Abstract
Introduction:
Cardiac patients are more prone to develop hemodynamic instability on induction of anesthesia and endotracheal intubation. The Airtraq® optical laryngoscope is a single-use rigid video laryngoscope that has been developed to facilitate tracheal intubation. There are limited studies comparing differences in the circulatory responses to Airtraq® and direct Macintosh larynngoscopy in cardiac patients.
Aim:
The purpose of our study was to evaluate whether there was clinically significant difference between the hemodynamic response to orotracheal intubation guided by either of the two devices (Airtraq® and Macintosh laryngoscopes) in patients who underwent coronary artery bypass grafting surgery.
Material and methods:
In this clinical study we analyzed the hemodynamic response to endotracheal intubation performed with Airtraq® or Macintosh laryngoscopes in patients who underwent elective coronary artery bypass graft surgery under general anesthesia.
Results:
We analyzed: blood pressure (systolic, diastolic, mean), heart rate and peripheral oxygen saturation (all notified before induction in anesthesia, immediately after induction, at the time of intubation and thereafter one and five minutes after intubation). We also recorded the maximal values of blood pressure and heart rate, as well as calculated the product of heart rate and systolic blood pressure. There were statistically significant differences in the hemodynamic response between the groups. At the time of intubation, there was significant inter-group difference in heart rate, systolic, diastolic and mean blood pressure. Endotracheal intubation with Macintosh laryngoscope was accompanied by significant increase in blood pressure and heart rate compared to Airtraq® group.
Conclusion:
The Airtraq® laryngoscope performed better than the Macintosh laryngoscope in terms of hemodynamic to the patient undergoing routine coronary artery bypass graft surgery.
Keywords: Airtraq® laryngoscope, Macintosh laryngoscope, Coronary Artery Bypass Graft Surgery, Hemodynamic response
1. INTRODUCTION
Laryngoscopy and endotracheal intubation are an integral part of general anesthesia for cardiac surgery (1). The hemodynamic response to the stress of laryngoscopy and endotracheal intubation does not present a problem for most patients (2). However, cardiac patients are more prone to develop hemodynamic instability on induction of anesthesia and endotracheal intubation and frequently respond to stress with an increase of blood pressure and heart rate (3). Such hemodynamic changes may alter the delicate balance between myocardial oxygen demand and supply and precipitate myocardial ischemia in patients with coronary artery disease (1).
Despite recent developments in airway device technologies, the curved laryngoscope blade described by Macintosh in 1943 remains the most popular device used to facilitate endotracheal intubation, both inside and outside the operating theatre, and constitutes the gold standard (4).
The Airtraq® optical laryngoscope (Prodol S.A., Vizcaya, Spain) is a single-use rigid video laryngoscope that has been developed to facilitate tracheal intubation in both, patients with normal or difficult to intubate airway (5-7). The resulting glottic view is provided without an alignment of the oral, pharyngeal and tracheal axes. The device can be completed with a wireless clip-on camera for external broadcast and teaching purposes.
There are limited studies comparing differences in the circulatory responses to Airtraq® and direct Macintosh laryngoscopy in cardiac patients (3). However, few studies in non-cardiac patients indicate the Airtraq® to generate more hemodynamic stability subsequent to the endotracheal intubation procedure and minor trauma as compared to the Macintosh laryngoscope (8).
The purpose of our study was to evaluate whether there was a clinically significant difference between the hemodynamic response to endotracheal intubation guided by either of the two devices (Airtraq® and Macintosh laryngoscopes) in patients who underwent coronary artery bypass grafting surgery (CABG).
2. MATERIAL AND METHODS
After getting authorization from our institutional ethical review board and written informed consent from all patients study was performed. Sixty consecutive adult cardiac surgery patients who underwent CABG operation and obtained general anesthesia with endotracheal intubation in our center were randomly assigned to either the Airtraq or conventional laryngoscopy using a Macintosh laryngoscope blade.
Inclusion criteria were: normal anatomical predictors for endotracheal intubation (Mallampati score I and II, thyreomental distance >6cm, mouth opening of more than >3cm, normal head and neck movement, American society of Anesthesiologists physical status (ASA) I to III were selected.
Exclusion criteria were: anatomic features predictive for difficult airway, history of reactive airway disease, morbid obesity (BMI >35 kg m-2), gastro-esophageal reflux, vital organ dysfunction, conduction abnormality, permanent pacemaker and emergency procedures. We also excluded the patients with failed first intubation attempt.
Patients were randomized either to the MacIntosh group or the Airtraq® group. Therefore, group labels were written on a total of 40 cards (20 per group). The cards were put into opaque envelopes, effectively mixed, and put into a box. This was done by a person who was not involved in the study. After entering the operation room, an envelope was picked from the box, opened and the patient was assigned to the indicated group. All anesthesiologists performing tracheal intubations were skilled for both techniques. After informed consent was received the patients were analyzed for baseline characteristics of included patients comprising demographic data and patients ASA status, ejection fraction (EF%), comorbidities, Mallampati score, thyromental distance in cm.
According to our institutional protocol pre-operatively all the patients were fasted adequately and were normothermic. Night before surgery and on the morning of surgery 90 minutes before induction of anesthesia patients were premedicated with Diazepam 5mg orally. All antihypertensive and antianginal medications were continued till the morning of surgery with the exception of angiotensin-converting enzyme inhibitors and angiotensin-receptors blockers. In the operation theatre standard monitoring was used in all patients, which included: six leads electrocardiography (ECG), invasive arterial pressure, and pulse oximetry, measurement of end-tidal carbon dioxide and volatile anaesthetics levels as well as entropy monitoring. The monitoring system we use is Dataex-Ohmeda F-CU8 instrumentarium – Helsinki Finland.
All patients received general anesthesia according to our institutional regimen. After 2 minutes of pre-oxigenation (100% oxygen 6l/min) anesthesia was induced with midazolam (0,25mg/kg), fentanyl (5-10 μg/kg), rocuronium bromide (0,6mg/kg). Following induction of anaesthesia all patients were manually ventilated with Sevoflurane (2,0-2,5%) in oxygen for 2min. Trachea was intubated if the depth of anesthesia as measured by the entropy showed below 50, by one anesthesiologist experienced in the use of the both laryngoscopes. Before intubation, the endotracheal tube was lubricated with 2% lignocaine gel and threaded over the intubating device. Thereafter, in all patients the lungs were mechanically ventilated with intermittent positive-pressure ventilation with FiO2 0,5, Vt 6-8ml/kg, respiratory rate 12-16 for the duration of the procedure. Anaesthesia was maintained with Sevoflurane (0,8-1,5%), fresh gas flow 2L/min of O2 : Air and continuous infusion of sufentanil (0,3-0,6 μg/kg/h). For each attempt when Airtraq® was used, a video system which incorporates a video camera that attaches to the Airtraq® device and a wireless monitor which receives the images were also used, therefore using the Airtraq® as a video laryngoscope. For all attempts using Macintosh laryngoscope, the standard non-styletted non-hockey stick tracheal tube conformation was utilized.
Hemodynamic data analyzed were: blood pressure (systolic (SBP), diastolic (DBP) and mean (MBP), heart rate (HR) and arterial oxyhemoglobin saturation (Sa02%). We analyzed the data at five different time points: before induction of anesthesia T0 (baseline), immediately after induction T1, at the time of intubation T2, one minute after intubation T3 and five minutes after intubation T4. We also calculated the rate-pressure product (RPP) at every point of time. The maximum values of BP and HR were also analyzed. The measured values were recorded by screenshots of the monitor in the operation room at the specific time points.
Statistical analysis
Statistical analysis was performed by using SPSS 17,0. Data were expressed as mean and ± standard deviation and statistically analyzed using Mann-Whitney U test and Shapiro –Wilk test. A value less than 0.05 was considered as statistically significant for all tests.
3. RESULTS
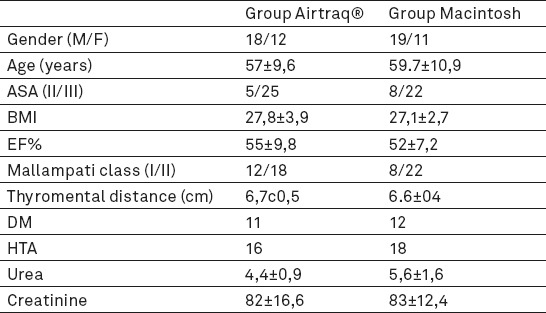
A total of 60 patients who fulfilled the inclusion criteria, were entered into the study. Thirty patients were intubated with Airtraq® laryngoscope, and thirty patients underwent tracheal intubation with Macintosh laryngoscope. The demographic data, BMI, ASA physical status classification, Mallampati class distribution, thyromental distance, EF%, incidence of hypertension, level of serum creatinine and urea were similar in both the groups (Table 1).
Table 1.
Patient demographic data and other details (mean ± SD). ASA- American society of Anesthesiologyst physical status, BMI- Body mass index, EF- Left ventricular ejection fraction, DM- Diabetes mellitus, HTA- Hypertension.
There were statistically significant differences in the hemodynamic response between the groups. Both the groups showed a reduction in arterial pressure after anesthetic induction but prior to laryngoscopy at T2, as a result of hemodynamic effects of the anesthetic drugs and loss of consciousness, but without significant difference between groups. At the time of intubation T3, there was significant inter-group difference in heart rate, systolic, diastolic and mean blood pressure (p<0.05). At the first minute after intubation T4 no significant difference in heart rate was observed between the two groups, but there was significant difference in systolic, diastolic and mean blood pressure between the groups (p<0.05). Heart rate returned to baseline within 5 min in both groups. Five minute after intubation T5 no significant difference was observed between groups, for heart rate, systolic, and mean blood pressure but there was statistically significant difference for diastolic blood pressure (p<0.05). Hemodynamic changes between groups are shown in Table 2.
Table 2.
Hemodynamic changes between groups. To – Baseline value, T1 – After induction in anesthesia, T2 – After intubation, T3 – 1min post intubation, T4 – 5min post intubation, HR- Heart rate, SBP – Systolic blood pressure, DBP – Diastolic blood pressure, MBP – Mean blood pressure, SaO2%–Peripheral oxygen saturation.

Blood pressure and heart rate were significantly higher in the Macintosh group than in the Airtraq® group.
There was no significant difference between the two groups (Airtraq® and Macintosh) in peripheral oxygen saturation during the observation period.
The calculated rate-pressure product at every point of time was statistically significant, at the time of intubation, one and five minute after intubation (p<0.05) (Figure 1).
Figure 1.
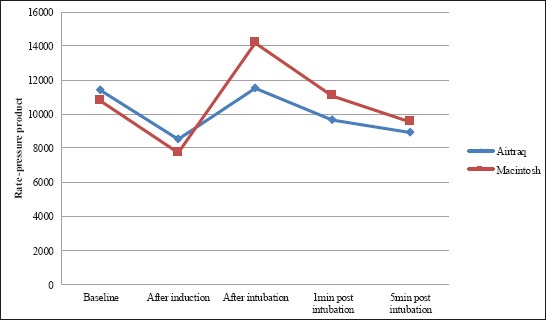
Rate-pressure product variation in the groups
4. DISCUSSION
Our findings demonstrate that the Airtraq® performed endotracheal intubation is better in term of hemodynamic stability compared with the Macintosh laryngoscope endotracheal intubation, in patient undergoing routine CABG surgery. Due to their underlying disease, these patients are at particular risk to develop peri-operative myocardial ischemia, due to an imbalance of myocardial oxygen supply and demand, as potentially induced by the procedure of endotracheal intubation, which can be associated with an increase in heart rate and arterial blood pressure (9-11).
We examined whether Airtraq® intubation attenuated hemodynamic responses to endotracheal intubation, compared with those that occurred with Macintosh laryngoscope. The results of this investigation suggest that Airtraq® do suppress the hemodynamic response to endotracheal intubation more than Macintosh laryngoscope. It is well known that the stimuli to airway structures are the main causes for circulatory responses to tracheal intubation (12). Laryngoscopy itself is one of the most invasive stimuli during endotracheal intubation (2, 13). Many anesthesiologists agree that a skilled anesthesiologist applies only a small force to the patient’s larynx when using a laryngoscope and that reducing the force on the larynx might prevent excessive hyperdynamic responses to endotracheal intubation (14-16). It is possible to separate the factors that contribute to the hemodynamic responses to endotracheal intubation (13). The first is the response to laryngoscopy and the second is the response to endotracheal intubation. Hemodynamic changes start within seconds of direct laryngoscopy, and there is a further increase in heart rate and blood pressure with passage of the tracheal tube. It is not known which component is more responsible for the hyperdynamic response to orotracheal intubation. We attempted to reduce the hyperdynamic responses to intubation by using Airtraq®. There was statistically significant difference in the cardiovascular variables between the Airtraq® and Macintosh groups.
Our results are confirmed by the variety of studies highlighting the usefulness of the Airtraq® in tracheal intubation (3, 7). Airtraq® resulted in less hemodynamic stimulation (heart rate and arterial blood pressure) post tracheal intubation compared to the Macintosh laryngoscope, in patients at low risk for difficult laryngoscopy and intubation (6, 7, 17-20). This finding probably reflects the fact that the Airtraq® requires reduced traction to lift the mandible [20,21] and provides a view of the glottis without the need to align the oral, pharyngeal and tracheal axes, and therefore requires less force to be applied during laryngoscopy (6). In addition, the passage of the tracheal tube through the vocal cords is atraumatic due to good glottis visualization and alignment of the tube to the axis of the trachea (20, 21). Other studies have demonstrated that tracheal tube insertion is the most invasive stimulus during the intubation manipulation (12, 13). Thus, the circulatory response to tracheal intubation may not be alleviated by avoiding laryngoscopic stimulation to the epiglottis and the base of the tongue unless the trachea is adequately pretreated with local anesthetic (12,22,23).
Singh et al. demonstrated in a comparison of 4 anesthetic induction agents, that stress response on conventional endotracheal intubation was most evident in patients with coronary artery disease when anesthesia was inducted with etomidate while midazolam was most effective in preventing intubation stress (24). In our study anesthesia was induced with midazolam. On the contrary although statistically significant, endotracheal intubation with the Airtraq® resulted in a clinically neglectable minimal increase in heart rate, while arterial blood pressure was not affected. Hence, the use of the Airtraq® device allowed maintaining stable hemodynamic conditions. Our results are confirmed by previously published data showing less hemodynamic alteration when endotracheal intubation is performed with the Airtraq®, compared to intubations with the Macintosh laryngoscope (21, 25). In a currently published meta-analysis Lu et al. concluded that the Airtraq® produces less hemodynamic stimulation, which may be an advantage in geriatrics or in patients with coronary heart disease or primary hypertension (26).
In the study of Maharaj et al. comparing Airtraq® and Macintosh, in which a near identical anesthetic technique to that used in this study was utilized, the same changes were seen in heart rate and blood pressure (6, 7, 21). In other study, comparing the GlideScope (Verathon Inc., Bothell, WA) to the laryngeal mask airway, in which also a near identical anesthetic technique to that used in this study was utilized, no changes in heart rate were seen, whereas blood pressure decreased slightly following tracheal intubation with both devices (27).
In the study of Schälte at al., Airtraq® was used for routine intubation in high risk cardio-surgical patients. Their findings demonstrate minimal but significant increase of the heart rate and decrease of mean arterial blood pressure one min after intubation. At four and five minutes after intubation, no significant changes in heart rate and MAP, compared to the baseline values could be detected. They concluded that the use of the Airtraq® allowed maintaining a stable hemodynamic situation. Compared to our study, they didn’t have control group and patients were anesthetized with sufentanil, etomidat and rocuronium (3).
Rate pressure product is an index of myocardial oxygen consumption (28), a value exciding 22,000 may be associated with myocardial ischemia (29). In our study, in both groups, the rate pressure product did not reach 22,000 at any point of time. Hence, both the Airtraq® and the Macintosh are safe to use in patients with ischemic heart disease.
A major limitation of this study is the relatively small sample size. Another limitation was that measurements and intervention were made without blinding of the researcher to the experimental group, which has the potential for bias. This study was carried out by an experienced user of each device. The results seen may be differing in the hand of less experienced users. Adequacy of muscle relaxation was not measured.
5. CONCLUSION
Conclusion our results demonstrate that routine endotracheal intubation using Airtraq® in patients undergoing routine CABG surgery can reduce hemodynamically changes and allow maintaining a stable hemodynamic situation, compared to the Macintosh laryngoscope. Further studies in this clinical context are necessary to confirm and extend these initial positive findings.
Acknowledgments
Assistance with the study: Gordana Taleska- writing assistance and Marija Jovanovski- Srceva general support.
Footnotes
CONFLICTS OF INTEREST: NONE DECLARED.
REFERENCES
- 1.Muralidhar K, Hema CN, Sanjay B, Keshava M, Murugesan C. Haemodynamic response to endotracheal intubation in coronary artery disease: Direct versus video laryngoscopy. Indian J Anaesth. 2011 May-Jun;55(3):260–265. doi: 10.4103/0019-5049.82673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kovak AL. Controlling the hemodynamic response to laryngoscopy and enfotracheal intubation. J Clin Anesth. 1996 Feb;8(1):63–79. doi: 10.1016/0952-8180(95)00147-6. [DOI] [PubMed] [Google Scholar]
- 3.Schälte G, Scheid U, Rex S, Coburn M, Fiedler B, Rossaint R, Zoremba N. The use of the Airtraq®optical laryngoscope for routine tracheal intubation in high-risk cardiosurgical patients. BMC Res Notes. 2011;4:425. doi: 10.1186/1756-0500-4-425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Macintosh RR. A new laryngoscope. Lancet. 1943;i:205. [Google Scholar]
- 5.Maharaj CH, Higgins BD, Harte BH, Laffey JG. Evaluation of intubation using the Airtraq or Macintosh laryngoscope by anaesthetists in easy and simulated difficult laryngoscopy - a manikin study. Anaesthesia. 2006;61:469–477. doi: 10.1111/j.1365-2044.2006.04547.x. [DOI] [PubMed] [Google Scholar]
- 6.Maharaj CH, O'Croinin D, Curley G, Harte BH, Laffey JG. A comparison of tracheal intubation using the Airtraq or the Macintosh laryngoscope in routine airway management: A randomised controlled clinical trial. Anaesthesia. 2006;61:1093–1099. doi: 10.1111/j.1365-2044.2006.04819.x. [DOI] [PubMed] [Google Scholar]
- 7.Maharaj CH, Costello JF, Harte BH, Laffey JG. Evaluation of the Airtraq and Macintosh laryngoscopes in patients at increased risk for difficult tracheal intubation. Anaesthesia. 2008;63:182–188. doi: 10.1111/j.1365-2044.2007.05316.x. [DOI] [PubMed] [Google Scholar]
- 8.Chalkeidis O, Kotsovolis G, Kalakonas A, Filippidou M, Triantafyllou C, Vaikos D, Koutsioumpas E. A comparison between the Airtraq and Macintosh laryngoscopes for routine airway management by experienced anesthesiologists: a randomized clinical trial. Acta Anaesthesiol Taiwan. 2010;48:15–20. doi: 10.1016/S1875-4597(10)60004-5. [DOI] [PubMed] [Google Scholar]
- 9.Landesberg G, Beattie WS, Mosseri M, Jaffe AS, et al. Perioperative myocardial infarction. Circulation. 2009;119:2936–2944. doi: 10.1161/CIRCULATIONAHA.108.828228. [DOI] [PubMed] [Google Scholar]
- 10.Modesti PA, Simonetti I, Olivo G. Perioperative myocardial infarction in non-cardiac surgery. Pathophysiology and clinical implications. Intern Emerg Med. 2006;1:77–86. doi: 10.1007/BF02934735. [DOI] [PubMed] [Google Scholar]
- 11.Friedrich A, Helmy T. Prevention of perioperative myocardial infarction. Int Anesthesiol Clin. 2009;47:13–36. doi: 10.1097/AIA.0b013e3181b6c303. [DOI] [PubMed] [Google Scholar]
- 12.Xue FS, Li CW, Liu KP, Sun HT, Zhang GH, Xu YC, Liu Y. Circulatory Responses to Fiberoptic Intubation in Anesthetized Children: A Comparison of Oral and Nasal Routes. Anesth Analg. 2007;104:283–288. doi: 10.1213/01.ane.0000253032.09962.e5. [DOI] [PubMed] [Google Scholar]
- 13.Adachi YU, Satomoto M, Higuchi H, Watanabe K. Fentanyl attenuates the hemodynamic response to endotracheal intubation more than the response to laryngoscopy. Anesth Analg. 2002 Jul;95(1):233–237. doi: 10.1097/00000539-200207000-00043. [DOI] [PubMed] [Google Scholar]
- 14.Bishop MJ, Harrington RM, Tencer AF. Force applied during tracheal intubation. Anesth Analg. 1992;74:411–414. doi: 10.1213/00000539-199203000-00016. [DOI] [PubMed] [Google Scholar]
- 15.Bucx MJ, Snijders CJ, Van Geel RT, et al. Forces acting on the maxillary incisor teeth during laryngoscopy using the Macintosh laryngoscope. Anaesthesia. 1994;49:1064–1070. doi: 10.1111/j.1365-2044.1994.tb04358.x. [DOI] [PubMed] [Google Scholar]
- 16.Tong JL, Ashworth DR, Smith JE. Cardiovascular responses following laryngoscope assisted, fibreoptic orotracheal intubation. Anaesthesia. 2005;60:754–758. doi: 10.1111/j.1365-2044.2005.04238.x. [DOI] [PubMed] [Google Scholar]
- 17.Tan PH, Yang LC, Shih HC, et al. Combined use of esmolol and nicardipine to blunt the haemodynamic changes following laryngoscopy and tracheal intubation. Anaesthesia. 2002;57:1207–1212. doi: 10.1046/j.1365-2044.2002.02624_4.x. [DOI] [PubMed] [Google Scholar]
- 18.Nathan N, Vandroux D, Benrhaiem M, et al. Low alfentanil target-concentrations improve hemodynamic and intubating conditions during induction with sevoflurane. Canadian Journal of Anaesthesia. 2004;51:382–387. doi: 10.1007/BF03018244. [DOI] [PubMed] [Google Scholar]
- 19.Montes FR, Giraldo JC, Betancur LA, et al. Endotracheal intubation with a lightwand or a laryngoscope results in similar hemodynamic variations in patients with coronary artery disease. Canadian Journal of Anaesthesia. 2003;50:824–828. doi: 10.1007/BF03019380. [DOI] [PubMed] [Google Scholar]
- 20.Maharaj CH, Buckley E, Harte BH, Laffey JG. Endotracheal intubation in patients with cervical spine immobilization: a comparison of Macintosh and Airtraq laryngoscopes. Anesthesiology. 2007;107:53–59. doi: 10.1097/01.anes.0000267529.71756.f0. [DOI] [PubMed] [Google Scholar]
- 21.Ndoko SK, Amathieu R, Tual L, Polliand C, Kamoun W, El Housseini L, Champault G, Dhonneur G. Tracheal intubation of morbidly obese patients: a randomized trial comparing performance of Macintosh and AirtraqTM laryngoscopes. British Journal of Anaesthesia. 2008;100(2):263–268. doi: 10.1093/bja/aem346. [DOI] [PubMed] [Google Scholar]
- 22.Latorre F, Hofmann M, Kleemann PP, Dick WF. Fiberoptic intubation and stress. Anaesthesist. 1993;42:423–426. [PubMed] [Google Scholar]
- 23.Hawkyard SJ, Morrison A, Doyle LA, et al. Attenuating the hypertensive response to laryngoscopy and endotracheal intubation using awake fibreoptic intubation. Acta Anaesthesiologica Scandinavica. 1992;36:1–4. doi: 10.1111/j.1399-6576.1992.tb03412.x. [DOI] [PubMed] [Google Scholar]
- 24.Singh R, Choudhury M, Kapoor PM, Kiran U. A randomized trial of anesthetic induction agents in patients with coronary artery disease and left ventricular dysfunction. Ann Card Anaesth. 2010;13(3):217–223. doi: 10.4103/0971-9784.69057. [DOI] [PubMed] [Google Scholar]
- 25.Gaszyński T, Gaszyński W. A comparison of the optical AirTraq and the standard Macintosh laryngoscope for endotracheal intubation in obese patients. Anestezjol Intens Ter. 2009;41:145–148. [PubMed] [Google Scholar]
- 26.Lu Y, Jiang H, Zhu YS. Airtraq laryngoscope versus conventional Macintosh laryngoscope: a systematic review and meta-analysis. Anaesthesia. 2011;66:1160–1167. doi: 10.1111/j.1365-2044.2011.06871.x. [DOI] [PubMed] [Google Scholar]
- 27.Fun WL, Lim Y, Teoh WH. Comparison of the GlideScope video laryngoscope vs. the intubating laryngeal mask for females with normal airways. European Journal of Anaesthesiology. 2007;24:486–491. doi: 10.1017/S0265021506002067. [DOI] [PubMed] [Google Scholar]
- 28.Gobel FL, Nordstrom LA, Nelson RR, Jorgensen CR, Wang Y. The rate- pressure product as an index of myocardial oxygen consumption during excercise in patients with angina pectoris. Circulation. 1978;57:549–556. doi: 10.1161/01.cir.57.3.549. [DOI] [PubMed] [Google Scholar]
- 29.Robinson BF. Relation of heart rate and systolic blood pressure to the onset of pain in angina pectoris. Circulation. 1967;35:1073–1083. doi: 10.1161/01.cir.35.6.1073. [DOI] [PubMed] [Google Scholar]


