Abstract
Aim
To compare landmark vs surface-shape measurements in a sample of patients with cleft lips and palates following secondary alveolar bone grafting.
Methods
The faces of 10 patients (4 males and 6 females) with an unilateral cleft lip and palate were captured using a 3D surface camera system before and 6 weeks after alveolar bone grafting. In each face, six coordinates were registered. The pre- and postoperative images were superimposed on areas that were not affected by the surgery. Using 3D modeling software landmarks, nasal symmetry, and surface-to-surface deviation, analysis was performed. All data were subjected to standard statistical analyses.
Results
Color map surface-to-surface comparison revealed a significant anteroposterior elevation in the nasal region of the cleft side after surgery.
Conclusion
The ala, alar base, and paranasal areas are increased anteroposteriorly after secondary bone grafting. This surgery tends to diminish the asymmetry in nasal morphology typically seen in patients with unilateral cleft lip and palate. Overall, 3D surface-to-surface analysis allows for a better quantification of treatment changes.
Keywords: bone graft, clefts, surface imaging, 3D imaging
Patients with unilateral cleft lips and palates (ULCP) often have missing teeth, asymmetric dental arches, and a hypoplastic maxilla in the area of the piriform rim. This often leads to spatial aberrations or impaction of teeth and a deformation of the nose1—in particular, nostril size, nose tip orientation, and columella length.2 Secondary alveolar bone grafting can help alleviate these problems and lead to an improvement in the morphology of the nasal region. The benefits of this surgery are a facilitated eruption of the teeth adjacent to the cleft and better orthodontic alignment because of the provided bone, closure of oronasal fistulas, provision of a continuous alveolar ridge for future restorations, and support and elevation of the alar base on the cleft side.3–5 Still, to date, only one study has reported the effects of secondary alveolar bone grafting on the morphology of the nasal region.1
The purpose of this study was to evaluate nasal morphology changes in patients with UCLP following secondary bone grafting using a three-dimensional (3D) surface acquisition system. The hypothesis of this study was that there was no difference between a landmark-based and a surface-shape analysis.
METHODS
Patients with UCLP treated with bone grafting surgery between March 1, 2007, and March 1, 2008, were invited to participate in this longitudinal prospective study. Inclusion criteria were nonsyndrome-associated UCLP and no nasal reconstructive surgery.
The study was approved by the institutional review board at the University of Texas Health Science Center at Houston, Houston, Texas. Also, the rationale and protocol for this study were explained to all patients, from whom informed consent was obtained.
A total of 10 consecutive patients, 4 males and 6 females, met the inclusion criteria. Their ages ranged from 7 to 21 years at the time of surgery, which was performed by one surgeon using a standardized clinical procedure.
3D stereophotogrammetry
All images were taken with the 3dMDface (3dMD) system 6 weeks postoperatively, because 60% of the swelling disappears within the first month after surgery.6 3dMDface is a portable system that uses a combination of stereophotogrammetry with three cameras on each side (one color and two infrared) and a structured light technique, which projects a random light pattern onto the individual surface.7 It captures photorealistic quality pictures of a full face in 1.5 milliseconds at highest resolution. According to the manufacturer, its accuracy is 0.5 mm and its clinical accuracy is 1.5% of the total observed variance.8
Three-dimensional images captured by surface-acquisition systems are highly repeatable and allow landmark data acquisition with high precision.9,10 During imaging, the patient is seated on an adjustable stool, with a distance between the camera and patient of 34 inches. Though the system works with two built-in flash units, in this investigation, a third was mounted between the cameras to reduce any shadows.
All 3D images were quantitatively analyzed using generic computer-modeling software (Rapidform 2006, INUS Technology). These evaluations included landmark analysis, 2D projection analysis, and surface-to-surface analysis.
Landmark analysis
Six anthropometric nose-related landmarks (Fig 1, Table 1) were digitized on each photo by one investigator (L.M.). During this digitization, the investigator was blinded about the patient’s status (pre- vs postoperative). The preoperative 3D images were then oriented to natural head position with soft tissue nasion set as the origin (0, 0, 0) of a 3D coordinate system (Fig 2).
Fig. 1.
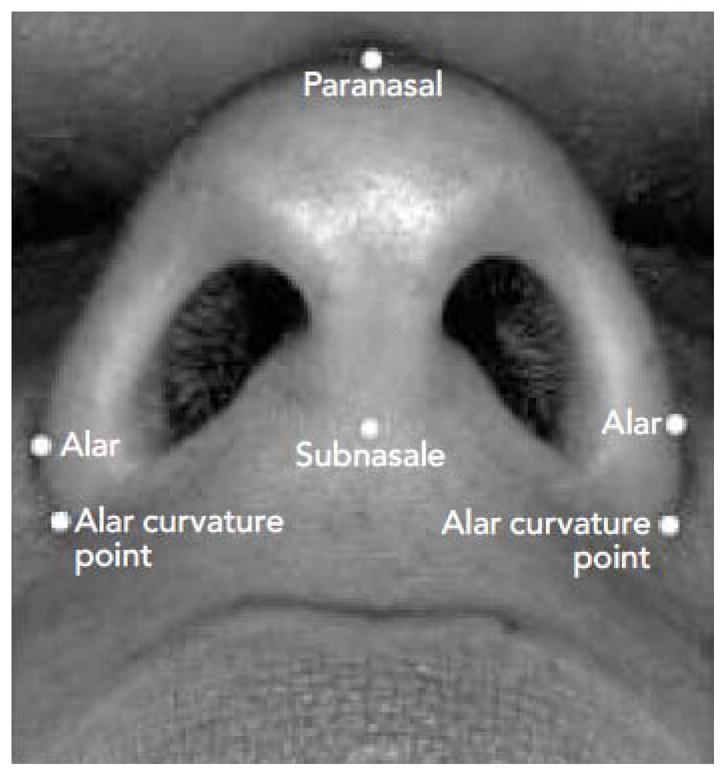
(Left) Location of the landmarks digitized in this study. Compare to Table 1.
Table 1.
Designation and definition of the landmarks digitized in this study
| Alar | Most lateral point on each alar contour |
| Paranasal | Most protruded point of nose apex |
| Subnasale | Junction of lower border of nasal septum and upper lip |
| Alar curvature point | Most lateral point of the curve base line of each ala, facial insertion of the nasal wingbase |
Fig. 2.
The 3D coordinate in this study: x-axis, immediately to left of the face on the coronal plane; y-axis, cranial to caudal of the face on the coronal plane; z-axis, dorsal to ventral of the face on the sagittal plane.
Subsequently, the postoperative image of the same patient was superimposed onto the preoperative one in areas that were not affected by the surgery using the least-square, best-fit superimposition algorithm. After this superimposition, the x, y, and z coordinates of each landmark were recorded, paired, and tabulated in a Microsoft Excel spreadsheet. For comparison purposes, the images were normalized (flipped) so the cleft side was always the left side and the noncleft side the right one.
The hypothesis was that the secondary alveolar bone grafting surgery was likely to change nasal morphology. To this end, analysis of variance (ANOVA) for repeated measurements was used. In this statistical model, the response variable was the coordinates of each landmark. The within-subject factors were the two time points at which the 3D images were taken (pre- and postoperatively) and the spatial location of all landmarks (x, y, z).
Nasal symmetry analysis
The pre- and postoperative nasal symmetry was calculated using the previously digitized landmarks. The comparison included alar width symmetry, alar length symmetry, and columella deviation. While alar width and length symmetry were measured both three- and two-dimensionally (axial plane), columella deviation was only measured two-dimensionally on the axial plane. Symmetry was calculated according to the following formulas:
| (Equation 1) |
| (Equation 2) |
| (Equation 3) |
| (Equation 4) |
| (Equation 5) |
The paired t test was selected to determine whether nasal symmetry changed significantly from before to after bone grafting surgery; the assumptions for paired t test were evaluated and not found to be violated.
Surface-to-surface deviation
Using the aforementioned 3D modeling software, the pre- and postoperative differences at the nasal area were recorded, calculated in millimeters, and presented as color maps. In this study, blue areas indicated negative changes (areas of depressions), whereas red areas designated positive changes (areas of elevation) in relation to preoperative status. A tolerance of 0.85 mm was applied to reflect the reproducibility error.11
A one-sample t test was used to detect whether the nasal change after surgery was significantly greater than 0; the assumptions for the one-sample t test were also evaluated and not found to be violated.
RESULTS
Landmarks analysis
The z coordinate of landmarks alar, alar curvature point, and subnasale differed significantly between before and after bone grafting. While these landmarks were elevated after surgery, they did not change in the other direction of space. Landmark alar changed from 2.37 mm (95% of confidence interval [CI], 0.57 to 4.17) preoperatively to 3.77 mm (95% CI, 2.12 to 5.41) postoperatively, a significant change of 1.40 mm (95% CI, −0.18 to 2.97). Landmark alar curvature point changed from −0.89 mm (95% CI, −3.18 to 1.40) preoperatively to 0.15 mm (95% CI, −1.89 to 2.19) postoperatively, a significant change of 1.04 mm (95% CI, −0.23 to 2.31). Landmark subnasale changed from 4.72 mm (95% CI, 2.09 to 7.37) preoperatively to 5.68 mm (95% CI, 3.48 to 7.89) postoperatively, again a significant change of 0.96 mm (−0.08 to 2.02). Finally, for landmark pronasale, no significant difference in either direction was observed.
Nasal symmetry analysis
Nasal symmetry did not change significantly after surgery for any measurement. Before grafting, the mean 3D alar width asymmetry was 113.6%, indicating that the alar width was greater on the cleft side. After grafting, the asymmetry was reduced to 109.2%, hinting at an improvement. The 2D measurements showed a similar result: The mean alar width asymmetry was reduced from 111.6% preoperatively to 107.8% postperatively.
Before bone grafting, the mean 3D alar length asymmetry was 103.1%, ie, the length was slightly greater on the cleft side. After surgery, the mean symmetry was 100.2%. The 2D projection measurements showed a similar result: The mean length asymmetry was reduced from 105.2% preoperatively to 101.7% postoperatively.
Finally, the mean columella deviation before grafting was 0.89 degrees toward the noncleft side, which increased to 1.30 degrees after surgery.
Surface-to-surface deviation
In all 10 patients, the color map of surface-to-surface deviations showed a red area in the nasal and paranasal areas (Fig 3). This indicates a regional elevation after grafting. The largest increase was observed in the alar area, which amounted to 2.93 ± 0.67 mm (95% CI, 2.45 to 3.42). A one-sample t test showed that this elevation was significant.
Fig. 3.
Example of surface-to-surface deviation color map in six patients: black areas, no surface changes (0.85-mm tolerance); blue areas, negative changes; and red areas, positive changes.
DISCUSSION
Secondary alveolar bone grafting is part of the standard of care for patients with UCLP. It has been repeatedly demonstrated that this procedure favors tooth eruption into the cleft area and also provides bony support for the alar base of the affected side.3–5 However, the current literature demonstrating the effects of this surgery on the nasal morphology is scarce. To these authors’ knowledge, only one previous study evaluated respective changes using 2D photographs and reported a significant improvement in nasal symmetry postoperatively due to a decrease in nostril height.1 Similarly, the present study demonstrated that after surgery, the ala and the alar base on the affected side were projected forward (z-axis), as documented by a significant change in the landmarks alar, alar curvature point, and subnasale. The nasal symmetry analysis revealed that the asymmetry of the nose, specifically alar width and length, tended to improve. It was also observed that the columella inclined or deviated less to the affected side after surgery.
While landmark studies showed not too many clinically significant changes, the 3D surface-to-surface analysis gave qualitatively clearer information, emphasizing that it should receive more attention in the future.12–13
CONCLUSION
This study demonstrates:
There is an increase in anteroposterior dimension that occurs in the alar, alar base, and paranasal areas of patients with UCLP after secondary alveolar bone grafting. This procedure has the tendency to diminish the asymmetry in nasal morphology of these patients.
Three-dimensional surface-to-surface analysis allows for better quantification of treatment changes.
References
- 1.Baeyens W, Daelemans A, Leloup T, De Mey A. Study of changes in nasal morphology in children with complete unilateral cleft lip and palate after secondary bone grafting measured with image analysis. Scand J Plast Reconstr Surg Hand Surg. 2006;40:345–351. doi: 10.1080/02844310601029928. [DOI] [PubMed] [Google Scholar]
- 2.Farkas L. Anthropometry of the Head and Face. New York: Raven Press; 1994. [Google Scholar]
- 3.Kokkinos PP, Ledoux WR, Kinnebrew MC, Weinberg R. Iliac apophyseal cartilage augmentation of the deficient piriform rim and maxilla in alveolar cleft grafting. Am J Orthod Dentofacial Orthop. 1997;112:145–153. doi: 10.1016/s0889-5406(97)70239-7. [DOI] [PubMed] [Google Scholar]
- 4.Trotman CA, Papillon F, Ross RB, Mc-Namara JA, Jr, Johnston LE., Jr A retrospective comparison of frontal facial dimensions in alveolar-bone-grafted and nongrafted unilateral cleft lip and palate patients. Angle Orthod. 1997;67:389–394. doi: 10.1043/0003-3219(1997)067<0389:ARCOFF>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 5.Boyne PJ, Sands NR. Combined orthodontic-surgical management of residual palato-alveolar cleft defects. Am J Orthod. 1976;70:20–37. doi: 10.1016/0002-9416(76)90258-x. [DOI] [PubMed] [Google Scholar]
- 6.Kau CH, Cronin AJ, Richmond S. A three-dimensional evaluation of postoperative swelling following orthognathic surgery at 6 months. Plast Reconstr Surg. 2007;119:2192–2199. doi: 10.1097/01.prs.0000260707.99001.79. [DOI] [PubMed] [Google Scholar]
- 7.Kau CH, Richmond S, Incrapera A, English J, Xia JJ. Three-dimensional surface acquisition systems for the study of facial morphology and their application to maxillofacial surgery. Int J Med Robot. 2007;3:97–110. doi: 10.1002/rcs.141. [DOI] [PubMed] [Google Scholar]
- 8.Aldridge K, Boyadjiev SA, Capone GT, DeLeon VB, Richtsmeier JT. Precision and error of three-dimensional phenotypic measures acquired from 3dMD photo-grammetric images. Am J Med Genet A. 2005;138A:247–253. doi: 10.1002/ajmg.a.30959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kau CH, Hunter LM, Hingston EJ. A different look: 3-dimensional facial imaging of a child with Binder syndrome. Am J Orthod Dentofacial Orthop. 2007;132:704–709. doi: 10.1016/j.ajodo.2007.01.020. [DOI] [PubMed] [Google Scholar]
- 10.Kau CH, Zhurov A, Richmond S, Cronin A, Savio C, Mallorie C. Facial templates: A new perspective in three dimensions. Orthod Craniofac Res. 2006;9:10–17. doi: 10.1111/j.1601-6343.2006.00359.x. [DOI] [PubMed] [Google Scholar]
- 11.Kau CH, Richmond S, Zhurov Al, et al. Reliability of measuring facial morphology with a 3-dimensional laser scanning system. Am J Orthod Dentofacial Orthop. 2005;128:424–430. doi: 10.1016/j.ajodo.2004.06.037. [DOI] [PubMed] [Google Scholar]
- 12.Kau CH, Cronin A, Durning P, Zhurov Al, Sandham A, Richmond S. A new method for the 3D measurement of postoperative swelling following orthognathic surgery. Orthod Craniofac Res. 2006;9:31–37. doi: 10.1111/j.1601-6343.2006.00341.x. [DOI] [PubMed] [Google Scholar]
- 13.Kau CH, Richmond S. Three-dimensional analysis of facial morphology surface changes in untreated children from 12 to 14 years of age. Am J Orthod Dentofacial Orthop. 2008;134:751–760. doi: 10.1016/j.ajodo.2007.01.037. [DOI] [PubMed] [Google Scholar]




