Abstract
Completion of the Human Papillomavirus (HPV) vaccine series is a national priority. This study not only identified correlates of intent to complete the vaccine series and actual series completion, but also tested the efficacy of a DVD intervention to promote series completion. Women’s beliefs that all three doses reduced cancer risk predicted intent and completion. Intention predicted completion, as did the belief that having a friend accompany the woman would promote completion. Beyond these effects, women assigned to the intervention were 2.44 times more likely than women in the control group to complete the series. Thus, in controlled analyses, a theory-grounded DVD intervention successfully promoted HPV series completion in a community setting. This method of intervention has high translational potential.
Keywords: Human Papillomavirus vaccination, cervical cancer, Appalachia, randomized controlled trial
Vaccination against the Human Papillomavirus (HPV), the most common sexually-transmitted infection, is a primary prevention strategy to protect women against cervical cancer (CDC, 2012). Annually, cervical cancer affects approximately 12,000 women in the United States and results in death for another 4,200 women (ACS, 2012). Women residing in rural and other medically underserved communities are disproportionately burdened by cervical cancer incidence and mortality (Freeman & Wingrove, 2005). Despite the fact that these women stand to benefit most from HPV vaccination, evidence suggests that HPV vaccination diffusion in the United States has been inequitable, HPV vaccination goals are not being met, and adherence to the full regimen is sub-optimal (Dorell, Stokley, Yankey, & Markowitz, 2011; Williams et al., 2012). Importantly, clinical evidence supporting vaccine efficacy to prevent HPV infection, pre-cancerous cervical lesions, and cervical cancer is based on completion of the entire three-dose regimen (Markowitz et al., 2007).
Young women 18–26 years old should be considered a priority population for HPV vaccination, considering their vaccination rates lag behind that of adolescent females. Whereas the national vaccination rate for adolescent females aged 13–17 is 48.7% (Dorell et al., 2012), vaccination rates for young women are estimated at 21% (Williams et al., 2012); regional variation in uptake ranges from 9% to 49% (Dempsey, Cohn, Dalton, & Ruffin, 2011). The few regional studies reporting three-dose completion rates indicate that rates range from as low as 2% to high as 47%, with disparities observed among African Americans, rural women, those covered by public insurance, and females living in educationally-disadvantaged neighborhoods (Chao, Velicer, Slezak, & Jacobsen, 2009; Crosby, Casey, Vanderpool, Collins, & Moore, 2011; Dempsey et al., 2011). For women completing all three doses, many fail to complete the series within the six-month protocol (Dempsey et al., 2011).
Lack of vaccination in young women represents a missed opportunity, given that this age group is burdened by the higest prevalence rate of HPV infection among all age groups (Dunne, Unger, & Sternberg, 2007). Many of these young women were not affored opportunities to receive the vaccine as adolescents and were not targeted by pharmaceutical companies’ marketing campaigns (Jain et al., 2009). Finally, these women do not qualify for the Vaccines for Children program and are often under- or uninsured, making them responsible for substanial out-of-pocket healthcare costs (Dempsey et al., 2011; Jain et al., 2009).
To date, much of the HPV vaccination-related research has solely focused on identifying predictors of vaccine acceptability, intent to vaccinate, and/or vaccine initiation without examining adherence to the full dosing schedule (Allen et al., 2010; Brewer et al., 2011; Bynum, Brandt, Sharpe, Williams, & Kerr, 2011; Chao, Velicer, Slezak, & Jacobsen, 2010; Lechuga, Swain, & Weinhardt, 2011; Reiter, 2009; Teitelman et al., 2011; Katz et al., 2010; Vanderpool, Casey, & Crosby, 2011). Past research examined different theories of health behavior as explanatory for variation in HPV vaccine acceptance. For example, Allen and colleagues (2009) used the transtheoretical model (Prochaska, 2008) to assess the stage of adoption of the HPV vaccine, the theory of reasoned action (Ajzen & Fishbein, 1980), and social cognitive theory (Bandura, 2004) to explain barriers to vaccine uptake. Constructs from the health belief model (Rosenstock, 1974) have also been reported extensively in the HPV vaccination literature (Allen et al., 2009; Bennett, Buchanan, & Adams, 2012; Brewer & Fazekas, 2007; Gerend & Shepherd, 2012; Katz et al., 2010; Krawczyk et al., 2012a; Krawczyk et al., 2012b; Teitelman et al., 2011).
In particular, the theory of planned behavior (TPB; Ajzen & Fishbein, 1980) has successfully predicted HPV vaccination intentions and vaccine uptake (Bennett et al., 2012; Gerend & Shepherd, 2012). This theory suggests that constructs such as attitude toward the behavior, subjective norms, perceived behavioral control, and intention to perform the behavior are the primary mechanisms for behavior change, including adherence (Ajzen & Fishbein, 1980; Bennett et al., 2012). Specifically, the subjective norms construct has received a great deal of attention in the HPV vaccine-related literature as a predictor of intention to vaccinate, as well as vaccine uptake (Allen et al., 2010; Bennett et al., 2012; Gerend & Shepherd, 2012; Juraskova et al., 2011; Kahn, Rosenthal, Hamann, & Bernstein, 2003; Krawczyk et al., 2012b; Teitelman et al., 2011).
Beyond understanding the theoretical underpinnings of a health behavior, there is value in developing interventions based on previous assessments of the target population. Consider the women who reside in the mountainous region of Appalachian Kentucky in the United States. These women shoulder a disproportionate burden of cervical cancer while also experiencing poor socioeconomic conditions, lower Pap testing rates, geographic isolation, and limited access to healthcare (ARC, 2008; Hopenhayn, King, Christian, Huang, & Christian, 2008; Huang et al., 2002; Wingo et al., 2008). From 2005–2009, the five-year cervical cancer incidence rate in this region was notably higher than the rest of the country (9.85 per 100,000 vs. 8.0, respectively; KCR, 2012; NCI, 2012). Cervical cancer mortality rates are 45% higher in Appalachian Kentucky (KCR, 2012; NCI, 2012). Approximately one in five women in eastern Kentucky has not had a Pap test in the past three years (KDPH, 2008). The majority of counties in Appalachian Kentucky are designated as healthcare professional shortage areas (HRSA, 2012), and all but three counties are considered distressed or at-risk by the Appalachian Regional Commission on the basis of federal unemployment, income, and poverty indicators (ARC, 2012).
There is substantial need to address cervical cancer prevention in this rural, medically underserved population. In response, we conducted multiple quantitative and qualitative studies related to HPV vaccination behaviors. Our first effort involved recruiting 495 young women in Appalachian Kentucky into a women’s health study (Crosby et al., 2011; Mills, Vanderpool, & Crosby, 2011; Vanderpool et al., 2011; Vanderpool, Crosby, Casey, & Bates, 2010). The HPV vaccine was offered at no cost. Young women 18–26 years of age were provided with vouchers for the full series and were encouraged to initiate the series in the clinic upon enrollment. Of 246 women recruited from rural health clinics, only 45% initiated dose one. Furthermore, only 14% of those who received dose one returned for dose two, and only 5% received dose three (Crosby et al., 2011). Through this work, we learned that access and free vaccination were not sufficient to help women overcome barriers to series completion. Our qualitative research suggested that young rural women report barriers to vaccination, including normative social influences (especially maternal and peer), insufficient knowledge, negative (even stigmatized) or ambivalent attitudes toward vaccination, questions concerning vaccine safety and efficacy, and barriers such as cost and anticipated vaccine pain (Cohen et al., in press; Head & Cohen, 2012; Mills, Head, & Vanderpool, in press).
Because of the cervical cancer burden and low rates of HPV vaccination in Appalachian Kentucky, as well as the fact that there have been few health communication studies that have assessed variables predicting completion of all three HPV vaccine doses among young women (Allen et al., 2010; Chao, Slezak, Coleman, & Jacobsen, 2009; Dempsey et al., 2011; Katz et al., 2010) or intervened on full series completion, we designed a randomized controlled trial to test a theory-grounded intervention targeted to the unique needs of this rural population of young women. Accordingly, the purpose of this study was twofold. First, the study used the TPB to identify correlates of positive intent to complete the three-dose series and actual series completion among a sample of women, ages 18–26, residing in Appalachian Kentucky. We hypothesized that women intending to complete the series, as well as actually completing all three doses, would be more likely to a) have supportive HPV vaccination attitudes, b) have norms supporting vaccine completion, and c) report perceived behavioral control beliefs favoring series completion. We also hypothesized that positive intention to complete the three-dose series would predict adherence to the full vaccine regimen. Second, and more importantly, the study tested the efficacy of a field-based DVD communication intervention designed to promote series completion. We hypothesized that women randomized to the DVD-arm would be significantly more likely than those receiving standard-of-care to complete the vaccine series, even after controlling for baseline level of intent to complete the series as well as controlling for other predictor variables corresponding with the TPB.
Method
Participants and Processes
In order to deliver an intervention immediately following the first dose of a vaccine and conduct a randomized trial of vaccine completion, it is necessary to begin with a population being newly vaccinated with dose one. From 2010–2011, we launched a social marketing campaign informed by Rogers’ (1995) diffusion of innovations designed to promote uptake of the first HPV vaccine dose (Cohen et al., in press). The social marketing campaign targeted young women from an eight-county catchment area of Appalachian Kentucky in the United States by promoting the availability of free HPV vaccines for 18–26 year old women. Research nurses provided free vaccination (dose one) at local health departments, medical clinics, community colleges, outdoor festivals, Wal-Mart stores, businesses, and women’s homes. To be eligible to receive dose one, women had to be 18–26 years old, not be pregnant, not previously vaccinated against HPV, and not have had prior vaccine reactions that prevented HPV vaccination. All vaccinated women received a standard-of-care pamphlet about the risks and benefits of the vaccine published by the Centers for Disease Control and Prevention.
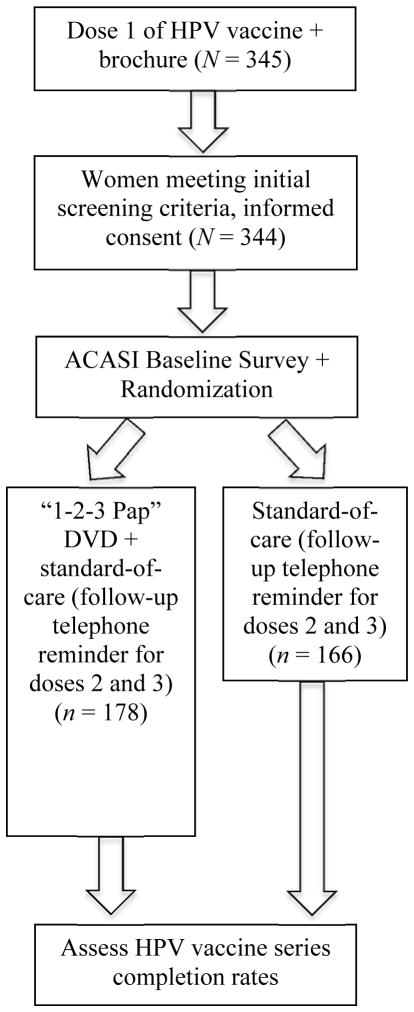
Following uptake of dose one, women were asked to participate in a research study (see Figure 1 for study design). All women agreed to participate. Three primary reasons explain this success: The women received dose one of the vaccine for free; the research nurses were from the women’s community; and women received a free t-shirt as part of the social marketing campaign. In essence, the research nurses’ small overture to participate in a research study was viewed favorably by our study participants. After providing written informed consent, women were asked to complete a baseline survey using audio-computer-assisted self-interviewing (ACASI) administered on a laptop computer. Intervention or comparison group allocations were assigned at the end of the ACASI using a random number sequence. Investigators and research nurses in the field were blinded to the allocation sequence. All research activities were approved by the University of Kentucky Institutional Review Board, including compensating women with $25 gift cards upon baseline survey completion.
Figure 1.
“1-2-3 Pap” Communication Intervention Study Design
Intervention
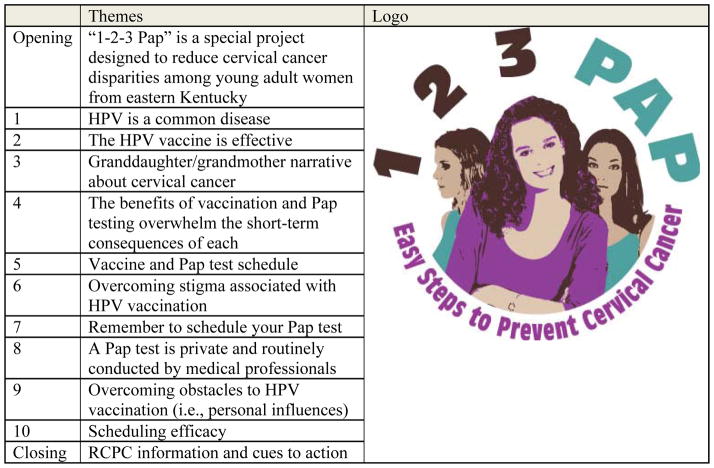
Women randomized to the intervention arm watched a 13-minute educational DVD, entitled “1-2-3 Pap,” from a laptop computer, using stereo headphones. Design and development of the DVD was guided by the information, motivation, behavioral skills model (IMB; Fisher & Fisher, 2002), which has been widely used in HIV prevention projects (Fisher & Fisher, 2002), and more recently, improving adherence to health recommendations (Ferrer, Morrow, Fisher, & Fisher, 2010). The IMB was developed as a well-validated, comprehensive framework for integrating commonly used health behavior constructs into a single model for message design. The IMB specifies a three-phase process for intervention development, including eliciting the information, motivation, and skills factors important to the target behavior. Accordingly, DVD content was based on formative research with young women from Appalachian Kentucky regarding their HPV vaccination and Pap testing behavior (Cohen et al., in press). The resultant intervention design included specific health information relevant to the target health behavior and specific to the population; personal motivation and normative cues; and skills training to increase efficacy (Fisher, Fisher, & Harman, 2003). Specifically, the content of the DVD included risks of HPV and HPV-related harm, encouraged women to consider the benefits of vaccination and Pap tests, informed patients about the necessity to complete the vaccine series, motivated series completion, enhanced self-efficacy for series completion, and helped women overcome personal obstacles to series completion. The DVD was organized into 10 broad message segments (see Figure 2 for thematic overview) and included a roughly one-minute opening and closing with cues to action delivered by a local Appalachian, young female TV news reporter. The DVD footage also featured young women (proscriptive models), a nurse practitioner, and a physician, all of whom were from the target community. The young women and healthcare providers discussed eastern Kentucky cervical cancer statistics, HPV infection and its relation to cervical cancer, HPV vaccination, and Pap testing. It used a mixture of video footage, narrative and informational content sequences, still shots, and written captions. Recording and editing occurred at a local studio.
Figure 2.
1-2-3 Pap Themes and Logo
Study Measures
The baseline survey was informed by previous research (Brewer & Fazekas, 2007; Crosby et al., 2011; Crosby, Schoenberg, Hopenhayn, Moore, & Melhan, 2007) and included specific questions addressing TPB constructs. Wording of survey items and their response options are listed in Table 1. These measures were initially used to identify TPB correlates of positive intent to complete the three-dose vaccine series, as well as actual series completion. These measures were also controlled for during analysis assessing the intervention effect on series completion. Women’s vaccination dates and series completion were tracked by medical record review for up to nine months past the initial vaccine dose. This article includes all records that were complete according to study protocol by June 30, 2012; additional medical record review and checking for data completion and accuracy will continue.
Table 1.
Study Measures
| Construct | Survey Question | Response Options |
|---|---|---|
| Attitudes | Do you feel that HPV vaccinations will help some women prevent pain, possibly even death by preventing cervical cancer? | 6 point agreement scale; DK, Refusal, N/A |
| I feel that if I get all three shots of the HPV vaccine that I will decrease my chances of getting cervical cancer. | 5 point agreement scale; DK, Refusal, N/A | |
| Do you feel that HPV vaccinations will reduce the number of cases of cervical cancer? | 6 point agreement scale; DK, Refusal, N/A | |
|
| ||
| Subjective Norms | Have any of your friends been vaccinated against HPV? | Yes, No, DK, Refusal, N/A |
| Do you have friends who have failed to take doses 2 and 3? | Yes, No, DK, Refusal, N/A | |
| I would be much more likely to get dose 2 and dose 3 of the vaccine if my father encouraged me to do so. | 5 point agreement scale; DK, Refusal, N/A | |
| I would be much more likely to get dose 2 and dose 3 of the vaccine if my mother encouraged me to do so. | 5 point agreement scale; DK, Refusal, N/A | |
| I would be much more likely to get dose 2 and dose 3 of the vaccine if a friend went with me. | 5 point agreement scale; DK, Refusal, N/A | |
|
| ||
| Perceived Behavioral Control | Would childcare prevent you from getting dose 2 and 3? | Yes, No, DK, Refusal, N/A |
| Would your work schedule prevent you from getting dose 2 and 3? | Yes, No, DK, Refusal, N/A | |
| Would transportation prevent you from getting doses 2 and 3? | Yes, No, DK, Refusal, N/A | |
| I would be much more likely to get dose 2 and dose 3 of the vaccine if a health care provider called to remind me. | 5 point agreement scale; DK, Refusal, N/A | |
| I would not get dose 2 and dose 3 of the vaccine if I had to make a special appointment. | 5 point agreement scale; DK, Refusal, N/A | |
|
| ||
| Intention | Do you intend to get all three HPV vaccine shots? | Yes, No, DK, Refusal, N/A |
Note. DK=don’t know; N/A=not applicable.
Don’t know, refusal, and not applicable responses were recoded as missing.
Data Analysis
For the first purpose of the study, continuous TPB correlates of young women’s intent to complete the vaccine series were evaluated by using independent groups t tests at the bivariate level. Next, dichotomous TPB correlates of intent, as well as two control variables (whether women reported ever having had penile-vaginal sex and whether they had ever been told they had an abnormal Pap test) were evaluated using chi-square tests at the bivariate level. Subsequently, a hierarchical logistic regression model was constructed using two blocks. The first block contained the two control variables if determined significant at p ≤. 10. The second block used a forward stepwise entry procedure to test all TPB continuous and dichotomous correlates significant at a screening level of p ≤. 10 at the bivariate level for their independent association with intent. At the multivariate level, significance was established by 95% confidence intervals and their respective p values.
For the second purpose of the study, the same bivariate procedures used in the cross-sectional study of intent were applied to vaccine series completion. Subsequently, a hierarchical logistic regression model was constructed using three blocks. The first block contained the two control variables if determined significant at p ≤. 10, in addition to containing intent as a predictor variable. The second block used a forward stepwise entry procedure as before and contained TPB continuous and dichotomous variables significant at a screening level of p ≤. 10 in the bivariate analysis. The third block contained only the independent variable (intervention vs. control). Multivariate significance was established by 95% confidence intervals and their respective p values. All analyses were conducted using SPSS version 19.0.
Results
From 2010–2011, 345 women received dose one of the HPV vaccine through the social marketing campaign. Subsequent to receiving the vaccine, 100% of the women agreed to participate in the randomized controlled trial; one woman agreed to participate, but did not have time to participate in the survey/passively refused to complete the survey. The final sample for analysis was 344 women. The mean age was 22 years (SD = 2.4); the sample was primarily non-Hispanic White (94%), reflecting 2010 Census data for this region (Center, 2012). Ninety percent of the women had lived in southeastern Kentucky for over five years. Only one-quarter (25.6%) were employed full-time; however, almost half (48.0%) reported some college as their highest level of education. Thirty percent of the women were married and 39.0% reported having children at home. The sample was sexually experienced, with 93.9% reporting they had ever had penile-vaginal sex; half the sample (49.3%) reported current birth control use. Almost half of the women (46.0%) reported ever having an abnormal Pap test, 21.8% had been told by a medical provider that they have a sexually-transmitted disease, and 15.7% had been told they have HPV.1
Positive intent to complete the vaccine series was indicated by 64.3% of the women (n = 220). Just over one-third (37.8%) of the sample completed the three-dose series. Randomization produced roughly equivalent sized groups, with 178 (51.7%) randomized to the intervention condition and 166 (48.3%) randomized to the standard-of-care condition. Of note, randomization did not yield equivalence regarding intent. Positive intent was indicated by 58.2% of those randomized to the intervention condition and 70.9% in the control condition (p = .014). Nearly half of the women (43.3%) randomized to the DVD intervention completed the three-dose series, whereas 31.9% of women assigned to the comparison group completed the series, for a percent relative difference of 35.7% (p = .03).
Bivariate Findings
Table 2 displays the bivariate findings from the cross-sectional study of positive intent; there were no differences by group assignment for any of the continuous-level or dichotomous correlates (data not shown). As hypothesized, the majority of assessed TPB correlates were significantly associated with intent (p ≤. 10), each in the anticipated direction. For example, women with positive intent to complete the vaccine series were more likely to agree that getting all three doses of the HPV vaccine would decrease their chance of getting cervical cancer (i.e., supportive vaccine attitudes). Likewise, women with positive intent were less likely to report childcare, transportation, and work as barriers to series completion. However, inconsistent with our supportive norms hypothesis, women with positive intent were less likely to agree with statements that their mother and father encouraged vaccination. The control variables, history of an abnormal Pap (p = .001) and having had previous sexual intercourse (p = .001), were both significantly associated with positive intent to complete the vaccine series (data not shown).
Table 2.
Correlates of Positive Intent to Complete the Three-Dose HPV Vaccine Series (N = 344)
| Mean among those with negative intent | Mean among those with positive intent | t | p value | |
|---|---|---|---|---|
| Continuous-level Correlatesa | ||||
| 3 doses decreases my cervical cancer riskb | 2.33 | 0.99 | 9.50 | .0001 |
| Vaccine prevents cervical cancer pain and deathc | 2.05 | 1.78 | 2.29 | .02 |
| HPV vaccine will reduce number of cervical cancer casesc | 2.11 | 1.26 | 7.77 | .0001 |
| Provider phone call reminder helpfulb | 2.12 | 1.28 | 5.62 | .0001 |
| Would not return if special appointmentb | 2.72 | 2.87 | 1.24 | .22 |
| Would return if friend came with meb | 2.84 | 2.36 | 3.56 | .0001 |
| Father encourages vaccine completionb | 1.27 | 1.77 | 2.59 | .01 |
| Mother encourages vaccine completionb | 1.06 | 1.40 | 3.82 | .0001 |
| Dichotomous Correlatesd | % Negative intent | % Positive intent | p value | |
| Childcare would prevent return | ||||
| Yes | 68.2+ | 31.8 | .001 | |
| No | 33.4 | 66.6 | ||
| Transportation issues would prevent return | ||||
| Yes | 54.5+ | 45.5− | .0001 | |
| No | 29.7 | 70.3 | ||
| Work schedule would not prevent return | ||||
| Yes | 62.5+ | 37.5− | .0001 | |
| No | 24.2− | 75.8+ | ||
| Friends have been vaccinated | ||||
| Yes | 38.9 | 61.1 | .50 | |
| No | 42.8 | 57.2 | ||
| Friends failed to complete full vaccine series | ||||
| Yes | 36.1 | 63.9 | 1.00 | |
| No | 36.1 | 63.9 | ||
Lower scores represent greater agreement with the statement
5 point agreement scale
6 point agreement scale
+ represents significantly higher frequencies based on standardized residual (≥2 or ≤ −2); - represents significantly lower frequencies based on standardized residual (≥2 or ≤ −2).
Table 3 displays the bivariate findings for actual vaccine series completion. As shown, five of eight TPB predictors assessed at the continuous level were significantly associated with series completion (p ≤. 10). For example, women who completed the vaccine series were more likely to agree that the HPV vaccine will reduce the number of cervical cancer case (i.e., supportive vaccine attitudes). Two dichotomous variables, transportation and work schedule, achieved significance as would be expected; in other words, those who did not complete the vaccine series were more likely to report that these barriers would prevent their return for subsequent doses. Inconsistent with our subjective norms hypothesis, however, neither father encouragement to complete the vaccine series nor peer vaccination behaviors were significantly correlated with series completion. Of the two control variables, history of an abnormal Pap was significantly correlated with series completion (p = .03), while history of previous sexual intercourse was not (p = .664; data not shown).
Table 3.
Correlates of Vaccine Series Completion (N = 344)
| Mean for series non-completers | Mean for series completers | t | p value | |
|---|---|---|---|---|
| Continuous-level Correlatesa | ||||
| 3 doses decrease my cervical cancer risk a | 1.72 | 0.95 | 5.85 | .0001 |
| Vaccine prevents cervical cancer pain and deathc | 1.90 | 1.84 | .54 | .59 |
| HPV vaccine will reduce number of cervical cancer casesc | 1.74 | 1.27 | 4.82 | .001 |
| Provider phone call reminder helpfulb | 1.74 | 1.33 | 2.83 | .005 |
| Would not return if special appointmentb | 2.79 | 2.88 | .76 | .44 |
| Would return if friend came with meb | 2.72 | 2.22 | 3.70 | .001 |
| Father encourages vaccine completionb | 1.57 | 1.65 | .54 | .59 |
| Mother encourages vaccine completionb | 1.19 | 1.42 | 1.75 | .08 |
| Dichotomous Correlatesd | % series incomplete | % series complete | p value | |
| Childcare would prevent return | ||||
| Yes | 60.9 | 39.1 | .870 | |
| No | 62.6 | 37.4 | ||
| Transportation issues would prevent return | ||||
| Yes | 78.5 | 21.5− | .001 | |
| No | 57.0 | 43.0 | ||
| Work schedule would prevent return | ||||
| Yes | 78.1+ | 21.9− | .001 | |
| No | 55.7 | 44.3 | ||
| Friends have been vaccinated | ||||
| Yes | 66.4 | 33.6 | .78 | |
| No | 68.0 | 32.0 | ||
| Friends failed to complete full vaccine series | ||||
| Yes | 69.4 | 30.6 | .39 | |
| No | 62.1 | 37.9 | ||
Lower scores represent greater agreement with the statement
5 point agreement scale
6 point agreement scale
+ represents significantly higher frequencies based on standardized residual (≥2 or ≤ −2); - represents significantly lower frequencies based on standardized residual (≥2 or ≤ −2).
Multivariate Findings
Table 4 displays the results of the two-block model regressing intent on the assessed correlates. The model fit the data well, χ2 (8) = 135.32, p = .001. As shown, of the two control variables that were forced into block one, both the experience of ever having an abnormal Pap test result (p = .002) and having had previous sexual intercourse (p = .026) were significantly associated with intent. Six of the correlates retained multivariate significance in block two, and each was associated with intent in the anticipated direction, with the exception of father encouragement, which was consistent with the bivariate findings.
Table 4.
Multivariate Findings for Positive Intent to Complete the Vaccine Series (N = 308)
| AORa | 95% CI | p value | |
|---|---|---|---|
| Correlate | |||
| Sexually experienced | 6.62 | 1.61–34.48 | .026 |
| Ever had abnormal Pap test result | 3.05 | 1.53–6.06 | .002 |
| 3 doses decreases my cervical cancer risk | 1.42 | 1.09–1.87 | .011 |
| HPV vaccine will reduce number of cervical cancer cases | 1.75 | 1.23–2.50 | .002 |
| Would return with provider phone call | 1.40 | 1.09–1.81 | .009 |
| Father encourages vaccine completion | 0.72 | 0.54–0.95 | .019 |
| Work schedule would not prevent return | 3.97 | 2.07–7.60 | .001 |
| Childcare would not prevent return | 5.94 | 1.54–22.89 | .010 |
Note. AOR=adjusted odds ratio; CI=confidence interval.
Odds ratio adjusted for all other variables in the model
Table 5 displays the results of the three-block model regressing series completion on the predictor variables assessed at baseline. The model fit the data well, χ2 (5) =52.97, p = .001. As hypothesized, positive intent was a strong predictor of series completion, with those indicating positive intent being about 2.1 times more likely to complete the series (p = .016). The one control variable, ever having an abnormal Pap test result, failed to achieve multivariate significance despite being forced into block one. Only two of the variables entered in block two achieved multivariate significance. Women indicating a belief that all three doses would reduce their risk of cervical cancer were 1.5 times more likely to complete the series than those not having this attitude (p = .001). Also, women indicating that they would be more likely to complete the series if a friend went with them were about 1.5 times more likely to complete the series than those not indicating this facilitating factor (p = .011). Most importantly, women randomized to the intervention were 2.44 times more likely to complete the vaccine series than those assigned to the standard-of-care condition (p = .001).
Table 5.
Multivariate Findings for Completion of Vaccine Series (N = 336)
| AORa | 95% CI | p value | |
|---|---|---|---|
| Predictor Variable | |||
| Ever had abnormal Pap test result | 1.20 | 0.73–1.99 | .466 |
| Intend to complete the series | 2.07 | 1.15–3.76 | .016 |
| Would return if friend came with me | 1.29 | 1.06–1.56 | .011 |
| 3 doses decreases my cervical cancer risk | 1.49 | 1.18–1.87 | .001 |
| Randomized to intervention condition | 2.44 | 1.47–4.05 | .001 |
Note. AOR=adjusted odds ratio; CI=confidence interval.
Odds ratio adjusted for all other variables in the model
Discussion
To our knowledge, this is the first communication intervention trial to promote completion of the three-dose HPV vaccine series in a community setting. Previous intervention studies have focused exclusively on college students’ HPV vaccine knowledge, intentions, and initiation using different educational approaches (Hopfer, 2012; Krawczyk et al., 2012a; Leonard, Kola, & Walsh, 2011). Alternatively, our DVD-based intervention to improve vaccine adherence was conducted in a real-world setting, using nurse providers working in a challenging social-cultural environment.
As posited by the TPB, intention was a strong predictor of completing the three-dose vaccine regimen among this sample of Appalachian Kentucky women. Previous research suggests that intention is the strongest correlate of HPV vaccination uptake among young women (Gerend & Shepherd, 2012; Juraskova et al., 2011). Although intention is a meaningful predictor of health behavior, it often falls short in fully explaining behavioral outcomes (Armitage & Conner, 2001; Webb & Sheeran, 2006). Beyond intention to vaccinate, our data demonstrate that a field-based DVD intervention can have an equally strong effect on future behavior. In essence, the effect of the DVD was robust given that the model was constructed to preferentially allow a large number of other variables to explain the variance in series completion. Although this study is the first to examine the outcome of adherence, this effect size is consistent with the findings of Hopfer’s (2012) “combined” peer-expert video intervention in improving vaccine acceptance.
Impressively, 31.9% of the comparison group achieved series completion while only receiving standard-of-care procedures, including an informational HPV vaccine brochure and reminder telephone calls for doses 2 and 3. This vaccine series completion rate is lower than Chao and colleagues’ (2009) research in southern California (47.1%); however, women in that study were followed over a two-year period and were part of a managed care insurance plan with a large network of primary care providers. The rate in our study is substantially higher than Dempsey et al.’s (2011) research in Michigan (10%) among 19–26 year old women and the previous Crosby et al. (2011) study (clinic-recruited sample 4.5%), which was conducted with a similar population of medically underserved women in Appalachian Kentucky. Our findings may serve as an example for practitioners in medically underserved communities. Specifically, working with manufacturer reimbursement programs to provide vaccines at low or no cost and following standard-of-care procedures that include follow-up phone call reminders and community-based vaccination clinics can optimize HPV vaccination adherence rates.
The bivariate data predicting intention to vaccinate were intriguing. These data partially supported two TPB-related hypotheses examining intent to complete the series outcome: positive attitudes toward HPV vaccination and access to care barriers (as viewed through the lens of perceived behavioral control). One unique finding was the inverse relationship between parental encouragement and intention to vaccinate. One possible explanation is that because these women had already received dose one, their reported belief that a parent did not encourage vaccination actually strengthened their existing intention to complete the full dosing regimen (a possible reactance effect; Brehm & Brehm, 1981).
Additionally, in the multivariate model, women reporting the experience of an abnormal Pap test were three times as likely to report positive intent to complete the vaccine series, suggesting these women may experience increased perceived susceptibility to cervical cancer and desire to take proactive steps to prevent the disease. Clinicians should consider an abnormal Pap test as an opportunity to educate young women about the benefits of the HPV vaccine (Kepka, Berkowitz, Yabroff, Roland, & Saraiya, 2012). Believing that three doses of the vaccine reduces personal cervical cancer risk and reduces incidence of cervical cancer was also predictive of positive intent to complete the vaccine series in the final model. Similarly, lack of scheduling barriers predicted positive intent. These data suggest the benefits of including vaccine efficacy data related to the prevention of pre-cancerous cervical lesions and cervical cancer, as well as strategies for overcoming common barriers to vaccination in persuasive messages.
Bivariate data were mixed in offering support of our hypotheses relative to predicting series completion. Although having a friend accompany the woman for subsequent doses and favorable perceptions of vaccine efficacy significantly predicted completion, perceptions of paternal encouragement and peer vaccination behaviors were not significant. As expected, barriers of transportation and work schedule were significantly associated with series completion; however, the barrier of childcare was not.
The final multivariate model did not support parental influence or peer behaviors as significant predictors of series completion. Several studies have suggested that normative social influence (particularly maternal influence and health care providers) predicts vaccination series initiation (Kester, Zimet, Fortenberry, Kahn, & Shew, 2012; Krieger, Kam, Katz, & Roberto, 2011; Krieger, Katz, Kam, & Roberto, 2012). However, our study population had already initiated the vaccine series; therefore, parental influence may not be as relevant. Related, parental influences may fade or become less salient for young women making health decisions as adults (Teitelman et al., 2011). Prescriptive norms may be more meaningful for adolescent audiences given that parental permission is legally required for vaccination.
These findings suggest that the TPB offers more limited explanatory power for predicting behavioral adoption over time and that studying series completion as distinct from initial vaccine uptake and intention to receive three doses of the vaccine is an important area for scholarly consideration (Dempsey et al., 2011). Our findings show that potential barriers to and facilitators of series completion are quite different. There is no “one-sized fits all” approach to encouraging vaccination uptake and series completion. Rather, communication interventions should differentiate persuasive strategies appropriate to improving uptake and improving series completion in target populations sharing similar socio-cultural beliefs and barriers to vaccination.
Limitations
There are noted limitations to our research. We recognize the cross-sectional nature of the baseline survey does not allow for measuring temporal changes in health-related attitudes and beliefs, the influence of subjective norms, perceived behavioral control, and behavioral intentions. An alternative approach would examine differences in key TPB variables between the comparison and intervention groups at doses 2 and 3, in addition to baseline/dose 1. Moreover, there may be other theoretical constructs, structural barriers, and cultural practices that are unaccounted for in our analysis and participants may have experienced difficulties in recalling past sexual health experiences. Because ours was a community-based study, we did not include a probability sample of patients. However, random assignment of participants to each condition was designed to ensure the translatability of the intervention effects to similar populations.
Despite these limitations, our study focused on improving health equity and reducing cervical cancer disparities among a high-risk population of young women residing in the Appalachian Mountains of eastern Kentucky. Women in this medically underserved region are disparately burdened by cervical cancer compared to other Kentucky women and the general female population residing in the United States. These findings of significant improvements in series completion after the DVD-based intervention are robust, as they were achieved in comparison to an idealized standard-of-care protocol. One limitation to external validity is that the vaccine was provided at no cost; however, in medically underserved communities similar to Appalachian Kentucky, providers can be reimbursed for vaccine costs through manufacturers’ vaccine assistance programs, and the vaccine can remain free to women.
Areas for Future Research
Clearly, the DVD production process should be repeated with other populations to create effective, appropriate, and translatable communication strategies. Notably, our theory-based DVD was guided by information gathered from formative research conducted in the target community (Cohen & Head, in press; Head & Cohen, 2012). Similar processes of formative research used for this study could garner insights into the appropriate substitution of local data, expert, and peer narratives. Future research may also consider appropriate ways to target messages to other groups. If our video were shown to adolescent girls, messages related to Pap testing, which may not be appropriate for females under age 18, could be excluded from the video. Alternatively, key message components could be maintained and video footage re-shot for use with males because they are now eligible for the HPV vaccine (Dunne et al., 2011).
In an era of more “personalized” medicine, educational interventions at the point of clinical services may become routine. Future research may also consider how brief clinical assessments of individual patient’s barriers to vaccination (and adherence) may be used to create tailored digital educational messages to enhance vaccination schedule adherence. Given the Affordable Care Act’s incentives for improving digitization of medical records, future research also may consider how digital educational materials can be integrated into the electronic medical record and patient education system. The digital video format ensures the fidelity of the message, supports potential integration into existing clinic resources, and is compatible with delivery in community settings (e.g., delivered via iPad, portable DVD, kiosk, laptop, or desktop computer), provided equipment security and patient privacy concerns are addressed.
Finally, future research may consider how training nurse practitioners and community health workers may be used to improve the delivery of vaccinations in medically underserved communities. For example, training staff to assist with pharmaceutical companies’ reimbursement paperwork could serve as a cost-effective measure to obtaining free or low-cost vaccine supplies for the provider, as well as eliminate patient costs.
Conclusions
A theory-grounded DVD education intervention was successful in improving HPV vaccination completion rates. Our approach has the potential to be adapted and replicated with other populations of women, including other rural communities and African American and Hispanic populations; these populations also are recognized for cervical cancer disparities and share many similarities with our target population, such as low socioeconomic status, limited access to care, and poor living environments (Freeman & Wingrove, 2005). As advocated by Glasgow and colleagues (2004), ultimately, the long-term goal of this evidence-based intervention is widespread dissemination; in fact, dissemination has been a priority since conceptualization of the study. For decades, there has been a documented chasm between research and public health practice (Green, Ottoson, García, & Hiatt, 2009; IOM, 2001). An intervention such as ours can be can be modified to other populations, can be delivered in a variety of non-clinical settings, and requires few time, staff, and organizational resources to implement. Indeed, it could become routine clinical practice to show the video to women immediately after receiving dose one of the HPV vaccine.
Findings also suggest the potential for translating this approach to other vaccination contexts in which adherence to a multiple dosage regimen is necessary (e.g., Hepatitis B; H1N1 for children). Theory-based communication interventions designed to overcome barriers to dissemination from the beginning (Glasgow, Marcus, Bull, & Wilson, 2004) and promote successful translation from research to practice (Schoenwald & Hoagwood, 2001) help to make an immediate impact on population-level cancer incidence, morbidity, and mortality.
Acknowledgments
The authors would like to thank Seth M. Noar, PhD, Katharine J. Head, MA, Margaret L. McGladrey, MA, and Schyler B. Simpson, MA for their assistance in message testing and development of the DVD intervention. We would also like to recognize Pamela Stamper, RN and Nebraska A. Jones, RN for their assistance in recruiting study participants and data collection.
This publication was supported by Cooperative Agreement Number 1U48DP001932-01 from the Centers for Disease Control and Prevention. The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Footnotes
The HPV vaccine is not therapeutic for existing HPV infection or cervical abnormalities; however, women with a history of HPV infection and/or an abnormal Pap are still eligible for HPV vaccination to help prevent against infection with HPV virus types not already acquired (Markowitz et al., 2007).
Design concept of study: Crosby, Vanderpool, Cohen, Bates, Collins, Jones, Casey
Acquisition of data: Bates, Jones
Data analysis and interpretation: Crosby, Cohen, Vanderpool, Bates, Jones
Manuscript draft: Vanderpool, Cohen, Crosby
Acquisition of funding: Crosby
Administrative, technical, or material assistance: Collins, Vanderpool, Cohen, Bates, Jones, Casey, Crosby
Supervision: Crosby, Bates
References
- ACS. Cancer Facts and Figures 2012. 2012 from http://www.cancer.org/acs/groups/content/@epidemiologysurveilance/documents/document/acspc-031941.pdf.
- Ajzen I, Fishbein M. Understanding attitudes and predicting social behavior. Englewood Cliffs, NJ: Prentice-Hall; 1980. [Google Scholar]
- Allen JD, Coronado GD, Williams RS, Glenn B, Escoffery C, Fernandez M, Mullen PD. A systematic review of measures used in studies of Human Papillomavirus (HPV) vaccine acceptability. Vaccine. 2010;28(24):4027–4037. doi: 10.1016/j.vaccine.2010.03.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen JD, Mohllajee AP, Shelton RC, Othus MKD, Fontenot HB, Hanna R. Stage of adoption of the human papillomavirus vaccine among college women. Preventive Medicine. 2009;48(5):420–425. doi: 10.1016/j.ypmed.2008.12.005. [DOI] [PubMed] [Google Scholar]
- ARC. Underlying socioeconomic factors influencing health disparities in the Appalachian region final report. 2008 Retrieved July 24, 2012, from http://www.arc.gov/assets/research_reports/SocioeconomicFactorsInfluencingHealthDisparitiesinAppalachianRegion5.pdf.
- ARC. Uemployment Rates, 2010. 2012 Retrieved March 12, 2012, from http://www.arc.gov/reports/region_report.asp?FIPS=21999&REPORT_ID=35.
- Armitage CJ, Conner M. Efficacy of the Theory of Planned Behaviour: A meta-analytic review. British Journal of Social Psychology. 2001;40(Pt 4):471–499. doi: 10.1348/014466601164939. [DOI] [PubMed] [Google Scholar]
- Bandura A. Health promotion by social cognitive means. Health Education and Behavior. 2004;31(2):143–164. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- Bennett KK, Buchanan JA, Adams AD. Social-cognitive predictors of intention to vaccinate against the human papillomavirus in college-age women. The Journal of Social Psychology. 2012;152(4):480–492. doi: 10.1080/00224545.2011.639408. [DOI] [PubMed] [Google Scholar]
- Brehm S, Brehm JW. Psychological Reactance: A thoery of freedom and control. New York, NY: Academic Press; 1981. [Google Scholar]
- Brewer NT, Fazekas KI. Predictors of HPV vaccine acceptability: A theory-informed, systematic review. Prev Med. 2007;45(2–3):107–114. doi: 10.1016/j.ypmed.2007.05.013. [DOI] [PubMed] [Google Scholar]
- Brewer NT, Gottlieb SL, Reiter PL, McRee AL, Liddon N, Markowitz L, Smith JS. Longitudinal predictors of human papillomavirus vaccine initiation among adolescent girls in a high-risk geographic area. Sexually Transmitted Diseases. 2011;38(3):197–204. doi: 10.1097/OLQ.0b013e3181f12dbf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bynum SA, Brandt HM, Sharpe PA, Williams MS, Kerr JC. Working to close the gap: Identifying predictors of HPV vaccine uptake among young african american women. Journal of Health Caree for the Poor and Underserved. 2011;22(2):549–561. doi: 10.1353/hpu.2011.0060. [DOI] [PubMed] [Google Scholar]
- CDC. Genital HPV Infection-CDC Fact Sheet. 2012 from http://www.cdc.gov/std/HPV/STDFact-HPV.htm.
- Center KSD. Kentucky Counties -- 2010 Census Redistricting Data Demographic Profiles. 2012 Retrieved September 27, 2012, from http://ksdc.louisville.edu/1census.htm.
- Chao C, Slezak JM, Coleman KJ, Jacobsen SJ. Papanicolaou Screening Behavior in Mothers and Human Papillomavirus Vaccine Uptake in Adolescent Girls. American Journal of Public Health. 2009;99(6):1137–1142. doi: 10.2105/ajph.2008.147876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chao C, Velicer C, Slezak JM, Jacobsen SJ. Correlates for completion of 3-dose regimen of HPV vaccine in female members of a managed care organization. Mayo Clinic Proceedings. 2009;84(10):864–870. doi: 10.4065/84.10.864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chao C, Velicer C, Slezak JM, Jacobsen SJ. Correlates for Human Papillomavirus Vaccination of Adolescent Girls and Young Women in a Managed Care Organization. American Journal of Epidemiology. 2010;171(3):357–367. doi: 10.1093/aje/kwp365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen EL, Head KJ. HPV vaccine diffusion: Differences in risk communication among early-adopters and non-adopters. Journal of Health Communication (in press) [Google Scholar]
- Cohen EL, Vanderpool RC, Crosby RA, Noar SM, Bates W, Collins T, Casey B. 1-2-3 Pap: An HPV prevention campaign to reduce cervical cancer in Eastern Kentucky. In: Kreps GL, Dutta MJ, editors. Communication and health disparities. Cresskill, NJ: Hampton Press; (in press) [Google Scholar]
- Crosby R, Casey B, Vanderpool R, Collins T, Moore GR. Uptake of free HPV vaccination among young women: A comparison of rural versus urban rates. Journal of Rural Health. 2011 doi: 10.1111/j.1748-0361.2010.00354.x. online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crosby R, Schoenberg N, Hopenhayn C, Moore G, Melhan W. Correlates of intent to be vaccinated against human papillomavirus: an exploratory study of college-aged women. Sexual Health. 2007;4(1):71–73. doi: 10.1071/sh06046. SH06046 [pii] [DOI] [PubMed] [Google Scholar]
- Dempsey A, Cohn L, Dalton V, Ruffin M. Worsening disparities in HPV vaccine utilization among 19–26 year old women. Vaccine. 2011;29(3):528–534. doi: 10.1016/j.vaccine.2010.10.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dorell C, Stokley S, Yankey D, Markowitz L. National and state vaccination coverage among adolescents aged 13 through 17 Years- United States, 2010. Morbidity and Mortality Weekly Report. 2011;60(33):1117–1123. [PubMed] [Google Scholar]
- Dunne EF, Markowitz LE, Chesson H, Saraiya M, Gee J, Unger ER. Recommendations on the use of quadrivalent Human Papillomavirus vaccine in males — Advisory Committee on Immunization Practices (ACIP), 2011. Morbidity and Mortality Weekly Report. 2011;60(50):1705–1708. [PubMed] [Google Scholar]
- Dunne EF, Unger ER, Sternberg M, et al. Prevalence of hpv infection among females in the United States. Journal of the American Medical Association. 2007;297(8):813–819. doi: 10.1001/jama.297.8.813. [DOI] [PubMed] [Google Scholar]
- Ferrer RA, Morrow KM, Fisher WA, Fisher JD. Toward an information–motivation–behavioral skills model of microbicide adherence in clinical trials. AIDS Care. 2010;22(8):997–1005. doi: 10.1080/09540121003623719. [DOI] [PubMed] [Google Scholar]
- Fisher JD, Fisher WA. The information-motivation-behavioral skills model. In: DiClemente RJ, Crosby RA, Kegler MC, editors. Emerging theories in health promotion practice and research:Strategies for improving public health. 1. San Francisco: Jossey-Bass; 2002. pp. 40–70. [Google Scholar]
- Fisher WA, Fisher JD, Harman J. The Information-Motivation-Behavioral Skills Model: A general social psychological approach to understanding and promoting health behavior. In: Suls J, Wallston K, editors. Social Psychological Foundations of Health and Illness. Malden, MA: Blackwell Publishing, Ltd; 2003. pp. 82–106. [Google Scholar]
- Freeman HP, Wingrove BK. Excess cervical cancer mortality: A marker for low access to health care in poor communities. Rockville, MD: National Cancer Institute, Center to Reduce Cancer Health Disparities; 2005. [Google Scholar]
- Gerend MA, Shepherd JE. Predicting human papillomavirus vaccine uptake in young adult women: Comparing the Health Belief Model and Theory of Planned Behavior. Annals of Behavioral Medicine. 2012;44(2):171–180. doi: 10.1007/s12160-012-9366-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glasgow RE, Marcus AC, Bull SS, Wilson KM. Disseminating effective cancer screening interventions. Cancer. 2004;101(S5):1239–1250. doi: 10.1002/cncr.20509. [DOI] [PubMed] [Google Scholar]
- Green LW, Ottoson JM, García C, Hiatt RA. Diffusion Theory and Knowledge Dissemination, Utilization, and Integration in Public Health. Annu Rev Public Health. 2009;30(1):151–174. doi: 10.1146/annurev.publhealth.031308.100049. [DOI] [PubMed] [Google Scholar]
- Head KJ, Cohen EL. Young women’s perspectives on cervical cancer prevention in Appalachian Kentucky. Qualitative Health Research. 2012;22(4):476–487. doi: 10.1177/1049732311425053. [DOI] [PubMed] [Google Scholar]
- Hopenhayn C, King JB, Christian A, Huang B, Christian WJ. Variability of cervical cancer rates accross 5 Appalachian states, 1998–2003. Cancer. 2008;113(10):2974–2980. doi: 10.1002/cncr.23749. [DOI] [PubMed] [Google Scholar]
- Hopfer S. Effects of a narrative HPV vaccination intervention aimed at reaching college women: a randomized controlled trial. Prev Sci. 2012;13(2):173–182. doi: 10.1007/s11121-011-0254-1. [DOI] [PubMed] [Google Scholar]
- HRSA. Health Professional Shortage Areas by State and County. 2012 Retrieved July 24, 2012, from http://hpsafind.hrsa.gov/HPSASearch.aspx.
- Huang B, Wyatt S, Tucker T, Bottorff D, Lengerich E, Hall H. Cancer death rates – Appalachia, 1994–1998. Morbidity and Mortality Weekly Report. 2002;51:527–529. [PubMed] [Google Scholar]
- IOM. Crossing the quality chasm: A new health system for the 21st century. Washington, D.C: National Academy Press; 2001. [PubMed] [Google Scholar]
- Jain N, Euler GL, Shefer A, Lu P, Yankey D, Markowitz L. Human papillomavirus (HPV) awareness and vaccination initiation among women in the United States, National Immunization Survey-Adult 2007. Preventive Medicine. 2009;48:426–431. doi: 10.1016/j.ypmed.2008.11.010. [DOI] [PubMed] [Google Scholar]
- Juraskova I, O’Brien M, Mullan B, Bari R, Laidsaar-Powell R, McCaffery K. HPV vaccination and the effect of information framing on intentions and behaviour: An application of the Theory of Planned Behaviour and Moral Norm. International Journal of Behavioral Medicine. 2011:1–8. doi: 10.1007/s12529-011-9182-5. [DOI] [PubMed] [Google Scholar]
- Kahn JA, Rosenthal SL, Hamann T, Bernstein DI. Attitudes about human papillomavirus vaccine in young women. International Journal of STD and AIDS. 2003;14(5):300–306. doi: 10.1258/095646203321605486. [DOI] [PubMed] [Google Scholar]
- Katz IT, Ware NC, Gray G, Haberer JE, Mellins CA, Bangsberg DR. Scaling up human papillomavirus vaccination: A conceptual framework of vaccine adherence. Sexual Health. 2010;7(3):279–286. doi: 10.1071/SH09130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- KCR. Cervical cancer incidence, 2005–2009. 2012 July 24, 2012, from http://www.kcr.uky.edu/
- KDPH. Kentucky Behavioral Risk Factor Surveillance System (BRFSS) 2008 annual report. 2008 Retrieved July 24, 2012, from http://chfs.ky.gov/NR/rdonlyres/73E49DF2-81D3-4E05-BDC3-DA348F4E7F1E/0/Kentucky2008BRFSSAnnualReport.pdf.
- Kepka D, Berkowitz Z, Yabroff KR, Roland K, Saraiya M. Human papillomavirus vaccine practices in the USA: Do primary care providers use sexual history and cervical cancer screening results to make HPV vaccine recommendations? Sexually Transmitted Infections. 2012;88(6):433–435. doi: 10.1136/sextrans-2011-050437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kester LM, Zimet GD, Fortenberry JD, Kahn JA, Shew ML. A national study of HPV vaccination of adolescent girls: Rates, predictors, and reasons for non-vaccination. Maternal and Child Health Journal. 2012 doi: 10.1007/s10995-012-1066-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krawczyk A, Lau E, Perez S, Delisle V, Amsel R, Rosberger Z. How to inform: Comparing written and video education interventions to increase human papillomavirus knowledge and vaccination intentions in young adults. Journal of American College Health. 2012a;60(4):316–322. doi: 10.1080/07448481.2011.615355. [DOI] [PubMed] [Google Scholar]
- Krawczyk AL, Perez S, Lau E, Holcroft CA, Amsel R, Knäuper B, Rosberger Z. Human papillomavirus vaccination intentions and uptake in college women. Health Psychology. 2012b;31(5):685–693. doi: 10.1037/a0027012. [DOI] [PubMed] [Google Scholar]
- Krieger JL, Kam J, Katz ML, Roberto A. Does mother know best: An actor-partner model of college age females’ HPV vaccination behavior. Human Communication Research. 2011;37:107–124. [Google Scholar]
- Krieger JL, Katz M, Kam J, Roberto A. Appalachian and non-Appalachian pediatricians’ encouragement of the Human Papillomavirus (HPV) vaccine: Implications for health disparities. Women’s Health Issues. 2012;22(1):e19–e26. doi: 10.1016/j.whi.2011.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lechuga J, Swain GR, Weinhardt LS. The cross-cultural variation of predictors of human papillomavirus vaccination intentions. Journal of Women’s Health. 2011;20(2):225–230. doi: 10.1089/jwh.2010.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leonard S, Kola S, Walsh JC. The efficacy of a web-based educational intervention in promoting acceptability of the HPV vaccine. Paper presented at the 25th Annual Conference of the European Health Psychology Society (EHPS); Crete, Greece. 2011. [Google Scholar]
- Markowitz L, Dunne EF, Saraiya M, Lawson H, Chesson H, Unger E. Morbidity and Mortality Weekly Report. Vol. 56. Atlanta, GA: Centers for Disease Control and Prevention; 2007. Quadrivalent human papillomavirus vaccine: Recommendations of the ACIP; pp. 1–24. [PubMed] [Google Scholar]
- Mills LA, Head KJ, Vanderpool RC. HPV vaccination among young adult women: A perspective from the mountains of Appalachian Kentucky. Preventing Chronic Disease. doi: 10.5888/pcd10.120183. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mills LA, Vanderpool RC, Crosby RA. Sexually related behaviors as predictors of hpv vaccinaton among young rural women. Journal of Women’s Health. 2011;20(12):1909–1915. doi: 10.1089/jwh.2011.3000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCI. State Cancer Profiles, Kentucky. 2012 Retrieved July 24, 2012, from http://statecancerprofiles.cancer.gov/
- Prochaska J, Redding C, Evers K. The Transtheoretical Model and Stages of Change. In: Glanz K, Rimer BK, Viswanath K, editors. Health Behavior and Health Education: Theory, Research, and Practice. San Francisco: Jossey-Bass; 2008. [Google Scholar]
- Reiter PL, Brewer NT, Gottlieb SL, McRee A, Smith JS. Parents’ health beliefs and HPV vaccination of their adolescent daughters. Social Science and Medicine. 2009;69:475–480. doi: 10.1016/j.socscimed.2009.05.024. [DOI] [PubMed] [Google Scholar]
- Rogers EM. Diffusion of innovations. 4. New York: The Free Press; 1995. [Google Scholar]
- Rosenstock I. The Health Belief Model and Preventive Health Behavior. Health Education Monographs. 1974;2(4):354–386. doi: 10.1177/109019817800600406. [DOI] [PubMed] [Google Scholar]
- Schoenwald SK, Hoagwood K. Effectiveness, transportability, and dissemination of interventions: What matters when? Psychiatric Services. 2001;52(9):1190–1197. doi: 10.1176/appi.ps.52.9.1190. [DOI] [PubMed] [Google Scholar]
- Teitelman AM, Stringer M, Nguyen GT, Hanlon AL, Averbuch T, Stimpfel AW. Social cognitive and clinical factors associated with HPV vaccine initiation among urban, economically disadvantaged women. Journal of Obstetric, Gynecologic, and Neonatal Nursing. 2011;40(6):691–701. doi: 10.1111/j.1552-6909.2011.01297.x. [DOI] [PubMed] [Google Scholar]
- Vanderpool RC, Casey B, Crosby R. HPV-related risk perceptions and HPV vaccine uptake among a sample of young rural women. Journal of Community Health. 2011;36(6):903–909. doi: 10.1007/s10900-010-9345-3. [DOI] [PubMed] [Google Scholar]
- Vanderpool RC, Crosby RA, Casey BR, Bates W. Predictors of Human Papillomavirus (HPV) vaccine uptake among young rural women. Paper presented at the APHA 138 Annual Meeting; Denver, CO. 2010. [Google Scholar]
- Webb TL, Sheeran P. Does changing behavioral intentions engender behavior change? A meta-analysis of the experimental evidence. Psychol Bulletin. 2006;132(2):249–268. doi: 10.1037/0033-2909.132.2.249. [DOI] [PubMed] [Google Scholar]
- Williams WW, Lu P, Singleton JA, Bridges CB, Wortley PM, Byrd KK. Adult vaccination coverage-United States, 2010. Morbidity and Mortality Weekly Report. 2012;61:66–72. [PubMed] [Google Scholar]
- Wingo PA, Tucker TC, Jamison PM, Martin H, McLaughlin C, Bayakly R, Richards TB. Cancer in Appalachia, 2001–2003. Cancer. 2008;112(1):181–192. doi: 10.1002/cncr.23132. [DOI] [PubMed] [Google Scholar]