Abstract
Aim:
This study sought to assess whether the volume and osmolarity of contrast media (CM) influences the occurrence of contrast induced nephropathy (CIN) following coronarography procedure. CIN can be defined as an increase in the serum concentration of creatinine greater than a 25% from baseline during the period of 12 to 48 hours after the administration of radiocontrast media.
Material and methods:
We examined 100 patients without diabetes with serum creatinine concentration from 45 mmol/l to 141 mmol/l and 100 patients with diabetes with serum creatinine concentration from 46 mmol/l to 161 mmol/l who underwent coronary angiography. During procedure they received iso-osmolar contrast medium, Visipaque 320 (iodixanol-320), for group without diabetes from 40 to 340 ml and for group with diabetes from 49 to 310 ml.
Results:
CIN occurred in 27 (13,5%) of the 200 study patients. There was a trend toward higher prevalence of CIN (16% vs.11%, p = 0.086) in the diabetic group compared with the non-diabetic group. Patient with diabetes received less contrast media, they are younger but number patients with CIN are higher.
Conclusion:
Increasing contrast media dose is associated with the occurrence of CIN following coronarography. But, another risk factors like diabetes mellitus, old age, male sex and preexisting kidney disease have influence of developing CIN after coronarography.
Keywords: contrast media, contrast induced nephropathy, coronarography
1. INTRODUCTION
The use of iodine-based radio-contrast media are necessary during coronarography for visualization of coronary artery. Contrast media have direct toxic effects on renal tubular cells causing vacuolization and altered mitochondrial function, Also, it seems that mechanisms which mediated by nitric oxide and prostaglandin induced vasodilatation (1, 2). Hemodynamic changes of renal blood flow, which causes hypoxia in the renal medulla and direct toxic effects of contrast media on renal cells, are thought to contribute to the pathogenesis of contrast induced nephropathy (CIN). CIN can be defined as an increase in the serum concentration of creatinine greater than a 25% from baseline during the period of 12 to 48 hours after the administration of radiocontrast media. The incidence of CIN is estimated to be 1-2% (3, 4). However, the risk for developing CIN may be as high as 50% in some patient subgroups, such as those with diabetes mellitus and pre-existing renal impairment. Some patients are asymptomatic and elevation of creatinine returns to normal within 3 to 5 days. But, minority of patients may have symptoms like: anuria, mineral disbalance, hypotension or hypertension and they may require hemodialysis. Some radiologist reported that volumes of low osmolarity contrast media (iohexol or iopamidol) greater than 100 mL were associated with markedly increased incidence of contrast nephropathy (5mL/kg strongly predict nephropathy requiring dialysis) (5).
The route of administration contrast is also important, with contrast media being more nephrotoxic when administered intraarterially. This effect is thought to be due to the fact that the acute intrarenal concentration of contrast media is much higher after intraarterial rather than IV injection (6). The way of administration contrast has influence on CIN. To compare the incidence of contrast-induced nephropathy (CIN) and vascular complications in patients undergoing cardiac catheterization using traditional manual contrast injection techniques and automated contrast injector show that using automated contrast injectors resulted in a significant decrease in vascular and renal complications (7). The osmolarity of the contrast media plays an important role: the use of an low osmolarity contrast media reduces the risk of nephropathy in high-risk patients compared with the use of high osmolarity contrast media (8, 9).
2. PATIENTS AND METHODS
In this prospective clinic study we examined 100 patients without diabetes with serum creatinine concentration from 45 mmol/l to 141 mmol/l and 100 patients with diabetes with serum creatinine concentration from 46 mmol/l to 161 mmol/l who underwent coronary angiography. During procedure they received iso-osmolar contrast medium, Visipague iodixanol, using automated contrast injectors (Figure 1). The group of patients without diabetes (n=100) received from 40 to 340 ml and group of patients with diabetes (n=100) from 49 to 310 ml of contrast. Serum creatinine concentration was obtained 24 h and 48 h after contrast media administration. Increase of 25 % of serum creatinine after 48 hours was defined as contrast induced nephropathy (Figure 2).
Figure 1.

Automated contrast injector (UKC Sarajevo)
Figure 2.
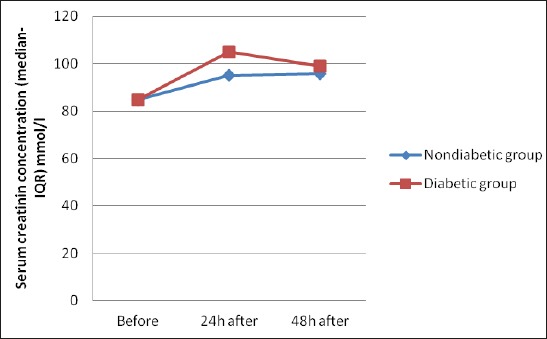
Creatinin before, 24 and 48 after coronarografy for groups.
3. RESULTS
Results are presented by tables and figures.
Amount of contrast during coronarography show significant more (p =0.0413) contrast for group without diabetes mellitus.
Serum creatinine concentration 48 hours after coronarography was significant higher in group with diabetes (p =0.0005) than group without diabetes (p=0.0317).
4. DISCUSSION
In this study the total amount of iso-osmolar contrast medium, Visipaque 320 (iodixanol-320), was significantly higher in the nondiabetic group than diabetic group (157,86 ml vs. 149,15 ml; p=0,0413) (Table 1). Some institution show that the mean volume of CM for coronary angiography was 130 ml, and for percutaneous coronary intervention was 191 ml (10). Serum creatinine concentration 48 hours after coronarography was significant higher in group with diabetes (p =0.0005) than group without diabetes (p=0.0317) (Table 2). Contrast induced nephropathy occurred in 27 (13,5%) of the 200 study patients. There was a trend toward higher prevalence of CIN (16% vs.11%, p = 0.086) in the diabetic group compared with the non-diabetic group (Table 3 and 4). The study of Laskey W and all shows that the overall rate of CIN in patients with chronic kidney disease and DM undergoing coronary angiographic procedures was 10.5% (11).
Table 1.
Amount of contrast during coronarografy for diabetic and nondiabetic group. IQR = interkvartalni raspon, p<0.05 prema Mann-Whitnijevom testu.
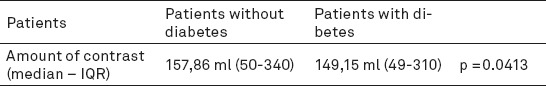
Table 2.
Dinamic of creatinin before, 24 and 48 after coronarography for groups
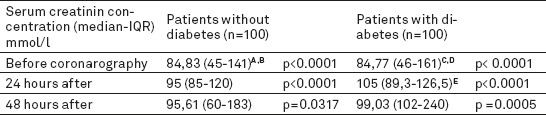
Table 3.
Patients characteristics in diabetic group with CIN after coronarografy
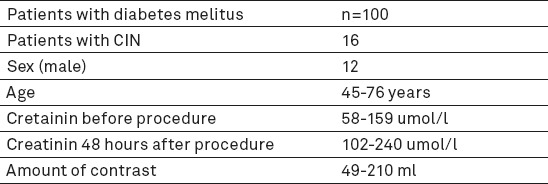
Table 4.
Patients characteristics in non diabetic group with CIN after coronarografy
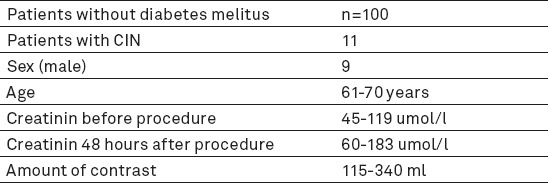
Patient with CIN characteristics are shown in Tables 1, 2 and 3. The reason for CIN are not only contrast media. Patient with diabetes received less contrast media, they are younger but number patients with CIN are higher. Age, sex, preexisting serum creatinine concentration and diabetes are also reasons for CIN during coronarography.
5. CONCLUSION
The volume, the osmolality and the route of contrast medium administration are associated with the occurrence of CIN following coronarography (procedure-related risk factors). But another risk like diabetes mellitus, old age, male sex and preexisting kidney disease have influence of developing CIN after coronarography (patient-related factors).
Footnotes
CONFLICT OF INTEREST: NONE DECLARED.
REFERENCES
- 1.Wongand GTC, Irwin MG. Contrast induced nephropathy. Br J Anaesth. 2007;99(4):474–483. doi: 10.1093/bja/aem237. [DOI] [PubMed] [Google Scholar]
- 2.Jorgensen AL. Contrast-Induced Nephropathy: Pathophysiology and Preventive Strategies. Critical Care Nurse. 2013;33(1):37–47. doi: 10.4037/ccn2013680. [DOI] [PubMed] [Google Scholar]
- 3.Benko A, Fraser M, Magner P, Capusten B, Barret B, Myers A, et al. Canadian Association of Radiologists: Consesus Guidelines for the Prevention of Contrast- Induced nephropathy. Can J Assoc Radiol. 2011;58(2):79–87. [PubMed] [Google Scholar]
- 4.Weisbord SD, Palevsky PM. Strategies for the prevention of contrast-induced acute kidney injury. Curr Opin Nephrol Hypertens. 2010;19(6):539–549. doi: 10.1097/MNH.0b013e32833d42e3. [DOI] [PubMed] [Google Scholar]
- 5.Lewington A, Kanagasundaram S. Renal Association Clinical Practice Guidelines on acute kidney injury. Nephron Clin Pract. 2011;118(Suppl1):c349–c390. doi: 10.1159/000328075. [DOI] [PubMed] [Google Scholar]
- 6.Dong M, Jiao Z, Liu T, Guo F, Li G. Effect of administration route on the renal safety of contrast agents: a meta-analysis of randomized controlled trials. J Nephrol. 2012;25(3):290–301. doi: 10.5301/jn.5000067. [DOI] [PubMed] [Google Scholar]
- 7.Godley RW, Joshi K, Breall JA. A comparasion of the use of traditional hand injection versus automated injectors during cardiac catheterisation. J Invasive Cardiol. 2012;24(12):628–630. [PubMed] [Google Scholar]
- 8.From AM, Al Badarin FJ, McDonald FS, Bartholmai BJ, Cha SS, Rihal CS. Iodixanol versus low-osmolar contrast media for prevention of contrast induced nephropathy: meta-analysis of randomized, controlled trials. Circ Cardiovasc Interv. 2010;3(4):351–358. doi: 10.1161/CIRCINTERVENTIONS.109.917070. [DOI] [PubMed] [Google Scholar]
- 9.Heinrich MC, Häberle L, Müller V, Bautz W, Uder M. Nephrotoxicity of iso-osmolar iodixanol compared with nonionic low-osmolar contrast media: meta-analysis of randomized controlled trials. Radiology. 2009;250(1):68–86. doi: 10.1148/radiol.2501080833. [DOI] [PubMed] [Google Scholar]
- 10.Tombach B, Bremer C, Reimer P. Renal tolerance of a neutral gadolinium chelate (gadobutrol) in patients with chronic renal failure: results of a randomized study. Radiology. 2001;218:651–657. doi: 10.1148/radiology.218.3.r01mr12651. [DOI] [PubMed] [Google Scholar]
- 11.Laskey W, Aspelin P, Davidson C, Rudnick M, Aubry P, Kumar S, et al. Nephrotoxicity of iodixanol versus iopamidol in patients with chronic kidney disease and diabetes mellitus undergoing coronary angiographic procedures. Am Heart J. 2009;158(5):822–828. doi: 10.1016/j.ahj.2009.08.016. [DOI] [PubMed] [Google Scholar]


