-2 summarize the clinical and radiological features of adult cases of heterotaxy polysplenia syndrome.
Table 1.
Summary of clinical and radiological findings of Polysplenia syndrome (PSS)/Heterotaxy syndrome (HS)/Situs ambiguous (SA) in adults (case reports)
| Author & Year | Case Diagnosis | Age & Sex | Poly splenia | Interrupted IVC | Liver | Intestinal Malrotation | Preduodenal portal vein | Stomach | Pancreas | Heart | Lungs |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Vanhoenacker et al. 2001 [28] | HS | 45 F | Right | Lt.-IVC with Azy. Cont. | Left sided | NR | NR | Right | Truncated | Dextro- cardia | NR |
| Abut et al 2003 [10] | SA | 62 F | Right | Rt./Azy.Cont. | Mid line | Yes | NR | Right | NR | ASD | Bilateral bilobed lungs |
| Ito et al 2003 [24] | HS | 76 M | Right | Lt.IVC with azygos cont. | Midline | Nonrotation | NR | Right | Truncated | Levocardia | NR |
| Plata-Munoz et al 2004 [23] | PSS | 56 M | Left | Rt./Azy.Cont. | NR | Yes- Levo rotation | Yes | Left | Truncated | NR | NR |
| Kapa et al 2007 [29] | PSS/HS | 25 M | Left | Rt./Azy.Cont. | N | NR | NR | Left | Truncated | Coarctation of aorta | NR |
| Tsutsumi et al 2007 [26] | SA | 73 M | Right | Interrupted IVC | Midline (CHA from SMA) | Yes – SB - left side | Yes | Right | Pancreas divisum | Levocardia | NR |
| Maier et al 2007 [30] | PSS | 30 F | Left | Lt.IVC Haz.cont. | N | Yes SB-Left LB-Right |
NR | Left | Annular Pancreas | NR | NR |
| Seo et al. 2008 [31] | PSS | 41 F | Left | NR | N (LHA from LGA) | N | Yes | Left | N | N | N |
| Low et al 2011 [8] | PSS | 62 F | Right | Left IVC | Midline | NR | Yes | Right | Truncated | NR | Bilateral Hyparter ial bronchi |
| Celik et al 2011 [14] | HS | 38 M | Right | NR | Left sided | NR | NR | Right | NR | PDA, aberrant RSA | NR |
| De Wailly et al 2011 [27] | PSS | 56 F | Left | Rt./Azy.Cont. | N(HA from SMA | NR | Yes | Left | Anular pancreas | NR | NR |
| Kim et al 2011 [32] | SA | 42 M | Left | Lt./Haz.Cont. | N | Yes SB- Right LB-Left |
NR | Left | NR | N | NR |
| Kim et al 2011 [32] | SA | 52 F | Right | Left IVC drain directly into right atrium | Midline | SMV anterior to SMA | NR | Right | NR | Sick sinus syndrome | NR |
| Jeong et al 2012 [33] | PSS | 49 F | Left | Rt./Azy.Cont. | Midline | Yes SB- Right LB- Left |
Yes | Left | Truncated | NR | NR |
| Mehta et al 2012 [34] | Interrupted IVC syndrome | 50 F | Left | Rt./Azy.Cont. | N | Yes SB- Right LB- Left Caecum in midline |
NR | Left | NR | N | N |
| Turkalj et al 2012 35] | PSS | 45 F | Left | NR | Midline | Yes | Yes | Left | Truncated | NR | NR |
| Dilli et al 2012 [36] | HS | 58 F | Left | Left IVC Retroaortic RRV. | Left dominant liver, Right GB | Yes SB- Left LB- Right |
NR | Left | N | Dextro- cardia, right aortic arch | NR |
| Jo et al 2013 [16] | HS with isolated levocardia | 19 M | Right | Lt.IVC drain into right atrium directly | Midline | Yes SB- Right LB-Left |
NR | Right | Truncated | Isolated levocardia | Bilateral Bilobed lungs |
| Brahmbhatt et al. 2014 [37] | HS - PSS | 77 M | Right | Interrupted IVC Left sided | Left sided | NR | NR | Right | NR | Double SVC Sick sinus syndrome | NR |
N- Normal; NR- Anomaly Not reported; M- Male; F- Female; 11 females and 8 males
Azy.Cont- Azygos continuation of IVC; Haz.Cont.- Hemiazygos continuation of IVC; SMA- Superior mesenteric artery; SMV- Superior mesenteric vein; HA/CHA- common hepatic artery; LHA- Left hepatic artery; LGA- Left gastric artery; PDA- Patent ductus arteriosus; SB- Small bowel; LB- Large bowel; RRV- Right renal vein; RSA-Right subclavian artery; HS-Heterotaxy Syndrome; PSS- Polysplenia syndrome; SA-Situs ambiguous
Note: Only adult cases published after 2000 included in the table and the authors do not claim it to be a complete list of the cases.
Clinical & Imaging Findings
Cardiac anomalies & Viscero-atrial situs: Heterotaxy syndrome is known to be associated with complex cardiac anomalies which are less common in polysplenia than in asplenia [13]. Approximately 10% of patients with polysplenia syndrome may reach adulthood without any complications. It is generally expected that in polysplenia bilateral pulmonary atria are present with right pulmonary veins opening into the systemic right atrium. But in adult cases of polysplenia cardiac anomalies are rare and our patient did not show any cardiac anomaly and the cardiac apex was normal, pointing to the left (Levocardia). Both right and left pulmonary veins were normally opening into left atrium. The left-sided arch of aorta was giving origin to five branches, the right common carotid, left common carotid, left vertebral, left subclavian and an aberrant retroesophageal right subclavian artery and it is the only anomaly observed. Though association of aberrant right subclavian artery with heterotaxy polysplenia syndrome has been reported in the literature [14,15], aortic origin of left vertebral artery has not been reported so far with polysplenia syndrome. The authors could find only two case reports of association of aberrant right subclavian artery with polysplenia syndrome suggesting the extreme rarity of occurrence.
Our patient presented thoracic left isomerism in which there is presence of bilobed lungs bilaterally (the right lung had only two lobes with absence of horizontal fissure) with hyparterial bronchi. Both right and left main bronchi were passing below the corresponding pulmonary artery to reach the lung hilum. Bilateral bilobed lungs were present only in 55 % of 146 autopsied cases of polysplenia reviewed [4]. Presence of bilateral bilobed lungs with heterotaxy polysplenia syndrome has been reported in the literature [16,17]. Recently Burton et al in an autopsy case series reported the presence of bilateral bilobed lungs in 48.9 % cases of plysplenia [18].
Venous anomalies: Interruption of the IVC with azygos/hemiazygos continuation is the second most common abnormality associated with polysplenia syndrome [13]. Out of 19 case reports reviewed, right sided IVC was present in 7 and left sided IVC in 9 cases [Table-1]. The suprarenal segment of the IVC was absent due to failure of development of anastomosis between right subcardinal vein and the hepatocardiac channel (derived from right vitelline vein) but the suprahepatic segment is usually present draining the hepatic veins and opening directly into the right atrium. In the present case, the renal segment of the normally placed IVC after receiving the right renal vein entered the retrocrural space and continued as the azygos vein while the left renal vein continued as hemiazygos vein. Normally the azygos vein begins as lumbar azygos vein from the posterior aspect of IVC at the level of renal vein and the hemiazygos vein is similarly connected to left renal vein. The azygos and the hemiazygos veins develop from thoracic part of the embryonic right and left supracardinal veins which are connected caudally to corresponding subcardinal veins. The preaortic segment of the left renal vein was absent due to failure of development of intersubcardinal anastomosis and the persistence and enlargement of connection between left supracardinal and subcardinal veins result in hemiazygos continuation of left renal vein. To the best of our knowledge, this is the first case report of association of left renal vein continuing as hemiazygos with hetreotaxy polysplenia syndrome. Absence of right sided IVC with hemiazygos continuation of left IVC and right renal vein joining the azygos vein was reported in a 10 year old boy with heterotaxy syndrome [19].
Formation of IVC was also anomalous in the present case. The IVC was formed by the union of left common iliac vein (LCIV) with right external iliac vein (REIV). The right internal iliac vein (RIIV) crossed the midline to drain into LCIV. The right common iliac vein was not formed. Though sporadic case reports on anomalous formation of IVC by the union of LCIV and REIV have appeared in the literature [20,21], its association with heterotaxy polysplenia syndrome has not been reported previously. To the best of our knowledge the present case is the first such association of anomalous IVC formation with polysplenia.
Splenic and Gastric anomalies: In polysplenia syndrome, by definition, multiple spleens, number varying from 2 to 16, are present either on the left or right side, but mostly along the greater curvature of stomach. In the present case both stomach and eight splenules were located in the right upper quadrant. Out of 19 case reports analyzed (Table-1) right sided stomach was observed in 9 cases and right sided spleens in 9 cases. Discordant position between stomach and spleen in one case was reviewed by Gayer et al [5] and another case was reported by Applegate et al [12] (Table-2). Applegate et al reported the presence of right sided stomach in 5 cases and a single spleen in 6 out of 10 cases with polysplenia syndrome [12]. Reviewing abdominal manifestations of situs anomalies, Fulcher and Turner reported polysplenia in 7 out of 8 cases [22]. In another review, right sided stomach was observed in 14 out of 23 cases [23]. In an autopsy case series 87.0 % cases of polysplenia had right sided stomach [18]. Normal clockwise rotation during development brings the stomach to the left side and counterclockwise rotation brings it to the right side. Because spleen develops in the dorsal mesogastrium, discordant position of spleen and stomach is not expected. and only two cases of right sided stomach with left sided spleens were reported [5,12].
Table 2.
Summary of clinical and radiological findings of Polysplenia syndrome (PSS)/Heterotaxy syndrome (HS)/Situs ambiguous (SA) in adults (Case Series/Review)
| Author & Year | Total No. | Sex | Spleen | Stomach | Liver | Intestinal Malrotation | Preduodenal portal vein | Pancreas | IVC | Heart | Lungs |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Applegate et al 1999 [12] * | 10 (Own series) | F – 9 M - 1 |
Right- 5 Left - 5 Multiple-4 (R-2,L-2) Single- 6 (R-3,L-3) |
Right - 5 Left- 3 Middle- 2 (R/M-1, L/M-1) |
Midline- 5 Right – 4 Left - 1 |
Yes-3 unknown- 7 |
---- | ---- | Right-3 Left – 4 Azy.Cont.-8 |
Apex, R- 1 Apex – L- 9 Arch – R-4 Arch- L - 6 |
Bilobed – 3 Unknown- 7 |
| Gayer et al 1999 [5] ** | 8 (Own series) | F- 5 M- 3 |
Right- 6 Left - 2 |
Right- 6 Left - 2 |
Midline – 4 Right – 1 Left - 3 |
Yes– 5 Unknown- 2 Normal -1 |
Yes - 7 | Short- 4 Normal-3 |
Right-1 Left – 7 Azy.Cont.-6 |
Levo– 6 Dextro- 2 |
---- |
| 15 (Review of reported cases) | F- 7 M- 8 |
Right- 7 Left - 6 Left-2 (Bizarre shaped) |
Right- 8 Left - 7 |
Midline – 8 Right – 7 |
Yes – 5 Unknown- 8 Normal -2 |
Yes – 7 Unknown- 8 |
Short- 7 Normal-2 Unknown-6 |
Right-8 Left – 4 Unknown 3 Azy.Cont.-13 |
Levo – 11 Unknown-4 |
---- | |
| Fulcher & Turner, 2002 [22] | 8 (Own series) | F- 4 M- 4 |
Right- 3 Left - 5 Multipl.7 |
Right- 3 Left - 5 |
Midline– 5 Right– 3 |
Yes - 7 | ---- | Short - 6 | Right– 6 Left– 1 Duplicate-1 Azy.Cont.-7 |
Levo– 7 Dextro- 1 Left arch– 7 Aorta left side-7 |
---- |
| Plata-Munoz et al. 2004 [23] | 23 (Review of reported cases) | F- 12 M- 11 |
Right- 14 Left - 9 |
---- | Midline-11 | Yes-10 Unknown-11 Normal-2 |
Yes-14 Unknown-9 |
Short- 10 Normal-5 Unknown-8 |
Right-9 Left– 11 Unknown-3 Rt.Cont. -8 Lt.Cont.- 8 |
---- |
Total 64 cases, Females 37and Males 27.
Applegate et al [12] reported the presence of a right sided stomach with single left sided spleen in one of his 10 patients.
Gayer et al [5] reported the presence of a right sided stomach with left sided multiple spleens in one patient in his review of 15 published cases.
Pancreatic anomalies: Truncated or short pancreas, due to congenital agenesis of dorsal pancreas, is one of the frequently associated anomalies with polysplenia syndrome. Partial agenesis of dorsal pancreas results in absence of tail and part of body of the pancreas as in the present case. Both splenic and pancreatic anomalies occur together in the heterotaxy polysplenia syndrome because both organs develop in the dorsal mesogastrium. Truncated pancreas is observed in 8 out of 19 case reports analyzed [Table-1]. Other pancreatic anomalies reported to be associated with polysplenia syndrome include annular pancreas, pancreas divisum and pancreatic malrotation [24]. In the present case the head of pancreas was observed on the left side in the concavity of reversed loop of duodenum extending up to the midline. Though short and truncated pancreas was associated with polysplenia, unfortunately, description of position of head of pancreas was lacking in most of the case reports.
Intestinal malrotation: Polysplenia syndrome may also be associated with intestinal malrotaion. Out of 19 case reports analyzed, intestinal rotational anomalies were present in 11 cases [Table-1]. In our case the small bowel loops were all located on the left side and the ileocaecal junction was located in the left iliac fossa to the left of midline. Ascending colon was present on the left side and descending colon on the right side. Moreover, third part of duodenum was not seen horizontally in its normal position. The presence of rotational anomaly is also indicated by the presence of “SMV Rotation sign” [25] and possibly by the direction of superior and inferior mesenteric arteries. Nichols and Li [25] suggested that the SMV rotation sign on CT is a very useful radiographic finding that should suggest a diagnosis of intestinal malrotation. They argued that the SMV lying in the mesentery will describe a counterclockwise rotation around the SMA, the axis of the midgut rotational process, during normal development. The final position of the SMV relative to SMA reflects the degree of rotation that has occurred. In the present case the SMV was present on the left side of SMA (reversal of the normal relationship). It was also noticed that the SMA was directed downwards and to the left and IMA downwards and to the right correlating with the position of bowel loops. Fulcher and Turner observed intestinal rotational anomalies in 7 out of 8 cases [22]. Malrotated intestine was seen in 60.4 % cases of polysplenia in an autopsy case series [18].
Preduodenal Portal Vein (PDPV): Preduodenal portal vein is another anomaly frequently associated with polysplenia syndrome and Gayer et al described this anomaly in 7 out of 8 cases of his own series [5] (Table 2). Out of 19 case reports (Table 1), the PDPV was present in 7 cases. PDPV is a surgically important anomaly and can produce pressure symptoms on the duodenum and bile duct. This congenital anomaly occurs due to atrophy of part of left vitelline vein and middle and cranial anastomoses between the right and left vitelline veins and persistence of caudal ventral anastomosis.
Liver: A midline or bridging liver associated with polysplenia syndrome was observed in 8 out of 19 case reports analyzed [Table-1]. Midline symmetrical liver was observed in 58.1 % cases of polysplenia [18]. In two cases, anomalous origin of hepatic artery from superior mesenteric artery was reported [26, 27]. In our patient also the common hepatic artery was originating from the superior mesenteric artery.
No anomaly could be detected in the urogenital organs. The main right renal artery was passing anterior to IVC to reach renal hilum (precaval course). Precaval position of single main right renal artery is extremely rare and its association with polysplenia is being reported for the first time.
Treatment & Prognosis
Management of adult cases of polysplenia (left isomerism) is mainly palliative and symptom specific. In the present case, the renal stones were surgically removed. Surgical correction of cardiac anomalies are suggested in childhood. Prognosis is not good in cases of polysplenia associated with severe cardiac anomalies and it is reported that 75 % of patients die before 5 years of age [19, 23]. Only 5 – 10 % of patients without cardiac involvement reach adulthood [23]. Adult patients with polysplenia syndrome may not exhibit any specific symptoms and are generally diagnosed incidentally while investigating for other reasons as in the present case. Presence of associated anomalies such as preduodenal portal vein, intestinal malrotation and vascular anomalies are surgically important and prior knowledge of such anomalies will help to avoid complications during surgical and interventional procedures.
Conclusion
Patients with heterotaxy polysplenia syndrome exhibit a wide spectrum of anomalies involving thoraco-abdominal viscera and vessels. In many adult cases, the polysplenia syndrome is incidentally detected when the patients were being evaluated for other reasons. To avoid misdiagnosis and misinterpretation of the diverse anomalies associated with heterotaxy polysplenia syndrome, proper recognition of all the anomalies is crucial. Accurate diagnosis is also essential for proper planning of surgical and interventional procedures and to obviate damage to important structures. A thorough and comprehensive evaluation of both chest and abdomen, employing appropriate imaging modalities like echocardiography, ultrasonography, CT and MRI is essential to appreciate diverse visceral and vascular abnormalities of heterotaxy syndrome.
TEACHING POINT
Abnormal arrangement of thoraco-abdominal visceral and vascular structures in association with dysmorphism, is called heterotaxy syndrome or situs ambiguous syndrome which can be subdivided into polysplenia and asplenia syndromes. Because the heterotaxy polysplenia syndrome has no single pathognomonic feature, in every case comprehensive description of all clinical and radiological features is mandatory. The most consistently seen features associated with this syndrome are polysplenia, right sided stomach, interrupted IVC with azygos continuation, bilateral bilobed lungs, midline symmetrical liver and intestinal malrotation.
Table 3.
Summary table for heterotaxy polysplenia (left isomerism) syndrome.
| Aetiology | Exact cause not known. Congenital with multifactorial inheritance- autosomal dominant, autosomal recessive and X-linked recessive. |
| Incidence | variable; 1 per 250,000 live births [8]; 1 per 40000 live births [9]; 1 per 2700 in highly inbred community of Asian Muslims. [11] |
| Gender ratio | Females > Males |
| Age predilection | Infancy. 50% patients die by 4 months of age and 75% before 5 years of age [18]; only about 5–10% reach adulthood because of absence of severe cardiovascular anomalies[20]. |
| Risk factors | Unknown. Mutations in some genes were reported in some patients with heterotaxy syndrome. |
| Treatment | Surgical correction ; management is mainly palliative in adult cases |
| Prognosis | Poor (75% patients die before 5 years of age). |
| Findings on imaging |
|
Table 4.
Differential table for heterotaxy polysplenia (left isomerism) syndrome
| Disorder | X-ray | Echocardiography | USG | CT | MRI |
|---|---|---|---|---|---|
|
Heterotaxy (Situs ambiguous) Polysplenia (Left isomerism) Syndrome |
|
|
|
|
|
|
Heterotaxy (Situs ambiguous) Asplenia (Right isomerism) Syndrome |
|
|
|
|
|
| Situs inversus totalis |
|
|
|
|
|
ABBREVIATIONS
- AO/AA
Aorta
- AV
Azygos vein
- ASD
Atrial septal defect
- CECT
Contrast enhanced computed tomography
- CHA/HA
Common hepatic artery
- F
Female
- GB
Gall bladder
- HS
Heterotaxy syndrome
- IMA
Inferior mesenteric artery
- IVP
Intravenous pyelography
- LB
Large bowel
- LGA
Left gastric artery
- LHA
Left hepatic artery
- LRV
Left renal vein
- M
Male
- MR
Magnetic resonance
- N
Normal
- NR
Not reported
- PDPV
Preduodenal portal vein
- PUJ
Pelvi-ureteric junction
- PSS
Polysplenia syndrome
- RRA
Right renal artery
- SMA
Superior mesenteric artery
- SMV
Superior mesenteric vein
- SB
Small bowel
- ST
Stomach
- SP
Splenules
- SpA
Splenic artery
- SVC
Superior vena cava
- SA
Situs ambiguous
- TGA
Transposition of great arteries
- TAPVC
Total anomalous pulmonary venous connection
- USG
Ultrasonography
REFERENCES
- 1.Jacobs JP, Anderson RH, Weinberg PM, et al. The nomenclature, definition and classification of cardiac structures in the setting of heterotaxy. Cardiology in the Young. 2007;17( Suppl S4):1–28. doi: 10.1017/S1047951107001138. [DOI] [PubMed] [Google Scholar]
- 2.Kim SJ. Heterotaxy syndrome. Korean Circ J. 2011;41:227–232. doi: 10.4070/kcj.2011.41.5.227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ghosh S, Yarmish G, Godelman A, Haramati LB, Spindola- Franco H. Anomalies of visceroatrial situs. AJR. 2009;193:1107–1117. doi: 10.2214/AJR.09.2411. [DOI] [PubMed] [Google Scholar]
- 4.Peoples WM, Moller JH, Edwards JE. Polysplenia: a review of 146 cases. Pediatr Cardiol. 1983;4(2):129–137. doi: 10.1007/BF02076338. [DOI] [PubMed] [Google Scholar]
- 5.Gayer G, Apter S, Jonas T, et al. Polysplenia syndrome detected in adulthood: report of eight cases and review of the literature. Abdom Imaging. 1999;24(2):1768–184. doi: 10.1007/s002619900471. [DOI] [PubMed] [Google Scholar]
- 6.Zhu L, Belmont JW, Ware SM. Genetics of human heterotaxias. Eur J Human Genet. 2006;14(1):17–25. doi: 10.1038/sj.ejhg.5201506. [DOI] [PubMed] [Google Scholar]
- 7.Shiraishi I, Ichikawa H. Human heterotaxy syndrome- from molecular genetics to clinical features, management and prognosis. Circ J. 2012;76(9):2066–2075. doi: 10.1253/circj.cj-12-0957. [DOI] [PubMed] [Google Scholar]
- 8.Low JP, Williams D, Chaganti JR. Polysplenia syndrome with agenesis of dorsal pancreas and preduodenal portal vein presenting with obstructive jaundice- a case report asnd literature review. Br J Radiol. 2011;84:e219–e222. doi: 10.1259/bjr/27680217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rose V, Izukawa T, Moes CAF. Syndromes of asplenia and polysplenia. A review of cardiac and non-cardiac malformations in 60 cases with special reference to diagnosis and prognosis. Br Heart J. 1975;37:840–852. doi: 10.1136/hrt.37.8.840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Abut E, Arman A, Guveli H, et al. Malposition of internal organs: A case of situs ambiguous anomaly in an adult. Turk J Gastroenterol. 2003;14(2):151–155. [PubMed] [Google Scholar]
- 11.Gatrad AR, Read AP, Watson GH. Consanguinity and complex cardiac anomalies with situs ambiguous. Arch Dis Child. 1984;59:242–245. doi: 10.1136/adc.59.3.242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Applegate KE, Goske MJ, Pierce G, Murphy D. Situs revisited: Imaging of the heterotaxy syndrome. Radiographics. 1999;19:832–852. doi: 10.1148/radiographics.19.4.g99jl31837. [DOI] [PubMed] [Google Scholar]
- 13.Tawfik AM, Batouty NM, Zaky MM, Eladalany MA, Elmokadem AH. Polysplenia syndrome: a review of the relationship with viscero-atrial situs and the spectrum of extra- cardiac anomalies. Surg Radiol Anat. 2013;35:647–653. doi: 10.1007/s00276-013-1100-x. [DOI] [PubMed] [Google Scholar]
- 14.Celik KM, Celik T, Iyisoy A, Guler A. An unusual combination of congenital anomalies in an adult patient: Patent ductus arteriosus, Kommerell’s diverticulum with aberrant right subclavian artery and heterotaxy syndrome. Hellenic J Cardiol. 2011;52(5):469–472. [PubMed] [Google Scholar]
- 15.Ergun T, Lakadamyali H, Lakadamyali H, Eldem O. Adult polysplenic syndrome accompanied by aberrant right subclavian artery and hemangioma in a cleft spleen: a case report. Ann vasc Surg. 2008;22(4):579–581. doi: 10.1016/j.avsg.2007.12.017. [DOI] [PubMed] [Google Scholar]
- 16.Jo DS, Jung SS, Joo CU. A case of unusual visceral heterotaxy syndrome with isolated levocardia. Korean Circ J. 2013;43:705–709. doi: 10.4070/kcj.2013.43.10.705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Muneta S, Sakai S, Fukuda H, Imamura Y, Matsumoto I. Polysplenia syndrome with various visceral anomalies in an adult: Embryological and clinical considerations. Internal Medicine. 1992;31:1026–1031. doi: 10.2169/internalmedicine.31.1026. [DOI] [PubMed] [Google Scholar]
- 18.Burton EC, Olson M, Rooper L. Defects in laterality with emphasis on heterotaxy syndromes with asplenia and polysplenia: an autopsy case series at a single institution. Pediatr Dev Pathol. 2014;17(4):250–264. doi: 10.2350/13-11-1406-OA.1. [DOI] [PubMed] [Google Scholar]
- 19.Van de Perre, Vanhoenacker FM, Petre C, Van Doorn J, De Schepper AM. Heterotaxy syndrome. JBR-BTR. 2004;87:158–159. [PubMed] [Google Scholar]
- 20.Oto A, Akpman E, Surucu HS, et al. Right internal iliac vein joining the left common iliac vein: case report demonstrated by CT angiography. Surg radiol Anat. 2003;25:339–341. doi: 10.1007/s00276-003-0123-0. [DOI] [PubMed] [Google Scholar]
- 21.Cardinot TM, Aragao AHBM, Babinski MA, et al. Rare variation in course and affluence of internal iliac vein due to its anatomical and surgical significance. Surg Radiol Anat. 2006;28:422–425. doi: 10.1007/s00276-006-0110-3. [DOI] [PubMed] [Google Scholar]
- 22.Fulcher AS, Turner MA. Abdominal manifestations of situs anomalies in adults. Radiographics. 2002;22:1439–1456. doi: 10.1148/rg.226025016. [DOI] [PubMed] [Google Scholar]
- 23.Plata-Munoz JJ, Hernandez-Ramirez D, Anthon FJ, Podgatez E, Avila-Flores F, Chan C. Polysplenia syndrome in the adult patient. Case report with review of literature. Ann Hepatol. 2004;3(3):114–117. [PubMed] [Google Scholar]
- 24.Ito H, Ohgi S, Kanno T, Ishibashi T. Heterotaxy syndrome with pancreatic malrotation: CT features. Abdom Imaging. 2003;28(6):856–858. doi: 10.1007/s00261-003-0034-x. [DOI] [PubMed] [Google Scholar]
- 25.Nichols DM, Li DK. Superior mesenteric vein rotation: A CT sign of midgut malrotation. AJR. 1983;141:707–708. doi: 10.2214/ajr.141.4.707. [DOI] [PubMed] [Google Scholar]
- 26.Tsutsumi R, Nagata Y, Enjoji A, et al. Situs ambiguous with gastric cancer: Report of a case. Surg Today. 2007;37:676–679. doi: 10.1007/s00595-006-3445-9. [DOI] [PubMed] [Google Scholar]
- 27.De Wailly P, Metzler P, Sautot-vial N, Olivier D, Meunier B, Faure JP. Pre-duodenal portal vein in polysplenia syndrome: Clinical effects and surgical application. Surg Radiol Anat. 2011;33:451–454. doi: 10.1007/s00276-010-0768-4. [DOI] [PubMed] [Google Scholar]
- 28.Vanhoenacker FM, De Ruysscher D, De Backer AI, De Schepper AM. Heterotaxy syndrome in adult with polysplenia, visceral and cardiovascular malposition. JBR- BTR. 2001;84(1):1–4. [PubMed] [Google Scholar]
- 29.Kapa S, Gleeson FC, Vege SS. Dorsal pancreas agenesis and polysplenia/Heterotaxy syndrome: A novel association with aortic coarctation and review of the literature. J Pancreas (online) 2007;8(4):433–437. [PubMed] [Google Scholar]
- 30.Maier M, Weisner W, Mengiardi B. Annular pancreas and agenesis of the dorsal pancreas in a patient with polysplenia syndrome. AJR. 2007;188:W150–W153. doi: 10.2214/AJR.05.1859. [DOI] [PubMed] [Google Scholar]
- 31.Seo HI, Jeon TY, Sim MS, Kim S. Polysplenia syndrome with preduodenal portal vein detected in adults. World J Gastroenterol. 2008;14:6418–6420. doi: 10.3748/wjg.14.6418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kim JG, Youn HJ, Kim GH, et al. Incidentally detected situs ambiguous in adults. J Cardiovasc Ultrasound. 2011;19(4):211–215. doi: 10.4250/jcu.2011.19.4.211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jeong JH, Kim GH, Song GA, et al. Polysplenia syndrome with congenital agenesis of dorsal pancreas presenting as acute pancreatitis and the role of endoscopic ultrasonography in its diagnosis. Korean J Gastroenterol. 2012;60(1):47–51. doi: 10.4166/kjg.2012.60.1.47. [DOI] [PubMed] [Google Scholar]
- 34.Mehta AJ, Kate AH, Gupta N, Chhajed PN. Interrupted inferior vena cava syndrome. JAPI. 2012;60:48–50. [PubMed] [Google Scholar]
- 35.Turkalj I, Petrovic K, Stojanivic S, Mikov I. Polysplenia in an adult patient. Intern Med. 2012;51:3219. doi: 10.2169/internalmedicine.51.8812. [DOI] [PubMed] [Google Scholar]
- 36.Dilli A, Gultekin SS, Ayaz UY, Kaplanoglu H, Hekimoglu B. A rare variation of the heterotaxy syndrome. Case Reports in Medicine. 2012 doi: 10.1155/2012/840453. Article ID. 840453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Brahmbhatt P, Barad B, Panchal M, Bhavsar V, Saleem A, Klosterman L. Left-sided liver and right sided polysplenia: A 77 -year-old patient with heterotaxy syndrome. Tenn Med. 2014;107(1):35–36. [PubMed] [Google Scholar]