Abstract
Introduction:
Among long term athletes there is always present hypertrophy of the left ventricle walls as well as increased cardiac mass. These changes are the result of the heart muscle adaptation to load during the years of training, which should not be considered as pathology. In people suffering from hypertrophic cardiomyopathy (HCM), there is also present hypertrophy of the left ventricle walls and increased mass of the heart, but these changes are the result of pathological changes in the heart caused by a genetic predisposition for the development HCM of. Differences between myocardial hypertrophy in athletes and HCM are not clearly differentiated and there are always dilemmas between pathological and physiological hypertrophy. The goal of the study is to determine and compare the echocardiographic cardiac parameters of longtime athletes to patients with hypertrophic cardiomyopathy.
Material and methods:
The study included 60 subjects divided into two groups: active athletes and people with hypertrophic cardiomyopathy.
Results:
Mean values of IVSd recorded in GB is IVSd=17.5 mm (n=20, 95% CI, 16.00–19.00 mm), while a significantly smaller mean value is recorded in GA, IVSd=10.0 mm (n=40, 95% CI, 9.00-11.00 mm). The mean value of the left ventricle in diastole (LVDd) recorded in the GA is LVDd=51 mm (n=40; 95% CI, 48.00 to 52.00 mm), while in the group with hypertrophic cardiomyopathy (GB) mean LVDd value is 42 mm (n=20; 95% CI, 40.00 to 48.00 mm). The mean value of the rear wall of the left ventricle (LVPWd) recorded in the GA is LVDd=10 mm (n=40; 95% CI, 9.00-10.00 mm) while in the group with hypertrophic cardiomyopathy (GB) mean LVDd is 14 mm (n=20; 95% CI, 12.00 to 16.00 mm). The mean of the left ventricle during systole (LVSD) observed in GA is LVSD=34 mm (n=40; 95% CI, 32.00 to 36.00 mm), while in the group with hypertrophic cardiomyopathy (GB) mean LVSD is 28 mm (n=20; 95% CI, 24.00 to 28.83 mm). The mean ejection fraction (EF%) observed in GA is EF=60% (n=40; 95% CI, 56.41 to 63.00%), while in the group with hypertrophic cardiomyopathy (GB) mean EF value is 69% (n=20; 95% CI, 62.00 to 70.83 mm). Somewhat higher mean diastolic left ventricular function (E/A) was observed in GA, E/A=1.76±0.15, and lower average values in the group with hypertrophic cardiomyopathy: (GB) E/A=0.78±0.02.
Conclusion:
Mean values of parameters intraventricular septum thickness in diastole (IVSd), the thickness of the rear wall of the left ventricle (LVPWd), the diameter of the left ventricle during systole (LVSD) were statistically different between groups of athletes (GA) compared to the group of patients with hypertrophic cardiomyopathy (GB).
Keywords: athlete’s heart, hypertrophic cardiomyopathy HCM
1. INTRODUCTION
In long term athletes there is always present hypertrophy of the left ventricle walls as well as increasing cardiac mass. These changes are the result of the heart muscle adaptation to load during the years of training, which should not be considered as pathology. In people suffering from hypertrophic cardiomyopathy (HCM), there is also present hypertrophy of the left ventricle walls and enlarged mass of the heart, but these changes are the result of pathological changes in the heart caused by a genetic predisposition for the development of (HCM). Differences between myocardial hypertrophy athletes and HCM are not clear and there are always dilemmas between pathological and physiological hypertrophy. Two-dimensional echocardiography allows to clearly differentiating pathological from physiological hypertrophy in athletes, which allow them continuation of sports activities without fear and the need for restrictions (1).
2. GOAL
This study goal is to determine and compare the echocardiographic cardiac parameters of the long term athletes and patients with hypertrophic cardiomyopathy. In addition, the goal is to establish the parameters that will certainly allow differentiation of morphological parameters which will enable creation of the protocol that can differentiate the physiological and pathological left ventricle hypertrophy.
3. MATERIAL AND METHODS
The study included 60 subjects divided into two groups: Group A (GA, n=40): active sportsmen and Group B (GB, n=20): patients with hypertrophic cardiomyopathy. All patients completed a survey (personal data, sports and family history, and history of disease), anthropometric measurements, clinical examination, measurement of the ACP and the SFO, ECG, and echocardiography. Echocardiographic examination of all respondents was performed by the specialist in internal medicine, cardiologist-specialized in ultrasonography. Two-dimensional and M mode Doppler echocardiogram was performed on echocardiography machine made by General Electric Medical System Logiq 5 Expert. Assessed are the following parameters: intraventricular septum in diastole (IVSd), the left ventricle during diastole (LVD), the rear wall of the left ventricle during diastole (LVPWd), intraventricular septum in systole (IVSs), the left ventricle during systole (LVs), the back wall of the left ventricle during systole (LVPWs), ejection fraction (EF), fractional shortening (FS), left ventricular diastolic function (E/A). The parameters were monitored in standard position (lying on the back) and were same for all respondents in order to avoid measurement errors. Listed normal values of the above echocardiogram parameters are in accordance to the American Society of Echocardiography. Statistical analysis is performed in the statistical program Med Calc for Windows, version 12.2.1.0. (MedCalc Software, Mariakerke, Belgium). Results are presented as mean with 95% confidence interval (CI 95%). Mann Whitney and Student’s t test were used. The values of these tests with value of p<0.05 are accepted as statistically significant.
4. RESULTS
The average value of systolic blood pressure (SBP–mmHg) for each group was as follows: GA: 115.8±7.2 and GB: 146.5±1-7mmHg. Average values of DCM (mmHg) per group were as follows: GA: 74.2±8.1; GB: 88.7±5,7mmHg. Average values of the SFO (strokes/min) were: GA: 59.4±11.6; GB: 73.1±7.8. Average values of echocardiographic parameters in a group of athletes were: 10.0±2.0mm IVSd; LVDd 50.4±5,6mm; LVPWd 9.8±1.4mm; LVSD 34.0±4,7mm; EF 61.0±7.5%; FS 34.0±7.58%; E 0.65±0.37; A 0.374±0.393 and E/A 1.76±0.15. In patients with HCM values were: 18.3±3,7mm IVSd; LVDd 43.55±8,0mm; LVPWd 14.5±3,4mm; LVSD 27.7±6.0mm; EF 65.4±8.5%; FS 38.25±0.96%; E 0.68±0.363; A 0.87±0.404 and E/A 0.78±0.02. Reference values for the parameters of ultrasound for athlete’s heart are: IVSd (mm) = ≤11 (sensitivity: 90; specificity: 39.4), LVDd ≤52 = (67.5, 52.1), PWD (mm) ≤ 10 = (75; 57.4) and LVSD (mm) ≤ 36 (70; 51.1). Limit values for the parameters of ultrasound for hypertrophic cardiomyopathy are: IVSd (mm) ≥13 (100; 96.5), LVDd ≤ 43 (65; 93), PWD (mm) ≥ 12 (65; 96) and LVSD (mm) ≤ 29 (80; 90.4).
Figure 1 show that mean IVSd recorded in GB IVSd=17.5 mm (n=20, 95% CI, 16.00 to 19.00 mm), was significantly higher than mean values in GA, IVSd=10.0 mm (n=40; 95% CI, 9.00-11.00 mm). There are statistically significant differences between the values recorded in the group of athletes (GA) in relation to the group of patients with hypertrophic cardiomyopathy (GB) U=3.00, Z=6.255, p <0.0001.
Figure 1.
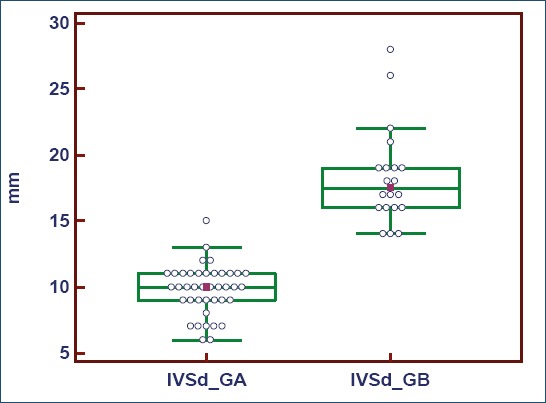
The intraventricular septum in diastole (IVSd)
Figure 2 present the mean size of the left ventricle during diastole (LVDd) recorded in the GA which is LVDd=51 mm (n=40; 95% CI, 48.00 to 52.00 mm), while in the group with hypertrophic cardiomyopathy (GB) mean LVDd is 42mm (n=20; 95% CI, 40.00 to 48.00 mm). There was a statistically significant difference between the values recorded in the group of athletes (GA) compared to the group of patients with hypertrophic cardiomyopathy (GB) U=192.00, Z=3.263, p=0.0011.
Figure 2.
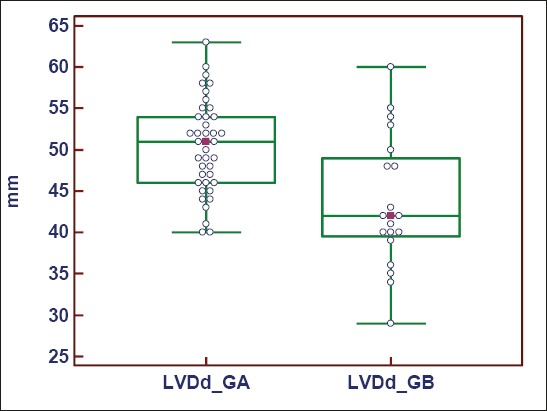
The diameter of the left ventricle during diastole (LVDd)
Mean value of the back wall of the left ventricle (LVPWd) recorded in the GA is LVDd=10 mm (n=40; 95% CI, 9.00-10.00 mm) while in the group with hypertrophic cardiomyopathy (GB) mean LVDd is 14 mm (n=20, 95% CI, 12.00 to 16.00 mm). There was a statistically significant difference between the values obtained in the group of athletes (GA) compared to the group of patients with hypertrophic cardiomyopathy (GB) U=58.50, Z= 5.412, p<0.0001 (Figure 3).
Figure 3.
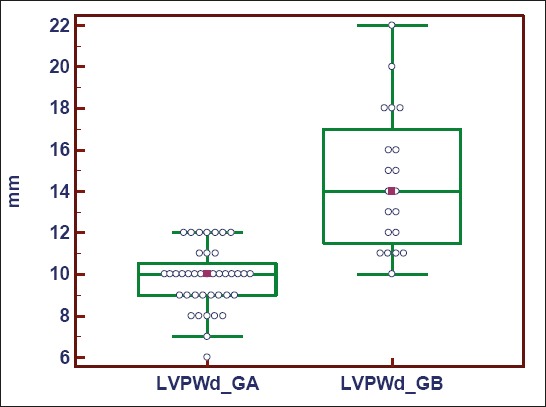
The thickness of the rear wall of the left ventricle (LVPWd)
The mean values of the left ventricle diameter during systole (LVSD) observed in GA is LVSD=34 mm (n=40; 95% CI, 32.00 to 36.00 mm), while in the group with hypertrophic cardiomyopathy (GB) mean LVSD is 28 mm (n=20, 95% CI, 24.00 to 28.83 mm). There was a statistically significant difference between the values obtained in the group of athletes (GA) compared to the group of patients with hypotrophic cardiomyopathy (GB) U=150.00, Z=3.923, p=0.0001 (Figure 4).
Figure 4.
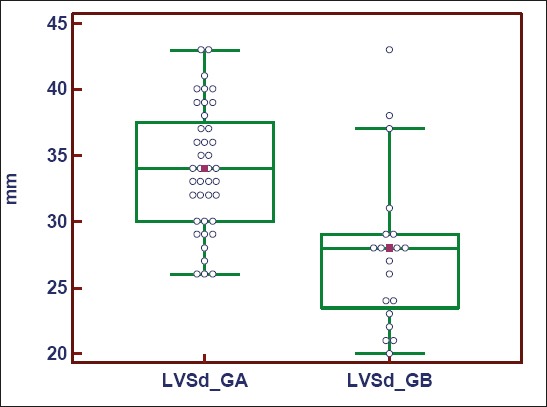
The diameter of the left ventricle during systole (LVSD)
The mean ejection fraction (EF%) observed in GA is EF=60% (n=40; 95% CI, 56.41 to 63.00%), while in the group with hypertrophic cardiomyopathy (GB) mean value of EF is 69% (n=20, 95% CI, 62.00 to 70.83 mm). There was a statistically significant difference between the values obtained by the group of athletes (GA) compared to the group of patients with hypertrophic cardiomyopathy (GB) U=222.00, Z=1.982, p=0.0474 (Figure 5).
Figure 5.
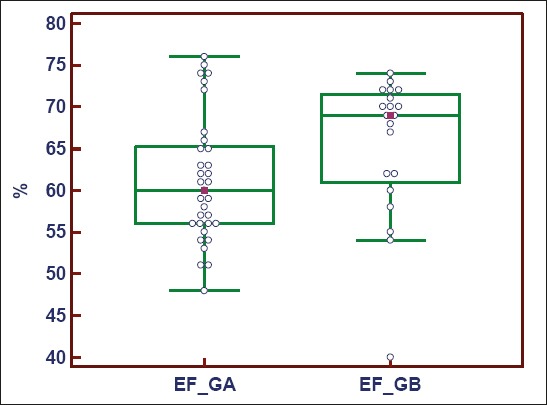
The ejection fraction mean
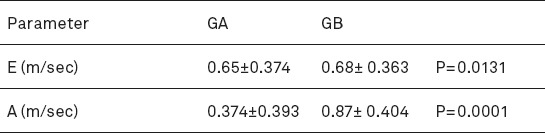
Diastolic function of the left ventricle (E/A) is calculated as the ratio of early diastolic filling (E) and atrial contraction (A).
Somewhat higher mean diastolic left ventricular function (E/A) is observed in GA, E/A=1.76 ± 0.15, while the lower mean in the group with hypertrophic cardiomyopathy (GB) E/A=0.78 ± 0.02. There was a statistically significant difference between the values obtained in the group of athletes (GA) than in patients with hypertrophic cardiomyopathy (GB) (p = 0.0001) (Table 1).
Table 1.
Diastolic function of the left ventricle (E/A)
5. DISCUSSION
Long-term training leads to changes in the heart that are called “athlete’s heart syndrome”. Diagnostics and problems of the athlete’s heart represent big challenge because of its morphological, functional and electrical physiological changes, which can range between physiological and pathological conditions. Evaluation of the athlete’s heart has always been a scientific conflict between those who consider it a physiological adaptation, highly efficient and healthy heart, and those who consider it sick heart, or at least state that borders with the pathological (1-3). Pluim et al. in 2000 published the results of a meta-analysis of cardiac structure and function of the athlete’s heart which compiled a total of 59 studies with data from the 1451 athletes. Echocardiographic parameters (LVDd, IVSd, LVPWd) are presented for the athletes (n=1451) and were recorded the following values: LVDd (52.1 to 56.2 mm), IVSd (10.5 to 11.8 mm), LVPWd (10.3 to 11.0 mm) (4). Our findings can be compared with the results of this meta-analysis. One of the goals of a meta-analysis was to detect differences between the impact of sports which require strength and endurance, and dynamic and static sports to cardiac adaptation. The group of authors from Italy (Caso et al.) published a paper in 2006 which defined the parameters that need to be analyzed and monitored in order to be able to distinguish between hypertrophic cardiomyopathy (HCM) and the athlete’s heart (5). The authors point out that there is a problem in misdiagnosis while both states can be simultaneously present in some patients. HCM is a genetic disease. In the general population 0.2% of the population (one affected among 500 citizens), and is the most common cause of sudden unexpected cardiac death in the young people in the United States, including the active athletes. HCM is idiopathic myocardial disorder which is characterized by hypertrophy, but without increase in the left ventricle, without any cardiac or systemic reasons that may be responsible for hypertrophy. The authors cite a well-known clinical signs associated with HCM as follows: HCM in the family history, followed by clinical symptoms that have minimal importance because the athletes are generally asymptomatic and clinical history only in a few cases syncope have occurred, palpitations, abdominal chest and dyspnea on exertion (5). Hypertrophic cardiomyopathy (HCM) is a rare but potentially fatal disease (6). The sudden death in young athletes is a dramatic event that has a significant social impact (7). HCM is one of the leading causes of sudden death and is associated with one-third of all sudden deaths (8). Because of this differentiation of HCM from non pathological athlete’s heart is very important (9). Echocardiography plays an important role in the differential diagnosis, but there is considerable overlap between both these states and their distinction remains a challenge (10,11,12). Mansencal and colleagues in 2007 published the results of echocardiography screening on professional tennis players (13). The survey was conducted during the French Open in 2004, and it includes a total of 160 participants: 80 athletes who are professional tennis players (50 men and 30 women) and a control matched group (by age and sex) to healthy volunteers (n=80). Left ventricular hypertrophy was detected in 18 men (36%) and 6 women (20%) among professional tennis players, while in the control group was observed in only two men (4%) and no women. The difference was statistically significant in both groups (p<0.0001 and p=0.02). In the group of tennis players (n=50) measurement results were as follows: IVSd (9.9±1mm), LVDd (54±3.5 mm) LVPWD (10±1.5 mm) and in the control group of men (n=50) measurement results were as follows: IVSd (8.5±1.3 mm), LVDd (52.2±3.3 mm) LVPWD (8.5±1.5 mm). Differences between these parameters were statistically significant (p<0.05). Since the “athlete’s hearth” syndrome only partly derive from the training, the two studies showed significant heritability in thickening the rear wall of the left ventricle, so that myocardial changes in athletes can be partially of genetic origin. Some studies revealed the significant association between left ventricular mass and genetic polymorphisms, such as the renin-angiotensin system. Possible genetic associations in the heart of the athletes should be investigated in the future because newer non-invasive techniques have allowed exploration of myocardial metabolism in athletes. For example, Pluim and colleagues applied the magnetic resonance spectroscopy and found that strength training is not associated with pathological changes in the myocardium due to the high energy of the phosphate metabolism (2). Finally, although it was confirmed that the athlete’s heart is a physiological change, there are some opinions that the intensive training can lead to the development of malignant ventricular arrhythmias and that training may be associated with sudden death, but that the possible endogenous role of aid (doping) cannot be completely excluded (14). Also, the fact that the heart remains increased after the end of training in many athletes is subject of the increased interest in this topic (14).
6. CONCLUSION
Mean values of parameters: intraventricular septum thickness in diastole (IVSd), the thickness of the rear wall of the left ventricle (LVPWd), the diameter of the left ventricle during systole (LVSD) were statistically different between groups of athletes (GA) compared to the group of patients with hypertrophic cardiomyopathy (GB). In the group of athletes were recorded lower values than in the group with hypertrophic cardiomyopathy. Mean values of the left ventricle diameter during diastole (LVDd) were statistically different between groups of athletes (GA) compared to the group of patients with hypotrophic cardiomyopathy (GB). In the group of athletes were recorded higher values in relation to the group with hypertrophic cardiomyopathy. Mean values of fractional shortening (FS%) were statistically significantly different between groups of athletes (GA) compared to the group of patients with hypertrophic cardiomyopathy (GD), in a manner that in a group of athletes were recorded lower values. Mean values of diastolic dysfunction left ventricular E/A were statistically different between groups of athletes (GA) compared to the group with hypertrophic cardiomyopathy, as in a group of athletes were recorded higher values of diastolic function of the left ventricle.
Footnotes
CONFLICT OF INTEREST: NONE DECLARED
REFERENCES
- 1.Fagard RH. Impact of different sports and training on cardiac structure and function. Cardiology Clinics. 1997;15:397–412. doi: 10.1016/s0733-8651(05)70348-9. [DOI] [PubMed] [Google Scholar]
- 2.Pluim BM, Zwinderman AH, van der Laarse A, et al. The athlete’s heart. A meta analysis of cardiac structure and function. Circulation. 1999;100:336–344. doi: 10.1161/01.cir.101.3.336. [DOI] [PubMed] [Google Scholar]
- 3.Pelliccia A, Maron BJ, et al. An echocardiographic assessment of cardiac morphology and common ECG findings in teenege professional soccer players: reference renges for use in screening Heart. 2001;85:649–654. doi: 10.1136/heart.85.6.649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pluim BM, Zwinderman AH, van der Laarse A, van der Wall EE. The Athlete’s Heart: A Meta-Analysis of Cardiac Structure and Function. Circulation. 2000;101:336–344. doi: 10.1161/01.cir.101.3.336. [DOI] [PubMed] [Google Scholar]
- 5.D'Andrea A, Limongelli G, Caso P, Sarubbi B, Della Pietra A, Brancaccio P, et al. Association between left ventricular structure and cardiac performance during effort in two morphological forms of athlete’s heart. Int J Cardiol. 2002;86:177–184. doi: 10.1016/s0167-5273(02)00194-8. [DOI] [PubMed] [Google Scholar]
- 6.Nienaber CA, Hiller S, Spielmann RP, Geiger M, Kuck KH. Syncope in hypertrophic cardiomyopathy: multivariate analysis of prognostic determinance. J Am Coll Cardiol. 1990;15:948–955. doi: 10.1016/0735-1097(90)90222-b. [DOI] [PubMed] [Google Scholar]
- 7.Maron BJ. Sudden death in young athletes. N Engl J Med. 2003;349:1064–1075. doi: 10.1056/NEJMra022783. [DOI] [PubMed] [Google Scholar]
- 8.Maron BJ, Shirani J, Poliac LC, et al. Sudden death in young competitive athletes. Clinical, demographic, and pathological profiles. JAMA. 1996;276:199–204. [PubMed] [Google Scholar]
- 9.Corrado D, Pelliccia A, Bjørnstad HH, et al. Cardiovascular pre-participation screening of young competitive athletes for prevention of sudden death: Proposal for a common European protocol. Consensus Statement of the Study Group of Sport Cardiology of the Working Group of Cardiac Rehabilitation and Exercise Physiology and the Working Group of Myocardial and Pericardial Diseases of the European Society of Cardiology. Eur Heart J. 2005;26:516–524. doi: 10.1093/eurheartj/ehi108. [DOI] [PubMed] [Google Scholar]
- 10.Stout M. Athlete’s heart and echocardiography: Athlete’s heart. Echocardiography. 2008;25:749–754. doi: 10.1111/j.1540-8175.2008.00670.x. [DOI] [PubMed] [Google Scholar]
- 11.Maron BJ. Distinguishing hypertrophic cardiomyopathy from athlete’s heart: A clinical problem of increasing magnitude and significance. Heart. 2005;91:1380–1382. doi: 10.1136/hrt.2005.060962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mansencal N, Marcadet DM, Martin F, Montalvan B, Dubourg O. Echocardiographic characteristics of professional tennis players at the Roland Garros French open. Am Heart J. 2007;154:527–531. doi: 10.1016/j.ahj.2007.04.056. [DOI] [PubMed] [Google Scholar]
- 13.Deligiannis A, Bjoirnstad H, Carrc F, et al. ESC Study Group of Sports Cardiology position paper on adverse cardiovascular efects of doping in athletes. Eur J Cardiovasc Prev Rehabil. 2006;13:687–694. doi: 10.1097/01.hjr.0000224482.95597.7a. [DOI] [PubMed] [Google Scholar]
- 14.Maron B, Peliccia A. The heart of trained athletes;cardiac remodeling and the risk of sports, including sudden death Circulation. 2006;114:1633–1644. doi: 10.1161/CIRCULATIONAHA.106.613562. [DOI] [PubMed] [Google Scholar]


