Abstract
A 55-year-old man with no medical history of relevance was referred to our department for chronic back pain. Plain radiographs of the abdomen showed a round calcified image with liquid level inside in the upper-left quadrant. On computed tomography (CT) a bulky solid-cystic mass with calcified wall of 65 × 34 mm was shown in the left adrenal gland with no-contrast enhancement. The patient underwent a laparoscopic approach. Intraoperatively there was a large hard stony mass depending on the left adrenal gland, which was entirely supplanted by the tumor. Complete excision was done. The patient underwent uneventful recovery. Histopathology examination showed a solid-cystic mass with a thick fibrous wall and calcified areas compatible with hydatid cyst. To date there have been published few cases of adrenal hydatid cyst. To our awareness it is the fourth case issued in all literature resected by the laparoscopic approach.
Keywords: Adrenal gland, hydatic cyst, laparoscopy
INTRODUCTION
Echinococcosis is a zoonotic disease caused by E. Granulosus. Humans are an intermediate host that became infected due to the ingestion of echinococcal eggs excreted in animal's feces.
Later, the larvae produce cysts that can grow until discovered incidentally or until they become symptomatic.
Commonly hydatid cysts can be found in the liver or lungs. But, although rare they can appear in any organ. The adrenal gland is considered an exceptional location. The reported incidence is 0,5%.[1]
We present a symptomatic patient with a hydatid cyst in the left adrenal gland.
CASE REPORT
A 55-year-old man with no medical history of relevance was referred to our department for chronic back pain. Plain radiographs of the abdomen showed a round calcified image with liquid level inside in the upper-left quadrant of the abdomen [Figures 1a and b]. Chest X-ray was normal. CT scan showed a solid-cystic mass with calcified wall of 65 × 34 mm in the left adrenal gland without contrast enhancement suggestive of adrenal echinococcosis [Figure 1c]. Also a calcified granuloma was found at the upper lobe of the left lung.
Figure 1.
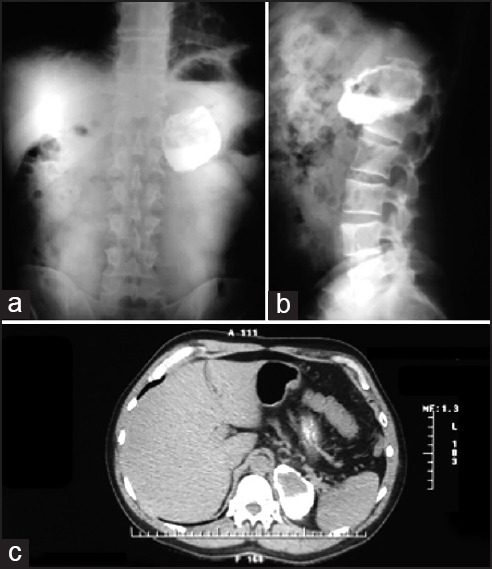
(a-b) Plain radiographs of the abdomen. Calcified image with liquid level inside in the upper-left quadrant of the abdomen (c) CT bulky solid-cystic mass with calcified wall of 65 × 34 mm in the left adrenal gland without enhancement after iv media contrast injection
The patient was in good general status. Hormonal profiles were within normal limits. Serology for E. granulosus was negative and Mantoux test was 12 mm.
Laparoscopic approach was done and the abdominal cavity was explored showing no abnormalities. A large hard stony mass entirely supplanting the left adrenal gland was found [Figure 2a]. After identification the adrenal vessels complete excision was done [Figure 2b–d]. Postoperative course was uneventful being discharged on postoperative day 2.
Figure 2.
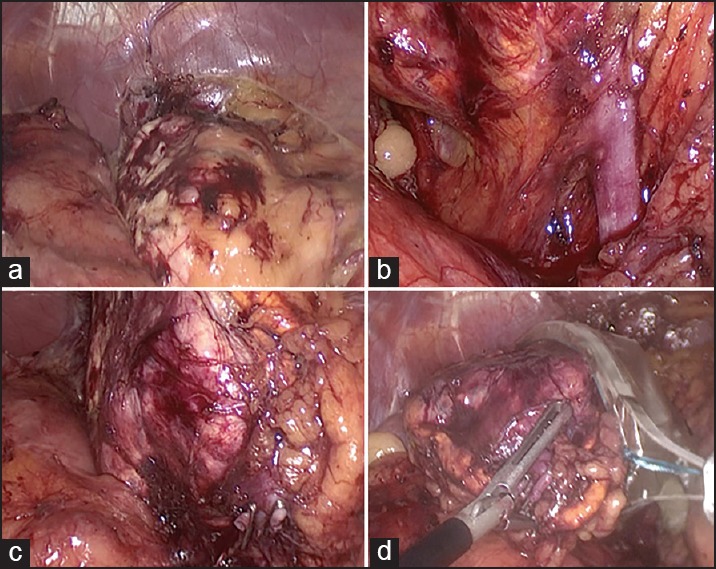
(a) Left adrenal gland entirely supplanted by a large hard stony-calcified mass (b) Left adrenal vein (c) Adrenal vein ligated and divided. (d) Removal of the hydatic cyst in an endobag
Pathological analysis confirmed the diagnosis. Macroscopic examination showed a solid-cystic mass of 5,5 × 3 cm with a thick fibrous wall and calcified areas. Examination of the content of the cyst showed a clear fluid with sandy material and calcified bodies. Protoscolices were present.
DISCUSSION
Hydatid cysts of the adrenal gland are extremely rare and account for 6% of all cystic tumors of the adrenal glands.[1,2] Most of the time are asymptomatic due to its slowly growth and are usually discovered incidentally.[2] The expansion of the cyst and the inflammatory reaction around it can irritate the peritoneum and cause flank pain such as in out patient. The major complication is the rupture of the cyst leading to an anaphylactic shock. I can rarely be associated with arterial hypertension (Goldblatt phenomenon).[3]
Serological tests are useful in the diagnosis of the disease but the sensitivity is determined by the site and condition of the cyst.[1,4] Location of the hydatid cysts in lungs, spleen, or kidneys are associated with lower quantity of antigens and therefore a lower quantity of antibodies.[1] This situation can lead to a false negative result.
Radiologic findings can range from cystic lesions (like the case presented) to a complete solid appearance. The World Health Organization has proposed a classification based on the US characteristics of the cyst.[1] The case described in our report is a type 5 (cyst with a thick calcified wall). CT scan showing fluid content within a cyst with a calcified wall and no-contrast enhancement is very suggestive of hydatid cyst.[4] Diagnosis can be made on US and CT findings.
Antihelmintic agents are used in endemic areas to treat systemic echinococcosis. But the results of treatment with albendazole or mebendazole in single lesions are not satisfactory and should be used in inoperable patients or in the case of a disseminated disease.[1,5]
Surgery remains the mainstay for the treatment of adrenal cysts and total excision is recommended. Despite being curative, surgery not always prevents a recurrence. Most authors suggest performing the resection of both the adrenal gland and cyst in large hydatid cyst because usually the gland is supplanted or destroyed by the cyst.[6] The laparoscopic approach is a reasonable procedure giving the low rates of morbidity and complications in experienced surgeons.
Although the hydatid cyst is a relative contraindication of the laparoscopy approach because of the risk of rupture and peritoneal dissemination, cyst image of our patient did not seem to be complicated, being extremely low the risks of breakage. Finally, the decision of laparoscopic approach was made on the presence of a single lesion with benign characteristics, well-defined margins, and complete plane between the cyst and adjacent structures.
In conclusion, adrenal location of hydatid cyst is rare but should be take into account when presented in endemic areas or in patients with history of hydatid disease.[4] Total surgical excision of the cyst is the treatment of choice with preservation of the adrenal gland. When this is not possible total adrenalectomy is recommended.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Dionigi G, Carrafiello G, Recaldini C, Sessa F, Boni L, Rovera F, et al. Laparoscopic resection of a primary hydatid cyst of the adrenal gland: A case report. J Med Case Rep. 2007;1:61. doi: 10.1186/1752-1947-1-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Defechereux T, Sauvant J, Gramatica L, Puccini M, De Micco C, Henry JF. Laparoscopic resection of an adrenal hydatid cyst. Eur J Surg. 2000;166:900–2. doi: 10.1080/110241500447317. [DOI] [PubMed] [Google Scholar]
- 3.Escudero MD, Sabater L, Calvete J, Campos B, Labios M, Lledo S. Arterial hypertension due to primary adrenal hydatid cyst. Surgery. 2002;132:984–5. doi: 10.1067/msy.2002.119313. [DOI] [PubMed] [Google Scholar]
- 4.Kumar S, Nanjappa B, Gowda KK. Laparoscopic management of a hydatid cyst of the adrenal gland. Korean J Urol. 2014;55:493–5. doi: 10.4111/kju.2014.55.7.493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Saimot AG. Medical treatment for liver hydatidosis. World J Surg. 2001;25:15–20. doi: 10.1007/s002680020003. [DOI] [PubMed] [Google Scholar]
- 6.Akcay MN, Akcay G, Balik AA, Boyuk A. Hydatid cysts of the adrenal gland: Review of nine patients. World J Surg. 2004;28:97–9. doi: 10.1007/s00268-003-6901-3. [DOI] [PubMed] [Google Scholar]


