Abstract
Alzheimer’s disease (AD) is the most common age-related dementia. Pathognomonic accumulation of cerebral β-amyloid plaques likely results from imbalanced production and removal of amyloid-β (Aβ) peptides. In AD, innate immune cells lose their ability to restrict cerebral Aβ accumulation. At least in principle, mononuclear phagocytes can be enlisted to clear Aβ/β-amyloid from the brain. While the classical focus has been on dampening neuroinflammation in the context of AD, we hypothesize that rebalancing cerebral innate immunity by inhibiting actions of key anti-inflammatory cytokines returns the brain to a physiological state. Recent experiments demonstrating beneficial effects of blocking anti-inflammatory cytokine signaling in pre-clinical mouse models provide supportive evidence. This concept represents an important step toward innate immune targeted therapy to combat AD.
Keywords: amyloid, apolipoprotein E, immunotherapy, interleukin-10, microglia, phagocytosis
1. The central role of cerebral innate immunity in Alzheimer’s disease
Alzheimer’s disease (AD) currently affects more than 5 million Americans, and newly diagnosed cases are expected to reach 10–15 million in the U.S.A. by 2050 [1], highlighting the major impact of the disease on public health. AD is characterized by intracellular neurofibrillary tangles (comprised of misfolded tau protein), extracellular amyloid-β (Aβ) accumulation (consisting of β-pleated sheet conformers of insoluble Aβ peptides) and neuroinflammation, earmarked by reactive astrocytes and brain-resident monocytes (microglia) surrounding β-amyloid deposits [2]. While a number of preventative and therapeutic strategies are being pursued, an effective treatment for AD does not yet exist.
A widely-accepted theory of AD pathogenesis holds that imbalanced production versus clearance of Aβ peptides precipitates disease. In recent decades, the major therapeutic approach has been aimed at reducing cerebral Aβ production. Specifically, drugs have been designed to inhibit the β- and γ-secretases responsible for Aβ production from amyloid precursor protein (APP) endoproteolysis. However, the secretases cleave a variety of other substrates, and lack of specificity has been implicated in resultant adverse events [3,4]. An alternative strategy that is gaining momentum is targeting the other side of the equation: Aβ clearance. This concept is rooted in the notion that failure of the innate immune system to clear Aβ, rather than overproduction of the peptides, is likely the etiologic culprit in sporadic AD [5]. Indeed, extensive microglial recruitment to plaques in human AD is accompanied by very little, if any, Aβ phagocytosis [5,6], and occurs with increased production of pro-inflammatory cytokines that associate with cognitive decline [7]. A parsimonious conclusion from these findings is that innate immune cells (including both CNS-resident microglia and peripheral mononuclear phagocytes) lose their physiologic ability to restrict cerebral Aβ accumulation and switch into a pathological state [2,7–10]. It remains unclear at what stage and to what degree a switch from ‘good’ to ‘bad’ microglia occurs, and whether this is reversible.
The most common form of the disease, sporadic or late-onset AD (LOAD), has a complex etiology that includes genetic, environmental, and lifestyle risk factors. Recent genome-wide association studies (GWAS) have identified a cluster of AD risk alleles belonging to core innate immune pathways [3,4,11]. A common phenotype linking these risk alleles is modulation of phagocytosis [12–15]. Consequently, regulation of inflammation and the cerebral innate immune response have become major areas of interest, both in terms of understanding AD etiology and for developing new therapeutic approaches. However, inconsistent results reported for non-steroidal anti-inflammatory drugs (NSAIDs) and AD prevention [16–19] imply that a more ‘surgical’ approach targeting select immune pathways is needed. However, refining therapeutic targets has been difficult. This is because activated microglia express a multitude of inflammatory cytokine and chemokine receptors in the context of AD-like pathology [20–24], and myriad cytokines and chemokines have been detected in AD patient brains and CSF [25–27].
While pro-inflammatory mediators have garnered the most attention in this regard, the cardinal anti-inflammatory regulators transforming growth factor-beta 1 (TGF-β1) [28] and interleukin-10 (IL-10) [25] are also elevated in human AD, raising a possible pathogenic role for these cytokines. Further, a functional polymorphism within the IL10 gene has been linked to increased risk for LOAD in some [29–32], but not all populations [33–35]. While an initial report suggested that the IL10 AD risk allele was associated with reduced IL-10 expression in healthy control plasma [32], those authors did not relate IL10 polymorphism to IL-10 activity in AD patients. This is important, because CNS IL-10 abundance is increased in neurological diseases; including stroke, multiple sclerosis, meningitis, and AD [36]. Further, we and others have shown that the IL-10 signaling pathway is abnormally elevated in AD patient sera and brains [25,37]. The earlier conclusion that IL-10 down-regulation is a risk factor for AD is at odds with recent integrative genomic evidence showing increased IL-10 signaling in AD brains [38,39]. Clearly, further work is necessary to understand the IL10 allele-AD risk relationship.
Contrary to the notion that all forms of inflammation are deleterious in the context of AD, awareness is being raised to the concept that blocking immunosuppressive pathways can be beneficial. In this regard, we demonstrated that TGF-β-Smad 2/3 signaling inhibition in peripheral macrophages caused brain infiltration of these cells and restriction of cerebral β-amyloidosis. Genetic blockade of the TGF-β signaling pathway led to dramatically elevated central and peripheral IL-10 abundance [40–42], prompting investigation into the putative contribution of IL-10 signaling in the context of AD. Indeed, new studies show that inhibiting IL-10/STAT3 signaling dramatically mitigates Alzheimer-like pathology [37], while brain overexpression of Il10 produces complementary effects [43]. This has led us to theorize that ‘rebalancing’ activation of the innate immune system, as opposed to shutting it off completely, represents a novel AD therapeutic approach.
2. Interleukin-10 signaling suppresses cerebral β-amyloid clearance
IL-10 is a prototypical anti-inflammatory cytokine that is produced by and regulates activation of T cells, dendritic cells, peripheral macrophages, and CNS resident microglia [44,45]. Signaling is elicited by binding of IL-10 to its cognate receptor (IL-10R), which triggers phosphorylation of Janus kinase 1 (JAK1) that, in turn, phosphorylates signal transducer and activator of transcription 3 (STAT3). STAT3 homodimerizes and translocates to the nucleus, where it transactivates genes including suppressor of cytokine signaling 3 (SOCS3). SOCS3 is then phosphorylated by Src family kinases and interacts with receptors for inflammatory cytokines; targeting them for ubiquitin-mediated degradation. Activation of the IL-10 pathway referees essential functions of monocytes including phagocytosis, cytokine production, expression of costimulators, and antigen presentation. The modus operandi of this cytokine is to suppress overly exuberant inflammatory responses by blocking the action of pro-inflammatory cytokines [45,46].
In the central nervous system, IL-10 expression is increased in response to major neurological diseases including stroke, multiple sclerosis, meningitis, and AD [47]. Increased IL-10 abundance in AD patients’ sera and brains has been reported [25,48], and we recently showed that all canonical IL-10 pathway signaling elements (i.e., IL-10R1 and downstream JAK1, phospho-JAK1 (pJAK1), STAT3, phospho-STAT3 and SOCS3) are overly abundant in AD hippocampi compared to age-matched, non-demented controls [37]. These results led us to hypothesize that elevated IL-10 signaling in the AD brain blocks physiological innate immune recognition, phagocytosis, and clearance of cerebral β-amyloid.
To test this hypothesis, effects of IL-10 modulation were independently examined in three different mouse models (TgCRND8, Tg2576 and APP/PS1) exhibiting cortical and hippocampal Aβ plaques, gliosis, synaptic deficits, and associated cognitive impairment. Cerebral Il10 overexpression using adeno-associated virus in TgCRND8 and Tg2576 mice exacerbated Aβ plaque number and size [43], while deletion of Il10 reduced the severity of cerebral amyloid angiopathy and amyloidosis in APP/PS1 mice [37]. In neither experimental scenario did changes in IL-10 abundance affect APP metabolism or Aβ production; suggesting that IL-10-dependent alteration of cerebral amyloid deposition is owed to Aβ clearance [37,43]. Further support came from in vitro evidence showing that the IL-10/STAT3 pathway modulates microglial Aβ phagocytosis. Specifically, recombinant IL-10 treatment of primary microglial cultures promoted nuclear translocation of downstream STAT3 [37] and decreased phagocytosis of Aβ40 [43] and Aβ42 microaggregates [37]. However, IL-10 had no effect on Aβ40 or Aβ42 astrocytic uptake [43]. Importantly, genetic ablation of Il10 or Stat3 in microglial cultures increased Aβ42 uptake into phagolysosomes [37].
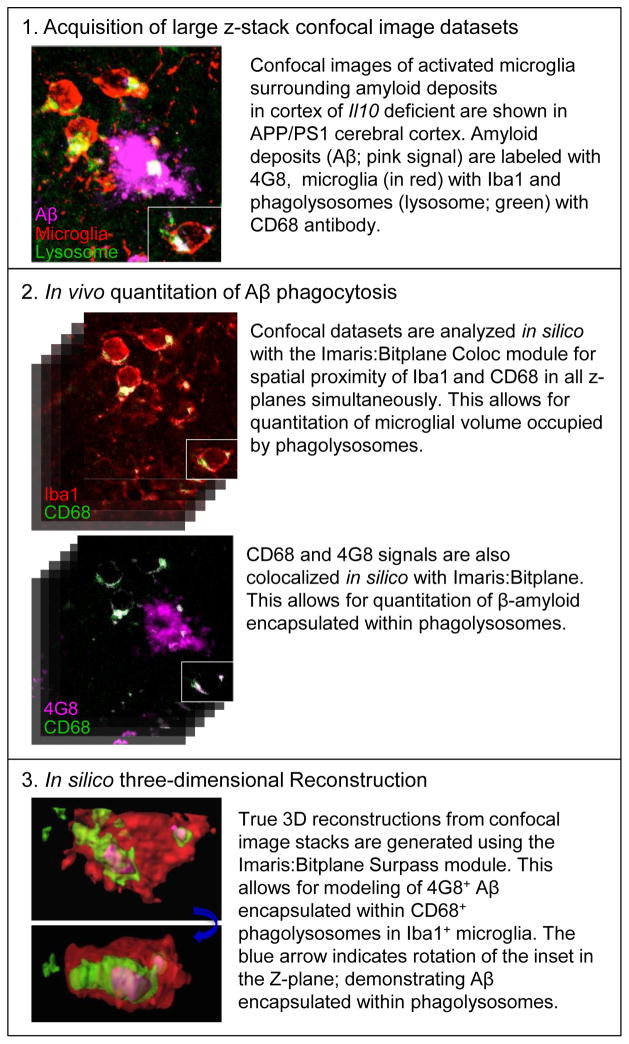
Essential validation of these observations came from in vivo experiments, where Il10 deficient APP/PS1 mice presented increased astrocytosis and reactive microglia [37]. Specifically, β-amyloid plaques, which appeared more diffuse than typical dense-cored plaques, were associated with greater numbers of monocytes compared with Il10 sufficient APP/PS1 mice [37]. Cell number was not the only monocyte phenotype that Il10 deficiency modified; intriguingly, mononuclear phagocytes infiltrating Aβ deposits expressed CD68 (a cell surface, phagolysosomal and endosomal marker) [49]. These striking results suggest that Il10 deficient monocytes are prone to penetrate β-amyloid plaques and to phagocytose Aβ deposits [37]. Finally, cutting-edge quantitative three-dimensional in silico modeling (q3DISM) allowed us to quantitate Aβ phagocytosis in vivo (Figure 1). Results from this line of investigation confirm that Il10 deficient monocytes are more efficient Aβ phagocytes versus Il10 sufficient cells. Altogether, these data suggest that 1) endogenous overproduction of IL-10 causes defective innate immune Aβ phagocytosis leading to plaque build-up, and 2) inhibition of the IL-10/STAT3 pathway returns the system to homeostasis; thereby enabling cerebral Aβ clearance.
Figure 1. Methodology for quantitative 3D in silico modeling (q3DISM) of Aβ phagocytosis.
This multi-stage q3DISM technique is depicted. This cutting-edge technology allows for true 3D quantitation of Aβ phagocytosis in vivo by mononuclear phagocytes.
3. Beneficial effects of blocking IL-10/STAT3 signaling in the context of Alzheimer’s disease
A key question is whether the effects of IL-10 modulation are restricted to cerebral amyloidosis or more broadly impact Alzheimer-like pathology. The first hint of this came from Il10 overexpression, which decreased synaptic protein abundance and worsened cognitive impairment [43]; whereas Il10 deletion led to stabilization of synaptic health and mitigated behavioral deficits [37]. These important findings indicate that the specific innate immune activation profile is of utmost importance for determining damaging vs. beneficial responses [10,41,50–52]. If left unchecked–or if overly repressed–cerebral innate immunity can perpetrate neuronal damage (directly or via Aβ); but if controlled, the system can be harnessed to clear the brain of damaging Aβ species without coming at the cost of bystander neuronal injury.
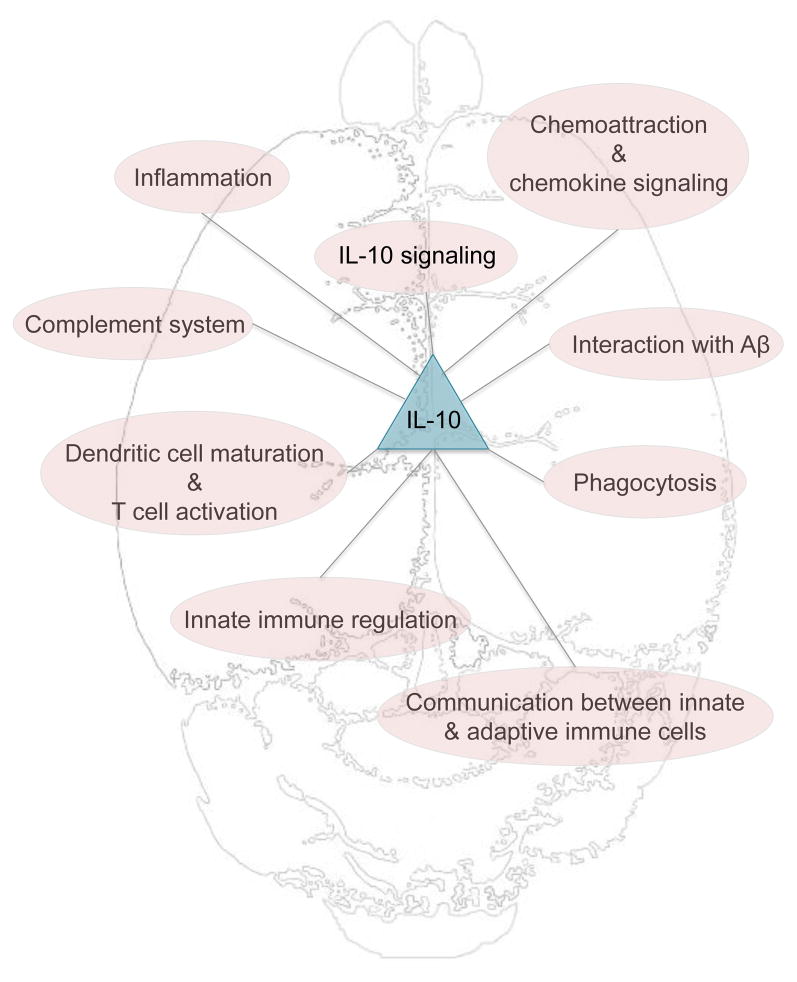
The notion that monocyte activation states are clearly divided between a pro-inflammatory M1 phenotype and a pro-phagocytic M2 phenotype has become obsolete [9,10,50]. Rather, microglia can assume a continuum of activation states characterized by expression of intersecting markers [10,53]. This concept was corroborated by analysis of Il10 dependent inflammatory genes via RNAseq [37] or NanoString [43]. In transgenic mouse models of cerebral amyloidosis, genes that were altered by Il10 overexpression or Il10 deficiency were further interrogated for immune-related function(s) [37,43]. Gene pathways were largely overlapping between these two opposing manipulations, and were responsible for: phagocytosis, chemoattraction/chemokine signaling, innate immune regulation (e.g., toll-like receptor signaling), inflammation and the acute phase response (e.g., LXR/RXR pathway), Aβ interaction, dendritic cell maturation and T cell activation, the protein complement system, communication between innate and adaptive immune cells, and IL-10 signaling itself (Figure 2). In both reports, mononuclear phagocyte activation state was neither absolutely M1 nor M2; rather, unique activation phenotypes fell within the continuum between M1 and M2 extremes [10,37,43]. Importantly, Il10 deficient APP/PS1 animals exhibited polarization of microglial activation away from a traditional M2 state but had increased phagocytic capacity, confirming–yet again–how the M1/M2 dichotomy is not a useful classification system [10,37,50,52].
Figure 2. Il10 dependent neuroinflammatory gene profiles in mouse models of cerebral amyloidosis.
The diagram shows the broad categories of major gene groups affected by experimental targeting of Il10 (overexpression or genetic ablation) according to transcriptomics published in [32–33].
4. Intersection between IL-10 and apolipoprotein E pathways
Of the differentially expressed genes identified by large-scale expression profiling in Il10 targeted cerebral amyloidosis mouse models, one hit stood out: apolipoprotein E (Apoe) [37,43]. This is because the ε4 allele of APOE is the strongest genetic susceptibility factor for human AD. Strikingly, Il10 overexpression increases cerebral Apoe mRNA abundance [43], while Il10 deficiency reduces Apoe expression [37] in mouse models. These findings are particularly interesting, because human ApoE isoform-specifically regulates Aβ metabolism, aggregation, deposition and clearance [54,55], and cerebral vasotonus [56]. Knocking in human APOE4 into mouse models of cerebral amyloidosis exacerbates microglial inflammation and Aβ deposition [57], while APOE2 promotes clearance of preexisting deposits [58].
Remarkably, cerebral Il10 overexpression increases murine APOE association with insoluble amyloid and promotes direct ApoE- Aβ interaction that inhibits phagocytosis of the complex [43]. Additionally, treatment of microglial cultures with Aβ bound to human ApoE isoforms reveals isoform-specific reduction of Aβ phagocytosis (E4 > E3 > E2) [37]. These results are particularly significant in light of previous studies showing ApoE isoform-dependent enhanced Aβ oligomerization and fibril stabilization [59–62], and Aβ clearance by glial cells can be negatively affected by ApoE-Aβ association [63]. Strikingly, this result mirrors the well-established relative risk of ApoE for human AD (E4 > E3 > E2) [64]. Importantly, Il10 deficiency rescues impaired Aβ phagocytosis by ApoE3 [37]. Altogether, these results provide the basis for mechanistic intersection between IL-10 signaling and the greatest genetic risk factor for LOAD: APOE.
5. Conclusions
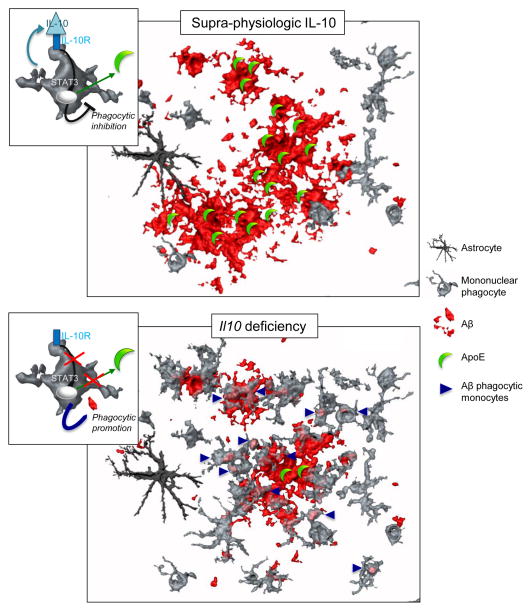
In this Opinion, we have illustrated the complex interplay between anti-inflammatory factors and AD pathoetiology. Specifically, evidence is presented that innate immunity is pathologically repressed by anti-inflammatory factors in the AD brain; obviating β-amyloid plaque phagocytosis and clearance. Specifically, elevated IL-10 signaling in the context of cerebral amyloidosis promotes a pathological form of cerebral innate immunity that licenses ApoE-Aβ binding and reduces Aβ clearance by mononuclear phagocytes. Therefore, IL-10 acts via dual mechanisms to promote cerebral amyloidosis–on the one hand, by retarding Aβ phagocytosis, and on the other, by promoting ApoE-Aβ co-deposition (Figure 3).
Figure 3. Proposed model for the impact of IL-10 on Aβ clearance by mononuclear phagocytes.
The top panel depicts effects of supra-physiologic IL-10; present in AD brains and in mouse models of cerebral amyloidosis. IL-10/STAT3 pathway activation reduces monocyte Aβ phagocytosis. Concomitantly, ApoE expression is increased and clusters in Aβ deposits, retarding Aβ clearance. The lower panel illustrates effects of Il10 ablation in mouse models of cerebral amyloidosis. Microglial phagocytic capacity is enhanced and ApoE expression, reduced, enabling Aβ clearance by mononuclear phagocytes.
Modulating IL-10/STAT3 signaling has proven effective in other therapeutic settings [65,66], and rebalancing cerebral innate immunity to promote beneficial neuroinflammation may be more efficacious than anti-inflammatory therapy for AD. However, several key issues need to be explored before moving forward and enlisting the innate immune system to clear Aβ as a therapeutic modality (see Outstanding Questions). First and foremost, whether activated monocytes in AD patients’ brains arise from infiltrating peripheral macrophages or expansion of resident microglia remains unknown. As discussed above, in late stages of AD (i.e., after amyloidosis is established) microglia are inefficient Aβ phagocytes [5,7]. However, several studies have shown that peripheral macrophages infiltrating the brain in mouse models of cerebral amyloidosis home to amyloid plaques and effectively clear Aβ [40,67,68]. To therapeutically target innate immunity in AD, it is therefore crucial to delineate the relative contribution(s) of central vs. peripheral mononuclear cells. Pan-inhibition of IL-10 signaling would not be judicious, because IL-10 is critically important to militate against peripheral inflammatory diseases (e.g., rheumathoid arthritis, psoriasis, and Crohn’s disease). Yet, it deserves mentioning that IL-10-based therapeutics have already proven effective in aging populations [69]. The observation that IL-10 can modulate ApoE-Aβ interaction is original, and has major implications for therapeutic strategies. A deeper understanding of the intersecting points between IL-10 and ApoE in the context of AD is needed. It is important to note that genetic blockade of both major anti-inflammatory pathways: TGF-β-Smad 2/3 [40] and IL-10/STAT3 [37], results in an innate immune shift towards cerebral amyloid clearance. This exciting new research focus on blocking anti-inflammatory pathways is eventually expected to lead to safe and effective AD treatment.
Outstanding Questions.
Do activated monocytes in AD patients’ brains arise from infiltrating peripheral macrophages or expansion of resident microglia? Is it possible to specifically target peripheral monocytes or CNS microglia in LOAD?
Are hematogenous monocytes more efficient Aβ phagocytes than brain-resident microglia? If so, what is the molecular mechanism for this important difference?
What is the mechanism underlying increased LOAD risk incurred by the polymorphic IL10 allele? Does the IL10 polymorphism affect IL-10 signaling independently of its action on reducing IL-10 expression?
Does IL-10 retard monocyte clearance of Aβ/β-amyloid, and therefore contribute to amyloid deposition in AD? What inflammatory genes does IL-10 signaling directly alter to influence monocyte Aβ phagocytosis and clearance?
Can we determine more specific therapeutic targets that are downstream of the IL-10 pathway? At what stage would blocking IL-10 signaling be most effective against LOAD?
How does IL-10 modulate ApoE-Aβ interaction, and does association of ApoE with lipids influence formation of this complex? Do lipids impact ApoE isoform-specific alteration of Aβ phagocytosis?
Does Il10 deletion mitigate Alzheimer-like pathology in Apoe-deficient mice, or in chimeric mice expressing human ApoE2, ApoE3, or ApoE4? Answering this important question could pave the way to understand the specific role(s) of ApoE isoforms in Il10 deficient mouse models of cerebral amyloidosis, and in the human disease.
Trends Box.
Recent GWAS have identified a cluster of AD risk alleles belonging to core innate immune pathways that modulate phagocytosis.
Functional polymorphism within the Il10 gene has been linked to increased risk for LOAD in certain populations, and IL-10 signaling is abnormally elevated in AD patient sera and brains.
Inhibiting IL-10/STAT3 signaling dramatically mitigates Alzheimer-like pathology, while brain overexpression of Il10 aggravates Aβ deposition in mouse models of cerebral amyloidosis.
Elevated IL-10 signaling reduces Aβ clearance by mononuclear phagocytes and licenses ApoE-Aβ binding.
IL-10/STAT3 pathway blockade enhances microglial Aβ phagocytic activity and decreases ApoE expression, thereby mitigating ApoE-Aβ binding that retards Aβ phagocytosis.
Blocking anti-inflammatory mediators represents a promising future treatment approach for AD.
Acknowledgments
We thank Alex Vesling and Drs. Tara Weitz and David Gate (USC Zilkha Neurgenetic Institute, Los Angeles, CA, USA) for helpful discussion. M-V.G-S is supported by a BrightFocus Foundation Alzheimer’s Disease Research Fellowship Award (A2015309F) and an Alzheimer’s Association, California Southland Chapter Young Investigator Award. This work was supported by the National Institute on Neurologic Disorders and Stroke (1R01NS076794-01, to T.T.), an Alzheimer’s Association Zenith Fellows Award (ZEN-10-174633, to T.T.), and an American Federation of Aging Research/Ellison Medical Foundation Julie Martin Mid-Career Award in Aging Research (M11472, to T.T.). We are grateful for startup funds from the Zilkha Neurogenetic Institute, which helped to make this work possible.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Brookmeyer R, et al. National estimates of the prevalence of Alzheimer’s disease in the United States. Alzheimers Dement. 2011;7:61–73. doi: 10.1016/j.jalz.2010.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Heneka MT, et al. Innate immunity in Alzheimer’s disease. Nature Immunol. 2015;16:229–236. doi: 10.1038/ni.3102. [DOI] [PubMed] [Google Scholar]
- 3.Yan R, Vassar R. Targeting the β secretase BACE1 for Alzheimer’s disease therapy. Lancet Neurol. 2014;13:319–329. doi: 10.1016/S1474-4422(13)70276-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Golde TE, et al. γ-Secretase inhibitors and modulators. Biochim Biophys Acta. 2013;1828:2898–2907. doi: 10.1016/j.bbamem.2013.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mawuenyega KG, et al. Decreased clearance of CNS beta-amyloid in Alzheimer’s disease. Science. 2010;330:1774. doi: 10.1126/science.1197623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hickman SE, et al. Microglial dysfunction and defective beta-amyloid clearance pathways in aging Alzheimer’s disease mice. J Neurosci. 2008;28:8354–8360. doi: 10.1523/JNEUROSCI.0616-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Johnston H, et al. Assessing the contribution of inflammation in models of Alzheimer’s disease. Biochem Soc Trans. 2011;39:886–890. doi: 10.1042/BST0390886. [DOI] [PubMed] [Google Scholar]
- 8.Orre M, et al. Isolation of glia from Alzheimer’s mice reveals inflammation and dysfunction. Neurobiol. 2014;35:2746–2760. doi: 10.1016/j.neurobiolaging.2014.06.004. [DOI] [PubMed] [Google Scholar]
- 9.Heneka MT, et al. Neuroinflammation in Alzheimer’s disease. Lancet Neurol. 2015;14:388–405. doi: 10.1016/S1474-4422(15)70016-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Town T, et al. The microglial “activation” continuum: from innate to adaptive responses. J Neuroinflammation. 2005;2:24. doi: 10.1186/1742-2094-2-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gjoneska E, et al. Conserved epigenomic signals in mice and humans reveal immune basis of Alzheimer’s disease. Nature. 2015;518:365–369. doi: 10.1038/nature14252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Reitz C, Mayeux R. Alzheimer disease: epidemiology, diagnostic criteria, risk factors and biomarkers. Biochem Pharmacol. 2014;88:640–651. doi: 10.1016/j.bcp.2013.12.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hazrati LN, et al. Genetic association of CR1 with Alzheimer’s disease: a tentative disease mechanism. Neurobiol Aging. 2012;33:2949.e5–2949.e12. doi: 10.1016/j.neurobiolaging.2012.07.001. [DOI] [PubMed] [Google Scholar]
- 14.Griciuc A, et al. Alzheimer’s Disease Risk Gene CD33 Inhibits Microglial Uptake of Amyloid Beta. Neuron. 2013;78:631–43. doi: 10.1016/j.neuron.2013.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hardy J, et al. Pathways to Alzheimer’s disease. J Intern Med. 2014;275:296–303. doi: 10.1111/joim.12192. [DOI] [PubMed] [Google Scholar]
- 16.Jaturapatporn D, et al. Aspirin, steroidal and non-steroidal anti-inflammatory drugs for the treatment of Alzheimer’s disease. Cochrane Database Syst Rev. 2012;2:CD006378. doi: 10.1002/14651858.CD006378.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Szekely CA, Zandi PP. Non-steroidal anti-inflammatory drugs and Alzheimer’s disease: the epidemiological evidence. CNS Neurol Disord Drug Targets. 2010;9:132–139. doi: 10.2174/187152710791012026. [DOI] [PubMed] [Google Scholar]
- 18.Breitner JC, et al. Extended results of the Alzheimer’s disease anti-inflammatory prevention trial. Alzheimers Dement. 2011;7:402–411. doi: 10.1016/j.jalz.2010.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Leoutsakos JMS, et al. Effects of non-steroidal anti-inflammatory drug treatments on cognitive decline vary by phase of pre-clinical Alzheimer disease: findings from the randomized controlled Alzheimer’s Disease Anti-inflammatory Prevention Trial. Int J Geriatr Psychiatry. 2012;27:364–374. doi: 10.1002/gps.2723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Heneka MT, et al. NLRP3 is activated in Alzheimer’s disease and contributes to pathology in APP/PS1 mice. Nature. 2013;493:674–678. doi: 10.1038/nature11729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fuhrmann M, et al. Microglial Cx3cr1 knockout prevents neuron loss in a mouse model of Alzheimer’s disease. Nat Neurosci. 2010;13:411–413. doi: 10.1038/nn.2511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Berg vom J, et al. Inhibition of IL12/IL23 signaling reduces Alzheimer’s disease–like pathology and cognitive decline. Nat Med. 2012;18:1812–1819. doi: 10.1038/nm.2965. [DOI] [PubMed] [Google Scholar]
- 23.Lee S, et al. CX3CR1 deficiency alters microglial activation and reduces beta-amyloid deposition in two Alzheimer’s disease mouse models. Am J Pathol. 2010;177:2549–2562. doi: 10.2353/ajpath.2010.100265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lee S, et al. Opposing effects of membrane-anchored CX3CL1 on amyloid and tau pathologies via the p38 MAPK pathway. J Neurosci. 2014;34:12538–12546. doi: 10.1523/JNEUROSCI.0853-14.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gezen-Ak D, et al. BDNF, TNFα, HSP90, CFH, and IL-10 serum levels in patients with early or late onset Alzheimer’s disease or mild cognitive impairment. J Alzheimers Dis. 2013;37:185–195. doi: 10.3233/JAD-130497. [DOI] [PubMed] [Google Scholar]
- 26.Akiyama H, et al. Inflammation and Alzheimer’s disease. Neurobiol Aging. 2000;21:383–421. doi: 10.1016/s0197-4580(00)00124-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Weeraratna AT, et al. Alterations in immunological and neurological gene expression patterns in Alzheimer’s disease tissues. Exp Cell Res. 2007;313:450–461. doi: 10.1016/j.yexcr.2006.10.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wyss-Coray T, et al. Amyloidogenic role of cytokine TGF-beta1 in transgenic mice and in Alzheimer’s disease. Nature. 1997;389:603–606. doi: 10.1038/39321. [DOI] [PubMed] [Google Scholar]
- 29.Vural P, et al. The combinations of TNFalpha-308 and IL-6 -174 or IL-10 -1082 genes polymorphisms suggest an association with susceptibility to sporadic late-onset Alzheimer’s disease. Acta Neurol Scand. 2009;120:396–401. doi: 10.1111/j.1600-0404.2009.01230.x. [DOI] [PubMed] [Google Scholar]
- 30.Arosio B, et al. Interleukin-10 and interleukin-6 gene polymorphisms as risk factors for Alzheimer’s disease. Neurobiol Aging. 2004;25:1009–1015. doi: 10.1016/j.neurobiolaging.2003.10.009. [DOI] [PubMed] [Google Scholar]
- 31.Lio D, et al. Interleukin-10 promoter polymorphism in sporadic Alzheimer’s disease. Genes Immun. 2003;4:234–238. doi: 10.1038/sj.gene.6363964. [DOI] [PubMed] [Google Scholar]
- 32.Ma SL, et al. The association between promoter polymorphism of the interleukin-10 gene and Alzheimer’s disease. Neurobiol Aging. 2005;26:1005–1010. doi: 10.1016/j.neurobiolaging.2004.08.010. [DOI] [PubMed] [Google Scholar]
- 33.Depboylu C, et al. Lack of association of interleukin-10 promoter region polymorphisms with Alzheimer’s disease. Neurosci Lett. 2003;342:132–134. doi: 10.1016/s0304-3940(03)00231-3. [DOI] [PubMed] [Google Scholar]
- 34.Ramos EM, et al. Tumor necrosis factor alpha and interleukin 10 promoter region polymorphisms and risk of late-onset Alzheimer disease. Arch Neurol. 2006;63:1165–1169. doi: 10.1001/archneur.63.8.1165. [DOI] [PubMed] [Google Scholar]
- 35.Scassellati C, et al. Promoter haplotypes of interleukin-10 gene and sporadic Alzheimer’s disease. Neurosci Lett. 2004;356:119–122. doi: 10.1016/j.neulet.2003.11.033. [DOI] [PubMed] [Google Scholar]
- 36.Strle K, et al. Interleukin-10 in the brain. Crit Rev Immunol. 2001;21:427–449. [PubMed] [Google Scholar]
- 37.Guillot-Sestier MV, et al. Il10 deficiency rebalances innate immunity to mitigate Alzheimer-like pathology. Neuron. 2015;85:534–548. doi: 10.1016/j.neuron.2014.12.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhang B, et al. Integrated systems approach identifies genetic nodes and networks in late-onset Alzheimer’s disease. Cell. 2013;153:707–720. doi: 10.1016/j.cell.2013.03.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Li X, et al. Integrated genomic approaches identify major pathways and upstream regulators in late onset Alzheimer’s disease. Sci Rep. 2015;5:12393. doi: 10.1038/srep12393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Town T, et al. Blocking TGF-beta-Smad2/3 innate immune signaling mitigates Alzheimer-like pathology. Nat Med. 2008;14:681–687. doi: 10.1038/nm1781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gate D, et al. Macrophages in Alzheimer’s disease: the blood-borne identity. J Neural Transm. 2010;117:961–970. doi: 10.1007/s00702-010-0422-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rezai-Zadeh K, et al. How to get from here to there: macrophage recruitment in Alzheimer’s disease. Curr Alzheimer Res. 2011;8:156–163. doi: 10.2174/156720511795256017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chakrabarty P, et al. IL-10 alters immunoproteostasis in APP mice, increasing plaque burden and worsening cognitive behavior. Neuron. 2015;85:519–533. doi: 10.1016/j.neuron.2014.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Williams LM, et al. Interleukin-10 suppression of myeloid cell activation--a continuing puzzle. Immunology. 2004;113:281–292. doi: 10.1111/j.1365-2567.2004.01988.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Murray PJ. Understanding and exploiting the endogenous interleukin-10/STAT3-mediated anti-inflammatory response. Curr Opin Pharmacol. 2006;6:379–386. doi: 10.1016/j.coph.2006.01.010. [DOI] [PubMed] [Google Scholar]
- 46.Banchereau J, et al. From IL-2 to IL-37: the expanding spectrum of anti-inflammatory cytokines. Nat Immunol. 2012;13:925–931. doi: 10.1038/ni.2406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Doty KR, et al. The role of the immune system in neurodegenerative disorders: Adaptive or maladaptive? Brain research. 2014 doi: 10.1016/j.brainres.2014.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Loewenbrueck KF, et al. Th1 responses to beta-amyloid in young humans convert to regulatory IL-10 responses in Down syndrome and Alzheimer’s disease. Neurobiol Aging. 2010;31:1732–1742. doi: 10.1016/j.neurobiolaging.2008.09.007. [DOI] [PubMed] [Google Scholar]
- 49.Holness CL, Simmons DL. Molecular cloning of CD68, a human macrophage marker related to lysosomal glycoproteins. Blood. 1993;81:1607–1613. [PubMed] [Google Scholar]
- 50.Guillot-Sestier MV, Town T. Innate immunity in Alzheimer’s disease: a complex affair. CNS Neurol Disord Drug Targets. 2013;12:593–607. doi: 10.2174/1871527311312050008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rezai-Zadeh K, et al. CNS infiltration of peripheral immune cells: D-Day for neurodegenerative disease? J Neuroimmune Pharmacol. 2009;4:462–475. doi: 10.1007/s11481-009-9166-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Weitz TM, Town T. Microglia in Alzheimer’s Disease: It’s All About Context. Int J Alzheimers Dis. 2012;2012:314185. doi: 10.1155/2012/314185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lee DC, et al. Review: experimental manipulations of microglia in mouse models of Alzheimer’s pathology: activation reduces amyloid but hastens tau pathology. Neuropathol Appl Neurobiol. 2013;39:69–85. doi: 10.1111/nan.12002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kanekiyo T, et al. ApoE and Aβ in Alzheimer’s disease: accidental encounters or partners? Neuron. 2014;81:740–754. doi: 10.1016/j.neuron.2014.01.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Tai LM, et al. Levels of soluble apolipoprotein E/amyloid-β (Aβ) complex are reduced and oligomeric Aβ increased with APOE4 and Alzheimer disease in a transgenic mouse model and human samples. J Biol Chem. 2013;288:5914–5926. doi: 10.1074/jbc.M112.442103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Paris D, et al. Isoform-specific vasoconstriction induced by apolipoprotein E and modulation of this effect by Alzheimer’s beta-amyloid peptide. Neurosci Lett. 1998;256:73–76. doi: 10.1016/s0304-3940(98)00764-2. [DOI] [PubMed] [Google Scholar]
- 57.Rodriguez GA, et al. Human APOE4 increases microglia reactivity at Aβ plaques in a mouse model of Aβ deposition. J Neuroinflammation. 2014;11:111. doi: 10.1186/1742-2094-11-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hudry E, et al. Gene transfer of human Apoe isoforms results in differential modulation of amyloid deposition and neurotoxicity in mouse brain. Sci Transl Med. 2013;5:212ra161. doi: 10.1126/scitranslmed.3007000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hashimoto T, et al. Apolipoprotein E, especially apolipoprotein E4, increases the oligomerization of amyloid β peptide. J Neurosci. 2012;32:15181–15192. doi: 10.1523/JNEUROSCI.1542-12.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Garai K, et al. The binding of apolipoprotein E to oligomers and fibrils of amyloid-β alters the kinetics of amyloid aggregation. Biochemistry. 2014;53:6323–6331. doi: 10.1021/bi5008172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Cerf E, et al. High ability of apolipoprotein E4 to stabilize amyloid-β peptide oligomers, the pathological entities responsible for Alzheimer’s disease. FASEB J. 2011;25:1585–1595. doi: 10.1096/fj.10-175976. [DOI] [PubMed] [Google Scholar]
- 62.Pankiewicz JE, et al. Blocking the apoE/Aβ interaction ameliorates Aβ-related pathology in APOE ε2 and ε4 targeted replacement Alzheimer model mice. Acta Neuropathol Commun. 2014;2:75. doi: 10.1186/s40478-014-0075-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Mulder SD, et al. Apolipoproteins E and J interfere with amyloid-beta uptake by primary human astrocytes and microglia in vitro. Glia. 2014;62:493–503. doi: 10.1002/glia.22619. [DOI] [PubMed] [Google Scholar]
- 64.Yu JT, et al. Apolipoprotein E in Alzheimer’s disease: an update. Annu Rev Neurosci. 2014;37:79–100. doi: 10.1146/annurev-neuro-071013-014300. [DOI] [PubMed] [Google Scholar]
- 65.Ni G, et al. Manipulating IL-10 signalling blockade for better immunotherapy. Cell Immunol. 2015;293:126–129. doi: 10.1016/j.cellimm.2014.12.012. [DOI] [PubMed] [Google Scholar]
- 66.Munoz J, et al. STAT3 inhibitors: finding a home in lymphoma and leukemia. Oncologist. 2014;19:536–544. doi: 10.1634/theoncologist.2013-0407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Simard AR, et al. Bone marrow-derived microglia play a critical role in restricting senile plaque formation in Alzheimer’s disease. Neuron. 2006;49:489–502. doi: 10.1016/j.neuron.2006.01.022. [DOI] [PubMed] [Google Scholar]
- 68.Simard AR, Rivest S. Neuroprotective properties of the innate immune system and bone marrow stem cells in Alzheimer’s disease. Mol Psychiatry. 2006;11:327–335. doi: 10.1038/sj.mp.4001809. [DOI] [PubMed] [Google Scholar]
- 69.Kwilasz AJ, et al. The therapeutic potential of interleukin-10 in neuroimmune diseases. Neuropharmacology. 2014 doi: 10.1016/j.neuropharm.2014.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]