Abstract
BACKGROUND:
Transanal endoscopic microsurgery is a minimally invasive technique that allows full-thickness resection and suture closure of the defect for large rectal adenomas, selected low-risk rectal cancers, or small cancers in patients who have a high risk for major surgery. Our aim, in the given prospective study was to report our initial clinical experience with TAMIS, and to evaluate its effects on postoperative anorectal functions.
MATERIALS AND METHODS:
In 10 patients treated with TAMIS for benign and malignant rectal tumors, preoperative and postoperative anorectal function was evaluated with anorectal manometry and Cleveland Clinic Incontinence Score.
RESULTS:
The mean distance of the tumors from the anal verge was 5.6 cm, and mean tumor diameter was 2.6 cm. All resection margins were tumor free. There was no difference in preoperative and 3-week postoperative anorectalmanometry findings; only mean minimum rectal sensory volume was lower at 3 weeks after surgery. The Cleveland Clinic Incontinence Score was normal in all patients except one which resolved by 6 weeks after surgery.The mean postoperative follow-up was 28 weeks without any recurrences.
CONCLUSION:
Transanal minimally invasive surgery is a safe and effective procedure for treatment of rectal tumors and can be performed without impairing anorectal functions.
Keywords: Rectum, cancer, adenoma, TAMIS, manometry
INTRODUCTION
Low rectal cancers and large benign rectal tumors that cannot be excised endoscopically are treated typically with abdominoperineal or low anterior resection.Transanal endoscopic microsurgery is a minimally invasive technique that allows full-thickness resection and suture closure of the defect for large rectal adenomas, selected low-risk rectal cancers, or small cancers in patients who have a high risk for major surgery.[1,2,3] The advantages of transanal endoscopic microsurgery over local excision include improved quality of resection, decreased frequency of local recurrence, and improved survival in patients who have early stage rectal cancer. Treatment of rectal tumors with transanal endoscopic microsurgery is safe and effective and has similar long-term morbidity and mortality as conventional transanal excision.[4,5,6] However, the world wide experience of transanal endoscopic microsurgery is limited because of the high cost of the specialized surgical equipment and the difficult learning curve of the procedure.[7,8,9] In addition, transanal endoscopic microsurgery commonly may be complicated by postoperative dysfunction of the anorectal sphincter.[10,11,12]
Transanal minimally invasive surgery (TAMIS) combines singleport access with the principles of transanal excision.[13] In this procedure, a single-incision laparoscopic surgery multichannel port is introduced into the anal canal, and transanal excision is performed with laparoscopic instruments. Following studies using the transanal single port reported that the procedure was effective and safe for excision of early rectal cancer and adenomas, with excellent visibility of the operative field and low morbidity. Compared with transanal endoscopic microsurgery, TAMIS has a shorter learning curve, faster device setup before surgery, lower cost, and easier surgical manipulation.[14,15,16,17] However, there is a lack of information about the effects of TAMIS on anorectal function in the literature. Our aim, in the presented prospective study was to report our initial clinical experience with TAMIS and to evaluate it's effects on postoperative anorectal functions.
MATERIALS AND METHODS
This prospective study was performed in 10 patients who were treated for benign and malignant rectal tumors with TAMIS between May and November 2013, and were not appropriate candidates for endoscopic lesion removal, because of the tumor size, localization, etc. All patients had endoscopic biopsy and pelvic phase-array magnetic resonance imaging scan for local staging. For patients with a biopsy-proven malignant lesion, treatment with TAMIS was offered only to patients with cT1cN0 invasive carcinoma, lesion diameter <3 cm, well-differentiated histology, the absence of lymphovascular invasion, and tumor grade 2 to 3. Institutional Review Board approval was obtained before starting the study and informed consent was obtained from all patients.
Data about patient demographics and characteristics of the lesion (location, maximum diameter, and distance to the anal verge), diagnoses from preoperative biopsy and final postoperative pathology, resection margins, operative time, and complications were recorded prospectively. Fecal incontinence severity was assessed using the validated Clevel and Clinic Incontinence Score questionnaire (possible score range: Normal continence, 0; complete incontinence, 20), which was completed by all patients before and at 3 weeks after surgery.[18]
The bowel preparation was performed the day before surgery (Phospho-Soda, CB Fleet Company, Lynchburg, VA), and patients were hospitalized on the day of surgery. Antibiotic prophylaxis included cefuroxime (1 g) and metronidazole (1 g) given intravenously before starting surgery. Surgery was performed with the patient in the lithotomy position under general anesthesia. A single-incision laparoscopic surgery port (SILS Port, Covidien, Mansfield, MA) was inserted into the anal canal and pneumorectum was established with carbon dioxide insufflation (pressure, 15 to 18 mmHg). Excision of the lesion was performed using basic laparoscopic instruments, a laparoscope (5 mm; 30°), and an ultrasonically activated scalpel (Harmonic Scalpel, 5 mm, Ethicon, Somerville, NJ). For all lesions, planned margins >1 cm were marked around the tumor with monopolar cautery, full-thickness excision was performed, and the defect was closed with absorbable monofilament sutures [Figure 1].
Figure 1.
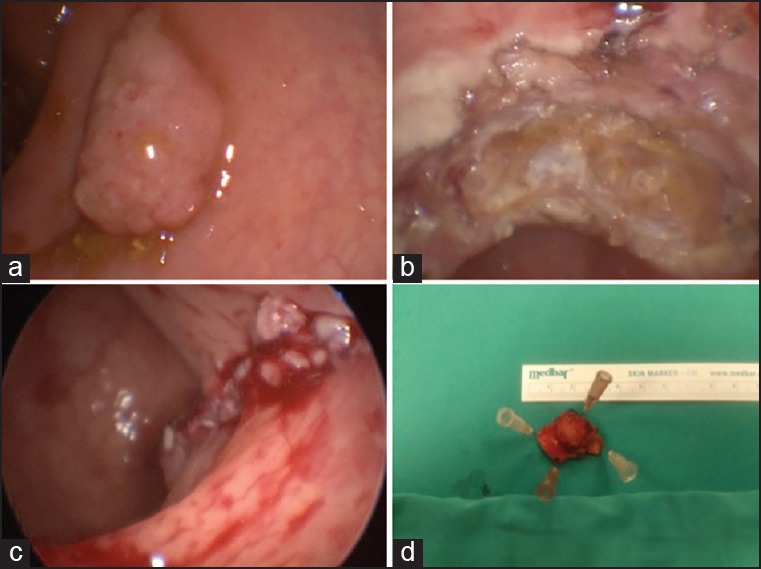
Transanal minimally invasive surgery for rectal tumors. Figures belong to patient number 5. (a) Endoscopic view of a tumor before excision, pre-operative biopsy revealed an intramucosal carcinoma pTis-cN0. (b) Endoscopic view of the full thickness excision area, perirectal fat is exposed. (c) Endoscopic view of the closed surgical defect with running sutures with regular straight laparoscopic needle holder. (d) Excised tumor: Margins are circumferentially tumor free, final histology showed a T1 adenocarcinoma
All patients were discharged from the hospital on the day after surgery and advised to maintain a soft diet for 3 days after surgery. Follow-up evaluation included digital examination at 1 week and proctoscopy at 3 weeks after surgery.
Anorectal manometry was performed before and at 3 weeks after surgery with a manometric sensor (external diameter, 2.1 mm) with four circular orifices and a latex microballoon (Solar GI High Resolution Anorectal Manometry, Medical Measurement Systems, Enschede, The Netherlands). Tracings and pressure contours were analyzed with software (Measurement and Analysis Software, Medical Measurement Systems). Anorectal manometric parameters were recorded including (1) mean resting anal pressure during an interval of 30 s; (2) maximum squeeze pressure recorded during maximal sphincter contractions (duration of each contraction, 5 s; average of three measurements); (3) squeeze endurance (the patient was asked to squeeze for as long as possible until sphincter pressure decreased to the baseline level or until 30 s had passed); and (4) minimum rectal sensory volume (the balloon in the rectum was inflated gradually and the patient was instructed to indicate the first sensation). Rectoanal inhibitory reflex with 50-cm3 rectal distention and sphincter reflex contractions during coughing were also evaluated in each patient.First urge and maximum tolerable volume were not measured because of potential risks of postoperative wound dehiscence.
Statistical analyses were performed with SPSS software (SPSS: An IBM Company, version 6.0, IBM Corporation, Armonk, NY, USA). Variables were reported as mean ± standard deviation or number (%). Statistical comparisons were made with t test. Statistical significance was defined by P ≤.05.
RESULTS
Mean age of the patients was 66 ± 10 (ranged between 51-84) years, and most patients had posterior or posterolateral rectal wall tumors [Table 1]. The mean distance of the tumor from the anal verge was 5.6 ± 2.4 (ranged between 3-10) cm. The mean tumor diameter was 2.6 ± 1.2 (ranged between 0.4-5) cm, and the mean distance of the tumor from there section margins was 7.2 ± 2.7 (ranged between 4-12) mm [Table 1].
Table 1.
Characteristics of tumors and patients who had transanal minimally invasive surgery for rectal tumors
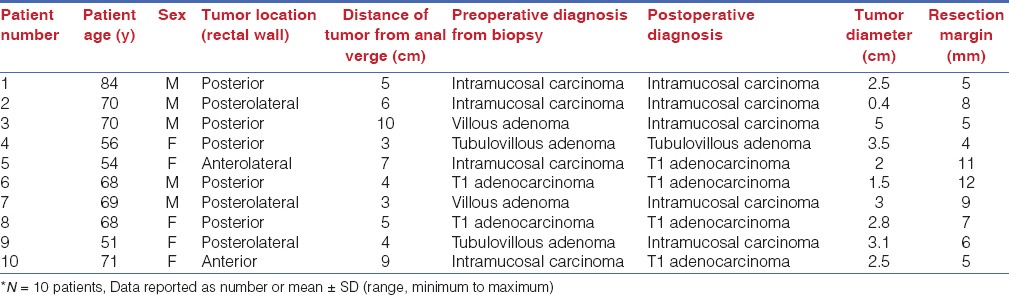
All patients were discharged from the hospital on the day after surgery except 1 man (age: 84 years) who had a preoperative diagnosis of sigmoid cancer and synchronous rectal intramucosal carcinoma [Table 1]; this patient had resection of the rectal tumor with TAMIS and laparoscopic anterior resection for the sigmoid cancer in the same operation (total operative time, 220 min), and he was discharged from the hospital on the seventh postoperative day without any complications.
The mean total operative time for the TAMIS procedure (including device setup and positioning of the patient) was 98.8 min (range, 45 to 185 min). The only technical difficulty during surgery was a temporary loss of pneumorectum in all operations.
Histology of the preoperative biopsy showed four benign lesions (two villous and two tubulovillous adenomas) and six malignant lesions [Table 1]. After resection of the rectal tumor with TAMIS, the postoperative pathologic diagnosis was different from the preoperative diagnosis in five patients, including three patients with preoperative diagnosis of adenomas (two villous and one tubulovillous) who had postoperative diagnosis of intramucosal carcinoma. Two other patients who had intramucosal carcinomas in preoperative biopsy were found to be a low-grade T1 adenocarcinoma with no lymphovascular invasion in the evaluation of extracted specimen [Table 1]. Overall, there were four patients who had postoperative T1 adenocarcinoma. The other two was preoperatively diagnosed with good histopathologic features which were confirmed by postoperative histologic evaluation. Preoperative magnetic resonance imaging scans for local tumor staging in these patients showed negative lymph nodes. All tumors were removed completely, with no tumor remaining at the macroscopic and histologic resection margins [Table 1].
All patients were completely continent before surgery according to CCIS (all scores = 0). Three weeks after surgery, one of the patients had a complaint of flatus incontinence and defecation urge. As this patient's postoperative score was 3, overall mean CCIS scores increased to 0.3 ± 0.68 at postoperative third week evaluation (P > 0.05). Six weeks after the surgery, this patient reported that the complaints were resolved.
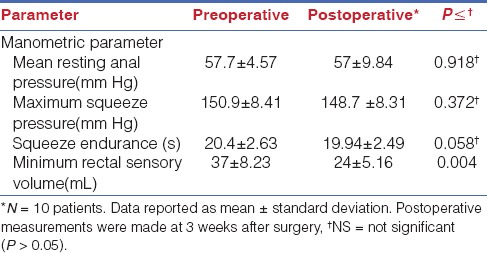
The preoperative and postoperative anorectal manometric parameters were normal for all patients, but mean minimum rectal sensory volume was significantly less at 3 weeks after, than before surgery [Table 2]. Rectoanal inhibitory reflex and sphincter reflex contractions were positive for all patients before and after surgery.
Table 2.
Anorectal manometry and clevel and clinic incontinence score before and after transanal minimally invasive surgery for rectal tumors
There were no perioperative complications. The most recent follow-up of all patients (mean, 27 week; range, 16 to 40 week) showed that no patients had any complications such as hemorrhage, suture dehiscence, leakage, or recurrence.
DISCUSSION
Rectal tumors located in the lower part of the rectum and the anal canal may be excised effectively using the transanal approach. However, transanal excision of rectal cancers, including stage I cancers may be associated with poor locoregional control.[19,20] In contrast, local excision with transanal endoscopic microsurgery on selected patients who have T1 rectal cancer may provide excellent survival, low frequency of recurrence, and outcomes comparable to those achieved with radical resection.[21,22] Transanal endoscopic microsurgery may enable more precise dissection by providing a better view of the surgical area, and this may explain the better recurrence-free survival with transanal endoscopic microsurgery than transanal excision.[3]
Surgeons may not have access to transanal endoscopic microsurgery equipment because of financial constraints, and/or flat or large tumors in the upper or middle third of the rectum may be unsuitable for colonoscopic polypectomy. In these cases, the surgeon may refer the patient to a specialized center for endoscopic treatment or may perform open or laparoscopic low anterior resection, even though the lesion may be treatable with local excision. Low anterior resection may be associated with major morbidity including anastomotic leak, sexual and urinary dysfunction, functional morbidity from a permanent colostomy, and mortality.[23,24,25] Transanal endoscopic microsurgery was the only surgical technique available for endoscopic resection of rectal tumors until TAMIS was described.[26] Increased used of TAMIS may be attributed, in part, to the low cost of TAMIS compared with transanal endoscopic microsurgery; the current hospital cost of a disposable laparoscopic surgery port, which is available in most laparoscopic surgery clinics, is approximately $500 (United States). In this study, we used TAMIS for lesions of the upper or middle third of the rectum because transanal endoscopic microsurgery equipment was not available in our hospital. Furthermore, in the 84-year-old man who had synchronous sigmoid and rectal cancer, the morbidity and mortality of a low anterior resection and stoma were avoided by removing the malignant rectal tumor with TAMIS.
In a previous study of the TAMIS procedure in 50 patients for treatment of benign and malignant rectal tumors, three patients (6%) had tumor at the resection margins (in two patients excision for a villous adenoma, and in one patient excision of a T2 adenocarcinoma); frequency of recurrence was 4%, including recurrence in two patients at 6 and 18 months after surgery.[27] Therefore, the frequency of tumor at the resection margins and recurrence were reported as similar between TAMIS and transanal endoscopic microsurgery.[22,27,28] In this study, all 10 patients had no tumor at the resection margins and all were recurrence free at the end of postoperative 28th week [Table 1]. We believe that, the advantage of TAMIS, providing wider visibility in the rectal lumen (36°) than transanal endoscopic microsurgery (22°) resulted with tumor free resection margins even for lower third rectal lesions. However, further study is justified to evaluate long-term follow-up after TAMIS.
The reported complications associated with the TAMIS procedure are infrequent and include minor complications such as suture dehiscence or rectal bleeding that were treated nonoperatively. Iatrogenic peritoneal entry during excision with TAMIS was reported for one patient, but it was also treated transanally without open surgery.[27,29] In this study, all 10 excisions had no perioperative or postoperative complications.
In most TAMIS procedures, technical difficulty may include loss of pneumorectum. Smoke formation during cauterization may impair visualization, and suction that is used to clear the smoke may cause loss of endoluminal pressure. Transanal endoscopic microsurgery enables controlled endoluminal pressure because the microsurgery device includes suction and insufflation systems. Although the loss of endoluminal pressure during TAMIS may have prolonged the operative time in the present study (mean, 99 min), the mean operative time was similar to that reported with transanal endoscopic microsurgery.[4]
Transanal endoscopic microsurgery includes the transanal insertion and repositioning of a rigid rectoscope (diameter, 40 mm). Therefore, anal dilation is necessary before starting transanal endoscopic microsurgery, and the anal sphincter remains dilated during the entire procedure. The rectoscope may damage the internal anal sphincter, and anorectal distension may damage the external anal sphincter. As a result, short-term anal dysfunction was reported after transanal endoscopic microsurgery.[10,11,12,30] This may include internal anal sphincter defects on endoanal ultrasonography in 29% patients, variable degrees of incontinence in21% patients, disturbed anorectal function in 50% patients at 3 weeks after the procedure, and decreased anal manometric parameters (anal resting pressure, squeeze pressure, threshold volume, maximum tolerable volume, and rectal compliance) at short-term follow-up.[10]
Hypothetically, TAMIS may result in less impairment of anal sphincter functions than TEM, as TAMIS port is flexible, soft, and smaller (diameter, 30 mm) and may enable safe and atraumatic transanal access without anal dilation. In the presented study, we used anorectal manometry which is an objective method to evaluate anorectal sphincter functions, as it is not easy to detect minor anorectal dysfunctions either clinically or by using specific continence questionnaires. Although the mean minimum rectal sensory volume was lower at 3 weeks after than before TAMIS, the other parameters were unchanged, and 9 of 10 patients had perfect continence score after TAMIS without any complaints [Table 2]. Rectal sensation and rectal wall compliance may affect continence control and may cause anorectal dysfunction including defecation urge and increased stool frequency. Decreased mean minimum rectal sensory volume after TAMIS [Table 2] may have been caused by the full-thickness excision and suture repair of the rectal wall in all patients. In the present study, only one patient had flatus incontinence and defecation urge after surgery; she had a 3.5-cm diameter tumor in the lower rectum that was removed with a negative resection margin, and the wide full-thickness resection may have changed rectal sensation and decreased the minimum rectal sensory volume. The clinical and manometric results suggest that the small, soft, and pliable port used in TAMIS did not cause anal sphincter dysfunction.
Limitations of the present study include the small number of patients, absence of endosonographic evaluation of sphincter integrity, and short follow-up. Despite these limitations, we recommend TAMIS as a safe, cost-effective, and efficient method for tumors that otherwise may be treated with transanal endoscopic microsurgery. The TAMIS may provide a high quality of resection without damaging the anal sphincter or impairing anorectal function. Larger, randomized, prospective studies are justified to evaluate long-term anorectal function and oncologic outcomes after TAMIS.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Langer C, Liersch T, Süss M, Siemer A, Markus P, Ghadimi BM, et al. Surgical cure for early rectal carcinoma and large adenoma: Transanal endoscopic microsurgery (using ultrasound or electrosurgery) compared to conventional local and radical resection. Int J Colorectal Dis. 2003;18:222–9. doi: 10.1007/s00384-002-0441-4. [DOI] [PubMed] [Google Scholar]
- 2.Buess G. Review: Transanal endoscopic microsurgery (TEM) J R Coll Surg Edinb. 1993;38:239–45. [PubMed] [Google Scholar]
- 3.Saclarides TJ, Smith L, Ko ST, Orkin B, Buess G. Transanal endoscopic microsurgery. Dis Colon Rectum. 1992;35:1183–91. doi: 10.1007/BF02251975. [DOI] [PubMed] [Google Scholar]
- 4.Guerrieri M, Baldarelli M, Morino M, Trompetto M, Da Rold A, Selmi I, et al. Transanal endoscopic microsurgery in rectal adenomas: Experience of six Italian centres. Dig Liver Dis. 2006;38:202–7. doi: 10.1016/j.dld.2005.11.014. [DOI] [PubMed] [Google Scholar]
- 5.Zacharakis E, Freilich S, Rekhraj S, Athanasiou T, Paraskeva P, Ziprin P, et al. Transanal endoscopic microsurgery for rectal tumors: The St. Mary's experience. Am J Surg. 2007;194:694–8. doi: 10.1016/j.amjsurg.2007.03.005. [DOI] [PubMed] [Google Scholar]
- 6.Nash GM, Weiser MR, Guillem JG, Temple LK, Shia J, Gonen M, et al. Long-term survival after transanal excision of T1 rectal cancer. Dis Colon Rectum. 2009;52:577–82. doi: 10.1007/DCR.0b013e3181a0adbd. [DOI] [PubMed] [Google Scholar]
- 7.Maslekar S, Pillinger SH, Sharma A, Taylor A, Monson JR. Cost analysis of transanal endoscopic microsurgery for rectal tumours. Colorectal Dis. 2007;9:229–34. doi: 10.1111/j.1463-1318.2006.01132.x. [DOI] [PubMed] [Google Scholar]
- 8.Koebrugge B, Bosscha K, Ernst MF. Transanal endoscopic microsurgery for local excision of rectal lesions: Is there a learning curve? Dig Surg. 2009;26:372–7. doi: 10.1159/000257228. [DOI] [PubMed] [Google Scholar]
- 9.Middleton PF, Sutherland LM, Maddern GJ. Transanal endoscopic microsurgery: A systematic review. Dis Colon Rectum. 2005;48:270–84. doi: 10.1007/s10350-004-0804-8. [DOI] [PubMed] [Google Scholar]
- 10.Herman RM, Richter P, Walega P, Popiela T. Anorectal sphincter function and rectal barostat study in patients following transanal endoscopic microsurgery. Int J Colorectal Dis. 2001;16:370–6. doi: 10.1007/s003840100325. [DOI] [PubMed] [Google Scholar]
- 11.Kennedy ML, Lubowski DZ, King DW. Transanal endoscopic microsurgery excision: Is anorectal function compromised? Dis Colon Rectum. 2002;45:601–4. doi: 10.1007/s10350-004-6252-7. [DOI] [PubMed] [Google Scholar]
- 12.Wang HS, Lin JK, Yang SH, Jiang JK, Chen WS, Lin TC. Prospective study of the functional results of transanal endoscopic microsurgery. Hepatogastroenterology. 2003;50:1376–80. [PubMed] [Google Scholar]
- 13.Atallah S, Albert M, Larach S. Transanal minimally invasive surgery: A giant leap forward. Surg Endosc. 2010;24:2200–5. doi: 10.1007/s00464-010-0927-z. [DOI] [PubMed] [Google Scholar]
- 14.Lim SB, Seo SI, Lee JL, Kwak JY, Jang TY, Kim CW, et al. Feasibility of transanalminimally invasive surgery for mid-rectal lesions. Surg Endosc. 2012;26:3127–32. doi: 10.1007/s00464-012-2303-7. [DOI] [PubMed] [Google Scholar]
- 15.Ragupathi M, Haas EM. Transanal endoscopic video-assisted excision: Application of single-port access. JSLS. 2011;15:53–8. doi: 10.4293/108680810X12924466009005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lorenz C, Nimmesgern T, Langwieler TE. Transanal endoscopic surgery using different single-port devices. Surg Technol Int. 2011;21:107–11. [PubMed] [Google Scholar]
- 17.Van den Boezem PB, Kruyt PM, Stommel MW, Tobon Morales R, Cuesta MA, Sietses C. Transanal single-port surgery for the resection of large polyps. Dig Surg. 2011;28:412–6. doi: 10.1159/000334882. [DOI] [PubMed] [Google Scholar]
- 18.Rockwood TH, Church JM, Fleshman JW, Kane RL, Mavrantonis C, Thorson AG, et al. Patient and surgeon ranking of the severity of symptoms associated with fecal incontinence: The fecal incontinence severity index. Dis Colon Rectum. 1999;42:1525–32. doi: 10.1007/BF02236199. [DOI] [PubMed] [Google Scholar]
- 19.You YN, Baxter NN, Stewart A, Nelson H. Is the increasing rate of local excision for stage I rectal cancer in the United States justified?: A nationwide cohort study from the National Cancer Database. Ann Surg. 2007;245:726–33. doi: 10.1097/01.sla.0000252590.95116.4f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Endreseth BH, Myrvold HE, Romundstad P, Hestvik UE, Bjerkeset T, Wibe A, et al. Transanal excision vs. major surgery for T1 rectal cancer. Dis Colon Rectum. 2005;48:1380–8. doi: 10.1007/s10350-005-0044-6. [DOI] [PubMed] [Google Scholar]
- 21.Winde G, Nottberg H, Keller R, Schmid KW, Bünte H. Surgical cure for early rectal carcinomas (T1). Transanal endoscopic microsurgery vs. anterior resection. Dis Colon Rectum. 1996;39:969–76. doi: 10.1007/BF02054683. [DOI] [PubMed] [Google Scholar]
- 22.Heintz A, Mörschel M, Junginger T. Comparison of results after transanal endoscopic microsurgery and radical resection for T1 carcinoma of the rectum. Surg Endosc. 1998;12:1145–8. doi: 10.1007/s004649900802. [DOI] [PubMed] [Google Scholar]
- 23.Havenga K, Enker WE, McDermott K, Cohen AM, Minsky BD, Guillem J. Male and female sexual and urinary function after total mesorectal excision with autonomic nerve preservation for carcinoma of the rectum. J Am Coll Surg. 1996;182:495–502. [PubMed] [Google Scholar]
- 24.Karanjia ND, Corder AP, Bearn P, Heald RJ. Leakage from stapled low anastomosis after total mesorectal excision for carcinoma of the rectum. Br J Surg. 1994;81:1224–6. doi: 10.1002/bjs.1800810850. [DOI] [PubMed] [Google Scholar]
- 25.MacFarlane JK, Ryall RD, Heald RJ. Mesorectal excision for rectal cancer. Lancet. 1993;341:457–60. doi: 10.1016/0140-6736(93)90207-w. [DOI] [PubMed] [Google Scholar]
- 26.Azimuddin K, Riether RD, Stasik JJ, Rosen L, Khubchandani IT, Reed JF., 3rd Transanal endoscopic microsurgery for excision of rectal lesions: Technique and initial results. Surg Laparosc Endosc Percutan Tech. 2000;10:372–8. [PubMed] [Google Scholar]
- 27.Albert MR, Atallah SB, deBeche-Adams TC, Izfar S, Larach SW. Transanal minimally invasive surgery (TAMIS) for local excision of benign neoplasms and early-stage rectal cancer: Efficacy and outcomes in the first 50 patients. Dis Colon Rectum. 2013;56:301–7. doi: 10.1097/DCR.0b013e31827ca313. [DOI] [PubMed] [Google Scholar]
- 28.Moore JS, Cataldo PA, Osler T, Hyman NH. Transanal endoscopic microsurgery is more effective than traditional transanal excision for resection of rectal masses. Dis Colon Rectum. 2008;51:1026–30. doi: 10.1007/s10350-008-9337-x. [DOI] [PubMed] [Google Scholar]
- 29.Sevá-Pereira G, Trombeta VL, CapochimRomagnolo LG. Transanal minimally invasive surgery (TAMIS) using a new disposable device: Our initial experience. Tech Coloproctol. 2014;18:393–7. doi: 10.1007/s10151-013-1036-5. [DOI] [PubMed] [Google Scholar]
- 30.Kreis ME, Jehle EC, Haug V, Manncke K, Buess GF, Becker HD, et al. Functional results after transanal endoscopic microsurgery. Dis Colon Rectum. 1996;39:1116–21. doi: 10.1007/BF02081411. [DOI] [PubMed] [Google Scholar]


