Abstract
Low calcium absorption is associated with low bone mass and fracture. In this study, we use gold standard methods of fractional calcium absorption (FCA) to determine whether polymorphisms of intestinal receptors, vitamin D receptor (VDR) and estrogen receptor α (ESR1), influence the response to energy restriction. Fractional calcium absorption was measured using dual stable isotopes (42Ca and 43Ca) in women given adequate calcium and vitamin D and examined at baseline and after 6 weeks of energy restriction or no intervention. After genotyping, the relationship between VDR and ESR1 genotypes/haplotypes and FCA response was assessed using several genetic models. One-hundred and sixty-eight women (53 ± 11 years of age) were included in this analysis. The ESR1 polymorphisms, PvuII and XbaI and VDR polymorphisms (TaqI, ApaI) did not significantly influence FCA. The BB genotype of the VDR polymorphism, BsmI, was associated with a greater decrease in FCA than the Bb/ bb genotype. Multiple linear regression showed that the BsmI polymorphism or the VDR haplotype, BAt, in addition to changes in weight and vitamin D intake explained ~16% of the variation in changes in FCA. In conclusion, the reduction in calcium absorption due to energy restriction is greatest for those with the BB genotype. Previous candidate gene studies show that VDR polymorphisms are associated with higher risk for osteoporosis, and the current study supports the notion that the BsmI polymorphism in intestinal VDR may be contributing to alterations in bone health.
Keywords: calcium absorption, estrogen receptor (ESR1), gene polymorphism, vitamin D receptor (VDR)
Introduction
The pathogenesis of osteoporosis is influenced by a wide variety of environmental factors such as age, nutrition, and race. Calcium absorption is an important determinant of bone mineral density (BMD) and osteoporotic fracture risk [1]. Dietary and hormonal factors do not completely explain the variation in calcium absorption. Up to 79% of the variation in calcium absorption is unexplained and may be due to genetic variability [2-7].
Vitamin D is a major regulator of the saturable component of calcium absorption in the small intestine and bone remodeling, and its effects are largely mediated by the vitamin D nuclear receptor (VDR). The VDR gene has been postulated to be a major locus for the genetic effects on calcium absorption, but there are limited studies [8, 9]. In a cross-over design study using 2 levels of calcium intake (1500 mg/d for 2 weeks and <300 mg/d for 2 weeks) in sixty postmenopausal women, the VDR polymorphism, BsmI, was found to be associated with calcium absorption, but only during very low calcium intake [8]. Also, in a small cross-sectional study in premenopausal women consuming the recommended calcium intake, it was found that a VDR haplotype (BsmI, ApaI, TaqI polymorphisms) is associated with calcium absorption [9]. The ESR1 gene is another strong candidate for the genetic regulation of calcium absorption because of the presence of estrogen receptor-α in the intestine and the well-established role of estrogen in intestinal calcium absorption [10, 11]. However, the association between the commonly studied ESR1 polymorphisms, XbaI and PvuII, and calcium absorption has not been extensively examined [12]. It has previously been shown that calcium absorption is attenuated with energy restriction in older women [13]. Therefore, the goal in this investigation was to determine whether the known effects of energy restriction to reduce calcium absorption are further influenced by several well-studied VDR and ESR1 polymorphisms.
Materials and Methods
Subjects
One hundred and ninety-nine overweight or obese women who participated in previous calcium absorption trials in the laboratory from 2001-2012 were eligible to be included in this study [13-15]. Of these, one hundred and sixty-eight women (ages 24-75 yrs) had whole blood drawn and were included in this retrospective analysis. These samples are part of the Osteoporosis, Weight Loss and Endocrine database (trials supported by AG12161). All participants were free from any disease state or medications known to influence bone metabolism, and none of them were on hormone replacement therapy. The subjects signed an informed consent approved by the Institutional Review Board at Rutgers University and Saint Peters University Hospital, New Brunswick, NJ, USA.
Study Design
Prior to the calcium absorption measurement, all women were provided with 1-1.2g/day of calcium (diet plus supplement) for a month to stabilize calcium intake (Citracal, Bayer Inc., Morristown, NJ, USA). Similarly, all women were given 400 IU of vitamin D in the form of a multivitamin tablet (NatureMade, Mission Hill, CA, USA). After the 1 month stabilization period, women were assigned to groups that either lost weight (WL, n = 104) or maintained weight (WM, n=64). Women in the WM group were asked to maintain their weight during the 6 week intervention. In the WL group, subjects were asked to reduce energy intake by 500-600 kcal/day using a standard nutrition education and behavior modification weight-reduction program that was offered weekly under the supervision of a dietitian (8-10/group).
Calcium absorption was measured at baseline and after 6 weeks of energy restriction or no intervention. A subset of 14 WL and 13 WM women were randomly assigned in a double blind manner to a higher intake of vitamin D3 (2500 IU/d) over 6 weeks, as described previously [14]. Because these women were equally distributed between the WL and WM groups using an identical protocol and showed similar FCA trends, they were also included in this analysis.
Bone and body composition
A total body scan using dual-energy x-ray absorptiometry (Lunar Prodigy Advanced; GE-Lunar, Madison, WI; enCORE software, v. 8.10.027) was performed to characterize the population for baseline body composition of soft tissues and bone (CV < 1%).
Biochemical Analysis
Serum 25-hydroxyvitamin D [25(OH)D], 1,25 dihydroxyvitamin D [1,25(OH)2D3], and ultra-sensitive estradiol (E2) were measured by radioimmunoassay (RIA; DiaSorin, Stillwater, MI, USA; CV <12.5% for vitamin D; DSL, Webster, TX, USA; CV < 8.9% for E2) using internal standards on all samples and external standards on a subset (vitamin D external quality-assessment scheme). Intact parathyroid hormone (PTH) was determined by immunoradioassay (Scantibodies, Santee, CA, USA, CV <6.8%; DSL, Webster, TX, USA; CV, < 5.2%).
True fractional calcium absorption (FCA)
The stable isotopes, 42Ca (96% enrichment) and 43Ca (90% enrichment), were prepared for human use by the Pharmacy Department at St. Peters University Hospital, New Brunswick, NJ and purchased from Trace Sciences International (Delaware, USA). After mixtures were prepared, samples were tested for sterility and pyrogenicity. The dose was individualized (0.012mg/kg Ca42 and 0.017mg/kg Ca43) and prepared in syringes prior to the test. Briefly, the Ca absorption test required women to be admitted to the clinic between 7 and 9 AM after an overnight fast. After a fasting blood and urine sample were taken, a standard breakfast consisting of milk, toast, fruit and orange juice was served. The total Ca load of this meal was 200 mg and included 43Ca mixed with 120 ml skim milk (153 mg Ca). The milk was consumed under supervision, and the cup was rinsed with deionized water 3 times and all of this water was also consumed by volunteers. Immediately after breakfast, 42Ca was injected intravenously. A precision balance scale was used to weigh the syringes used containing the isotopes before and after the test. Instructions were given how to collect a pooled 24-hour urine sample. Volunteers were monitored during the day and remained at the University Inn overnight, and the 24-hour urine collection was collected by the researchers the following morning. Calcium was precipitated in urine samples as the oxalate salt and ashed to assess mineral content. Ratios of each isotope to 44Ca in 24 hour urine samples were determined by high-resolution, inductively coupled plasma mass spectrometry (Element-1; Finnigan MAT) (1% precision and accuracy). The day-to-day CV was 1.2%, as measured twice in 6 women [13]. Samples were measured before and six weeks after the dietary intervention.
Genotype and Haplotype Analysis
Genotypes for the VDR gene polymorphisms (BsmI, TaqI, ApaI) and ESR1 gene polymorphisms (XbaI and PvuII) were determined through polymerase chain reaction–restriction fragment length polymorphism (PCR–RFLP) analysis. Using the QIAamp DNA Blood Mini Kit (QIAGEN, Valencia, CA, USA), genomic DNA was extracted from whole blood samples that had been collected at baseline from each study subject. PCR amplification using a MJ Mini thermal cycler (Bio-Rad, Hercules, CA, USA) for each of the polymorphisms was then carried out as described previously [16, 17]. Forward and reverse primers for PCR for each individual VDR and ESR1 polymorphism were purchased from Sigma-Aldrich, St. Louis, MO, USA. The PCR products were then digested by their respective endonucleases (New England Biolabs, Ipswich, MA, USA) and run on a 1.75% agarose gel stained with ethidium bromide for visualization. Alleles with and without restriction sites for the polymorphism are denoted by lower and upper case letters, respectively (e.g. BsmI, “b” = presence of restriction site and “B” = absence of restriction site). Subsequent haplotype reconstruction was performed using PHASEv2.1.1 [18, 19].
Statistical Analysis
The genotype frequencies for each polymorphism were tested against Hardy-Weinberg ratios and larger study populations by the χ2 test. Linkage disequilibrium (LD), which is the non-random association of alleles at different positions on a gene, of the 3'UTR VDR polymorphisms, BsmI, ApaI, and TaqI and the ESR1 polymorphisms located in intron 1, XbaI and PvuII, was determined using Haploview v4.2 (Broad Institute, Cambridge, MA, USA) [20].
Additive, dominant, and recessive models were defined and tested for each of the VDR and ESR1 polymorphisms. The additive model treats all three genotypes (e.g. YY, Yy, yy) differently, whereas the dominant model assumes that only one copy of the recessive allele is sufficient to result in a phenotype, and the recessive model assumes that two copies of the recessive allele are required to result in a specific phenotype. One-way analysis of covariance (ANCOVA), including age, BMI, and estradiol as covariates with Tukey's post-hoc analyses was used to determine how the individual VDR and ESR1 polymorphisms and haplotypes predict variations in FCA at baseline. Two-way ANOVA, using diet and the additive, dominant, or recessive genetic models as the two independent factors was conducted to determine the genetic influence on changes in FCA. Estradiol and age were included as covariates in subsequent analyses. Tukey's post-hoc analysis was performed when the F statistic for the model was below the specified α value of 0.05. Kruskal-Wallis non-parametric ANOVA was also used due to the different group sizes.
Multiple linear regression models were used to quantify the amount of variability in the FCA response that is attributable to the gene polymorphisms. The additive, dominant, and recessive genetic models, as well as the percent change in fat intake, vitamin D intake, body weight, serum PTH, 25OHD, 1,25(OH)2D, and estradiol were used as independent predictors of change in FCA. The magnitude of the FCA difference between genotype groups was estimated by effect size using the standardized difference between two means.
All variables were tested for normality by comparing the mean and median and creating normal probability plots of the individual variables. If the variables were not normally distributed we reported the median and interquartile range, and conducted log transformations. Statistical analyses were carried out using SAS v9.2 software (SAS Institute, Cary, North Carolina). A P-value < 0.05 was considered to be statistically significant.
Results
Baseline characteristics of body composition, FCA, serum concentrations of hormones, and nutrient intake are included in Table 1 for 168 women. The population is largely Caucasian (86%). Characteristics in the WL and WM groups did not differ significantly at baseline (Table 1).
Table 1.
Baseline characteristics of women1
| Variable | All (n=168) | Weight loss (n=104) | Weight maintenance (n=64) | P value for WL/WM groups2 |
|---|---|---|---|---|
| Age | 53.0 ± 11.4 | 53.1 ± 11.5 | 52.7 ± 11.3 | 0.799 |
| Weight (kg) | 75.8 ± 10.2 | 76.2 ± 10.8 | 75.0 ± 9.1 | 0.422 |
| BMI (kg/m2) | 28.6 ± 3.2 | 28.5 ± 3.3 | 28.7 ± 3.0 | 0.657 |
| Lean mass (kg)3 | 40.1 ± 4.8 | 40.2 ± 4.9 | 40.0 ± 4.7 | 0.848 |
| Fat mass (kg)3 | 31.6 ± 6.9 | 31.9 ± 7.2 | 31.2 ± 6.3 | 0.493 |
| BMC (g)4 | 2442 ± 336 | 2452 ± 330 | 2424 ± 348 | 0.601 |
| FCA (%) | 24.9 ± 7.6 | 24.6 ± 7.0 | 25.5 ± 8.5 | 0.471 |
| Hormones | ||||
| Estradiol (pg/ml)6 | 22.7 ± 21.5 | 23.3 ± 22.2 | 21.9 ± 20.5 | 0.690 |
| PTH (pg/ml) | 40.2 ± 21.7 | 40.9 ± 22.6 | 39.0 ± 20.4 | 0.398 |
| 25(OH)D (ng/ml) | 29.6 ± 8.6 | 28.7 ± 8.1 | 31.0 ± 9.4 | 0.093 |
| 1,25(OH)2D (pg/ml) | 50.6 ± 16.6 | 51.3 ± 16.6 | 49.4 ± 16.8 | 0.488 |
| Nutrient Intake7 | ||||
| Calcium (mg/day) | 1193 ± 401 | 1181 ± 417 | 1212 ± 375 | 0.628 |
| Vitamin D (μg/day)5 | 11.9 ± 2.2 | 11.9 ± 2.5 | 11.8 ± 1.9 | 0.776 |
BMI body mass index, FCA true fractional calcium absorption, BMC total body bone mineral content, 1,25(OH)2D 1,25-dihydroxyvitamin D3, 25OHD 25-hydroxyvitamin D (multiply by 2.5 to convert to nmol/L), PTH parathyroid hormone
Data (mean ± SD)
Analysis was performed using a one-way ANOVA.
Missing subjects, c(n=1), d(n=2); e(n=4)
Missing subjects, c(n=1), d(n=2); e(n=4)
Missing subjects, c(n=1), d(n=2); e(n=4)
Estradiol was non-normally distributed, therefore we calculated the median and IQR for each group: All, 16.1 (3.6-133.5); WL, 17.5 (4.9-133.5); WM, 15.2 (3.6-125.0). The log transformation of estradiol was normally distributed.
Nutrient intake includes the amount from diet plus multivitamin/mineral with 10 μg (400 IU) of vitamin D and 200 mg Ca plus individualized Ca supplement.
Genotype Frequencies
The genotype frequencies for the VDR and ESR1 polymorphisms in the entire population were found to be in Hardy-Weinberg equilibrium. The χ2 analysis revealed that frequencies of the ApaI, FokI, and PvuII genotypes are comparable to a larger population (Table 2) [21]. The BsmI, ApaI, and TaqI polymorphisms on the VDR gene were in strong linkage disequilibrium (LD) with one another (D' > 0.88), where D'=1.0 represents perfect LD. The XbaI and PvuII polymorphisms on the ESR1 gene were also in strong LD with one another (D' > 0.79). This strong LD among the polymorphisms justified the determination of the VDR and ESR1 haplotypes. The frequencies for the most common haplotypes in our population are presented in Table 3. Chi square (χ2) analysis showed that the frequencies of the ESR1 haplotypes did not differ significantly from a larger reference population [22,23].
Table 2.
VDR and ESR1 genotype frequencies in the current study compared to a larger population [21]
| Gene | Polymorphism1 | Current study n=168 | 1000 Genomes Project n=1092 |
|---|---|---|---|
| VDR | BsmI* | ||
| BB | 14.9% | 7.0% | |
| Bb | 42.9% | 39.0% | |
| bb | 42.3% | 54.0% | |
| ApaI | |||
| AA | 29.2% | 25.4% | |
| Aa | 51.2% | 50.0% | |
| aa | 19.6% | 24.6% | |
| TaqI* | |||
| TT | 41.1% | 54.2% | |
| Tt | 46.4% | 38.9% | |
| tt | 12.5% | 7.0% | |
| FokI* | |||
| FF | 44.1% | 42.6% | |
| Ff | 42.9% | 45.3% | |
| Ff | 13.1% | 12.0% | |
| ESR1 | PvuII | ||
| PP | 23.8% | 19.0% | |
| Pp | 44.1% | 49.2% | |
| Pp | 32.1% | 31.8% | |
| XbaI* | |||
| XX | 13.1% | 6.6% | |
| Xx | 43.5% | 38.1% | |
| xx | 43.5% | 55.4% |
VDR vitamin D receptor gene, ESR1 estrogen receptor-α
Reference SNP (rs) numbers for “common” genotypes: BsmI – rs1544410; ApaI – rs7975232; TaqI – rs731236; FokI – rs2228570; PvuII – rs2234693; XbaI – rs9340799
Differed significantly compared to reference population [21]
Table 3.
Weight, hormone, and calcium absorption changes due to six week intervention
Women in the WL group lost 4.0 ± 1.5% of initial body weight, which was significantly more than women who maintained weight (0.02 ± 1.5%) (p < 0.0001). Serum concentrations of 25(OH)D increased significantly more in the WL (3.4 ± 6.2 ng/mL) than WM group (0.8 ± 4.6 ng/mL) (p < 0.01). However, the greater decrease in FCA for the WL group (−9.0 ± 21.6%) than the WM group (−4.0 ± 19.1%) did not reach significance (p = 0.13). In addition, there were no significant differences for changes in serum 1,25(OH)2D (WL: 0.6 ± 15; WM: 0.9 ± 16.6 pg/mL), PTH (WL: −3.5 ± 12.1; WM: −1.7 ± 13.8 pg/mL), and estradiol (WL: 1.7 ± 33.1; WM: 0.9 ± 22.8 pg/mL) due to energy restriction over the 6 week study. There were also no significant differences in weight changes with the BB genotype compared to Bb or bb genotypes.
VDR polymorphisms and calcium absorption
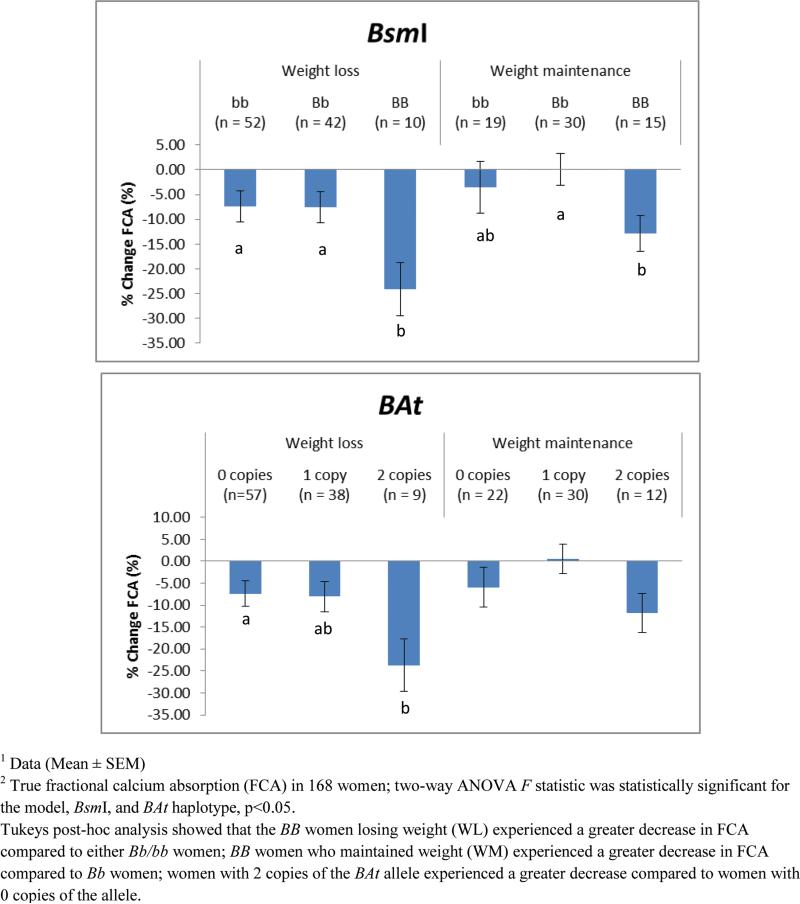
Baseline FCA was not significantly influenced by VDR polymorphisms (p > 0.10), BsmI (BB: 25.5 ± 1.6%, Bb: 24.4 ± 0.8%, bb: 25.3 ± 1.0%), ApaI (AA: 23.7 ± 1.1%, Aa: 25.6 ± 0.8%, aa: 25.0 ± 1.4%), TaqI (TT: 24.8 ± 1.0%, Tt: 24.7 ± 0.8%, tt: 26.2 ± 1.7%), and FokI (FF: 24.5 ± 0.9%, Ff: 25.6 ± 0.9%, ff: 24.2 ± 1.7%). Using the additive model in the 2-way ANOVA, the BB genotype resulted in an attenuated FCA response compared to Bb or bb (p < 0.01). Tukey's post-hoc analysis indicated that for women who lost weight, those with the BB genotype experienced a greater decrease in FCA (−24.1 ± 5.4%) compared to women with either the bb (−7.3 ± 3.3%) or the Bb genotypes (−7.6 ± 3.1%) (p < 0.05). Meanwhile, among women who maintained weight, those with the BB genotype (−12.8 ± 3.6%) experienced a greater decrease in FCA compared to women with the Bb genotype (0.1 ± 3.3%) (p < 0.05), but not those with the bb genotype (−3.6 ± 5.2%) (Figure 1). Because there were no significant differences between the Bb and bb genotypes and the additive model is not always adequate when the minor allele frequency is not close to 50%, we also tested recessive and dominant models for the individual polymorphisms [24]. Using the recessive model for BsmI, we also found that women with the BB genotype experienced a greater percentage decrease in FCA, compared to women in the combined group of bb/Bb genotypes (WL: p < 0.05; WM: p <0.06). There was a moderate to large effect size of the BsmI genotypes of 0.67 and 0.86 in the WM and WL groups, respectively.
Figure 1.
BsmI and BAt recessive models predict greater decrease in FCA during weight loss1,2
The additive model for the BAt haplotype showed that in the WL group, women with 2 copies (−23.7 ± 6.0%) experienced a significantly greater decrease in FCA (p < 0.05) compared to women with 0 copies (−7.4 ± 2.9%), but not those with 1 copy (−8.1± 3.4%). In the weight maintenance group there was a trend (p < 0.10) for women with 2 copies of the BAt allele (−11.9 ± 4.5%) to experience a greater decrease than women with 1 copy of the allele (0.5 ± 3.3%), but not those with 0 copies (−5.9 ± 4.5) (Figure 1). Using the recessive model for the BAt haplotype showed that having 2 copies compared to 0 or 1 copy resulted in a 16% greater decrease in FCA in the WL group (p < 0.05); whereas having 2 copies of the BAt allele resulted in a 10% greater decrease in FCA in the WM group (p > 0.10). Similar, to the BB genotype, the BAt haplotype had a large effect size of 0.81 in the WL group. When we included age and baseline estradiol (log-transformed) in the two-way ANOVA analysis, the BsmI polymorphism remained a significant predictor of change in FCA.
There were more women who have 0/1 copies of the BAt allele than women who have 2 copies, and more women with the Bb and bb genotypes than the BB genotype, as expected and described in Tables 2-3. Therefore, we also used non-parametric analysis, which revealed that the relationship between the BsmI and BAt recessive models and change in FCA remained significant (p <0.05).
Multiple linear regression analysis including percent change in FCA as the dependent variable, revealed that the recessive BsmI model and percent change in weight and vitamin D intake (dietary + supplement) were significant predictors of change in FCA over a 6 week period (p <0.05) and explained about 16% of the variation in FCA response (Table 4). Having the BB genotype led to a 0.23 standard deviation decrease in FCA. The regression model which replaced the BsmI model with the BAt haplotype predicted about 15% of the variation. In this model having two copies of the BAt allele resulted in a 0.21 standard deviation decrease in FCA (Table 4). When the changes in hormones were included in the multiple linear regression analysis, they were not found to be significant predictors of change in FCA. Because estradiol is not normally distributed in our population, we also repeated these statistical tests using log-transformed change in estradiol, which revealed the same findings. Also, understanding that both vitamin D intake and change in 25(OH)D are strongly correlated, we included change in 25(OH)D and vitamin D intake in separate models, and vitamin D intake was the only significant predictor.
Table 4.
| Variable | β coefficient | R2 | P value |
|---|---|---|---|
| BsmI | −0.229 | 4.3% | 0.006 |
| Weight | 0.155 | 2.4% | 0.041 |
| Vitamin D intake | 0.302 | 9.5% | <0.001 |
| Model R2 = 16.2% | |||
| BAt | −0.207 | 3.3% | 0.004 |
| Weight | 0.158 | 2.4% | 0.012 |
| Vitamin D intake | 0.294 | 9.5% | <0.001 |
| Model R2 = 15.2% | |||
BsmI genotype or BAt haplotype recessive models include independent predictors (Fat intake, vitamin D intake, body weight, serum PTH, 25OHD, 1,25D, and estradiol). Only significant predictors are included in the table. Abbreviations: VDR vitamin D receptor gene, FCA true fractional calcium absorption
A separate analysis was conducted for the WL and WM groups. In both the WL and WM group the BsmI recessive model remained a significant predictor of calcium absorption change (β = −0.229,−0.255 respectively, p <0.05). The BAt recessive model was only a significant predictor of calcium absorption change in the WL group (β = −0.210, p <0.05).
ESR1 polymorphisms and calcium absorption
The ESR1 polymorphisms, PvuII and XbaI, did not have any effect on baseline FCA or the response to energy restriction. In addition, these genotypes and haplotypes did not explain any of the variation in calcium absorption response.
Discussion
Calcium absorption is an important predictor of fracture risk, yet the large majority of calcium absorption variability cannot be explained by diet and hormones alone [1-6]. The association between VDR and ESR1 gene polymorphisms and fracture risk has been examined extensively [25-29]. In the current study, we examined common polymorphisms of the VDR and ESR1 genes, to determine their influence on fractional calcium absorption. We found that the VDR BsmI BB genotype and the BAt haplotype predicted a greater decrease in calcium absorption during short term energy restriction.
One mechanism believed to regulate the decline in bone mass during weight reduction is a reduction in calcium absorption during energy restriction [13]. It is believed that decreases in estradiol due to loss of fat mass, as well as increases in cortisol due to the presence of a low-energy state, may attribute to these observed decreases [13,14]. Lower fat intake during energy restriction may also contribute to the reduced calcium absorption [2,4]. It may also be related to the extent of weight loss, but this has not been confirmed in a clinical trial [30].
The current findings indicate that during energy restriction, genetic differences (e.g., BB genotype and BAt haplotype) exacerbate the expected decrease in calcium absorption. Previous studies have also found that there is less efficient absorption associated with the BB genotype [8,9]. An examination of late postmenopausal women revealed that the BB genotype compared tothe bb genotype is associated with reduced calcium absorption in women with low (300 mg/d) calcium intake, but not when intake was higher [8]. Also, in a cross-sectional study, premenopausal women with the BAt haplotype had significantly lower levels of calcium absorption than women with the baT haplotype [9]. In addition, in a separate pilot analysis of twenty-seven women who were randomly assigned in a double blind manner to 2500 IU/d or 400 IU/d supplemental vitamin D3 intake, the FCA response to high vitamin D intake was significantly attenuated in women with the BB compared to bb genotype [31]. These data indicate that VDR polymorphisms exhibit a modest effect on calcium absorption even under stable conditions, suggesting that weight loss is not the only contributing factor to calcium absorption. Nevertheless, the BB phenotype is more strongly expressed under more stressful physiological conditions, such as energy and calcium intake restriction, known to alter calcium demands [8, 9, 16].
With greater decreases in calcium absorption due to the BB genotype and the BAt haplotype, both would be expected to negatively affect bone. In fact, previous meta-analyses have suggested that the BB genotype is associated with lower BMD and greater fracture risk than bb [25, 26]. In a meta-analysis of 39 studies it was shown that postmenopausal women with the BB genotype had significantly lower BMD at the spine than women with the bb genotype [25]. Similarly, in a more recent meta-analysis of 17 studies, there was a higher frequency of the BB genotype in fracture cases that included hip, spine and other sites [26]. GWAS studies have not been able to replicate this association, but these findings may differ due to the use of heterogeneous populations [32-35]. Our results, in addition to the findings in meta-analyses, suggest that the negative influence of VDR polymorphisms on bone health [25, 26] acts, at least in part, through a classical nutrition mechanism (intestinal absorption) and extends the speculation of others [36]. Understanding that lower calcium absorption might contribute to bone loss associated with weight reduction, it is important to consider that women with the BB genotype may be at an increased risk for detrimental bone outcomes.
Despite these findings, the mechanism through which the BsmI site and the BAt haplotype predict changes in calcium absorption is unknown. The reduction of calcium absorption in the WL women even though there is an increase in serum 25(OH)D suggests there may be a weight loss-induced vitamin D resistance that is exacerbated in the presence of the BB genotype. The BsmI polymorphism displays cell-type specific effects on mRNA stability [37], and studies report that the BsmI polymorphism, in conjunction with other 3’ UTR polymorphisms alters the transcription and stability of VDR mRNA [37,38]. Additionally, it has been found that a genetic polymorphism in the VDR promotor leads to lower VDR expression in the duodenum [39]. Therefore, it may be that the BsmI polymorphism modulates FCA in a similar manner by affecting the transcription and stability of intestinal VDR mRNA. It is also possible that the B allele and the BAt haplotype are in linkage disequilibrium with alleles of a functional polymorphic site that alters the transcript levels of the VDR gene or the stability of the resultant protein, thus affecting the VDR dependent intestinal calcium absorption [37]. A study examining the impact of the BsmI polymorphism and BsmI-ApaI-TaqI haplotypes on stability efficiency of VDR mRNA in intestinal cells may help elucidate the mechanism through which these polymorphisms influence FCA.
Our candidate gene study has strengths and limitations. Compared to other studies that have examined the relationship between candidate genes and bone health outcomes, our sample size is small [25,26]. Yet, in comparison to other calcium absorption studies that have examined the association with VDR and ESR1 gene polymorphisms [8,9], our sample size is larger providing more definitive evidence that the BB genotype is a risk factor for low absorption. Because of our small sample size, we were also able to reduce the heterogeneity of the population by controlling for Ca and vitamin D intake, weight, race, and sunlight exposure. However, using a primarily Caucasian and overweight/obese population may have skewed the frequencies of the BsmI polymorphism and the VDR haplotypes compared to the greater racial diversity in other studies [21], reducing the generalizability of the findings. For instance, there is a greater frequency of the B allele in the Caucasian population compared to both Asian and African populations [37]. Furthermore, in a recent study including 402 obese and 489 non-obese women, the B allele was found to be significantly more frequent in obese individuals [40]. Moreover, we purposefully included individuals of all ages to maximize the sample size for the genetic polymorphisms, with the assumption that the genotype would exacerbate the effect of diet on FCA, if there was indeed a gene-nutrient interaction.
Another advantage of small studies is that they allow for the use of more valid outcome measurements (e.g., FCA using dual isotopes) on a limited sample, which would be cost-prohibitive or too invasive to impose on a larger sample. Thus, a strength of this study is that we used the dual stable-isotope method that is considered a gold standard to calculate calcium absorption that has not been used previously to examine the influence of genotypes [8,9,12].
This study is also unique because we analyzed the associations between the polymorphisms and the outcome variables using the additive, dominant, and recessive models. Many genetic studies only employ the additive model, which considers the genotypes, YY, Yy, and yy, to be different; however, this model is not always sufficient [24]. Furthermore, because our data remained significant after including hormones such as estradiol in two-way ANOVA and multiple linear regression analyses, we are more confident that the gene effect on calcium absorption was due to the polymorphisms and not due to other confounding variables. Nevertheless, the absence of these findings may be a limitation of sample size.
Recognizing that there are a multitude of polymorphisms on both the ESR1 and VDR candidate genes, we posit that genotyping subjects for additional polymorphisms within the VDR and ESR1 candidate genes will provide a more complete picture of the genetic basis for the variation in calcium absorption. Additionally, studying the relationship between other candidate genes such as GC, CYP2R1, CYP27B1, CYP24A1, CYP27A1, and DHCR7, all of which are important in vitamin D metabolism [41-43], and calcium absorption, may help explain the variation in absorption in response to diet or disease conditions. Overall, this work underscores the importance of both the genomic and/or metabolic profile, and the need to focus attention on treatment for those who need it most.
Highlights.
Low calcium absorption is associated with low bone mass and fracture risk, and caloric restriction reduces calcium absorption.
The influence of vitamin D receptor and estrogen receptor-α gene polymorphisms on fractional calcium absorption was examined during caloric restriction.
The BB genotype of the vitamin D receptor polymorphism, BsmI, was associated with the greatest reduction in calcium absorption.
Acknowledgements
We would like to thank Dr. Derek Gordon in the Genetics Department, Rutgers University for his advice on mathematical and statistical approaches on the data analysis. We would also like to thank Drs. Cifuentes, Riedt and Pop and the clinical staff who contributed to these efforts.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of interest: Brian Chang, Yvette Schlussel, Deeptha Sukumar, Stephen Schneider, and Sue Shapses declare that they have no conflict of interest.
Reference List
- 1.Nordin BE, O'Loughlin PD, Need AG, Horowitz M, Morris HA. Radiocalcium absorption is reduced in postmenopausal women with vertebral and most types of peripheral fractures. Osteoporos Int. 2004;15:27–31. doi: 10.1007/s00198-003-1493-1. doi: 10.1007/s00198-003-1493-1. [DOI] [PubMed] [Google Scholar]
- 2.Shapses SA, Sukumar D, Schneider SH, Schlussel Y, Brolin RE, Taich L. Hormonal and dietary influences on true fractional calcium absorption in women: role of obesity. Osteoporos Int. 2012;23:2607–14. doi: 10.1007/s00198-012-1901-5. doi: 10.1007/s00198-012-1901-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ramsubeik K, Keuler NS, Davis LA, Hansen KE. Factors associated with calcium absorption in postmenopausal women: A post hoc analysis of dual isotope studies. J Acad Nutr Diet. 2013;114:761–67. doi: 10.1016/j.jand.2013.07.041. doi: 10.1016/j.jand.2013.07.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wolf RL, Cauley JA, Baker CE, Ferrell RE, Charron M, Caggiula AW, et al. Factors associated with calcium absorption efficiency in pre and perimenopausal women. Am J Clin Nutr. 2000;72:466–71. doi: 10.1093/ajcn/72.2.466. [DOI] [PubMed] [Google Scholar]
- 5.Need AG, Morris HA, Horowitz M, Scopacasa E, Nordin BE. Relationships between intestinal calcium absorption, serum vitamin D metabolites and smoking in postmenopausal women. Osteoporos Int. 2002;13:83–8. doi: 10.1007/s198-002-8342-9. doi: 10.1007/s198-002-8342-9. [DOI] [PubMed] [Google Scholar]
- 6.Dawson-Hughes B. Calcium through the lifecycle. In: Weaver CM, Heaney RP, editors. Calcium in Human Health. Humana Press; 2006. pp. 369–77. [Google Scholar]
- 7.Replogle RA, Li Q, Zhang M, Fleet JC. Gene-by-diet interactions influence calcium absorption and bone density in mice. J Bone Miner Res. 2014;29:657–65. doi: 10.1002/jbmr.2065. doi: 10.1002/jbmr.2065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dawson-Hughes B, Harris SS, Finneran S. Calcium absorption on high and low calcium intakes in relation to vitamin D receptor genotype. J Clin Endocrinol Metab. 1995;80:3657–61. doi: 10.1210/jcem.80.12.8530616. http://dx.doi.org/10.1210/jcem.80.12.8530616. [DOI] [PubMed] [Google Scholar]
- 9.Wishart JM, Horowitz M, Need AG, Scopacasa F, Morris HA, Clifton PM, et al. Relations between calcium intake, calcitriol, polymorphisms of the vitamin D receptor gene, and calcium absorption in premenopausal women. Am J Clin Nutr. 1997;65:798–802. doi: 10.1093/ajcn/65.3.798. [DOI] [PubMed] [Google Scholar]
- 10.Fleet JC, Schoch RD. Molecular mechanisms for regulation of intestinal calcium absorption by vitamin D and other factors. Crit Rev Clin Lab Sci. 47:181–95. doi: 10.3109/10408363.2010.536429. doi: 103109/10408363.2010.536429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Taylor AH, Al-Azzawi F. Immunolocalisation of oestrogen receptor beta in human tissues. J Mol Endocrinol. 2000;24:145–55. doi: 10.1677/jme.0.0240145. doi: 10.1677/jme.0.0240145. [DOI] [PubMed] [Google Scholar]
- 12.Elnenaei MO, Chandra R, Mangion T, Moniz C. Genomic and metabolomic patterns segregate with responses to calcium and vitamin D supplementation. Br J Nutr. 2011;105:71–9. doi: 10.1017/S0007114510003065. http://dx.doi.org/10.1017/S0007114510003065. [DOI] [PubMed] [Google Scholar]
- 13.Cifuentes M, Riedt CS, Brolin RE, Field MP, Sherrell RM, Shapses SA. Weight loss and calcium intake influence calcium absorption in overweight postmenopausal women. Am J Clin Nutr. 2004;80:123–30. doi: 10.1093/ajcn/80.1.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shapses SA, Sukumar D, Schneider SH, Schlussel Y, Sherrell RM, Field MP, et al. Vitamin D supplementation and calcium absorption during caloric restriction: a randomized double-blind trial. Am J Clin Nutr. 2013;97:637–45. doi: 10.3945/ajcn.112.044909. doi: 10.3945/ajcn.112.044909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Riedt CS, Schlussel Y, von Thun N, Ambia-Sobhan H, Stahl Y, Field MP, et al. Premenopausal women do not lose bone during moderate weight loss with adequate or higher calcium intake. Am J Clin Nutr. 2007;85:972–80. doi: 10.1093/ajcn/85.4.972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ames SK, Ellis KJ, Gunn SK, Copeland KC, Abrams SA. Vitamin D receptor gene FokI polymorphism predicts calcium absorption and bone mineral density in children. J Bone Miner Res. 1999;14:740–46. doi: 10.1359/jbmr.1999.14.5.740. doi: 10.1359/jbmr.1999.14.5.740. [DOI] [PubMed] [Google Scholar]
- 17.Lorentzon M, Lorentzon R, Nordstrom P. Vitamin D receptor gene polymorphism is associated with birth height, growth to adolescence, and adult stature in healthy caucasian men: a cross-sectional and longitudinal study. J Clin Endocrinol Metab. 2000;85:1666–70. doi: 10.1210/jcem.85.4.6566. http://dx.doi.org/10.1210/jcem.85.4.6566. [DOI] [PubMed] [Google Scholar]
- 18.Stephens M, Smith NJ, Donnelly P. A new statistical method for haplotype reconstruction from population data. Am J Hum Genet. 2001;68:978–89. doi: 10.1086/319501. doi: 10.1086/319501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stephens M, Scheet P. Accounting for decay of linkage disequilibrium in haplotype inference and missing-data imputation. Am J Hum Genet. 2005;76:449–62. doi: 10.1086/428594. doi: 10.1086/428594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Barrett JC, Fry B, Maller J, Daly MJ. Haploview: analysis and visualization of LD and haplotype maps. Bioinformatics. 2005;21:263–65. doi: 10.1093/bioinformatics/bth457. doi: 10.1093/bioinformatics/bth457. [DOI] [PubMed] [Google Scholar]
- 21.1000 Genomes Project Consortium. Abecasis GR, Auton A, Brooks LD, DePristo MA, Durbin RM, et al. An integrated map of variation from 1,092 human genomes. Nature. 2012;495:56–65. doi: 10.1038/nature11632. doi:10.1038/nature11632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Uitterlinden AG, Pols HA, Burger H, Huang Q, Van Daele PL, Van Duijn CM, et al. A large-scale population-based study of the association of vitamin D receptor gene polymorphisms with bone mineral density. J Bone Miner Res. 1996;11:1241–48. doi: 10.1002/jbmr.5650110908. doi: 10.1002/jbmr.5650110908. [DOI] [PubMed] [Google Scholar]
- 23.Bagger YZ, Jorgensen HL, Heegaard AM, Bayer L, Hansen L, Hassager C. No major effect of estrogen receptor gene polymorphisms on bone mineral density or bone loss in postmenopausal women. Bone. 2000;26:111–16. doi: 10.1016/s8756-3282(99)00261-6. doi: 10.1016/S8756-3282(99)00261-6. [DOI] [PubMed] [Google Scholar]
- 24.Lettre G, Lange C, Hirschhorn JN. Genetic model testing and statistical power in population-based association studies of quantitative traits. Genet Epidemiol. 2007;31:358–62. doi: 10.1002/gepi.20217. doi: 10.1002/gepi.20217. [DOI] [PubMed] [Google Scholar]
- 25.Thakkinistan A, D'Este C, Eisman J, Nguyen T, Attia J. Meta-analysis of molecular association studies: vitamin D receptor gene polymorphisms and BMD as a case study. J Bone Miner Res. 2004;18:419–28. doi: 10.1359/JBMR.0301265. doi: 10.1359/JBMR.0301265. [DOI] [PubMed] [Google Scholar]
- 26.Ji GR, Yao M, Sun CY, Li ZH, Han Z. BsmI, TaqI, ApaI, and FokI polymorphisms in the vitamin D receptor (VDR) gene and risk of fracture in Caucasians: A meta-analysis. Bone. 2010;47:681–86. doi: 10.1016/j.bone.2010.06.024. doi: 10.1016/j.bone.2010.06.024. [DOI] [PubMed] [Google Scholar]
- 27.Bustamante M, Nogues X, Enjuanes A, Elosua R, Garcia-Giralt N, Perez-Edo L, et al. COLIA1, ESR1, VDR and TGFB1 polymorphisms and haplotypes in relation to BMD in Spanish postmenopausal women. Osteoporos Int. 2007;18:235–43. doi: 10.1007/s00198-006-0225-8. doi: 10.1007/s00198-006-0225-8. [DOI] [PubMed] [Google Scholar]
- 28.Perez A, Ulla M, Garcia B, Lavezzo M, Elias E, Binci M, et al. Genotypes and clinical aspects associated with bone mineral density in Argentine postmenopausal women. J Bone Miner Metab. 2008;26:358–65. doi: 10.1007/s00774-007-0840-2. doi: 10.1007/s00774-007-0840-2. [DOI] [PubMed] [Google Scholar]
- 29.Kiel DP, Myers RH, Cupples LA, Kong XF, Zhu XH, Ordovas J, et al. The BsmI vitamin D receptor restriction fragment length polymorphism (bb) influences the effect of calcium intake on bone mineral density. J Bone Miner Res. 1997;12:1049–57. doi: 10.1359/jbmr.1997.12.7.1049. doi: 10.1359/jbmr.1997.12.7.1049. [DOI] [PubMed] [Google Scholar]
- 30.Cifuentes M, Morano AB, Chowdhury HA, Shapses SA. Energy restriction reduces fractional calcium absorption in mature obese and lean rats. J Nutr. 2002;132:2660–6. doi: 10.1093/jn/132.9.2660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chang B, Sukumar D, Schlussel Y, Gordon D, Shapses SA. Vitamin D receptor polymorphisms predict greater decrease in calcium absorption. FASEB J. 2014;28:373. [Google Scholar]
- 32.Kiel DP, Demissie S, Dupuis J, Lunetta KL, Murabito JM, Karasik D. Genome-wide association with bone mass and geometry in the Framingham Heart Study. BMD Med Genet. 2007;19:S1–14. doi: 10.1186/1471-2350-8-S1-S14. doi: 10.1186/1471-2350-8-S1-S14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Richards JB, Rivadeneira F, Inouye M, Pastinen TM, Soranzo N, Wilson SG, et al. Bone mineral density, osteoporosis, and osteoporotic fractures: a genome-wide association study. Lancet. 2008;371:1505–12. doi: 10.1016/S0140-6736(08)60599-1. doi: 10.1016/S0140-6736(08)60599-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Estrada K, Styrkarsdottir U, Evangelou E, Hsu YH, Duncan EL, Ntzani EE, et al. Genome-wide meta-analysis identifies 56 bone mineral density loci and reveals 14 loci associated with risk of fracture. Nat Genet. 2012;44:491–501. doi: 10.1038/ng.2249. doi: 10.1038/ng.2249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Valdivielso JM, Fernandez E. Vitamin D receptor polymorphisms and disease. Clin Chim Act. 2006;371:1–12. doi: 10.1016/j.cca.2006.02.016. [DOI] [PubMed] [Google Scholar]
- 36.Barger-Lux MJ, Heaney RP, Hayes J, DeLuca HF, Johnson ML, Gong G. Vitamin D receptor gene polymorphism, bone mass, body size, and vitamin D receptor density. Calcif Tissue Int. 1995;57:161–62. doi: 10.1007/BF00298438. [DOI] [PubMed] [Google Scholar]
- 37.Uitterlinden AG, Fang Y, van Meurs JB, Pols H A, van Leeuwen JP. Genetics and biology of vitamin D receptor polymorphisms. Gene. 2004;338:143–56. doi: 10.1016/j.gene.2004.05.014. doi: 10.1016/j.gene.2004.05.014. [DOI] [PubMed] [Google Scholar]
- 38.Whitfield GK, Remus LS, Jurutka PW, Zitzer H, Oza AK, Dang HT, et al. Functionally relevant polymorphisms in the human nuclear vitamin D receptor gene. Mol Cell Endocrinol. 2001;177:145–59. doi: 10.1016/s0303-7207(01)00406-3. doi:10.1016/S0303-7207(01)00406-3. [DOI] [PubMed] [Google Scholar]
- 39.Walters JR, Barley NF, Khanji M, Rhodes-Kendler O. Duodenal expression of the epithelial calcium transporter gene TRPV6: is there evidence for Vitamin D-dependence in humans? J Steroid Biochem Mio Biol. 2004;89-90:317–9. doi: 10.1016/j.jsbmb.2004.03.028. doi:10.1016/j.jsbmb.2004.03.028. [DOI] [PubMed] [Google Scholar]
- 40.Al-Daghri NM, Guerini FR, Al-Attas OS, Alokail MS, Alkharfy KM, Draz HM, et al. Vitamin D receptor gene polymorphisms are associated with obesity and inflammosome activity. PLoS One. 2014;9:e102141. doi: 10.1371/journal.pone.0102141. doi: 10.1371/journal.pone.0102141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Waterhouse M, Tran B, Armstrong BK, Baxter C, Ebeling PR, English DR, et al. Environmental, personal, and genetic determinants of response to vitamin D supplementation in older adults. J Clin Endocrinol Metab. 99:E1332–40. doi: 10.1210/jc.2013-4101. http://dx.doi.org/10.1210/jc.2013-4101. [DOI] [PubMed] [Google Scholar]
- 42.Powe CE, Evans MK, Wenger J, Zonderman AB, Berg AH, Nalls M, et al. Vitamin D-binding protein and vitamin D status of black Americans and white Americans. N Engl J Med. 2013;369:1991–2000. doi: 10.1056/NEJMoa1306357. doi: 10.1056/NEJMoa1306357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wang TJ, Zhang F, Richards JB, Kestenbaum B, van Meurs JB, Berry D, et al. Common genetic determinants of vitamin D insufficiency: a genome wide association study. Lancet. 2010;376:180–88. doi: 10.1016/S0140-6736(10)60588-0. doi: 10.1016/S0140-6736(10)60588-0. [DOI] [PMC free article] [PubMed] [Google Scholar]