Abstract
Persistent Mullerian duct syndrome (PMDS) is one of the three rare intersex disorders caused by defective anti-mullerian hormone or its receptor, characterized by undescended testes with presence of underdeveloped derivatives of mullerian duct in genetically male infant or adult with normal external genitals and virilization. This population will essentially have normal, 46(XY), phenotype. We hereby present a case of PMDS, presented with incarcerated left inguinal hernia associated with cryptorchidism and seminoma of right testes. Patient underwent laparoscopic hernia repair with bilateral orchidectomy and hysterectomy with uneventful postoperative recovery. Here we highlight the importance of minimal access approach for this scenario in terms of better visualization, less blood loss, combining multiple procedures along with early return to work and excellent cosmetic outcome.
Keywords: Hysterectomy, laparoscopic surgery, orchidectomy, Persistent Mullerian duct syndrome, seminoma testes
INTRODUCTION
There are three conditions of intersex associated with persistence of derivatives of mullerian duct: Persistent Mullerian duct syndrome (PMDS), mixed gonadal dysgenesis, and dysenteric male pseudo-hermaphroditism.[1] PMDS is typically characterized by undescended testes with presence of small underdeveloped uterus in genetically male infant or adult with normal external genitals and virilization. The condition is usually detected during evaluation for undescended testes/infertility or during surgery for other abdominal condition. Treatment is controversial, and various treatment options include gonadal biopsy, orchidopexy, orchidectomy, excision of derivatives of mullerian duct, etc. Laparoscopy is very useful in such cases as it is diagnostic and therapeutic at the same time and also offers advantages of minimally invasive approach. We hereby report a rare case of PMDS with left inguinal hernia along with seminoma of right testes managed by laparoscopic approach.
CASE REPORT
A 38-year-old male was evaluated in an emergency department for a painful swelling in left inguinal region for 5 days. Swelling was reducible initially for about 1-year. Detailed history, revealed associated infertility, investigated elsewhere having 14 years of married life. He reported normal sexual activity and had well developed secondary sexual characters with male pattern voice. Per abdominal examination was unremarkable. On genital examination, he had male genitals with normal appearing penis along with bilaterally undescended testes and underdeveloped scrotum. He also had left sided complete inguinal hernia, which was partially reducible without any signs of strangulation. On reviewing old medical records, it was found that he had bilateral intra-abdominal testes with presence of rudimentary uterus. Semen analysis showed aspermia. Karyotyping analysis detected 46(XY) chromosome pattern. Cross-sectional imaging confirmed presence of the uterus with bilateral intra-abdominal testes located along the iliac vessels [Figure 1].
Figure 1.
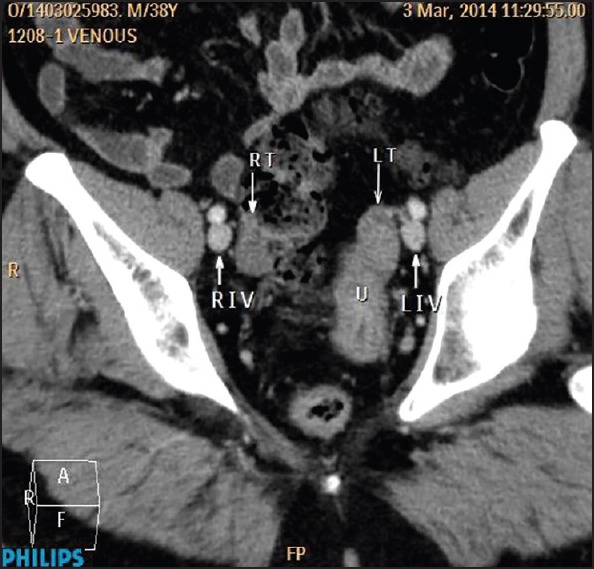
Multi-detector computed tomography pelvis: Oblique coronal section showing presence of bilateral intra-abdominal testes with uterus. RT – right testes, LT – left testes, U – uterus, RIV – right iliac vessels, LIV – left iliac vessels
Patient planned for diagnostic laparoscopy with bilateral orchidectomy and possible hysterectomy with hernia repair. Patient and family were explained regarding condition, and informed consent was obtained. Diagnostic laparoscopy revealed presence of small underdeveloped uterus with bilateral adenexa and undescended testes [Figure 2a]. There was the presence of left indirect inguinal hernia with omentum herniating into the sac [Figure 2b]. Subsequently, hernial contents were reduced, and laparoscopic hysterectomy with bilateral orchidectomy was performed. This was followed by trans-abdominal preperitoneal mesh repair of left inguinal hernia. Specimen retrieved via small pfannenstiel incision. Operating time was 190 min with 50 ml blood loss. Postoperatively liquids started after 6 h and diet started the next day. Patient was discharged on 2nd postoperative day without any complications.
Figure 2.
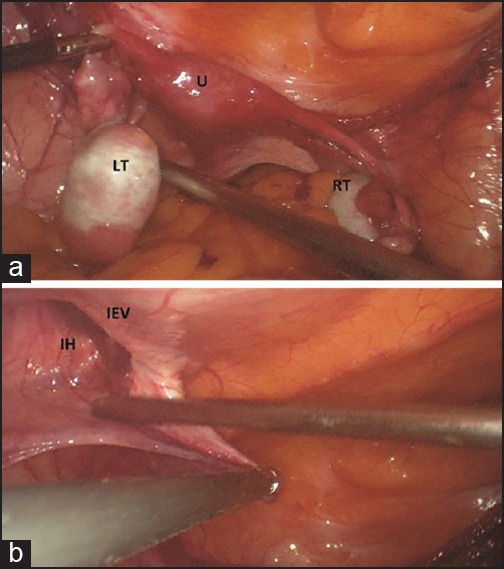
Intra-operative picture: (a) Presence of underdeveloped uterus with bilateral adenexa and bilateral undescended testes. RT – right testes, LT – left testes, U – uterus. (b) Presence of left inguinal hernia (after reducing contents). IH – indirect inguinal hernia, IEV – inferior epigastric vessels
Histopathological analysis showed the presence of rudimentary uterus with cervix. Both testes showed presence of atrophic seminiferous tubules without any evidence of spermatogenesis. Surprisingly, section from right testes had showed presence of seminoma, stage I, which was confirmed by immunohistochemistry. Based on clinical examination, intra-operative findings and histological features, we propose a diagnosis of PMDS.
DISCUSSION
Persistent Mullerian duct syndrome is an uncommon variety of pseudo-hermaphroditism seen in phenotypically normal males with chromosome 46, XY. This condition occurs due failure of fetal anti-mullerian hormone (AMH) to induce regression of mullerian ducts either due to mutation in gene coding for AMH (chromosome 19) or AMH receptors (chromosome 12). The syndrome can be sporadic or inherited in an autosomal recessive manner.[2] These individuals develop testes and have normal androgenic function with the development of near normal Wolffian duct derivatives and normal external genitals. Interestingly, all of them have either unilateral or bilateral undescended testes, probably due to close structural relationship between the gonad and the retained mullerian duct structures and sometimes it is associated with inguinal hernia as in this case. Almost always there is presence either of derivatives of mullerian duct, that is, uterus, cervix and fallopian tubes, sometimes pulled inside ipsilateral or contralateral inguinal canal, condition referred to as hernia uteri inguinalis.[3] Few cases of preserved fertility in PMDS have been reported, however, infertility is common due to chronic cryptorchidism and obstruction of vas deference or other parts of male excretory ducts. There is a definite risk of malignant transformation in undescended testes as seen in cases of cryptorchidism. Malignant transformation of mullerian duct derivatives is rare with only two cases reported in the literature.[4,5]
Surgical management of this condition is controversial and depends on the status of the gonads, degree of development of the mullerian derivatives, fertility, and age of the patient.[6] Orchidopexy is the primary treatment in infants and children. Derivatives of mullerian ducts are carefully excised to preserve vas and to improve the chances of fertility. Orchidectomy is advised for testes that cannot be mobilized out of the inguinal canal so also for an adult where the risk of malignant transformation of the undescended testis is high.[7] In this patient, decision for orchidectomy was taken in view of high risk of malignancy which was subsequently proved to be present on histopathological analysis, while excision of the mullerian derivatives was based on the facts that apart from it being a rudimentary and nonfunctional organ, there is a small but definite risk of malignant change.
To conclude, in given scenario laparoscopy has offered a unique advantage in terms of better visualization, less blood loss, combining multiple procedures along with early return to work and excellent cosmetic outcome.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Rappaport R, Forest MG. Disorders of sexual differentiation. In: Bertrand J, Rappaport R, Gizonenko PC, editors. Pediatric Endocrinology. Baltimore, Tokyo: Williams & Wilkins; 1993. pp. 447–70. [Google Scholar]
- 2.Imbeaud S, Belville C, Messika-Zeitoun L, Rey R, di Clemente N, Josso N, et al. A 27 base-pair deletion of the anti-müllerian type II receptor gene is the most common cause of the persistent müllerian duct syndrome. Hum Mol Genet. 1996;5:1269–77. doi: 10.1093/hmg/5.9.1269. [DOI] [PubMed] [Google Scholar]
- 3.Berkmen F. Persistent müllerian duct syndrome with or without transverse testicular ectopia and testis tumours. Br J Urol. 1997;79:122–6. doi: 10.1046/j.1464-410x.1997.27226.x. [DOI] [PubMed] [Google Scholar]
- 4.Shinmura Y, Yokoi T, Tsutsui Y. A case of clear cell adenocarcinoma of the müllerian duct in persistent müllerian duct syndrome: The first reported case. Am J Surg Pathol. 2002;26:1231–4. doi: 10.1097/00000478-200209000-00014. [DOI] [PubMed] [Google Scholar]
- 5.Thiel DD, Erhard MJ. Uterine adenosarcoma in a boy with persistent müllerian duct syndrome: First reported case. J Pediatr Surg. 2005;40:e29–31. doi: 10.1016/j.jpedsurg.2005.05.071. [DOI] [PubMed] [Google Scholar]
- 6.Vandersteen DR, Chaumeton AK, Ireland K, Tank ES. Surgical management of persistent müllerian duct syndrome. Urology. 1997;49:941–5. doi: 10.1016/s0090-4295(97)00104-0. [DOI] [PubMed] [Google Scholar]
- 7.Loeff DS, Imbeaud S, Reyes HM, Meller JL, Rosenthal IM. Surgical and genetic aspects of persistent müllerian duct syndrome. J Pediatr Surg. 1994;29:61–5. doi: 10.1016/0022-3468(94)90525-8. [DOI] [PubMed] [Google Scholar]


