Abstract
Propionibacterium acnes has been implicated as a cause of infection following shoulder surgery, may occur up to 2 years after the index operation and has been shown to be responsible for up to 56% of shoulder infections after orthopedic implant. Male patients within the population undergoing shoulder surgery are particularly at risk, especially if their shoulder surgery involved prosthesis or was posttraumatic. P. acnes infection can be difficult to diagnose clinically and laboratory techniques require prolonged and specialized cultures. Usual inflammatory markers are not raised in infection with this low virulence organism. Delayed diagnosis with P. acnes infection can result in significant morbidity prior to prosthesis failure. Early diagnosis of P. acnes infection and appropriate treatment can improve clinical outcomes. It is important to be aware of P. acnes infection in shoulder surgery, to evaluate risk factors, to recognize the signs of P. acnes infection, and to promptly initiate treatment. The signs and symptoms of P. acnes infection are described and discussed. Data were collected from PubMed™, Web of Science, and the NICE Evidence Healthcare Databases - AMED (Ovid), BNI (Ovid), CINAHL (EBSCO), Embase (Ovid), HMIC: DH-Data and Kings Fund (Ovid), Medline (Ovid), and PsycINFO (Ovid). The search terms used were “P. acnes,” “infection,” “shoulder,” and “surgery.” In this review, we summarize the current understanding of the prevention and management of P. acnes infection following shoulder surgery.
Keywords: Infection, orthopedic, Propionibacterium acnes, prostheses, shoulder
INTRODUCTION
Propionibacterium acnes is a nonspore-forming, anaerobic, Gram-positive bacillus.[1,2,3] Paul Gerson Unna first described it in 1896,[2] as acne bacillus and in 1933, it was assigned to the genus of Propionibacterium.[4] It is of low virulence and is often a commensal in the lipid-rich sebaceous follicles and deep layers of the skin, conjunctiva, external auditory canal, respiratory tract, and intestinal tract.[2,3,5,6] P. acnes mostly colonizes the pilosebaceous follicles in the skin of the upper body, including the head, neck, shoulders, and especially the axilla.[5,7,8] Its pathogenic activity has been shown in endocarditis, endophthalmitis, septic arthritis, osteomyelitis, chronic prostatitis, sarcoidosis and synovitis, acne, pustulosis, hyperostosis, and Osteitis syndrome.[9,10,11,12,13,14,15,16] There are hemolytic and nonhemolytic phylotypes, with the former representing the most pathogenic strain.[17,18]
P. acnes adheres to cells, biofilms, and surfaces by means of antigenic proteins,[19,20] which can initiate an inflammatory response within the joint.[2] They also secrete cytotoxic chemicals and enzymes designed to degrade body tissues and the shoulder capsule.[2] Furthermore, P. acnes are able to secrete and live within an extracellular polysaccharide biofilm, aiding micro-colony formation, as well as avoiding phagocytosis, and surviving macrophage engulfment.[2,21] The combination of the bacteriumentocyto limb distribution and its role in prosthetic joint infection (PJI), accounting for up to 56% of shoulder infections involving orthopedic implants,[22] is now coercing shoulder surgeons to consider P. acnes as an “orthopedic pathogen.”[3] We present a comprehensive review of the current information on the identification and management of P. acnes following shoulder surgery.
MATERIALS AND METHODS
This review focuses on recent studies of: The patient subgroups that are more at the risk of infection; the pathophysiology of P. acnes in shoulder infections; the effect of P. acnes on the postoperative healing process of the shoulder; and the prevention and management of shoulder infection with P. acnes. Information was also gathered about the incidence of P. acnes infection. A schematic showing the search and selection strategy is shown in Figure 1. Searches were performed with PubMed™, Web of Science, and the NICE Evidence Healthcare Databases — AMED (Ovid), BNI (Ovid), CINAHL (EBSCO), Embase (Ovid), HMIC: DH-Data and Kings Fund (Ovid), Medline (Ovid), and PsycINFO (Ovid). The search terms used were “P. acnes,” “infection,” “shoulder,” and “surgery.”
Figure 1.
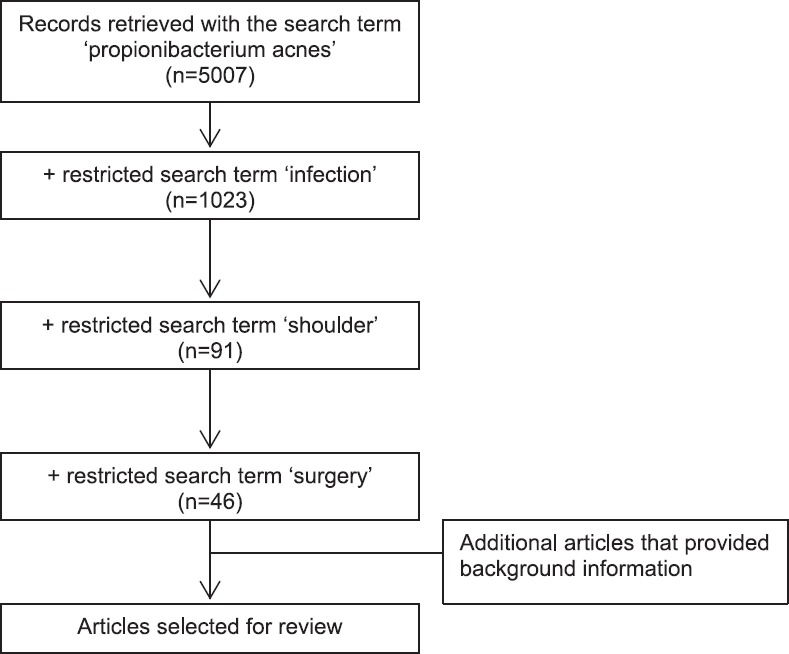
A schematic diagram of the literature search strategy
Incidence
Arthroplasty
Over the past decade, P. acnes has become increasingly recognized as a cause of infection in orthopedic surgery, especially postarthroplasty.[5,23,24] In shoulder arthroplasty, infection rates for anatomical arthroplasty have been reported to be <4%, but as high as 18% following reverse polarity arthroplasty.[25] In one study, the most common bacteria identified were Staphylococcus epidermidis and P. acnes.[25] In a retrospective review (over 7 years) from Canada, 80 patients were identified who had positive joint cultures after primary shoulder arthroplasty and P. acnes was found to be the second most common pathogenic organism in 25% of participants.[26] A study of PJI after total shoulder arthroplasty (in the last 33 years) found that Staphylococcus was the dominant organism, whereas from 2001 to 2008, the incidence of P. acnes was found to be almost as high as Staphylococcus.[27] This increasing incidence could be the result of changes in the microbiology of shoulder infections, heightened awareness of the organism, better surveillance, or improved laboratory diagnostic techniques.[27]
Soft tissue
Concerning soft tissue shoulder surgery, deep infection after rotator cuff repair can occur in up to 1.9% of cases, with studies finding P. acnes to be the most common causative organism.[8,28,29] Evidently, P. acnes appears to be a prominent organism in postoperative shoulder infections and is becoming increasingly prevalent.
Risk factors
Recorded risk factors for infection in shoulder arthroplasty, including P. acnes infection, are male gender, surgery of the upper body (especially the shoulder), increased duration of surgery, and interestingly, being the first surgery of the day.[8,27,30,31,32,33] The predominance of P. acnes in shoulder infections has been linked with the presence of the axillary lymph nodes.[34] Culturing of the epidermis during revision surgery found that 16/18 males had P. acnes infection, whereas only 7/12 female subjects tested positive.[35] Further studies have revealed that male gender and prior prosthetic implants are significant risk factors for P. acnes infection of the shoulder.[26,32,36] The male predisposition, of over 2.5 times higher risk than females after shoulder arthroplasty,[33] has been linked with the habitat of P. acnes being within the hair follicles and, therefore, the upper body of males would harbor more of the bacterium.[32,36] Moreover, males lacking signs of infection have a higher risk of P. acnes positive cultures during arthroplasty.[33] Interestingly, posttraumatic shoulder arthroplasty has 3 times higher risk of infection than elective surgery.[33] Reverse total arthroplasty also carries increased risk.[33] Younger age was identified as a risk factor, with each year of increasing age causing a risk reduction of 5%, however, body mass index and diabetes mellitus, which are usually associated with increased risk, were not found to be risk factors.[33] From the literature, it is evident that patients most at the risk of P. acnes infection are young people, males, those who have undergone upper limb surgery (especially reverse shoulder replacements), and posttraumatic surgery.
Diagnostic difficulties
Despite technological advances, the diagnosis of shoulder infections due to the low virulent P. acnes remains challenging. The nonspecific clinical presentation, inadequate culture performance, and the inability to accurately interpret positive cultures can delay diagnosis.[26] Inflammatory markers, usually indicative of infection, may not be raised with P. acnes infection.[6,37] In one study, C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) were both raised in only 10% of patients with P. acnes infections of the shoulder.[37] Furthermore, the sensitivities of CRP and ESR in shoulder infections were found to be 42% and 16%, respectively, whereas in the lower limbs, the sensitivities for CRP and ESR were found to be 88% and 75%, respectively.[38] Unlike in the lower limb, these inflammatory markers have been shown to be poor indicators of postoperative shoulder infections.[37] These data fit well with the distribution of P. acnes and its indolent nature. Owing to slow growth, P. acnes need longer culture times of up to 2 weeks, making infection harder to identify.[5,28,38] Furthermore, lowering the threshold for diagnosis (concentration of neutrophils in the tissues) would increase sensitivity because of the relatively low inflammatory response to the presence of P. acnes.[38] Interleukin-6 (IL-6), a factor involved in inflammation, has been studied as a way of detecting indolent infections of the shoulder and may represent as a possible new predictor.[39] Analysis of aspirated synovial fluid from 32 patients undergoing revision surgery for suspected PJI after arthroplasty for IL-6 titers showed that IL-6 levels were considerably increased in patients infected with P. acnes.[39] In a study presented at the British Elbow and Shoulder Society, P. acnes was found in 38% of patients (n = 101 patients) undergoing arthroscopic shoulder surgery for rotator cuff with enrichment medium. Furthermore, authors have concluded that to improve reliability, deoxyribonucleic acid and polymerase chain reaction tests are being developed, as contamination cannot be reliably ruled out via enrichment medium.
Clinical presentation
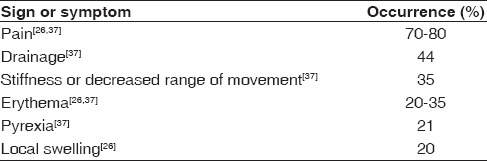
A common assumption is that P. acnes infection originates in the epidermis of the patient at reliably ruled out via enrichment surface to the surgical site.[35] Surface sterilization before surgery does not, however, eradicate the bacterium as the organism actually resides deep in the sebaceous glands. Scalpel incisions slice through these follicles seeding the bacteria.[35] Innovative methods of sterilization may, therefore, be required to penetrate the dermis and reduce P. acnes spread.[16] The need for intraoperative screening of wounds and prolonged cultures to assess the risk of developing a postoperative shoulder infection has been emphasized.[6,16,35] For low-grade P. acnes shoulder infections, pain may be the only symptom, followed by stiffness, with all other signs of infection, including fever, usually being absent.[6,8,21,40,41] Prolonged low-grade infection can result in loss of normal function of the joint or progress to sepsis.[25] The common patterns of clinical presentation are displayed in Table 1.[26,37]
Table 1.
Presentation of postoperative Propionibacterium acnes infection in the shoulder
The mean time from index surgery to diagnosis of P. acnes infection was 1.8 years following rotator cuff repair surgery,[8] whereas after arthroplasty, it has been shown to be 2.1 years.[40] It was also suggested that the variance in the clinical presentation of shoulder infections can not only be due to the nonspecific clinical manifestation of P. acnes, but also due to co-infection with other species of bacteria within the surgical site.[8]
Prosthesis failure
Infection is the most common cause of joint replacement failure in the shoulder, but some of the diagnosed aseptic loosening may also be due to low-grade P. acnes infection.[33,42] Of the 63 cases of aseptic loosening and 63 cases of PJI, in one cohort study assessing knee, hip, shoulder, and elbow revision surgeries, P. acnes was found in 12 and 2 cases, respectively, but none in cases of mechanical failure [Figure 2].[42] P. acnes could be a causative factor in some cases which were thought to be as aseptic loosening of joint implants and requires further research.[6,42] In a study including 75 patients undergoing shoulder revision arthroplasties with positive intraoperative cultures, P. acnes was found in 60% of cases.[43] 10 out of these 75 patients required re-revision, 7 had positive bacterial cultures of which 5 were P. acnes (71%).[43]
Figure 2.
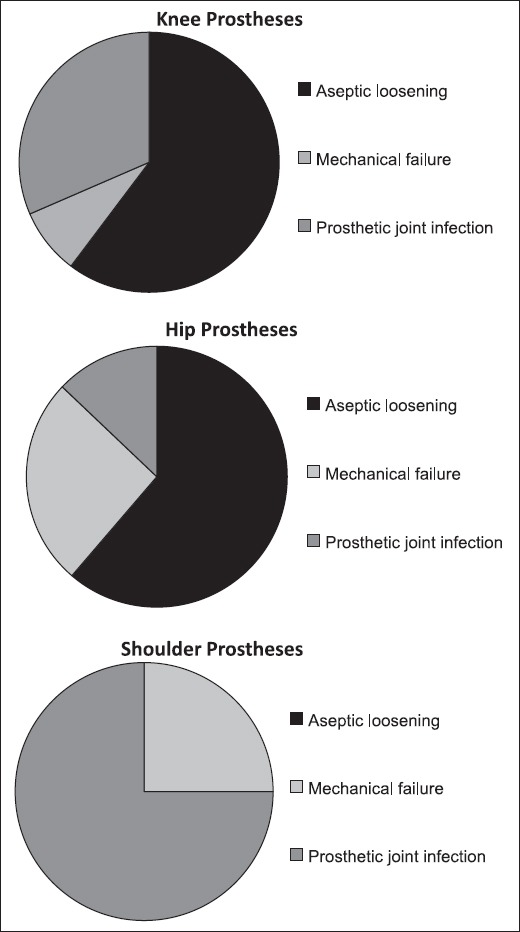
A comparison of causes of prosthesis failure in the knee, hip and shoulder. Adapted from Ref. 42
Drug resistance
Patient knowledge about P. acnes is mostly limited to acne vulgaris, a skin infection present in the vast majority of young adults and teenagers.[2,44,45] Hormonal changes and genetics cause sebaceous gland inflammation, dysfunction, and proliferation, providing an environment for the opportunistic P. acnes.[2] The treatment of this skin condition with experimental courses of broad-spectrum antibiotics, often combined with poor compliance, is thought to be a contributor to antibiotic resistance.[8] Gold standard antibiotics such as penicillins, vancomycin, tetracyclines, rifampicin, and erythromycin often eradicate the bacterium, however, over half of P. acnes cultures now carry resistance to more than one of the above antibiotics.[8,23,30,46,47]
Treatment and outcomes
With the increase in shoulder operations[48] and prevalence of P. acnes,[23] advances in the management of such infections have been accelerated.[23] Superficial surface infections can be controlled using wound care and antibiotics, however, deeper surgical site infection requires irrigation and surgical debridement with antibiotic treatment. Surgical debridement alone cannot eliminate infection, and intravenous antibiotic therapy may last up to 6 weeks.[23,49] Excess scar tissue, due to repeated surgery, can deteriorate functional outcome.[50] A retrospective study evaluating the characteristics and clinical outcomes of PJIs of the shoulder indicated that clinical trials have provided little evidence of the best antibiotic regimes for P. acnes.[23] Vancomycin and clindamycin are first-line for deep P. acnes infections of the shoulder; however, first-generation cephalosporins and penicillins may have a greater role in the future.[23] Rifampin and daptomycin combined (to avoid rifampin resistance) have been shown to yield the highest cure rate of 63% in an animal cage model.[51] In established low-grade infections with P. acnes, exchange of the prosthesis might provide the best clinical outcome.[34]
Prevention
The increasing prevalence of P. acnes and other bacteria likely to infect during a prosthetic shoulder operation has provided a demand for innovative methods of reducing contamination. The application of a liquid cyanoacrylate-based sealant onto the skin of patients before surgery to act as a barrier for surface infection, combined with the iodine wash, has been found to reduce rates of infection compared to just the iodine wash alone.[52] In a prospective study of 150 patients, there was no difference in ChloraPrep (2% chlorhexidine gluconate and 70% isopropyl alcohol), DuraPrep (0.7% iodophor and 74% isopropyl alcohol), or povidone-iodine scrub, and paint (0.75% iodine scrub and 1.0% iodine paint) to eliminate P. acnes, although ChloraPrep was most effective in eliminating coagulase negative Staphylococcus when used for preoperative preparation.[53] These two were the most common native organisms in shoulder cultures.[53]
Propionibacterium acnes and arthritis
P. acnes might play a role in the development of arthritis of the shoulder.[3] It has previously been shown that the injection of P. acnes into the joints of rats leads to arthritis.[3] Furthermore, there is a hypothesis that the relapsing-remitting cycles of pain in osteoarthritis may be linked to the flare-ups of the bacterial population within the joint.[3] This research was initiated due to the findings of high incidence of P. acnes in shoulders before arthroplasties, suggesting a correlation with arthropathy.[3] A recent publication, however, contradicts these findings.[54] Upon microbiological and histopathological analysis of tissue samples from 32 patients diagnosed with shoulder arthritis undergoing primary shoulder arthroplasty, no patients had findings or cultures compatible with P. acnes infection.[54] This study emphasizes the need for strictly controlled specimen collection during surgery to reduce contamination and the need to review prophylactic antibiotic regimens.[54]
Current policy at senior author's institution
Shoulder PJI is uncommon, but represents a significant problem. We follow common precautions for shoulder joint arthroplasty as in the knee and hip. We have preoperative screening for infection, double preparation of the joint in an anesthetic room and operating theater, and use ChloraPrep. To reduce the risk of infection, we ensure the isolation of the axilla, avoid incisions near the axilla, thoroughly lavage inside the joint, and give antibiotics as per microbiological guidelines locally. Antibiotic-impregnated cement can be used as well as repeat antibiotics in prolonged surgery (>2 h), if indicated, and separate postoperative wards for arthroplasty patients are utilized. For P. acnes, however, the most important aspect is to keep a low index of suspicion in cases of persistent postoperative pain. We have a low threshold for performing open controlled biopsy in such cases for microbiology and histopathology. We closely liaise with microbiology and pathology for PJI as we feel prolonged cultures and clinical-microbiological correlation are important to diagnose P. acnes infection. If biopsies are found to be positive, we perform a two-stage revision and treat with antibiotics as per sensitivities. Second stage is only performed after a clear, open biopsy.
CONCLUSION
P. acnes is a common cause of infection following shoulder surgery and is responsible for 1-in-2 shoulder infections after orthopedic implant. Younger men, among the population undergoing shoulder arthroplasty, are particularly at risk. P. acnes infection can be difficult to diagnose and delayed diagnosis can result in significant disease states leading up to prosthesis failure. With an increasing rate of antibiotic-resistant bacteria, P. acnes infection is becoming increasingly difficult to treat. In this review, we summarized the current understanding of the risk factors, clinical presentation, and management of P. acnes infection following shoulder surgery.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Achermann Y, Goldstein EJ, Coenye T, Shirtliff ME. Propionibacterium acnes: From commensal to opportunistic biofilm-associated implant pathogen. Clin Microbiol Rev. 2014;27:419–40. doi: 10.1128/CMR.00092-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aubin GG, Portillo ME, Trampuz A, Corvec S. Propionibacterium acnes, an emerging pathogen: From acne to implant-infections, from phylotype to resistance. Med Mal Infect. 2014;44:241–50. doi: 10.1016/j.medmal.2014.02.004. [DOI] [PubMed] [Google Scholar]
- 3.Levy O, Iyer S, Atoun E, Peter N, Hous N, Cash D, et al. Propionibacterium acnes: An underestimated etiology in the pathogenesis of osteoarthritis? J Shoulder Elbow Surg. 2013;22:505–11. doi: 10.1016/j.jse.2012.07.007. [DOI] [PubMed] [Google Scholar]
- 4.Douglas HC, Gunter SE. The taxonomic position of Corynebacterium acnes. J Bacteriol. 1946;52:15–23. doi: 10.1128/JB.52.1.15-23.1946. [DOI] [PubMed] [Google Scholar]
- 5.Athwal GS, Sperling JW, Rispoli DM, Cofield RH. Acute deep infection after surgical fixation of proximal humeral fractures. J Shoulder Elbow Surg. 2007;16:408–12. doi: 10.1016/j.jse.2006.09.021. [DOI] [PubMed] [Google Scholar]
- 6.Zeller V, Ghorbani A, Strady C, Leonard P, Mamoudy P, Desplaces N. Propionibacterium acnes: An agent of prosthetic joint infection and colonization. J Infect. 2007;55:119–24. doi: 10.1016/j.jinf.2007.02.006. [DOI] [PubMed] [Google Scholar]
- 7.Agak GW, Qin M, Nobe J, Kim MH, Krutzik SR, Tristan GR, et al. Propionibacterium acnes Induces an IL-17 response in acne vulgaris that is regulated by Vitamin A and Vitamin D. J Invest Dermatol. 2014;134:366–73. doi: 10.1038/jid.2013.334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Millett PJ, Yen YM, Price CS, Horan MP, van der Meijden OA, Elser F. Propionibacterium acnes infection as an occult cause of postoperative shoulder pain: A case series. Clin Orthop Relat Res. 2011;469:2824–30. doi: 10.1007/s11999-011-1767-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ang M, Chee SP. Propionibacterium acnes endogenous endophthalmitis presenting with bilateral scleritis and uveitis. Eye (Lond) 2010;24:944–5. doi: 10.1038/eye.2009.194. [DOI] [PubMed] [Google Scholar]
- 10.Bachmeyer C, Blanchard M, Zeller V, Graff W, Desplaces N, Stankovic K, et al. Tibial chronic osteomyelitis due to Propionibacterium acnes in a patient with sickle cell anemia. Int J Infect Dis. 2010;14(Suppl 3):e344. doi: 10.1016/j.ijid.2009.07.007. [DOI] [PubMed] [Google Scholar]
- 11.Fassi Fehri L, Mak TN, Laube B, Brinkmann V, Ogilvie LA, Mollenkopf H, et al. Prevalence of Propionibacterium acnes in diseased prostates and its inflammatory and transforming activity on prostate epithelial cells. Int J Med Microbiol. 2011;301:69–78. doi: 10.1016/j.ijmm.2010.08.014. [DOI] [PubMed] [Google Scholar]
- 12.Ghosh M, Talwani R, Gilliam BL. Propionibacterium skull osteomyelitis treated with daptomycin. Clin Neurol Neurosurg. 2009;111:610–2. doi: 10.1016/j.clineuro.2009.04.003. [DOI] [PubMed] [Google Scholar]
- 13.Guío L, Sarriá C, de las Cuevas C, Gamallo C, Duarte J. Chronic prosthetic valve endocarditis due to Propionibacterium acnes: An unexpected cause of prosthetic valve dysfunction. Rev Esp Cardiol. 2009;62:167–77. doi: 10.1016/s1885-5857(09)71535-x. [DOI] [PubMed] [Google Scholar]
- 14.Magrey M, Khan MA. New insights into synovitis, acne, pustulosis, hyperostosis, and osteitis (SAPHO) syndrome. Curr Rheumatol Rep. 2009;11:329–33. doi: 10.1007/s11926-009-0047-8. [DOI] [PubMed] [Google Scholar]
- 15.Omori M, Bito T, Yamada M, Ogura K, Eishi Y, Nishigori C. Systemic sarcoidosis with bone marrow involvement showing Propionibacterium acnes in the lymph nodes. J Eur Acad Dermatol Venereol. 2015;29:2059–60. doi: 10.1111/jdv.12594. [DOI] [PubMed] [Google Scholar]
- 16.Schneeberger AG, Gilbart MK, Sheikh R, Gerber C, Ruef C. Non-purulent low-grade infection as cause of pain following shoulder surgery: Preliminary results. Chir Organi Mov. 2009;93(Suppl 1):S71–7. doi: 10.1007/s12306-009-0010-x. [DOI] [PubMed] [Google Scholar]
- 17.Nodzo SR, Hohman DW, Crane JK, Duquin TR. Hemolysis as a clinical marker for Propionibacterium acnes orthopedic infection. Am J Orthop (Belle Mead NJ) 2014;43:E93–7. [PubMed] [Google Scholar]
- 18.Sampedro MF, Piper KE, McDowell A, Patrick S, Mandrekar JN, Rouse MS, et al. Species of Propionibacterium and Propionibacterium acnes phylotypes associated with orthopedic implants. Diagn Microbiol Infect Dis. 2009;64:138–45. doi: 10.1016/j.diagmicrobio.2009.01.024. [DOI] [PubMed] [Google Scholar]
- 19.Girvan RC, Knight DA, O’Loughlin CJ, Hayman CM, Hermans IF, Webster GA. MIS416, a non-toxic microparticle adjuvant derived from Propionibacterium acnes comprising immunostimulatory muramyl dipeptide and bacterial DNA promotes cross-priming and Th1 immunity. Vaccine. 2011;29:545–57. doi: 10.1016/j.vaccine.2010.10.040. [DOI] [PubMed] [Google Scholar]
- 20.Kumaran D, Kalab M, Rood IG, de Korte D, Ramirez-Arcos S. Adhesion of anaerobic bacteria to platelet containers. Vox Sang. 2014;107:188–91. doi: 10.1111/vox.12141. [DOI] [PubMed] [Google Scholar]
- 21.Pottinger P, Butler-Wu S, Neradilek MB, Merritt A, Bertelsen A, Jette JL, et al. Prognostic factors for bacterial cultures positive for Propionibacterium acnes and other organisms in a large series of revision shoulder arthroplasties performed for stiffness, pain, or loosening. J Bone Joint Surg Am. 2012;94:2075–83. doi: 10.2106/JBJS.K.00861. [DOI] [PubMed] [Google Scholar]
- 22.Levy PY, Fenollar F, Stein A, Borrione F, Cohen E, Lebail B, et al. Propionibacterium acnes postoperative shoulder arthritis: An emerging clinical entity. Clin Infect Dis. 2008;46:1884–6. doi: 10.1086/588477. [DOI] [PubMed] [Google Scholar]
- 23.Crane JK, Hohman DW, Nodzo SR, Duquin TR. Antimicrobial susceptibility of Propionibacterium acnes isolates from shoulder surgery. Antimicrob Agents Chemother. 2013;57:3424–6. doi: 10.1128/AAC.00463-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lorillou M, Martha B, Chidiac C, Ferry T Lyon Bone and Joint Infection Study Group. Chronic Propionibacterium acnes prosthesis joint infection manifesting as a large abscess with gas, without prosthesis loosening. BMJ Case Rep 2013. 2013 doi: 10.1136/bcr-2013-201090. pii: Bcr2013201090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Klatte TO, Junghans K, Al-Khateeb H, Rueger JM, Gehrke T, Kendoff D, et al. Single-stage revision for peri-prosthetic shoulder infection: Outcomes and results. Bone Joint J. 2013;95-B:391–5. doi: 10.1302/0301-620X.95B3.30134. [DOI] [PubMed] [Google Scholar]
- 26.Wang B, Toye B, Desjardins M, Lapner P, Lee C. A 7-year retrospective review from 2005 to 2011 of Propionibacterium acnes shoulder infections in Ottawa, Ontario, Canada. Diagn Microbiol Infect Dis. 2013;75:195–9. doi: 10.1016/j.diagmicrobio.2012.10.018. [DOI] [PubMed] [Google Scholar]
- 27.Singh JA, Sperling JW, Schleck C, Harmsen WS, Cofield RH. Periprosthetic infections after total shoulder arthroplasty: A 33-year perspective. J Shoulder Elbow Surg. 2012;21:1534–41. doi: 10.1016/j.jse.2012.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Athwal GS, Sperling JW, Rispoli DM, Cofield RH. Deep infection after rotator cuff repair. J Shoulder Elbow Surg. 2007;16:306–11. doi: 10.1016/j.jse.2006.05.013. [DOI] [PubMed] [Google Scholar]
- 29.Herrera MF, Bauer G, Reynolds F, Wilk RM, Bigliani LU, Levine WN. Infection after mini-open rotator cuff repair. J Shoulder Elbow Surg. 2002;11:605–8. doi: 10.1067/mse.2002.127302. [DOI] [PubMed] [Google Scholar]
- 30.Berthelot P, Carricajo A, Aubert G, Akhavan H, Gazielly D, Lucht F. Outbreak of postoperative shoulder arthritis due to Propionibacterium acnes infection in nondebilitated patients. Infect Control Hosp Epidemiol. 2006;27:987–90. doi: 10.1086/507287. [DOI] [PubMed] [Google Scholar]
- 31.Murray MR, Saltzman MD, Gryzlo SM, Terry MA, Woodward CC, Nuber GW. Efficacy of preoperative home use of 2% chlorhexidine gluconate cloth before shoulder surgery. J Shoulder Elbow Surg. 2011;20:928–33. doi: 10.1016/j.jse.2011.02.018. [DOI] [PubMed] [Google Scholar]
- 32.Patel A, Calfee RP, Plante M, Fischer SA, Green A. Propionibacterium acnes colonization of the human shoulder. J Shoulder Elbow Surg. 2009;18:897–902. doi: 10.1016/j.jse.2009.01.023. [DOI] [PubMed] [Google Scholar]
- 33.Richards J, Inacio MC, Beckett M, Navarro RA, Singh A, Dillon MT, et al. Patient and procedure-specific risk factors for deep infection after primary shoulder arthroplasty. Clin Orthop Relat Res. 2014;472:2809–15. doi: 10.1007/s11999-014-3696-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Achermann Y, Sahin F, Schwyzer HK, Kolling C, Wüst J, Vogt M. Characteristics and outcome of 16 periprosthetic shoulder joint infections. Infection. 2013;41:613–20. doi: 10.1007/s15010-012-0360-4. [DOI] [PubMed] [Google Scholar]
- 35.Matsen FA, 3rd, Butler-Wu S, Carofino BC, Jette JL, Bertelsen A, Bumgarner R. Origin of Propionibacterium in surgical wounds and evidence-based approach for culturing Propionibacterium from surgical sites. J Bone Joint Surg Am. 2013;95:e1811–7. doi: 10.2106/JBJS.L.01733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Piper KE, Jacobson MJ, Cofield RH, Sperling JW, Sanchez-Sotelo J, Osmon DR, et al. Microbiologic diagnosis of prosthetic shoulder infection by use of implant sonication. J Clin Microbiol. 2009;47:1878–84. doi: 10.1128/JCM.01686-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mook WR, Garrigues GE. Diagnosis and management of periprosthetic shoulder infections. J Bone Joint Surg Am. 2014;96:956–65. doi: 10.2106/JBJS.M.00402. [DOI] [PubMed] [Google Scholar]
- 38.Grosso MJ, Frangiamore SJ, Ricchetti ET, Bauer TW, Iannotti JP. Sensitivity of frozen section histology for identifying Propionibacterium acnes infections in revision shoulder arthroplasty. J Bone Joint Surg Am. 2014;96:442–7. doi: 10.2106/JBJS.M.00258. [DOI] [PubMed] [Google Scholar]
- 39.Frangiamore SJ, Saleh A, Kovac MF, Grosso MJ, Zhang X, Bauer TW, et al. Synovial fluid interleukin-6 as a predictor of periprosthetic shoulder infection. J Bone Joint Surg Am. 2015;97:63–70. doi: 10.2106/JBJS.N.00104. [DOI] [PubMed] [Google Scholar]
- 40.Dodson CC, Craig EV, Cordasco FA, Dines DM, Dines JS, Dicarlo E, et al. Propionibacterium acnes infection after shoulder arthroplasty: A diagnostic challenge. J Shoulder Elbow Surg. 2010;19:303–7. doi: 10.1016/j.jse.2009.07.065. [DOI] [PubMed] [Google Scholar]
- 41.Schneeberger AG, Yian E, Steens W. Injection-induced low-grade infection of the shoulder joint: Preliminary results. Arch Orthop Trauma Surg. 2012;132:1387–92. doi: 10.1007/s00402-012-1562-z. [DOI] [PubMed] [Google Scholar]
- 42.Portillo ME, Salvadó M, Alier A, Sorli L, Martínez S, Horcajada JP, et al. Prosthesis failure within 2 years of implantation is highly predictive of infection. Clin Orthop Relat Res. 2013;471:3672–8. doi: 10.1007/s11999-013-3200-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Topolski MS, Chin PY, Sperling JW, Cofield RH. Revision shoulder arthroplasty with positive intraoperative cultures: The value of preoperative studies and intraoperative histology. J Shoulder Elbow Surg. 2006;15:402–6. doi: 10.1016/j.jse.2005.10.001. [DOI] [PubMed] [Google Scholar]
- 44.Kistowska M, Meier B, Proust T, Feldmeyer L, Cozzio A, Kuendig T, et al. Propionibacterium acnes promotes Th17 and Th17/Th1 responses in acne patients. J Invest Dermatol. 2015;135:110–8. doi: 10.1038/jid.2014.290. [DOI] [PubMed] [Google Scholar]
- 45.Wang Y, Kuo S, Shu M, Yu J, Huang S, Dai A, et al. Staphylococcus epidermidis in the human skin microbiome mediates fermentation to inhibit the growth of Propionibacterium acnes: Implications of probiotics in acne vulgaris. Appl Microbiol Biotechnol. 2014;98:411–24. doi: 10.1007/s00253-013-5394-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Furustrand Tafin U, Trampuz A, Corvec S. In vitro emergence of rifampicin resistance in Propionibacterium acnes and molecular characterization of mutations in the rpoB gene. J Antimicrob Chemother. 2013;68:523–8. doi: 10.1093/jac/dks428. [DOI] [PubMed] [Google Scholar]
- 47.Portillo ME, Corvec S, Borens O, Trampuz A. Propionibacterium acnes: An underestimated pathogen in implant-associated infections. Biomed Res Int. 2013;2013:804391. doi: 10.1155/2013/804391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kim SH, Wise BL, Zhang Y, Szabo RM. Increasing incidence of shoulder arthroplasty in the United States. J Bone Joint Surg Am. 2011;93:2249–54. doi: 10.2106/JBJS.J.01994. [DOI] [PubMed] [Google Scholar]
- 49.Saper D, Capiro N, Ma R, Li X. Management of Propionibacterium acnes infection after shoulder surgery. Curr Rev Musculoskelet Med. 2015;8:67–74. doi: 10.1007/s12178-014-9256-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Saltzman MD, Marecek GS, Edwards SL, Kalainov DM. Infection after shoulder surgery. J Am Acad Orthop Surg. 2011;19:208–18. doi: 10.5435/00124635-201104000-00005. [DOI] [PubMed] [Google Scholar]
- 51.Furustrand Tafin U, Corvec S, Betrisey B, Zimmerli W, Trampuz A. Role of rifampin against Propionibacterium acnes biofilm in vitro and in an experimental foreign-body infection model. Antimicrob Agents Chemother. 2012;56:1885–91. doi: 10.1128/AAC.05552-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lorenzetti AJ, Wongworawat MD, Jobe CM, Phipatanakul WP. Cyanoacrylate microbial sealant may reduce the prevalence of positive cultures in revision shoulder arthroplasty. Clin Orthop Relat Res. 2013;471:3225–9. doi: 10.1007/s11999-013-2854-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Saltzman MD, Nuber GW, Gryzlo SM, Marecek GS, Koh JL. Efficacy of surgical preparation solutions in shoulder surgery. J Bone Joint Surg Am. 2009;91:1949–53. doi: 10.2106/JBJS.H.00768. [DOI] [PubMed] [Google Scholar]
- 54.Maccioni CB, Woodbridge AB, Balestro JC, Figtree MC, Hudson BJ, Cass B, et al. Low rate of Propionibacterium acnes in arthritic shoulders undergoing primary total shoulder replacement surgery using a strict specimen collection technique. J Shoulder Elbow Surg. 2015;24:1206–11. doi: 10.1016/j.jse.2014.12.026. [DOI] [PubMed] [Google Scholar]


