Abstract
Background
Hyperthyroidism is known to induce a hypercoagulable state. It stimulates plasma levels of procoagulative factors and reduces fibrinolytic activity. So far most of the data have been derived from patients with endogenous hyperthyroidism with a wide variability in the underlying pathogenesis and severity of the disease.
Objectives
In this study we experimentally induced thyrotoxicosis in healthy volunteers to explore the effects of thyroxine excess on the plasma proteome. Using a shotgun proteomics approach, the abundance of plasma proteins was monitored before, during and after thyrotoxicosis.
Methods
Sixteen healthy male subjects were sampled at baseline, 4 and 8 weeks under 250 µg/day thyroxine p.o., as well as 4 and 8 weeks after stopping the application. Plasma proteins were analyzed after depletion of 6 high-abundance proteins (MARS6) by LC-ESI-MS/MS mass spectrometry. Mass spectrometric raw data were processed using a label-free, intensity-based workflow. Subsequently, the linear dependence between protein abundances and fT4 levels were calculated using a Pearson correlation.
Results
All subjects developed biochemical thyrotoxicosis, and this effect was reversed within the first 4 weeks of follow-up. None of the volunteers noticed any subjective symptoms. Levels of 10 proteins involved in the coagulation cascade specifically correlated with fT4, supporting an influence of thyroid hormone levels on blood coagulation even at nonpathological levels.
Conclusions
The results suggest that experimental thyrotoxicosis exerts selective and specific thyroxine-induced effects on coagulation markers. Our study design allows assessment of thyroid hormone effects on plasma protein levels without secondary effects of other diseases or therapies.
Key Words: Plasma, Shotgun proteomics, Label-free quantification, Free thyroxine, Coagulation
Introduction
Since the first report more than a century ago, a relation between hyperthyroidism and hypercoagulation has been suspected [1]. This has been further substantiated in a number of recent studies where patients with various causes and a variable duration of endogenous hyperthyroidism have been investigated as to their coagulation system under basal conditions and following treatment to the euthyroid state. These data show that thyrotoxicosis stimulates several procoagulatory and fibrinolytic factors, namely factor VIII (FVIII), factor IX (FIX) and von Willebrand factor. In parallel, reduced fibrinolytic activity based on an increased level of plasminogen activator inhibitor I (PAI-I) has been reported [2]. Interestingly, clot lysis time decreased during normalizing thyroid function. A recent study applying confocal and electron microscopy to evaluate clot structure supported more compact clots in the hyperthyroid state [3]. Despite these clear effects in many published reports included in a recent large systematic meta-analysis, the authors concluded that ‘the majority of these studies suffer of major methodological flaws which leaves the net effect of thyroid hormone excess on the haemostatic system unclear’ [2]. Particularly, the mechanism mediating the influence of thyroid hormones on the coagulation system has not been elucidated yet.
Due to the effect of thyroid hormones on several fibrinolytic and coagulation parameters, plasma proteins have been seen as important factors in several clinical studies [2]. However, the impact of thyroid hormone levels on the total plasma protein pattern representing classical plasma proteins produced in the liver, as well as leakage proteins from tissues and organs as well as cytokines, is also of general interest [4]. Since blood is an easily accessible biofluid that reflects the systemic health status of a patient and is routinely collected for clinical diagnostics, plasma is a prime source for the identification of biomarker candidates with diagnostic and prognostic value. With the maturing of mass spectrometry techniques and data analysis workflows, proteomics can now be used as a tool to disclose biomarker candidates in plasma by performing nontargeted comprehensive analysis of plasma-derived peptides and proteins. After depletion of highly abundant proteins, hundreds of proteins can be identified and quantified.
The data of the studies on impact of thyroid hormones on plasma composition described above indicate that the clinical situation may be obscured by associated factors not well controlled so far. The investigation presented here tried to avoid these pitfalls by profiling pure thyroxine-related effects during experimentally induced thyrotoxicosis in otherwise healthy volunteers. By using an unsupervised proteomic approach, we further tried to avoid any preselection of factors and instead aimed at an unbiased view of thyroid hormone-mediated effects.
Material and Methods
Study Design and Sampling
Sixteen healthy male volunteers were prescribed 0.25 mg of levothyroxine per day with blood withdrawal at baseline, 4 and 8 weeks under T4 administration, and 4 and 8 weeks after stopping the application. Subjects were aged 27.75 ± 3.9 years and had a BMI of 21-30. For the different analysis methods, serum and EDTA plasma were stored at −80°C. This work was approved by the local ethics committee and written informed consent was obtained from all participants.
Assays
Serum levels of thyrotropin [i.e. thyroid-stimulating hormone (TSH)], free triiodothyronine (fT3) and free thyroxine (fT4) were measured using immunoassays. Sex hormone-binding globulin (SHBG) as well as FIX and FXIII subunit B concentrations were determined in EDTA plasma using a chemiluminescent enzyme immunoassay (detailed description in suppl. methods, for all online suppl. material, see www.karger.com/doi/10.1159/000381769).
Depletion of High-Abundance Proteins and Sample Preparation of EDTA Plasma
Depletion of the 6 high-abundance proteins was performed via multiaffinity chromatography (MARS6-human; Agilent Technologies, Waldbronn, Germany) according to the manufacturer's protocol. The nonbound fraction containing lower-abundance plasma proteins was precipitated with trichloroacetic acid (final concentration 15%), and the pellet was resuspended in 100 µl of UT-buffer (8 M urea and 2 M thiourea). Protein concentrations were determined using a Bradford Assay (Bio-Rad Laboratories, Munich, Germany) with bovine serum albumin as the standard protein.
Protein Identification and Quantification
Mass spectrometric analysis of tryptic peptide lysates was performed on an Orbitrap Velos Mass Spectrometer (Thermo Electron, Bremen, Germany) after prefractionation by RP-HPLC as described [5]. The obtained raw data were analyzed using the Refiner MS software version 7.6.6 (GeneData, Basel, Switzerland). For further details of sample preparation, protein identification and quantification, see the online supplementary methods.
Results
Subject Characteristics
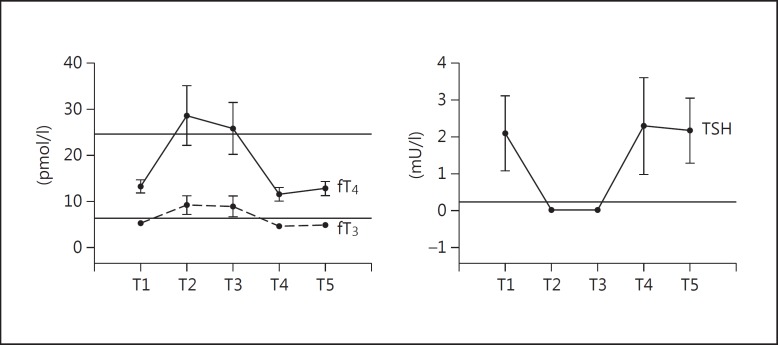
After 4 weeks of treatment with levothyroxine (time point 2 = T2), the mean fT4 levels rose from 13.24 ± 0.35 pmol/l (baseline = T1) to 28.6 ± 1.63 pmol/l, associated with an increase in the fT3 levels from 5.26 ± 0.13 to 9.19 ± 0.5 pmol/l. TSH was 2.1 ± 0.25 mU/l at baseline, dropping to 0.017 ± 0.007 mU/l after 4 weeks and staying at this low level (0.007 ± 0.002 mU/l) after 8 weeks (T3) as well. All thyroid hormone levels returned to pretreatment levels after discontinuation of levothyroxine exposure (T4) and stabilized (T5; fig. 1).
Fig. 1.
Kinetics of thyroid hormones fT4, fT3 and TSH levels after oral administration of 0.25 mg of levothyroxine per day. Hormone levels of each time point are shown as means ± SD. Horizontal lines indicate the maximum value of the reference interval for the specific TH (minimum value for TSH, respectively).
Proteomic Profiling of Plasma Proteins
Mass spectrometric analysis of all 80 plasma samples was performed in single LC-MS/MS runs. In total, 2,374 unique peptides representing 497 human proteins were identified. Only proteins identified in more than 60% of all samples (n = 439) were considered for quantification.
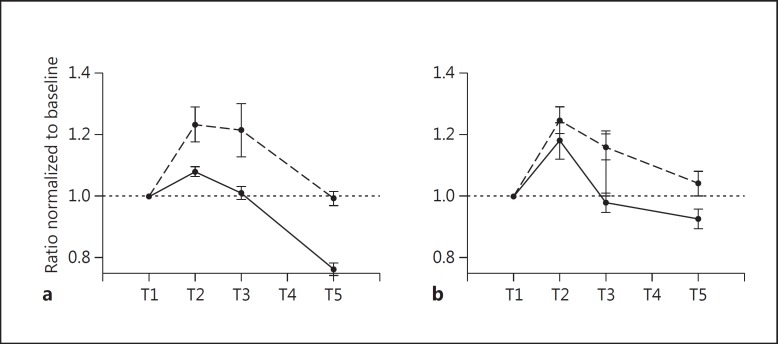
Among those proteins, SHBG could be quantified, a commonly used marker of thyrotoxicosis. In order to prove the sensitivity and validity of the proteomic approach, we first compared these LC-MS/MS-determined changes in SHBG protein levels due to levothyroxine treatment to the direct measurement of the protein using a routinely applied, highly sensitive ELISA (fig. 2). Both ELISA and LC-MS/MS measurement displayed very similar patterns, but the former seemed to be more sensitive.
Fig. 2.
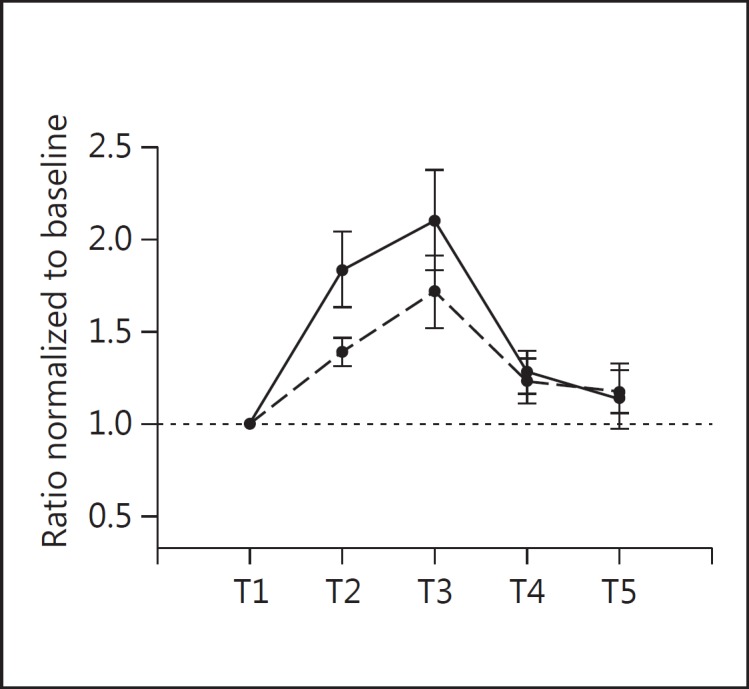
Relative change of SHBG. Protein levels of each time point are normalized to those at baseline immediately before levothyroxine administration (mean ± SEM). Black line: ELISA measurements; dashed line: proteomics data.
Correlation of Plasma Proteins with fT4 Levels
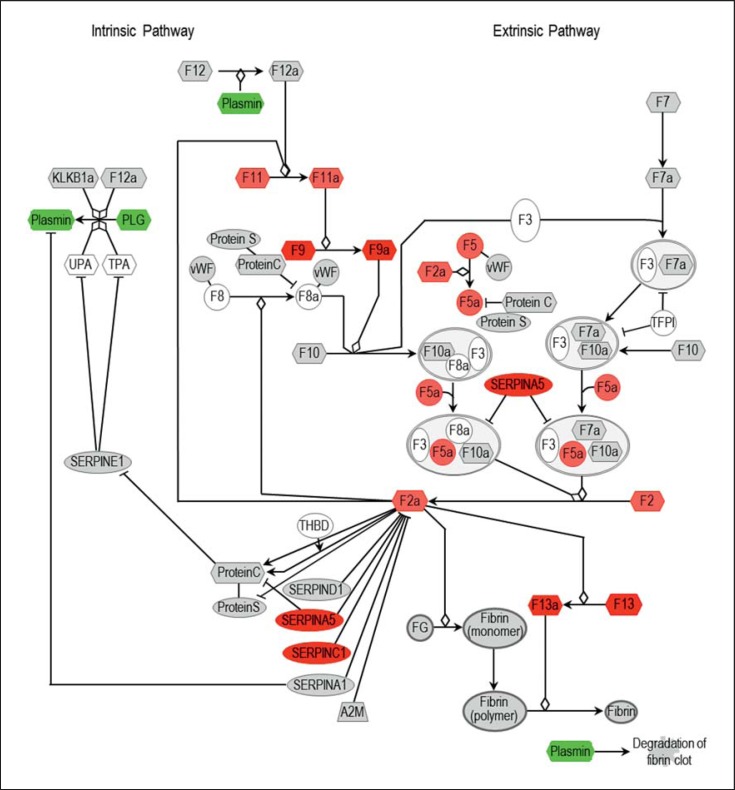
The fT4 levels and the protein abundance of the 439 proteins included in the analysis were correlated according to Pearson's correlation, revealing a large subset of proteins with a correlation coefficient |r| ≥0.8. Functional categorization of correlated proteins for canonical pathways revealed the coagulation cascade with a high number of assigned proteins. Of the 35 proteins assigned to the coagulation cascade, 24 proteins (almost 70%) were detected by our LC-MS/MS analysis (suppl. table S1). Out of these 24 proteins, 10 showed a significant correlation (|r| ≥0.8) with plasma fT4 levels (fig. 3).
Fig. 3.
Schematic view of the coagulation cascade. Colored boxes highlight proteins with r ≥0.9 (dark red); r ≥0.8 (light red); r ≤-0.9 (green). Gray boxes: proteins were covered by the analysis, but displayed no significant correlation (0.8 ≥ r ≥ −0.8). A2M = α2-Macroglobulin; F2 = coagulation factor II; FG = fibrinogen; KLKB1a = plasma kallikrein; PLG = plasminogen; SERPINA1 = α1-antitrypsin; SERPINA5 = protein C inhibitor; SERPINC = antithrombin III; SERPIND1 = heparin cofactor II; TFPI = tissue factor pathway inhibitor; THBD = thrombomodulin; TPA = tissue plasminogen activator; UPA = urokinase plasminogen activator; VWF = von Willebrand factor.
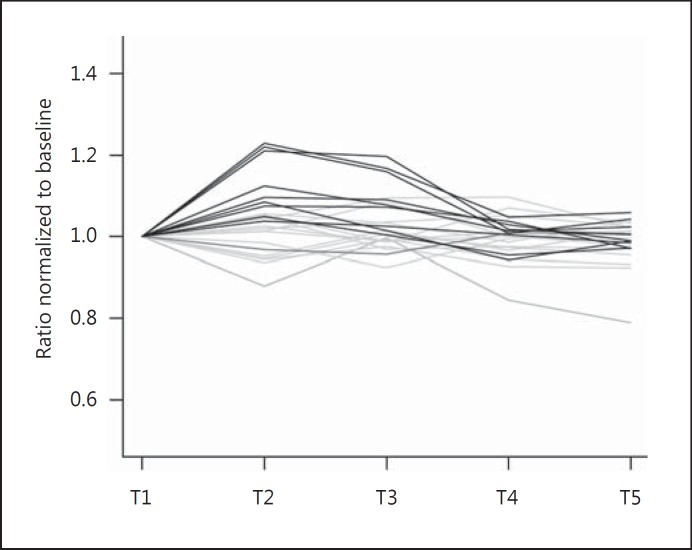
The majority of the coagulation proteins displayed a positive correlation. The strongest linear dependence was observed between coagulation FXIII subunit B and fT4 with a coefficient r = 0.991, revealing a strong increase in protein abundance caused by T4 administration. The FXIII subunit B protein level returned to baseline quickly after discontinuation of T4. Moreover, FIX could be found with an r = 0.938, whereas the correlation and significance of FV (r = 0.816), FII (r = 0.813) and FXI (r = 0.811) were slightly lower but showed the same tendency. Exemplarily, conventional ELISAs were performed for FIX and FXIII (fig. 4; online suppl. fig. S1), which yielded the same pattern and thus confirmed the data of the LC-MS/MS measurements. The other detected coagulation factors (FVII, FX, FXII, FXIII subunit A) showed no significant correlation with fT4. Other proteins with strong positive correlation included PAI-III, antithrombin III and α2-antiplasmin, all belonging to the serpin peptidase inhibitor family. In contrast, plasminogen was the only protein which displayed a significant negative correlation (r = −0.976; fig. 5).
Fig. 4.
Evaluation of LC-MS/MS results for FIX and FXIII subunit B by ELISA. Protein levels of each time point are normalized to those at baseline immediately before levothyroxine administration (mean ± SEM). Black line: ELISA measurements; dashed line: proteomics data.
Fig. 5.
Relative change to baseline of proteins involved in the coagulation cascade. Lines indicate the correlation between protein abundance and fT4 level: r ≥0.8 (black) and r ≤-0.8 (dark gray).
Discussion
The model of experimentally induced thyrotoxicosis has a number of advantages compared to endogenous hyperthyroidism as the extent and duration of thyroxine excess is defined. By treating healthy volunteers, a potential impact of comorbidity on the plasma proteome was excluded.
The fT4 levels reached in the current intervention study were all within the range that will be left untreated in clinical practice. Nevertheless, SHBG displayed elevated levels correlating with increased free T4 levels revealing toxic side effects even already at slightly increased thyroid hormone levels.
In contrast to many former studies targeting the effect of thyroid hormone imbalances on specific proteins such as those involved in coagulation and fibrinolysis [2], as a proof-of-principle study we aimed at a comprehensive monitoring of alterations in plasma protein levels independent of their biological function. Thus, a large number of proteins were quantified across all samples, including SHBG. This known marker protein exhibited comparable levels among the proteomics data and the ELISA measurements, confirming the technical feasibility of the shotgun proteomic approach.
Not surprisingly, the correlation analysis revealed a direct impact of thyroid hormones on proteins involved in the clotting cascade. Specifically, the procoagulatory factors XIII subunit B, II, XI and IX increased at higher fT4 levels. Concomitantly, plasminogen which is the main enzyme promoting fibrinolysis in its activated form plasmin was decreased. This indicates that increased fT4 levels may induce a hypercoagulable state by directly interfering with the synthesis of clotting factors in the liver. Indeed, it was recently demonstrated by the MEGA study that patients with increased fT4 levels possess an up to twofold higher risk for venous thrombosis and/or pulmonary embolism [6]. The effect of levothyroxine exposure on coagulation and fibrinolysis has already been addressed specifically in a controlled randomized crossover study in healthy volunteers [7]. Upon increase in free thyroxine, increased levels of procoagulant coagulation factors including FIX were observed, an observation that was confirmed in our study. However, not all details were matching. For example, in contrast to the data of van Zaane et al. [7], levels of von Willebrand factor did not change in our study. The differences observed for specific coagulation factors might reflect different stages of thyrotoxicosis and/or different properties of the assay methods used.
Additionally, the lower plasminogen levels detected in our proteomic study might indicate a hypofibrinolytic state. A large meta-analysis by Stuijver et al. [2] demonstrated elevated PAI-I levels in patients with hyperthyroidism, which also points towards hypofibrinolysis. PAI-I was not detected in our proteomic approach, but downregulation of plasminogen itself may also contribute to the hypofibrinolytic state, and blockade of fibrinolysis by increased PAI-I levels is not the only mechanism.
However, global plasma protein profiling disclosed protein alterations besides the typical proteins studied for the evaluation of coagulation and fibrinolysis [7]. Thus, another interesting finding was the increase in serpin A5 (protein C inhibitor), which is a potent inhibitor of activated protein C [8,9]. Activated protein C inhibits clot formation. An increase in serpin A5 lowers the inhibition of clot formation by activated protein C, further contributing to the prohemostatic role of elevated fT4 levels. Furthermore, several anticoagulatory factors such as antitrypsin, antithrombin III and α2-antiplasmin were also increased and may mirror an anticoagulatory compensatory mechanism, which is typical for the coagulation cascade.
Overall, this study provides new insights into the association of circulating plasma fT4 levels with a large subset of plasma proteins not restricted to proteins involved in coagulation and fibrinolysis, but also other protein classes which have to be analyzed in detail. Our study differs substantially from endogenous hyperthyroidism because it is limited to the direct effects of thyroxine addition and displays different dynamics and secretion patterns of thyroid hormones. Thus, our experimental approach has clear advantages for capturing pure thyroid hormone-dependent effects.
Conclusions
The results of this study suggest that experimental thyrotoxicosis exerts selective and specific thyroxine-induced effects on coagulation markers. The increase in procoagulant clotting factors, a decrease of fibrinolytic enzymes and an enhanced inhibition of the protein C pathway may contribute to the hypercoagulable state in thyrotoxicosis. Furthermore, the study design presented allows assessment of thyroid hormone effects such as those on the coagulation system but also on the whole set of plasma proteins without interference of other diseases or therapies.
Disclosure Statement
There are no conflicts of interest to report.
Supplementary Material
Supplementary data
Supplementary data
Supplementary data
Supplementary data
References
- 1.Squizzato A, Romualdi E, Büller HR, Gerdes VEA. Clinical review: thyroid dysfunction and effects on coagulation and fibrinolysis: a systematic review. J Clin Endocrinol Metab. 2007;92:2415–2420. doi: 10.1210/jc.2007-0199. [DOI] [PubMed] [Google Scholar]
- 2.Stuijver DJ, van Zaane B, Romualdi E, Brandjes DP, Gerdes VE, Squizzato A. The effect of hyperthyroidism on procoagulant, anticoagulant and fibrinolytic factors: a systematic review and meta-analysis. Thromb Haemost. 2012;108:1077–1088. doi: 10.1160/TH12-07-0496. [DOI] [PubMed] [Google Scholar]
- 3.Hooper JM, Stuijver DJ, Orme SM, et al. Thyroid dysfunction and fibrin network structure: a mechanism for increased thrombotic risk in hyperthyroid individuals. J Clin Endocrinol Metab. 2012;97:1463–1473. doi: 10.1210/jc.2011-2894. [DOI] [PubMed] [Google Scholar]
- 4.Anderson NL, Anderson NG. The human plasma proteome: history, character, and diagnostic prospects. Mol Cell Proteomics. 2002;1:845–867. doi: 10.1074/mcp.r200007-mcp200. [DOI] [PubMed] [Google Scholar]
- 5.Hammer E, Goritzka M, Ameling S, et al. Characterization of the human myocardial proteome in inflammatory dilated cardiomyopathy by label-free quantitative shotgun proteomics of heart biopsies. J Proteome Res. 2011;10:2161–2171. doi: 10.1021/pr1008042. [DOI] [PubMed] [Google Scholar]
- 6.Debeij J, van Zaane B, Dekkers OM, et al. High levels of procoagulant factors mediate the association between free thyroxine and the risk of venous thrombosis: the MEGA study. J Thromb Haemost. 2014;12:839–846. doi: 10.1111/jth.12573. [DOI] [PubMed] [Google Scholar]
- 7.van Zaane B, Squizzato A, Debeij J, et al. Alterations in coagulation and fibrinolysis after levothyroxine exposure in healthy volunteers: a controlled randomized crossover study. J Thromb Haemost. 2011;9:1816–1824. doi: 10.1111/j.1538-7836.2011.04430.x. [DOI] [PubMed] [Google Scholar]
- 8.Meijers JC, Kanters DH, Vlooswijk RA, van Erp HE, Hessing M, Bouma BN. Inactivation of human plasma kallikrein and factor XIa by protein C inhibitor. Biochem. 1988;27:4231–4237. doi: 10.1021/bi00412a005. [DOI] [PubMed] [Google Scholar]
- 9.España F, Berrettini M, Griffin JH. Purification and characterization of plasma protein C inhibitor. Thromb Res. 1989;55:369–384. doi: 10.1016/0049-3848(89)90069-8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary data
Supplementary data
Supplementary data
Supplementary data