Abstract
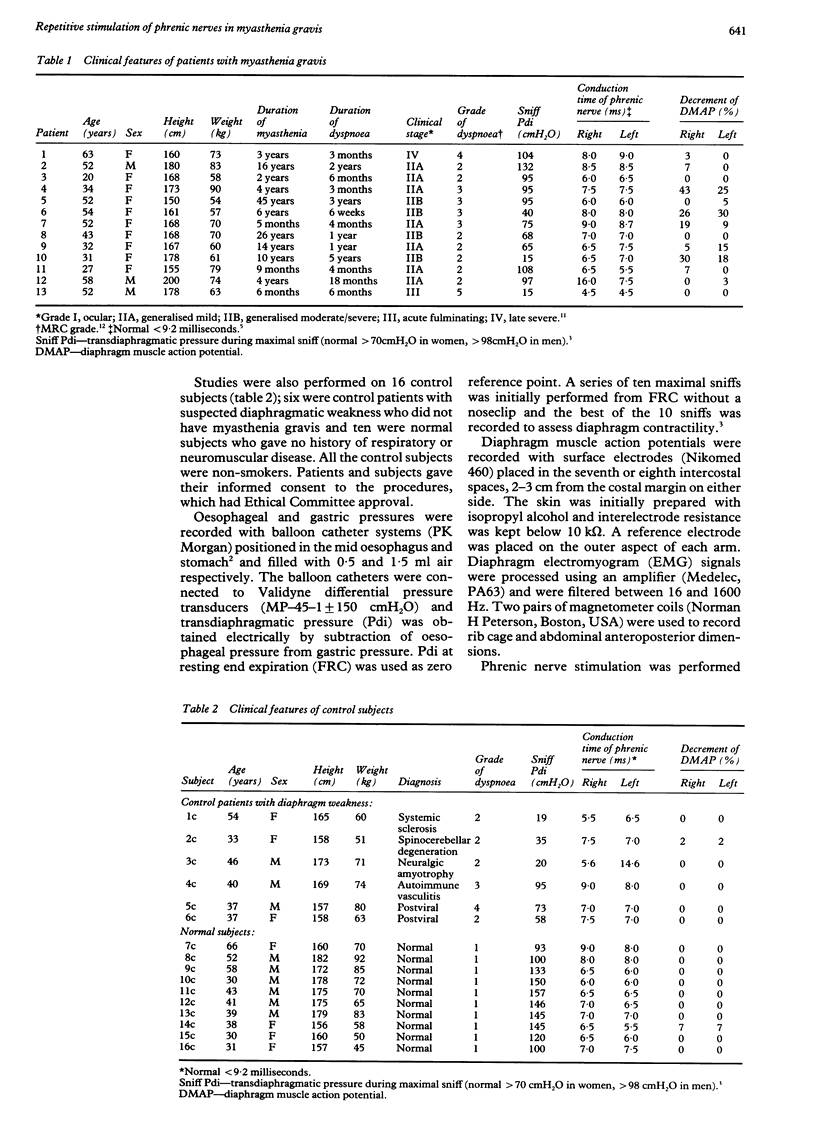
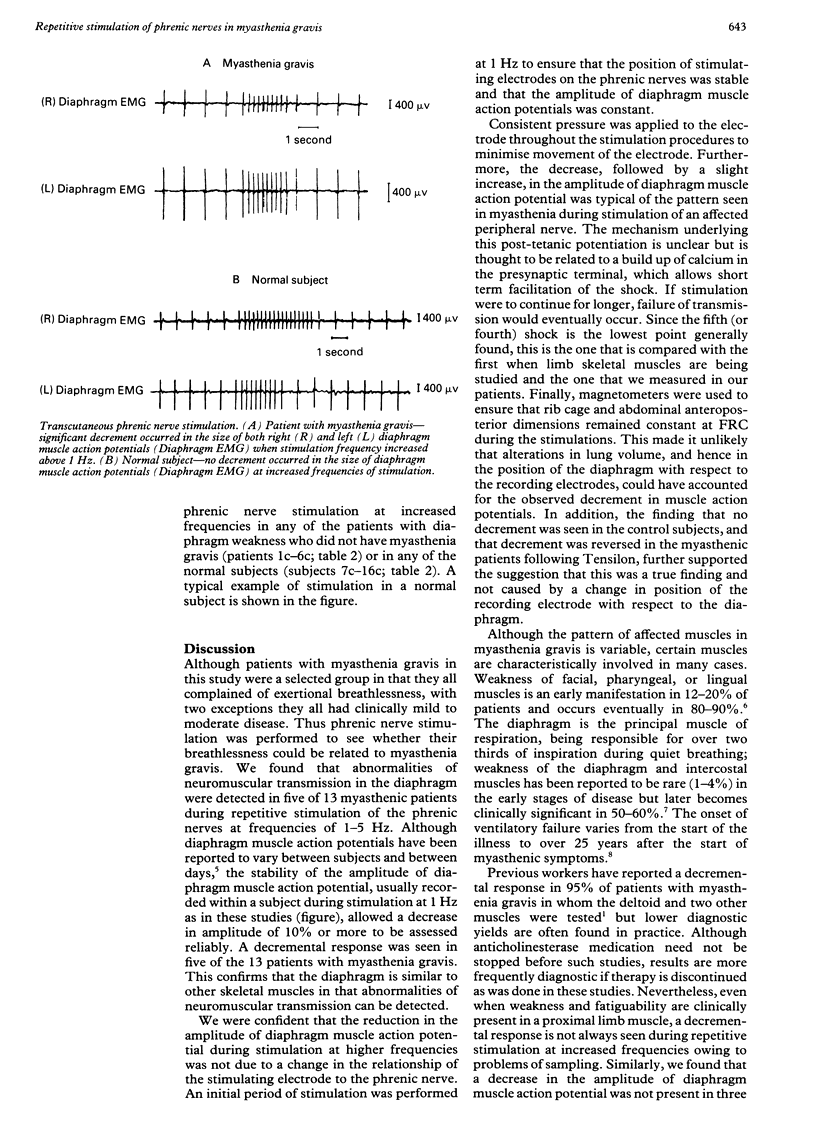
BACKGROUND: In the investigation of patients with myasthenia gravis, repetitive supramaximal stimulation of an affected peripheral nerve is commonly performed to detect abnormal transmission at the neuromuscular junction. A study was undertaken to determine whether abnormal transmission could similarly be detected during stimulation of the phrenic nerves. METHODS: The phrenic nerves were stimulated supramaximally with surface electrodes in 13 patients with myasthenia gravis and in 16 control subjects (six control patients with diaphragmatic weakness but not with myasthenia and ten normal subjects). The amplitude of diaphragm muscle action potentials was measured with surface electrodes during phrenic nerve stimulation at frequencies of 1-5 Hz for 3-4 seconds. RESULTS: In five patients with myasthenia gravis, a significant decrement (15-43% decrease) occurred in the amplitude of diaphragm muscle action potential during stimulation at 3 Hz. When stimulation frequency was reduced to 1 Hz, diaphragm muscle action potentials returned to their original amplitude within 4-5 seconds. The decrement in the amplitude of the diaphragm muscle action potential was reduced temporarily in three of four patients after the administration of intravenous edrophonium chloride (Tensilon). There was no significant change (< 10% decrease) in the amplitude of diaphragm muscle action potentials during stimulation at increased frequencies either in the 16 control subjects or in eight of the patients with myasthenia gravis. CONCLUSION: A significant reduction in the amplitude of diaphragm muscle action potential occurred in five of 13 patients with myasthenia gravis during phrenic nerve stimulation at 3 Hz but in none of the control subjects. This may be a useful and non-invasive method for identifying patients with myasthenia gravis in whom weakness of the diaphragm is suspected.
Full text
PDF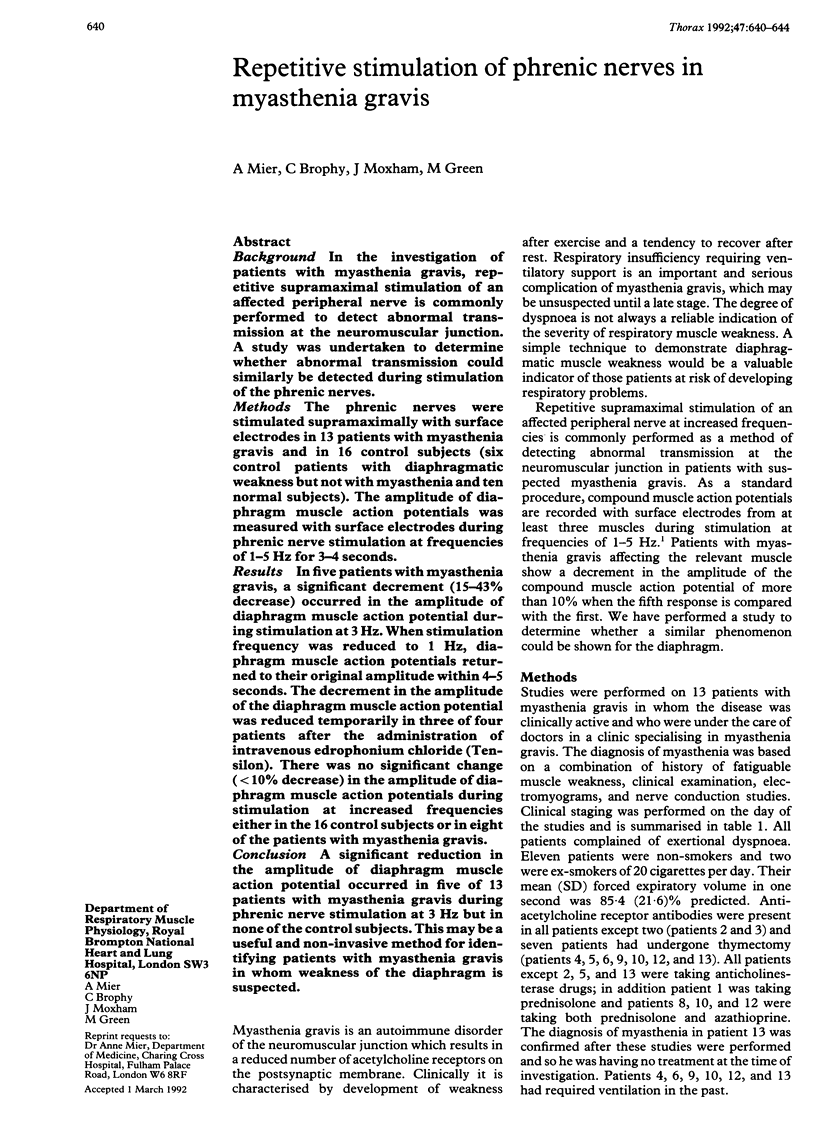


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- AGOSTONI E., RAHN H. Abdominal and thoracic pressures at different lung volumes. J Appl Physiol. 1960 Nov;15:1087–1092. doi: 10.1152/jappl.1960.15.6.1087. [DOI] [PubMed] [Google Scholar]
- Davis J. N. Phrenic nerve conduction in man. J Neurol Neurosurg Psychiatry. 1967 Oct;30(5):420–426. doi: 10.1136/jnnp.30.5.420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferguson I. T., Murphy R. P., Lascelles R. G. Ventilatory failure in myasthenia gravis. J Neurol Neurosurg Psychiatry. 1982 Mar;45(3):217–222. doi: 10.1136/jnnp.45.3.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGavin C. R., Artvinli M., Naoe H., McHardy G. J. Dyspnoea, disability, and distance walked: comparison of estimates of exercise performance in respiratory disease. Br Med J. 1978 Jul 22;2(6132):241–243. doi: 10.1136/bmj.2.6132.241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mier-Jedrzejowicz A., Brophy C., Moxham J., Green M. Assessment of diaphragm weakness. Am Rev Respir Dis. 1988 Apr;137(4):877–883. doi: 10.1164/ajrccm/137.4.877. [DOI] [PubMed] [Google Scholar]
- Miller J. M., Moxham J., Green M. The maximal sniff in the assessment of diaphragm function in man. Clin Sci (Lond) 1985 Jul;69(1):91–96. doi: 10.1042/cs0690091. [DOI] [PubMed] [Google Scholar]
- Ozdemir C., Young R. R. The results to be expected from electrical testing in the diagnosis of myasthenia gravis. Ann N Y Acad Sci. 1976;274:203–222. doi: 10.1111/j.1749-6632.1976.tb47686.x. [DOI] [PubMed] [Google Scholar]
- Perlo V. P., Poskanzer D. C., Schwab R. S., Viets H. R., Osserman K. E., Genkins G. Myasthenia gravis: evaluation of treatment in 1,355 patients. Neurology. 1966 May;16(5):431–439. doi: 10.1212/wnl.16.5.431. [DOI] [PubMed] [Google Scholar]
- SARNOFF S. J., SARNOFF L. C., WITTENBERGER J. L. Electrophrenic respiration. VII. The motor point of the phrenic nerve in relation to external stimulation. Surg Gynecol Obstet. 1951 Aug;93(2):190–196. [PubMed] [Google Scholar]



