Abstract
The purpose of this study was to evaluate changes in movement patterns during a sit-to-stand (STS) task before and after total hip arthroplasty (THA), and to compare biomechanical outcomes after THA to a control group. Forty-five subjects who underwent THA and twenty-three healthy control subjects participated in three-dimensional motion analysis. Pre-operatively, subjects exhibited inter-limb movement asymmetries with lower vertical ground reaction force (VGRF) and smaller moments on the operated limb. Although there were significant improvements in movement symmetry 3 months after THA, patients continued to demonstrate lower VGRF and smaller moments on the operated limb compared to non-operated and to control limbs. Future studies should identify the contributions of physical impairments and the influence of surgical approach on STS biomechanics.
Keywords: sit to stand, lateral trunk angle, biomechanics, total hip arthroplasty, joint moment
Total hip arthroplasty (THA) is the treatment of choice for end-stage hip osteoarthritis (OA). This surgery effectively reduces pain [1–4] and improves function [1–8] compared to pre-operative levels. Despite the pain resolution and a high level of patient satisfaction after THA [9], abnormal movement patterns persist during dynamic tasks such as walking [10,11], stair climbing [12] and rising from a chair [13–16]. Rising from a chair, defined here as the sit-to-stand task (STS) task, is an important metric of biomechanical recovery after THA. This task is a fundamental daily activity performed approximately 60 times per day by healthy adults [17]. It is a demanding task that requires greater muscle strength and produces higher joint forces than walking and stair climbing [18,19]. Unlike most other dynamic movements, rising from a chair is a bilateral support task in which both feet are in contact with the ground. Therefore, compensatory movement strategies that favor one leg can be used to accomplish the task, which makes the STS task a sensitive measure for evaluating movement asymmetry in individuals with unilateral lower extremity pathology.
When rising from a seated position, patients after THA unload their operated hip and shift weight to the non-operated side [13,14,16]. A study by Lamontagne and colleagues has also shown that the operated hip has less motion in the sagittal plane, smaller internal extension moment and different mechanics in the frontal and transverse planes compared to both the non-operated side and control subjects when rising from a chair [15]. While previous studies have analyzed lower limb biomechanics during STS in the THA population [13–16]; only one small study by Caplan and colleagues [16] was longitudinal (n = 7), while the other studies have been limited to cross sectional designs. In addition, none of these studies have evaluated trunk movement during the STS task in patients before and after THA. Trunk movement plays an important role in completing the STS [20–22]. Proximal adaptations may be a principal determinant of successful strategies in a population with substantial pelvic and hip muscular weakness that remains years after THA [23]. Quantifying trunk movement during STS may lead to better understanding of how patients before and after THA use compensatory strategies to rise out of a chair.
The purpose of this study was to evaluate STS movement strategies before and 3 months after THA and determine whether subjects 3 months after THA have joint kinetics and trunk kinematics that differ from a control group of older adults without lower extremity joint pathology. Specifically, we hypothesized that: 1) at 3 months after THA, patients will show improvements in movement symmetry that is driven by increased vertical ground reaction force (VGRF) and increased moments about the hip and knee joints of the operated limb compared to the pre-operative time point and 2) at 3 months after THA, the operated limb would have lower VGRF, and smaller hip and knee moments compared to the control group.
Methods
Subjects
This was a prospective longitudinal study. Subjects with end-stage hip OA between the ages of 35 and 85, who were scheduled to undergo THA between March 2012 and April 2014 were either referred by local orthopedic surgeons or responded to newspaper advertisements. Prior to enrollment, subjects were screened for eligibility using a telephone interview conducted by our research staff. Subjects were excluded if they had 1) neurological disorders that affected their ability to walk or rise from a chair, 2) any cardiovascular problems that limited their ability to climb a flight of stairs or walk for 6 minutes, 3) uncontrolled hypertension, or 4) history of cancer in the lower extremity. Subjects with bilateral limb involvement were allowed to participate in the parent study, but were excluded from this analysis if they had a prior arthroplasty surgery within the previous year; or planned to have an additional lower extremity arthroplasty (Fig. 2). This was done to avoid the potential confounding influence of contralateral joint impairments on biomechanical symmetry. Three-dimensional motion analysis was completed at 2–4 weeks prior to THA and 3 months after THA. The 3 month follow-up was specifically chosen as this is the time many patients are cleared to return to higher level activity, can participate in muscle strengthening exercises, and no longer have hip precautions. Therefore, it is the time that more progressive exercise and rehabilitation interventions may begin.
Fig. 2.
Flow chart of enrolled THA subjects.
All surgical procedures were performed by a modified Hardinge anterolateral, posterior, or direct lateral approach at a single Joint Center with a volume of approximately 800 THAs per year (Table 1). Patients from five surgeons were included in this study. Two surgeons performed the anterolateral approach, two different surgeons performed the posterior approach, and one surgeon performed the direct lateral approach.
Table 1.
Subject Characteristics.
| THA (Pre-Operative)
|
Control Group
|
|||
|---|---|---|---|---|
| Variable | Mean (SD) | Range | Mean (SD) | Range |
| Age (years) | 63.8 (8.0) | 42–82 | 67.9 (7.7) | 51–81 |
| Height (m) | 1.74 (0.10) | 153–1.89 | 1.67 (0.09) | 1.53–1.87 |
| Mass (kg) | 89.2 (22.1) | 51.4–146.5 | 71.4 (17.1) | 44.0–126.3 |
| BMI (kg/m2) | 29.4 (5.6) | 19.9–43.5 | 25.3 (4.1) | 17.6–36.1 |
| Sex: male/female (n) | 28/16 | – | 9/14 | – |
| Affected side: right/left (n) | 22 (49%)/23 (51%) | – | 13 (56%)/10 (44%) | – |
| Surgical approach. P/AL/DL |
30/14/1 | – | N/A | – |
A cross-sectional sample of older adults without symptomatic lower extremity joints pathology was also collected as control group. Subjects in the control group met all of the same inclusion and exclusion criteria as the THA population. Additionally, control subjects were excluded if they had a previous joint arthroplasty, were planning a joint arthroplasty or had pain greater than 4/10 in any lower extremity joint. Subjects in the control group only attended a single testing session. The study was approved by the Human Subjects Review Board at the University of Delaware and all subjects provided informed consent prior to participation.
Anthropometric Measures
Age, height, weight and sex were recorded, and body mass index (BMI) was calculated for subjects in the THA and control groups.
Motion Analysis
For the THA and control groups, the STS was collected using a three dimensional 8-camera motion capture system (VICON, Oxford Metrics, London, England) synchronized with two embedded force platforms (Bertec Corp., Worthington, OH, USA). Sixteen-millimeter spherical retro-reflective markers were placed bilaterally on anatomical structures that were used to define the trunk and lower extremity segments during the static trial. Markers were placed on the acromio-clavicular joint, iliac crest, greater trochanter, lateral femoral condyle, lateral malleolus, head of the 5th metatarsal, and 2 markers on the heel. To track segments movement during the dynamic trials, rigid thermoplastic shells with 4 markers were attached to the trunk (mid-thoracic area lateral to the spine) and bilaterally on the lower legs and thighs, and a shell with 3 markers was placed on the pelvis below the line between the 2 posterior superior iliac spines. The only difference in motion analysis for THA and control groups was in the method to compute the joint centers. For THA group, medial markers were used to compute knee and ankle joint centers during a static standing trial. Functional hip joint centers were determined using a built-in algorithm that calculates the most likely intersection of all axes (effective joint center) and most likely orientation of the axes (effective joint axis) between the pelvis and femur based on a separate dynamic trial in which subjects performed hip flexion, extension and abduction and circumduction during a single leg stance [24]. For the control group, knee, and ankle joint centers were computed by using virtual medial markers. These markers were created based on the joint width that measured between two femoral epicondyles and between two malleoli using a caliper. The hip joint centers were computed using the predictive method that places the hip joint center at one-quarter of the distance from the ipsilateral to the contralateral greater trochanter markers [25]. Given that the on-going THA study was conducted after the initiation of control group study, a different method was employed in THA study to measure joint centers that improves precision of center location, especially for the hip joint. The functional method improves hip joint center localization compared to predictive method and is recommended to be used for motion analysis in THA population [26].
Marker and force platform data were sampled at 120 Hz and 1080 Hz, and filtered at 6 Hz and 40 Hz, respectively, using a second-order phase corrected Butterworth filter. Visual 3D software (v5.00.25; C-Motion Inc., Germantown, MD, USA) was used to compute joint angles and moments for each limb by using kinematics and inverse dynamic analysis techniques. Joint angles were calculated using Euler X-Y-Z sequence corresponding to flexion/extension, abduction/adduction, and then rotation sequences. VGRF in newton was normalized to subject’s body weight in newton (N/BW, i.e. % of BW). Joint moments were expressed as external moments normalized to body mass times height (Nm/kg · m).
Movement Task
An adjustable-height piano stool without armrests or backrests was used for this task (Fig. 1). The height of the stool was set to the subject’s knee joint line when standing. Subjects were seated in the stool with the trunk in upright position and with no restrictions on their feet position. Subjects were also asked to hold the arms in the lap and to stand from the chair at their self-selected pace but not to turn or look behind for the stool while sitting down. Before collecting three STS trials, subjects were asked to practice the task twice. For subject’s safety, the stool was secured to the floor with adhesive tape to prevent movement during the task. The start and end of the STS task were defined as follows: the start–stand event occurred when the velocity of the left acromio-clavicular marker exceeded a threshold of 0.1 m/s in the anterior direction and end-stand occurred when the left acromio-clavicular marker reached the highest position in the vertical direction.
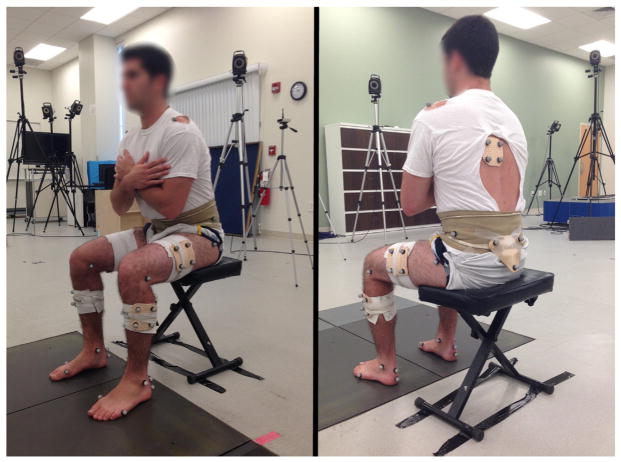
Fig. 1.
Marker and laboratory set-up for the sit to stand task, although subjects wore shoes during the activity.
Outcome Variables
Vertical ground reaction force (VGRF), sagittal and frontal hip and knee moments were calculated for each limb through the STS task. To characterize the loading pattern at the foot-floor interface, the peak VGRF for each limb was calculated and used in the analysis. Peak values for external hip and knee flexion moments, and peak external hip adduction moment, were assessed for each limb to identify any joint specific compensation during the movement. These moments represent the rotational force applied by external forces (ground reaction force) and inertial properties that act to flex the knee and hip in the sagittal plane and adduct the hip in the frontal plane. These moments must be counterbalanced by internal moments produced by the muscles and soft tissue around the joints. Therefore, the external flexion moments are surrogate measures of the extensor muscle function, whereas the hip adduction moment is a surrogate measure of hip abductor muscle function.
The lateral trunk angle was defined as the frontal plane angle of the trunk segment in relation to the pelvis segment. This angle was calculated at the time of maximum bilateral VGRF. Maximal bilateral VGRF was defined as the maximal summed value of the left and right VGRFs. Positive values for lateral trunk angle correspond with movement toward the operated side, while negative values represent angles toward the non-operated side.
Data Analysis
To test the first hypothesis, a two-way repeated measures analysis of variance (ANOVA) (time × limb) was used to detect main and interaction effects for the limb specific variables; VGRF and joint moments. In the event of a significant interaction effect, follow-up paired t-tests were used. Paired t-test was also used to assess the change in lateral trunk angle between pre-operative and post-operative time points. In addition, the one sample t-test was used to determine if lateral trunk angle at each time point was significantly different from zero.
To test the second hypothesis, paired t-tests were used to examine whether the limbs of control group were significantly different. A two-way mixed model ANOVA (group × limb) was used to examine the group differences between the 3 months THA group and the control group. Independent t-tests were used for post hoc testing when the interaction effect was significant to examine the differences between groups. Independent t-tests were also used to compare the trunk angle and the subject characteristics between the 3 months THA group and the control group. For analytical purposes, subjects in the control group were randomly assigned operated and non-operated limbs by way of coin flip; however, the percentage of left and right operated limbs was stratified during to match the percentage in our THA group.
For purposes of quantifying limb asymmetry, percent difference between limbs for VGRF and joint moments was computed at each time point by subtracting the operated from non-operated limb and then dividing by non-operated limb value. Percent change between pre-operative and post-operative time points was also assessed for each limb by subtracting the value at the pre-operative session from value at 3 months and then dividing by the pre-operative value.
Results
Forty five subjects were enrolled in this study (Fig. 2 and Table 1). All subjects in the THA group received home and outpatient physical therapy following THA, except for two subjects who received only home therapy. A total of twenty-three healthy control subjects were enrolled for comparative purposes. The THA group consisted of 51% of right-side operated limbs and 49% left-side operated limbs (Table 1). There were significant differences in height (P = 0.006), mass (P = 0.001), and BMI (P = 0.004) between subjects 3 months after THA and control group.
There was a significant limb-by-time interaction for peak VGRF (F1,44 = 19.14, P < 0.001) (Table 2 and Fig. 3A and B). Post hoc tests revealed a significant increase in peak VGRF on the operated limb (+6%, P = 0.001) and a significant decrease in the non-operated side (−4%, P = 0.005) compared to pre-operative values. Despite these changes, there were significant differences between limb at the pre-operative (24%, P < 0.001) and post-operative (16%, P < 0.001) sessions with higher peak VGRF under the non-operated limb at both time points.
Table 2.
Biomechanical Outcomes for THA and Control Groups.
| Biomechanical Variables, Mean (SD)
|
||||||
|---|---|---|---|---|---|---|
| Pre-Op
|
Post-Op
|
Control
|
||||
| Variable | OP | Non-OP | OP | Non-OP | OP | Non-OP |
| Peak VGRF (N/BW) | 0.51 (0.06) | 0.67 (0.05) | 0.54 (0.05) | 0.64 (0.05) | 0.61 (0.04) | 0.60 (0.03) |
| Peak hip flexion moment (Nm/kg · m) | 0.36 (0.08) | 0.48 (0.11) | 0.39 (0.09) | 0.44 (0.10) | 0.48 (0.09) | 0.47 (0.11) |
| Peak hip adduction moment (Nm/kg · m) | 0.08 (0.04) | 0.14 (0.07) | 0.09 (0.05) | 0.12 (0.06) | 0.12 (0.06) | 0.12 (0.05) |
| Peak knee flexion moment (Nm/kg · m) | 0.40 (0.08) | 0.58 (0.10) | 0.45 (0.09) | 0.58 (0.11) | 0.54 (0.09) | 0.52 (0.09) |
| Lateral trunk angle, (°) | 3.95 (5.90) | 2.36 (6.21) | 0.15 (3.69) | |||
Pre-op: pre-operative. Post-op: 3 months post-operative.
Fig. 3.
Average time series curves for VGRF for the non-operated and operated limbs, pre-operatively (Pre-op) (A), and 3 months post-operatively (Post-op) (B). Average time series curves for lateral trunk angle pre-operatively (C), and 3 months post-operatively (D), with error bars represent 1 standard deviation from the mean.
Peak hip flexion moment showed a significant limb-by-time interaction (F1,44 = 17.51, P = 0.001) (Table 2). Post hoc tests revealed a significant increase in peak hip flexion moment on the operated side (+8%, P = 0.024), and a significant decrease on the non-operated side (−8%, P = 0.012) 3 months after surgery compared to pre-operative values. However, there were greater peak hip flexion moments on the non-operated limb pre-operatively (24%, P < 0.001) and at the postoperative (11%, P = 0.002) sessions. For peak hip adduction moment, there was a significant limb-by-time interaction (F1,44 = 4.28, P = 0.044). There was no significant increase (P = 0.238) on the operated side at 3 months compared to the pre-operative value, and the non-operated side did not show any significant change (P = 0.111). However, there were higher peak hip adduction moments on the non-operated limb compared to the operated limb pre-operatively (41%, P < 0.001) and at the post-operative (25%, P = 0.010) sessions (Table 2).
Peak knee flexion moment (Table 2) showed a significant limb-by-time interaction (F1,44 = 10.52, P = 0.002). There was a significant increase (+11%, P < 0.001) on the operated side at 3 months compared to the pre-operative value, while the non-operated side did not show any significant change (P = 0.933). At both time points, there were significant differences, with greater peak knee flexion moments on the non-operated limb (P < 0.001).
For trunk movement, the one-sample t-tests revealed that subjects had a significant lateral trunk angle toward the operated side at both time points; with 3.95° and 2.36° (P < 0.001, and P = 0.014) before, and 3 months after surgery, respectively. Paired t-test revealed a significant decrease in lateral trunk angle across time points (P = 0.041). There was a high degree of variability with respect to trunk movement during the task (Fig. 3C and D).
There were no significant differences between limbs in the control group for any biomechanical variable (Table 2). For comparisons between the control group and the 3 months THA group, there was a significant group-by-limb interaction (F1,66 = 36.48, P < 0.001) for peak VGRF. Post hoc tests revealed lower peak VGRF on the operated limb compared to the control limb (P < 0.001), and higher peak VGRF on the non-operated limb compared to the control limb (P = 0.004).
For peak hip flexion moment, there was a significant group-by-limb interaction (F1,66 = 5.57, P = 0.021). Post hoc tests revealed lower peak hip flexion moment on the operated limb compared to the control limb (P < 0.001), but no significant difference between the non-operated limb and the control limb (P = 0.247). Examining peak knee flexion moment, revealed a significant group-by-limb interaction (F1,66 = 24.81, P < 0.001). Post hoc tests revealed lower peak knee flexion moment on the operated limb compared to the control limb (P < 0.001), and higher peak knee flexion moment on the non-operated limb compared to the control limb (P = 0.024). For peak hip adduction moment, there was no group-by-limb interaction (F1,66 = 2.42, P = 0.124), no effect of limb (F1,66 = 3.23, P = 0.077), and no effect of group (F1,66 = 1.93, P = 0.169).
For trunk kinematics, subjects in control group had a lateral trunk angle that was not significantly different than zero (P = 0.856). There was no significant difference in lateral trunk angle between the 3 months THA and control groups (P = 0.076) (Table 2).
Discussion
In this study, we evaluated movement patterns during sit-to-stand in patients before and 3 months after unilateral THA and compared the post-operative data to that of a control group. Prior to THA, subjects had lower frontal and sagittal moments on the operated side and had asymmetrical VGRF with less force on the operated side. Although there were significant improvements in kinetic and kinematic symmetry 3 months after THA compared to pre-operative values, subjects continued to rely on the non-operated leg. This was evident in the significant differences observed between limbs in the THA group and when compared to the control group.
Prior to THA, subjects preferentially shifted their weight toward the non-operated side and unloaded the operated side, as evidenced by the 24% lower peak VGRF on the operated limb. Previous authors have found similar weight bearing asymmetries in patients with hip OA using instrumented shoes [27] and conventional motion analysis [16,28]. The reduction in VGRF likely contributed to the reduced joint moments on the operated limb. Subjects before surgery had less peak hip (24%) and knee flexion (32%) moments on the operated side compared to the non-operated side. Previous studies have found that individuals with mild-moderate hip OA have 19%–20% lower sagittal hip and knee joint moments in the operated side [28], suggesting that the asymmetrical movement patterns may start early in the course of the disease and substantially increase by the time the patient is ready to undergo THA.
THA did have a positive influence on movement patterns and there were consistent improvements in symmetry 3 months after THA. These improvements were particularly evident for the VGRF as well as sagittal hip and knee moments, which demonstrated 6%–11% increase in the operated limb and a concomitant decrease of 4%–8% on the non-operated limb. There was also evidence of improvements in proximal asymmetries, as lateral trunk angle was reduced to 2.4° after surgery, from an initial angle of 3.95° pre-operatively. Despite a trend of improved symmetry at 3 months, most of the biomechanical variables still showed significant interlimb differences after THA, as demonstrated by the 16% higher peak VGRF on the non-operated limb 3 months after THA. It was also apparent that lower limb biomechanics were not restored to normal after THA. This was particularly true for the frontal plane kinetics, in which subjects after THA had 25% lower external hip adduction moment in the operated limb compared to the control group. It is possible that this difference in frontal plane mechanics is attributed to persistent hip abductor weakness, which is the weakest hip muscle group after THA [23].
Although the operated limb of patients after THA had lower VGRF and moments compared to the control group, there were also differences in the non-operated limb. Subjects 3 months after THA had almost 7% greater VGRF on the non-operated leg compared to the control group. Although we only evaluated subjects 3 months after THA, which can be argued is still in the recovery phase [29], other studies have shown that these asymmetries do not resolve in the long-term post-surgery. Boonstra et al reported that at one year following THA, patients placed 17% greater VGRF under the non-operated compared to operated limb [14], while Talis et al found that patients had 22% greater VGRF under the non-operated compared to operated limb even 4 years after THA [13]. Lamontagne et al [15] found lower hip kinematics and kinetics of the operated side of individuals up to 15 months after THA compared to both the non-operated side and to the healthy control subjects. This pattern of overloading coincides with the non-random progression of OA in lower extremity joints, in which the contralateral joints are the next most likely joints to show OA progression after THA [30]. It is possible that continued reliance on the non-operated limb expedites the cartilage wear and symptomatic progression on the non-operated side, although future prospective studies are needed to substantiate this possibility. Persistent movement asymmetries are also concerning because greater weight bearing asymmetry during the STS task is related to worse functional performance in patients after total knee arthroplasty (TKA) [31]. It is possible that favoring the non-operated limb to complete functional tasks does not completely compensate for the functional deficits associated with the surgical limb. It is logical to expect a similar phenomenon in patients with movement asymmetries after unilateral THA.
We expected that subjects would consistently shift their trunk toward the operated side to decrease the biomechanical demand on the hip abductors by lateralization of the VGRF and subsequent reduction in the external adduction moment. However, the high degree of variability at the trunk in the frontal plane suggests that patients after THA do not all adopt the same proximal strategy. It is possible that different physical impairments drive the variability in proximal compensations or that patients adopt different compensatory patterns prior to surgery. Pain avoidance, joint instability, or joint sensory deficits that were present prior to THA or developed after surgery may be factors that contribute to the unloading of the operated limb and may require targeted retraining to resolve. STS movement strategies may also be affected by different perioperative factors such as surgical approach, choice of implants, femoral neck/shaft offset, and leg length.
This study is not without limitations. First, our sample included subjects who underwent THA with different types of surgical approaches. The anterolateral and the direct lateral approaches entail cutting of the hip abductor muscles, whereas these muscles are not dissected in the posterior approach [32,33]. The surgical approach may affect the muscle strength recovery and the change in movement patterns after surgery. Second, the subjects in the control group were not matched to those in the THA group; BMI and mass were significantly higher in THA group which is expected in subjects who experience join pain and restricted mobility. However, peak VGRF was normalized to the individual’s weight, and joint moments were normalized to body mass and height, which accounts for the differences in the biomechanical variables.
This study is the first to have investigated the three dimensional lower limb joint kinetics and trunk compensations in patients before and 3 months after THA during the performance of the STS task. THA can decrease pain, improve functional ability, and reduce movement asymmetries in patients shortly after surgery; however, movement patterns continue to be distinctly asymmetrical and abnormal 3 months after THA. By 3 months after THA, patients are most likely participating in outpatient rehabilitation and transitioning to home or independent exercise programs. Examining movement symmetry at 3 months post-surgery may guide the physiotherapists to provide targeted interventions to normalize movement patterns. Work from patients after TKA has shown that greater movement asymmetries before and 3 months after surgery is correlated with worse functional performance [34] and muscle strength asymmetries [35], which may also hold true in the THA population. Further research is needed to identify the underlying impairments that can be targeted in the post-operative rehabilitation program. Moreover, further work is needed to examine the influence of surgical factors such as different common surgical approaches, choice of implants, femoral neck/shaft offset, and leg length on changes in STS biomechanics post-THA. Although we have evaluated biomechanical metrics 3 months after THA, movement patterns may continue to improve at longer term follow-ups [16]. Additional longitudinal research is warranted to identify whether movement asymmetries exist in the long-term.
Acknowledgments
Funding: This study was financially supported by the National Institutes of Health (K12 HD055931), Comprehensive Opportunities in Rehabilitation Research Training (CORRT), the University of Delaware Research Foundation, and a scholarship from The University of Jordan to Mrs. Abujaber.
We acknowledge Portia Flowers, PhD for assistance in data collection. Liza Walker and research core staff in Delaware Rehabilitation Institute are acknowledged for recruiting subjects. Finally, we thank all the participants in this study.
Footnotes
No author associated with this paper has disclosed any potential or pertinent conflicts which may be perceived to have impending conflict with this work. For full disclosure statements refer to http://dx.doi.org/10.1016/j.arth.2015.05.024.
References
- 1.Mangione CM, Goldman L, Orav EJ, et al. Health-related quality of life after elective surgery: measurement of longitudinal changes. J Gen Intern Med. 1997;12:686. doi: 10.1046/j.1525-1497.1997.07142.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.O’Brien S, Bennett D, Doran E, et al. Comparison of hip and knee arthroplasty outcomes at early and intermediate follow-up. Orthopedics. 2009;32:168. [PubMed] [Google Scholar]
- 3.Judd DL, Dennis DA, Thomas AC, et al. Muscle strength and functional recovery during the first year after THA. Clin Orthop Relat Res. 2013 doi: 10.1007/s11999-013-3136-y. http://dx.doi.org/10.1007/s11999-013-3136-y. [DOI] [PMC free article] [PubMed]
- 4.De Groot IB, Bussmann HJ, Stam HJ, et al. Small increase of actual physical activity 6 months after total hip or knee arthroplasty. Clin Orthop Relat Res. 2008;466:2201. doi: 10.1007/s11999-008-0315-3. http://dx.doi.org/10.1007/s11999-008-0315-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Heiberg KE, Ekeland A, Bruun-Olsen V, et al. Recovery and prediction of physical functioning outcomes during the first year after total hip arthroplasty. Arch Phys Med Rehabil. 2013;94:1352. doi: 10.1016/j.apmr.2013.01.017. http://dx.doi.org/10.1016/j.apmr.2013.01.017. [DOI] [PubMed] [Google Scholar]
- 6.Van den Akker-Scheek I, Zijlstra W, Groothoff JW, et al. Physical functioning before and after total hip arthroplasty: perception and performance. Phys Ther. 2008;88:712. doi: 10.2522/ptj.20060301. http://dx.doi.org/10.2522/ptj.20060301. [DOI] [PubMed] [Google Scholar]
- 7.Vissers MM, Bussmann JB, Verhaar J, et al. Recovery of physical functioning after total hip arthroplasty: systematic review and meta-analysis of the literature. Phys Ther. 2011;91:615. doi: 10.2522/ptj.20100201. http://dx.doi.org/10.2522/ptj.20100201. [DOI] [PubMed] [Google Scholar]
- 8.Fujita K, Makimoto K, Tanaka R, et al. Prospective study of physical activity and quality of life in Japanese women undergoing total hip arthroplasty. J Orthop Sci. 2013;18:45. doi: 10.1007/s00776-012-0318-5. http://dx.doi.org/10.1007/s00776-012-0318-5. [DOI] [PubMed] [Google Scholar]
- 9.Bourne RB, Chesworth B, Davis A, et al. Comparing patient outcomes after THA and TKA: is there a difference? Clin Orthop Relat Res. 2010;468:542. doi: 10.1007/s11999-009-1046-9. http://dx.doi.org/10.1007/s11999-009-1046-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Miki H, Sugano N, Hagio K, et al. Recovery of walking speed and symmetrical movement of the pelvis and lower extremity joints after unilateral THA. J Biomech. 2004;37:443. doi: 10.1016/j.jbiomech.2003.09.009. http://dx.doi.org/10.1016/j.jbiomech.2003.09.009. [DOI] [PubMed] [Google Scholar]
- 11.Perron M, Malouin F, Moffet H, et al. Three-dimensional gait analysis in women with a total hip arthroplasty. Clin Biomech. 2000;15:504. doi: 10.1016/s0268-0033(00)00002-4. [DOI] [PubMed] [Google Scholar]
- 12.Lamontagne M, Beaulieu ML, Beaulé PE. Comparison of joint mechanics of both lower limbs of THA patients with healthy participants during stair ascent and descent. J Orthop Res. 2011;29:305. doi: 10.1002/jor.21248. http://dx.doi.org/10.1002/jor.21248. [DOI] [PubMed] [Google Scholar]
- 13.Talis V, Grishin A, Solopova I. Asymmetric leg loading during sit-to-stand, walking and quiet standing in patients after unilateral total hip replacement surgery. Clin Biomech. 2008;23:424. doi: 10.1016/j.clinbiomech.2007.11.010. http://dx.doi.org/10.1016/j.clinbiomech.2007.11.010. [DOI] [PubMed] [Google Scholar]
- 14.Boonstra MC, Schreurs BW, Verdonschot N. The sit-to-stand movement: differences in performance between patients after primary total hip arthroplasty and revision total hip arthroplasty with acetabular bone impaction grafting. Phys Ther. 2011;91:547. doi: 10.2522/ptj.20090376. http://dx.doi.org/10.2522/ptj.20090376. [DOI] [PubMed] [Google Scholar]
- 15.Lamontagne M, Beaulieu ML, Varin D, et al. Lower-limb joint mechanics after total hip arthroplasty during sitting and standing tasks. J Orthop Res. 2012;30:1. doi: 10.1002/jor.22127. http://dx.doi.org/10.1002/jor.22127. [DOI] [PubMed] [Google Scholar]
- 16.Caplan N, Stewart S, Kashyap S, et al. The effect of total hip and hip resurfacing arthroplasty on vertical ground reaction force and impulse symmetry during a sit-to-stand task. Clin Biomech (Bristol, Avon) 2014;29:1164. doi: 10.1016/j.clinbiomech.2014.09.008. http://dx.doi.org/10.1016/j.clinbiomech.2014.09.008. [DOI] [PubMed] [Google Scholar]
- 17.Dall PM, Kerr A. Frequency of the sit to stand task: an observational study of free-living adults. Appl Ergon. 2010;41:58. doi: 10.1016/j.apergo.2009.04.005. http://dx.doi.org/10.1016/j.apergo.2009.04.005. [DOI] [PubMed] [Google Scholar]
- 18.Rodosky MW, Andriacchi TP, Andersson GB. The influence of chair height on lower limb mechanics during rising. J Orthop Res. 1989;7:266. doi: 10.1002/jor.1100070215. http://dx.doi.org/10.1002/jor.1100070215. [DOI] [PubMed] [Google Scholar]
- 19.Ploutz-Snyder LL, Manini T, Ploutz-Snyder RJ, et al. Functionally relevant thresholds of quadriceps femoris strength. J Gerontol A Biol Sci Med Sci. 2002;57:B144. doi: 10.1093/gerona/57.4.b144. [DOI] [PubMed] [Google Scholar]
- 20.Janssen WG, Bussmann HB, Stam HJ. Determinants of the sit-to-stand movement: a review. Phys Ther. 2002;82:866. [PubMed] [Google Scholar]
- 21.Doorenbosch CA, Harlaar J, Roebroeck ME, et al. Two strategies of transferring from sit-to-stand; the activation of monoarticular and biarticular muscles. J Biomech. 1994;27:1299. doi: 10.1016/0021-9290(94)90039-6. http://dx.doi.org/10.1016/0021-9290(94)90039-6. [DOI] [PubMed] [Google Scholar]
- 22.Goulart FR, Valls-Solé J. Patterned electromyographic activity in the sit-to-stand movement. Clin Neurophysiol. 1999;110:1634. doi: 10.1016/s1388-2457(99)00109-1. [DOI] [PubMed] [Google Scholar]
- 23.Rasch A, Dalén N, Berg HE. Muscle strength, gait, and balance in 20 patients with hip osteoarthritis followed for 2 years after THA. Acta Orthop. 2010;81:183. doi: 10.3109/17453671003793204. http://dx.doi.org/10.3109/17453671003793204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schwartz MH, Rozumalski A. A new method for estimating joint parameters from motion data. J Biomech. 2005;38:107. doi: 10.1016/j.jbiomech.2004.03.009. http://dx.doi.org/10.1016/j.jbiomech.2004.03.009. [DOI] [PubMed] [Google Scholar]
- 25.Weinhandl JT, O’Connor KM. Assessment of a greater trochanter-based method of locating the hip joint center. J Biomech. 2010;43:2633. doi: 10.1016/j.jbiomech.2010.05.023. http://dx.doi.org/10.1016/j.jbiomech.2010.05.023. [DOI] [PubMed] [Google Scholar]
- 26.Bouffard V, Begon M, Champagne A, et al. Hip joint center localisation: a biomechanical application to hip arthroplasty population. World J Orthop. 2012;3:131. doi: 10.5312/wjo.v3.i8.131. http://dx.doi.org/10.5312/wjo.v3.i8.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Martinez-Ramirez A, Weenk D, Lecumberri P, et al. Pre-operative ambulatory measurement of asymmetric leg loading during sit to stand in hip arthroplasty patients. IEEE Trans Neural Syst Rehabil Eng. 2013 doi: 10.1109/TNSRE.2013.2263394. http://dx.doi.org/10.1109/TNSRE.2013.2263394. [DOI] [PubMed]
- 28.Eitzen I, Fernandes L, Nordsletten L, et al. Weight-bearing asymmetries during sit-to-stand in patients with mild-to-moderate hip osteoarthritis. Gait Posture. 2014;39:683. doi: 10.1016/j.gaitpost.2013.09.010. http://dx.doi.org/10.1016/j.gaitpost.2013.09.010. [DOI] [PubMed] [Google Scholar]
- 29.Davis AM, Perruccio AV, Ibrahim S, et al. The trajectory of recovery and the interrelationships of symptoms, activity and participation in the first year following total hip and knee replacement. Osteoarthritis Cartilage. 2011;19:1413. doi: 10.1016/j.joca.2011.08.007. http://dx.doi.org/10.1016/j.joca.2011.08.007. [DOI] [PubMed] [Google Scholar]
- 30.Shakoor N, Block JA, Shott S, et al. Nonrandom evolution of end-stage osteoarthritis of the lower limbs. Arthritis Rheum. 2002;46:3185. doi: 10.1002/art.10649. [DOI] [PubMed] [Google Scholar]
- 31.Christiansen CL, Bade MJ, Judd DL, et al. Weight-bearing asymmetry during sit-stand transitions related to impairment and functional mobility after total knee arthroplasty. Arch Phys Med Rehabil. 2011;92:1624. doi: 10.1016/j.apmr.2011.05.010. http://dx.doi.org/10.1016/j.apmr.2011.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gore DR, Murray MP, Sepic SB, et al. Anterolateral compared to posterior approach in total hip arthroplasty: differences in component positioning, hip strength, and hip motion. Clin Orthop Relat Res. 1982:180. 7075057. [PubMed] [Google Scholar]
- 33.Hardinge K. The direct lateral approach to the hip. 1982;64:17. doi: 10.1302/0301-620X.64B1.7068713. [DOI] [PubMed] [Google Scholar]
- 34.Christiansen CL, Stevens-Lapsley JE. Weight-bearing asymmetry in relation to measures of impairment and functional mobility for people with knee osteoarthritis. Arch Phys Med Rehabil. 2010;91:1524. doi: 10.1016/j.apmr.2010.07.009. http://dx.doi.org/10.1016/j.apmr.2010.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mizner R, Snyder-Mackler L. Altered loading during walking and sit to stand is affected by quadriceps weakness after total knee arthroplasty. J Orthop Res. 2005;23:1083. doi: 10.1016/j.orthres.2005.01.021. http://dx.doi.org/10.1016/j.orthres.2005.OI.O21. [DOI] [PubMed] [Google Scholar]