Abstract
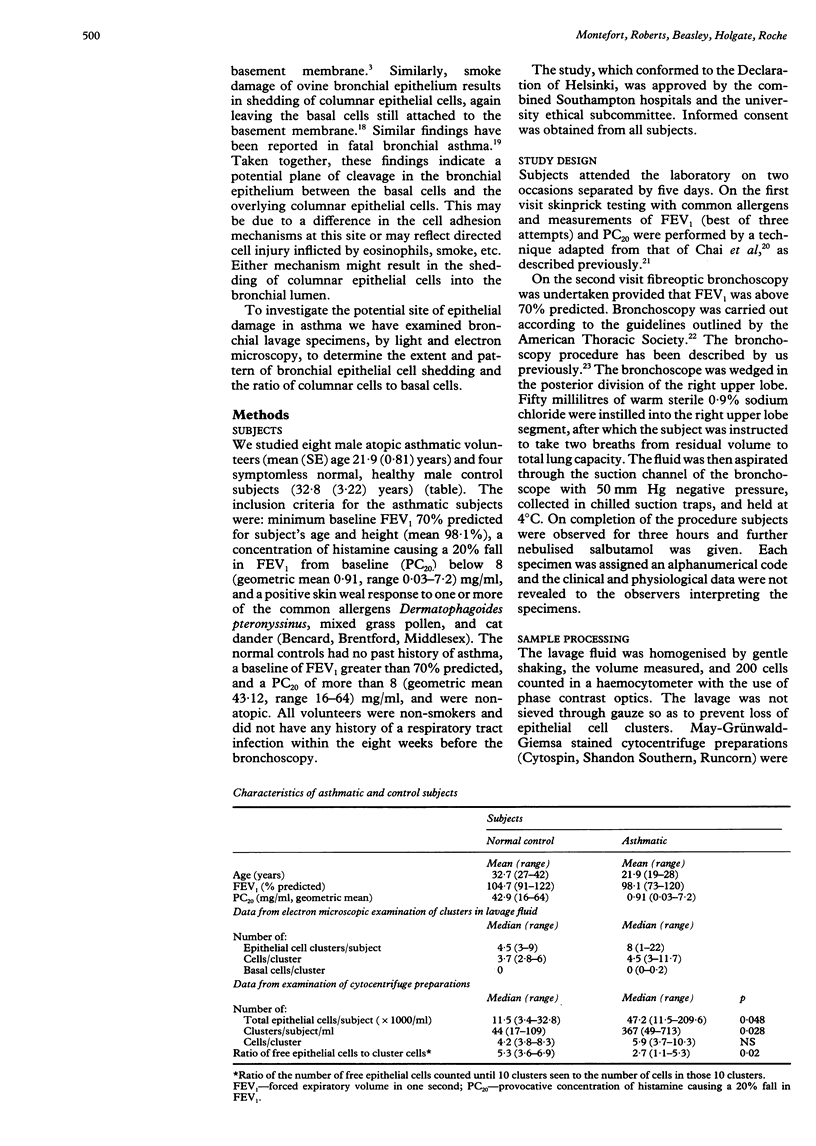
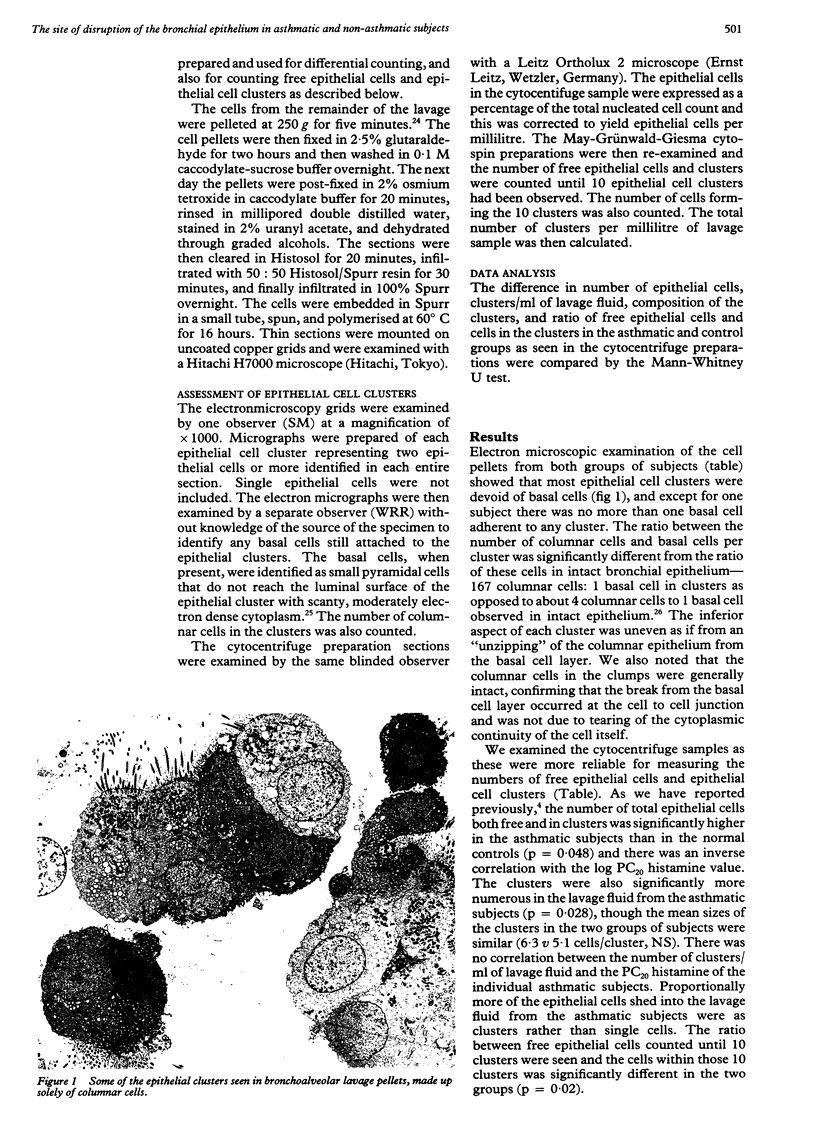
BACKGROUND: Attention has recently been focused on the basal cells of the tracheobronchial epithelium as the mechanism of anchorage of the tall columnar cells, which themselves do not appear to form hemidesmosomes with the basement membrane of the epithelium. Residual basal cells have been described as remaining attached to the basement membrane after epithelial denudation. This led this group to formulate the hypothesis that there may be a potential plane of cleavage between the basal cells and the overlying columnar cell layer within the bronchial epithelium, which becomes disrupted in asthma. METHODS: Bronchoalveolar lavage samples were obtained during bronchoscopy from eight patients with atopic asthma and four normal controls. Ultrathin sections of lavage cell pellets were examined by electron microscopy and the number of columnar and basal cells found in each epithelial cell cluster was counted. Cytocentrifuge preparations of the lavage samples from the same subjects were also examined for free epithelial cells and epithelial cell clusters. RESULTS: Electron microscopic examination of the cell pellets showed that basal cells were present in very small numbers in the epithelial clusters in all subjects (mean 0.03 (SE 0.02)/cluster) and the ratio of columnar cells to basal cells was far greater than was encountered in the intact bronchial epithelium (167 nu 4). The cytocentrifuge preparations showed an increased number of epithelial cell clusters and epithelial cells in the asthmatic patients. Although these clusters were similar in size in the two groups of subjects (6.3 nu 5.1 cells/cluster) the ratio of free epithelial cells to cells within the cluster was higher in the non-asthmatic subjects. CONCLUSIONS: It is proposed that shedding of epithelial cells occurs along a suprabasal plane and that there is a potential plane of cleavage between the suprabasal and the basal cell layers, which might be more vulnerable to the various insults.
Full text
PDF

Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Abdi S., Evans M. J., Cox R. A., Lubbesmeyer H., Herndon D. N., Traber D. L. Inhalation injury to tracheal epithelium in an ovine model of cotton smoke exposure. Early phase (30 minutes). Am Rev Respir Dis. 1990 Dec;142(6 Pt 1):1436–1439. doi: 10.1164/ajrccm/142.6_Pt_1.1436. [DOI] [PubMed] [Google Scholar]
- Barnes P. J. Asthma as an axon reflex. Lancet. 1986 Feb 1;1(8475):242–245. doi: 10.1016/s0140-6736(86)90777-4. [DOI] [PubMed] [Google Scholar]
- Beasley R., Roche W. R., Roberts J. A., Holgate S. T. Cellular events in the bronchi in mild asthma and after bronchial provocation. Am Rev Respir Dis. 1989 Mar;139(3):806–817. doi: 10.1164/ajrccm/139.3.806. [DOI] [PubMed] [Google Scholar]
- Christensen T. G., Breuer R., Hornstra L. J., Lucey E. C., Snider G. L. The ultrastructure of hamster bronchial epithelium. Exp Lung Res. 1987;13(3):253–277. doi: 10.3109/01902148709069593. [DOI] [PubMed] [Google Scholar]
- Cutz E., Levison H., Cooper D. M. Ultrastructure of airways in children with asthma. Histopathology. 1978 Nov;2(6):407–421. doi: 10.1111/j.1365-2559.1978.tb01735.x. [DOI] [PubMed] [Google Scholar]
- DUNNILL M. S. The pathology of asthma, with special reference to changes in the bronchial mucosa. J Clin Pathol. 1960 Jan;13:27–33. doi: 10.1136/jcp.13.1.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Djukanović R., Wilson J. W., Lai C. K., Holgate S. T., Howarth P. H. The safety aspects of fiberoptic bronchoscopy, bronchoalveolar lavage, and endobronchial biopsy in asthma. Am Rev Respir Dis. 1991 Apr;143(4 Pt 1):772–777. doi: 10.1164/ajrccm/143.4_Pt_1.772. [DOI] [PubMed] [Google Scholar]
- Elia C., Bucca C., Rolla G., Scappaticci E., Cantino D. A freeze-fracture study of human bronchial epithelium in normal, bronchitic and asthmatic subjects. J Submicrosc Cytol Pathol. 1988 Jul;20(3):509–517. [PubMed] [Google Scholar]
- Evans M. J., Cox R. A., Shami S. G., Plopper C. G. Junctional adhesion mechanisms in airway basal cells. Am J Respir Cell Mol Biol. 1990 Oct;3(4):341–347. doi: 10.1165/ajrcmb/3.4.341. [DOI] [PubMed] [Google Scholar]
- Evans M. J., Cox R. A., Shami S. G., Wilson B., Plopper C. G. The role of basal cells in attachment of columnar cells to the basal lamina of the trachea. Am J Respir Cell Mol Biol. 1989 Dec;1(6):463–469. doi: 10.1165/ajrcmb/1.6.463. [DOI] [PubMed] [Google Scholar]
- Evans M. J., Plopper C. G. The role of basal cells in adhesion of columnar epithelium to airway basement membrane. Am Rev Respir Dis. 1988 Aug;138(2):481–483. doi: 10.1164/ajrccm/138.2.481. [DOI] [PubMed] [Google Scholar]
- Evans M. J., Shami S. G., Cabral-Anderson L. J., Dekker N. P. Role of nonciliated cells in renewal of the bronchial epithelium of rats exposed to NO2. Am J Pathol. 1986 Apr;123(1):126–133. [PMC free article] [PubMed] [Google Scholar]
- Frigas E., Gleich G. J. The eosinophil and the pathophysiology of asthma. J Allergy Clin Immunol. 1986 Apr;77(4):527–537. doi: 10.1016/0091-6749(86)90341-6. [DOI] [PubMed] [Google Scholar]
- Garrod D. R. Desmosomes, cell adhesion molecules and the adhesive properties of cells in tissues. J Cell Sci Suppl. 1986;4:221–237. doi: 10.1242/jcs.1986.supplement_4.14. [DOI] [PubMed] [Google Scholar]
- Hogg J. C., Eggleston P. A. Is asthma an epithelial disease? Am Rev Respir Dis. 1984 Feb;129(2):207–208. [PubMed] [Google Scholar]
- Laitinen L. A., Heino M., Laitinen A., Kava T., Haahtela T. Damage of the airway epithelium and bronchial reactivity in patients with asthma. Am Rev Respir Dis. 1985 Apr;131(4):599–606. doi: 10.1164/arrd.1985.131.4.599. [DOI] [PubMed] [Google Scholar]
- NAYLOR B. The shedding of the mucosa of the bronchial tree in asthma. Thorax. 1962 Mar;17:69–72. doi: 10.1136/thx.17.1.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rafferty P., Holgate S. T. Terfenadine (Seldane) is a potent and selective histamine H1 receptor antagonist in asthmatic airways. Am Rev Respir Dis. 1987 Jan;135(1):181–184. doi: 10.1164/arrd.1987.135.1.181. [DOI] [PubMed] [Google Scholar]
- Springall D. R., Howarth P. H., Counihan H., Djukanovic R., Holgate S. T., Polak J. M. Endothelin immunoreactivity of airway epithelium in asthmatic patients. Lancet. 1991 Mar 23;337(8743):697–701. doi: 10.1016/0140-6736(91)90279-x. [DOI] [PubMed] [Google Scholar]
- Tandler B., Sherman J., Boat T. F. EDTA-mediated separation of cat tracheal lining epithelium. Am Rev Respir Dis. 1981 Oct;124(4):469–475. doi: 10.1164/arrd.1981.124.4.469. [DOI] [PubMed] [Google Scholar]
- Vanhoutte P. M. Epithelium-derived relaxing factor(s) and bronchial reactivity. Am Rev Respir Dis. 1988 Dec;138(6 Pt 2):S24–S30. doi: 10.1164/ajrccm/138.6_Pt_2.S24. [DOI] [PubMed] [Google Scholar]
- Yurchenco P. D., Schittny J. C. Molecular architecture of basement membranes. FASEB J. 1990 Apr 1;4(6):1577–1590. doi: 10.1096/fasebj.4.6.2180767. [DOI] [PubMed] [Google Scholar]