Abstract
Necrotizing enterocolitis (NEC) is the most common gastrointestinal emergency and remains a major cause of mortality for very-low-birth-weight infants (VLBWI) requiring surgery. To date, there have been no large-scale studies evaluating the incidence, associated clinical factors and outcomes of NEC for VLBWI in Korea. The 2,326 VLBWI of a total 2,386 Korean Neonatal Network (KNN) cohort born with a birth weight below 1,500 g between January 2013 to June 2014 were included in this analysis. The overall incidence of NEC (stage ≥ 2) among VLBWI in Korea was 6.8%; 149 infants had NEC stage ≥ 2 and 2,177 infants did not have NEC. Surgery was performed for 77 (53%) of the infants in the NEC group. NEC was related to lower gestational age (GA) and birth weight (P < 0.001). Multivariate logistic regression analysis demonstrated that NEC was consistently related to hypotension within one week after birth (OR 2.0, 95% CI 1.0-3.9). With respect to outcome, the NEC group had longer times to reach 100 mL/kg/day feeding (P < 0.001), longer TPN duration (P < 0.001) and hospitalization (P = 0.031) and higher PVL (P < 0.001) and mortality rate (P < 0.001). When the medical and surgical NEC groups were compared, GA was significantly lower and PDA was more found in the surgical NEC group. The overall incidence of NEC in Korea is similar to that of other multicenter studies. In addition to GA and birth weight, hypotension within a week of life is significantly related to NEC.
Keywords: Enterocolitis, Necrotizing; Incidence; Outcome; Very-low-birth-weight Infants
INTRODUCTION
Necrotizing enterocolitis (NEC) is the most common gastrointestinal emergency and remains a major cause for the mortality of very-low-birth-weight infants (VLBWI) requiring surgery. The pathogenesis of this disease remains elusive and controversial because the etiology of NEC is multifactorial and complex (1,2,3). Thus far, an inverse relationship between gestational age (GA) and the age of NEC onset has been well documented (4). Yet, NEC has also been related to vascular- or perfusion-related gastrointestinal compromises and inflammation (5,6,7). While many multi-center studies have reported national incidence of NEC and tried to identify individual risk factors related to the development of NEC, there has been no large-scale studies determined the association between multiple clinical factors and NEC in Korea. The Korean Neonatal Network (KNN) database was established in 2013 with the goal of promoting newborn health by improving data collection systems in participating facilities and studying various factors associated with the mortality and morbidity of VLBWI in Korea. A better understanding of clinical factors associated with NEC in a national cohort including all VLBWI in Korea will lead to better approaches and care for VLBWI in Korea, and further studies will be more precisely directed.
In this study, we aimed to observe the general distribution of NEC for VLBWI based on GA and birth weight and determine associated clinical factors involved with NEC in Korea. The secondary aim was to examine the relationship between multiple clinical factors and NEC and outcomes for NEC neonates compared to no NEC group. Thirdly, the differences between medical and surgical NEC were evaluated among NEC group in Korea.
MATERIALS AND METHODS
The data was collected for 2,386 VLBWI born between Jan 2013 and June 2014 from 55 NICUs using a standardized form defined as KNN electronic case report form (e-CRF). The inclusion criterion for this study was all VLBWI born in or transferred to participating neonatal centers within 28 days of birth. The progression of the infants was followed until death or discharge. Among these, 52 patients were simultaneously diagnosed of NEC ≥ 2 and spontaneous intestinal perforation (SIP), therefore, they were excluded from this analysis. The other 8 patients didn't have information on NEC and considered as missing data. As a result, a total of 2,326 infants weighing less than 1,500 g birth weight were included in this study. Also, of 149 NEC infants, 15 patients were unknown on their NEC management, thus, they were disregarded in the medical vs. surgical comparison. Data were collected by local staff using uniform definitions in the KNN.
Definitions
NEC is defined according to a modified Bell' staging classification grade ≥II including one or more of the following clinical signs: bilious, gastric aspirator emesis, abdominal distention, or occult or gross blood in stool. In addition, this classification includes one or more of the following radiographic findings: pneumatosis intestinalis, hepatobiliary gas, or pneumoperitoneum. The initial pH was defined measured using an arterial or venous sample taken within 1 hr of birth. Hypotension was determined when the blood pressure was consistently low and required inotropic agent use within 7 days of birth. Respiratory distress syndrome (RDS) was diagnosed from both clinical and radiographic findings. Bronchopulmonary dysplasia (BPD) was defined as the use of oxygen ≥0.21 at 36 weeks corrected gestational age or >28 days postnatal age. Pulmonary hypertension was defined when nitric oxide or sildenafil or iloprost was used within 1 week of birth. In this study, PDA was defined when pharmacological or surgical treatment was intervened. Intraventricular hemorrhages (IVH) were defined using Papile's grading system. Early-onset sepsis was defined as a positive blood culture performed ≤7 days after birth in the presence of clinical signs of infection. The other hospital outcomes were defined as per standardized data collection for KNN.
Statistical analysis
Before beginning our analysis, the available literature was reviewed to identify factors thought to be important for the development of NEC. Continuous variables were presented as means (±standard deviation, SD) and compared using the t-test or Wilcoxon rank sum test. Categorical variables were presented as percentages and frequencies and compared using the chi-square or Fisher's exact test.
Because GA and birth weight are independently strong factors, many of the possible factors potentially associated with increased risk for NEC in our univariate analysis were no longer significant. Therefore, 1:1 matching of GA and birth weight was performed. After 1:1 matching, we assessed baseline covariates between groups using the paired t-test or the Wilcoxon signed rank test for continuous variables and McNemar's test or the marginal homogeneity test for categorical variables. Multiple conditional logistic regression was used to identify factors independently associated with NEC. Statistical significance for unadjusted comparisons was determined using Fisher's exact test. All data were analyzed using SAS statistical software (SAS system for Windows, version 9.2; SAS institute, Cary, NC) and P values less than 0.05 were considered significant.
Ethics statement
The KNN registry was approved by the institutional review board at each participating hospital and informed consent was obtained from the parents at enrollment in NICUs participating in the KNN.
RESULTS
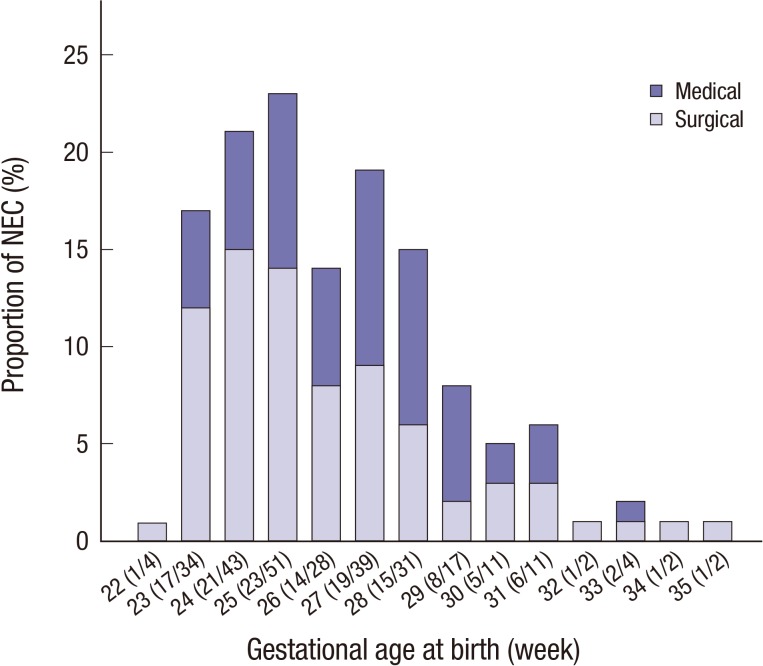
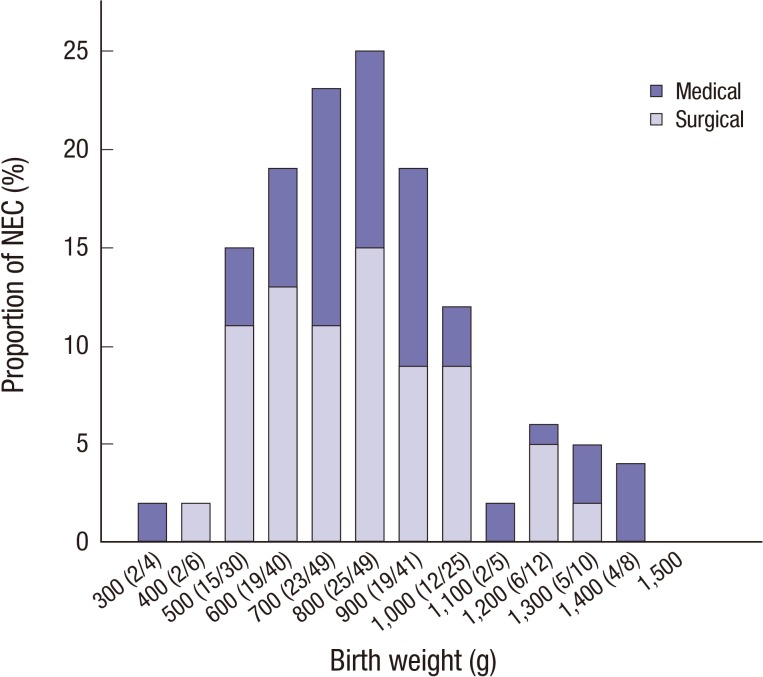
A total of 2,326 VLBWI were finally included and analyzed in the present study. Among them, 2,177 did not have NEC, while 149 (6.8%) met the criterion for NEC. Of the 149 infants in the NEC group, 77 (52%) had surgical management and 57 (38%) infants had medical management for NEC. As many studies have shown, NEC was significantly related to lower gestational age and birth weight (P<0.001). Fig. 1 and 2 demonstrate the distribution of NEC cases according to GA and birth weight. Fig. 1 shows a trend toward a decreasing incidence of NEC as the GA increases. The peak onset of NEC was 25 weeks of GA. The surgical management incidence was more prominently shown in lower GA groups, particularly those less than 28 weeks for neonates (Fig. 1). This inverse relationship between NEC and birth weight is also shown in Fig. 2.
Fig. 1. NEC incidence according to gestational age (week).
Fig. 2. NEC incidence according to birth weight (g).
NEC vs. no NEC group in a total population
The baseline characteristics and clinical outcomes of VLBWI with and without NEC are shown in Table 1. Compared with VLBWI without NEC, those with NEC are more likely to have resuscitation at delivery, hypotension, RDS, pneumothorax, massive pulmonary hemorrhage, pulmonary hypertension, IVH >grade II, sepsis and PDA (Table 1). With regards to clinical outcome, the NEC group had longer times to reach 100 mL/kg/day feeding (P<0.001), longer TPN duration (P<0.001) and hospitalization (P=0.031) and higher PVL (P<0.001) and mortality rate (P<0.001) (Table 2). A total of 63 (42.3%) patients in the NEC group died from different causes during hospitalization (Table 2). Meanwhile, a total of 38 (26.2%) patients from the NEC group died directly caused by NEC.
Table 1. Clinical characteristics of VLBWIs (n = 2,326); NEC vs. no NEC group.
| Characteristics | NEC (n = 149) | No NEC (n = 2,177) | P value |
|---|---|---|---|
| Gestational age (week) | 26.6 ± 2.7 | 29.1 ± 3.0 | < 0.001 |
| Birth weight (g) | 833 ± 245 | 1,095 ± 280 | < 0.001 |
| Male, n (%) | 69 (46.3) | 1,087 (50.0) | NS |
| Antenatal steroid use | 108/141 (76.6) | 1,601/2,333 (75.1) | NS |
| PROM ≥ 18 hr | 48 (32.9) | 770 (34.5) | NS |
| Maternal chorioamnionitis | 40/114 (35.9) | 627/1,843 (34.0) | NS |
| Resuscitation at delivery* | 143/147 (97.3) | 1,881/2,149 (87.9) | < 0.001 |
| Hypotension ≤ 1 week | 90 (60.4) | 567 (26.1) | < 0.001 |
| RDS | 140 (94.0) | 1,654 (76.0) | < 0.001 |
| Pneumothorax | 24 (16.1) | 100 (4.6) | < 0.001 |
| Massive pulmonary hemorrhage | 24 (16.1) | 126 (5.8) | < 0.001 |
| Pulmonary hypertension | 20 (13.4) | 133 (6.1) | < 0.001 |
| IVH > grade II | 48 (32.2) | 180 (8.3) | < 0.001 |
| Sepsis | 69 (46.3) | 404 (19.0) | <0.001 |
| No sepsis | 80/133 (60.2) | 1,773/2,158 (82.2) | <0.001 |
| Early sepsis | 12 (9.0) | 85 (3.9) | |
| Late sepsis | 41 (30.8) | 300 (13.9) | |
| PDA† | 88/(59.1) | 802/2,177 (36.8) | < 0.001 |
*Resuscitation included oxygen use or positive pressure ventilation or intubation or cardiac massage or drug use; †PDA was defined when pharmacological or surgical treatment was intervened. g, gram body weight; PROM, premature rupture of membrane; RDS, respiratory distress syndrome; IVH, intraventricular hemorrhage; PDA, patent ductus arteriosus.
Table 2. Clinical outcomes of VLBWI (n = 2,326); NEC vs. no NEC group.
| Outcomes | NEC (n = 149) | No NEC (n = 2,177) | P value |
|---|---|---|---|
| PDA ligation | 35 (23.5) | 252 (11.6) | NS |
| 100 mL/kg/day feeding (days) | 43.8 ± 35.4 | 23.5 ± 19.8 | < 0.001 |
| TPN duration* | 47.7 ± 36.2 | 24.3 ± 22.5 | < 0.001 |
| Hospitalized days* | 73.3 ± 49.21 | 64.2 ± 38.5 | 0.031 |
| PVL | 35/143 (24.5) | 170/2,112 (8.1) | < 0.001 |
| Mortality | 63/149 (42.3) | 201/2,177 (9.2) | < 0.001 |
*Expired patients were excluded. PVL, periventricular leukomalacia; PDA, patent ductus arteriosus; TPN, total parental nutrition.
NEC vs. no NEC group (1:1 matched)
Because GA and birth weight are significant contributing factors in the NEC group, they were respectively matched with those in the no NEC group (1:1 matching) to identify variables independently associated with an increased risk for NEC in our univariate analysis. Despite the fact that GA and birth weight were matched, hypotension, IVH >grade II were clinical factors independently associated with the NEC group (Table 3). With regards to clinical outcome, the NEC group had longer times to reach 100 mL/kg/day feeding (P=0.013), longer TPN duration (P<0.001) and higher PVL (P=0.004) (Table 4). We performed a multivariate logistic regression analysis after 1:1 matching. Hypotension ≤1 week was found to be consistently associated with NEC (Table 5).
Table 3. Clinical characteristics of NEC vs. no NEC group; 1:1matched.
| NEC (n=145) | No NEC (n=145) | P value | |
|---|---|---|---|
| Gestational age (week) | 26.6 ± 2.5 | 26.6 ± 2.6 | NS |
| Birth weight (g) | 837 ± 243 | 837 ± 243 | NS |
| Male, n (%) | 68 (46.9) | 79 (54.5) | NS |
| Antenatal steroid use | 105/137 (76.6) | 107/144 (74.3) | NS |
| PROM ≥ 18 hr | 47/142 (33.1) | 56 (38.6) | NS |
| Maternal chorioamnionitis | 40/111 (36.4) | 49/121 (40.5) | NS |
| Resuscitation at delivery | 139/143 (97.3) | 138/144 (95.8) | NS |
| Hypotension ≤ 1 week | 88(60.7) | 63 (43.4) | < 0.001 |
| RDS | 136 (93.8) | 133 (91.7) | NS |
| Pneumothorax | 22 (15.7) | 12 (8.3) | NS |
| Massive pulmonary hemorrhage | 22 (15.7) | 20 (13.8) | NS |
| Pulmonary hypertension | 19 (13.1) | 18 (1) | NS |
| IVH > grade II | 47 (32.4) | 28 (19.3) | 0.008 |
| Sepsis | 66 (45.5) | 48 (33.1) | 0.027 |
| PDA* | 87 (60.0) | 72 (49.7) | NS |
*PDA was defined when pharmacological or surgical treatment was intervened. g, gram body weight; PROM, premature rupture of membrane; RDS, respiratory distress syndrome; IVH, intraventricular hemorrhage; PVL, periventricular leukomalacia; PDA, patent ductus arteriosus.
Table 4. Clinical outcomes of NEC vs. No NEC group; 1:1 matched.
| Outcomes | NEC (n = 145) | No NEC (n = 145) | P value |
|---|---|---|---|
| PDA ligation | 35 (24.1) | 36 (24.8) | NS |
| 100 mL/kg/day feeding (days) | 42.4 ± 35.3 | 23.5 ± 36.2 | 0.013 |
| TPN duration* | 47.7 ± 36.2 | 35.5 ± 25.1 | < 0.001 |
| Hospitalized days* | 73.8 ± 49.4 | 83.6 ± 38.5 | NS |
| PVL | 34/139 (24.5) | 18/138 (13.0) | 0.004 |
*Expired patients were excluded. PVL, periventricular leukomalacia; PDA, patent ductus arteriosus; TPN, total parental nutrition.
Table 5. NEC risk factor in multiple conditional logistic regression analysis; 1:1 matched.
| Risk factors | OR | P value | 95% CI |
|---|---|---|---|
| Resuscitation at delivery | 1.667 | NS | 0.398-6.974 |
| < 36.0 C at admission | 1.000 | NS | 0.500-2.000 |
| Hypotension ≤ 1 week | 2.000 | 0.040 | 1.000-3.999 |
| RDS | 1.600 | NS | 0.523-4.891 |
| Pneumothorax | 1.909 | NS | 0.920-3.959 |
| Massive pulmonary hemorrhage | 1.118 | NS | 0.581-2.150 |
| Pulmonary hypertension* | 1.067 | NS | 0.527-2.157 |
| IVH > grade II | 2.545 | NS | 0.235-1.404 |
| Sepsis | 1.750 | NS | 0.707-2.862 |
Variables included in the multivariable logistic regression model: resuscitation at delivery, lower body temperature at admission (<36.0), hypotension, RDS, pneumothorax, massive pulmonary hemorrhage, pulmonary hypertension (<1 week), IVH>grade II, sepsis and early sepsis. *Use of nitrioxide or sildenafil or iloprost within 1 week of birth. RDS, respiratory distress syndrome; IVH, intraventricular hemorrhage.
Medical vs. Surgical NEC
After 15 NEC infants were not included due to their unknown NEC management, a total of 134 patients were compared on their NEC management. In evaluating differences between surgically and medically treated NEC, GA was significantly lower and PDA incidence was more prevalent in the surgical NEC group (Table 6). The rest of clinical factors did not have significant difference between the two groups including mortality. Because more PDA incidence might be due to lower GA in the surgical group, we adjusted GA between the two groups. Even after adjustment of GA, PDA incidence was significantly higher in the surgical NEC group (Table 6).
Table 6. Clinical characteristics of medical vs. surgical NEC (n = 145).
| Characteristics | Medical (n = 57) | Surgical (n = 77) | P value |
|---|---|---|---|
| Gestational age (week) | 27.1 ± 2.4 | 26.4 ± 2.7 | 0.032 |
| Birth weight (g) | 881 ± 270.7 | 813 ± 221.8 | NS |
| Male, n (%) | 26 (45.6) | 36 (46.8) | NS |
| Antenatal steroid use | 42 (75.0) | 54 (76.1) | NS |
| PROM ≥ 18 hr | 19 (33.3) | 23 (31.1) | NS |
| Maternal chorioamnionitis | 17 (35.4) | 19 (35.9) | NS |
| Resuscitation at delivery | 54 (94.8) | 75 (98.7) | NS |
| < 36.0 C at admission | 47 (88.7) | 52 (80.0) | NS |
| Hypotension ≤ 1 week | 88 (60.41) | 63 (43.5) | NS |
| RDS | 31 (54.4) | 50 (64.9) | NS |
| Surfactant use | 39 (68.4) | 55 (71.4) | NS |
| Pneumothorax | 11 (19.3) | 11(14.3) | NS |
| Massive pulmonary hemorrhage | 10 (17.5) | 11(14.3) | NS |
| Pulmonary hypertension | 6 (10.5) | 11 (14.3) | NS |
| IVH > grade II | 19 (23.2) | 20 (18.2) | NS |
| Sepsis | 23 (40.4) | 38 (49.4) | NS |
| PDA | 26 (45.6) | 57 (74.0) | <0.001/0.002† |
| PVL | 16 (29.6) | 17 (22.4) | NS |
| PDA ligation | 11 (19.3) | 24 (31.2) | NS |
| Mortality* | 9 (15.8) | 23 (29.9) | NS |
*Of the 38 expired patients directly caused by NEC, 6 patients had a missing data on their mortality and, thereby, were excluded in this analysis; †Modified P value: according to multivariable logistic regression analysis after adjusting gestational age. g, gram body weight; NSD, normal spontaneous delivery; PROM, premature rupture of membrane; RDS, respiratory distress syndrome; IVH, intraventricular hemorrhage; PVL, periventricular leukomalacia; PDA, patent ductus arteriosus.
DISCUSSION
This was the first cohort KNN study to report NEC incidence and outcomes for VLBWI in Korea based on of GA-specific information. The overall incidence of NEC among VLBWI in 55 NICUs in Korea is 6.8%, which is similar to that of other reported multi-center incidences for NEC. The typical reported incidence in other network databases is 5%-9% for VLBWI (4,8,9,10,11), but it is as high as 11% for preterm babies born at <28 week' gestation (9). Fanaroff et al. (8) reported that population-level incidence of NEC has not decreased in over a decade. On the other hand, the Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network reported that the GA specific mean incidence for NEC among VLBWI increased from 9% to 15% between 2003 and 2007 (9). Some authors have noted that the incidence of NEC may be increased if spontaneous intestinal perforation (SIP) is misclassified as NEC stage 3 (12). In our study, SIP was considered a different and separate disease entity from NEC. Thus, there was a simultaneous diagnosis of SIP and NEC for 52 neonates (2%) who were excluded in this analysis. More detailed information about feeding protocols of each unit may be further studied if an increasing trend for NEC incidence in Korea is noted in the future monitoring. In Fig. 1 and 2, the initial downward curves of the NEC incidence are noted for extremely premature infants. The lower incidence for NEC in those less than 25 weeks of gestational age (Fig. 1) and less than 800 g birth weight (Fig. 2) may be because extremely premature infants die earlier even before an NEC diagnosis may be made.
Thus far, GA and birth weight have well been documented to be predispositions for NEC. Hypotension is also considered an independently increased risk for NEC. Our findings add that clinical factors related to vascular- or perfusion-related gastrointestinal compromise such as hypotension within a week of life is significant clinical factors for NEC stage ≥2 for VLBWI in Korea. Hypotension in this study was identified within 7 days of birth, which may suggest a circulatory collapse that affects to the gastrointestinal circulatory system. This assault on gastrointestinal blood flow may later result in an increased incidence of NEC. Examination of lower GA and birth weight infants reveals that the mean or median age of the occurrence of NEC ranges from 13 to 23 days (13,14), and "classic" NEC occurring in preterm infants after 8 to 10 days of age might reveal that low blood pressure in the first week attributes to a risk factor for NEC in VLBW infants (12). In addition, hypotension has been documented to be related to patent ductus arteriosus (PDA) (15) and early sepsis (16). Yet, the incidence of PDA and early sepsis were not significantly different between the NEC and no NEC groups in this study. Even after 1:1 matching of GA and birth weight, immature host defense mechanisms such as vascular-or perfusion instability manifested as hypotension in this study was significantly more shown in the NEC group.
Since the reperfusion injury is implicated in the induction of inflammatory cascades of vascular injury and increased susceptibility to bacterial penetration (17,18,19), it was not surprising to observe that sepsis and PVL are associated with NEC. Hintz et al. (20) further reported that fetuses may be previously exposed to pro-inflammatory cytokines as a consequence of sepsis either from prenatal or perinatal infection. PVL diagnoses were more likely to occur in neonates with sepsis and surgery in the NEC group. Hintz (20) suggested that the cascade of inflammatory events lead to adverse neurodevelopmental outcomes. They noted that PVL was closely associated with surgical NEC which was later associated with poor neurodevelopmental outcomes at 18 to 22 month follow up. These results came out to be consistent with previous smaller studies (21,22,23). Further, Shah et al. (24) manifested that infants with both sepsis and NEC had a high incidence (80%) of white matter abnormalities consistent with non-cystic PVL by MRI at term equivalent and, after all, they had an increased risk of having lower Bayley Mental and Psychomotor Development Index scores at age 2 yr.
With regards to other hospital outcome, NEC group had prolonged hospital stays (4,20) and greater times to reach full feeding. In respect to NEC mortality, NEC usually leads to death in up to 30 to 50% of the premature infants who develop it (25,26). Our NEC mortality is 26.2% when 38 patients from the NEC group died directly caused by NEC which was lower than the reported range (2,4,12,20).
In the NEC group (n=149), the GA for surgical NEC was significantly lower than that for medically managed NEC. Yet, birth weight was not significantly different between the two groups. This finding suggests that the overall immaturity rather than low birth weight may contribute to the severity of NEC. The lack of immunity of gastrointestinal tract and a healthy gut environment together with an immature mucosal barrier, defense and circulatory regulation may result in disease progression. Surgical therapy seems to be one of the most important steps that contribute to clinical outcome as in short- and long-term outcomes neurologically (3,12,20). The surgical decision making for NEC is still challenging and must be carefully analyzed with wider array of factors into consideration and further studied are needed in the future.
However, this study has a few limitations. First, the time of diagnosis for NEC was not available for determining relationships between associated clinical variables, particularly IVH >2, PVL and sepsis, which were associated with NEC in our 1:1 matched data. In addition, we were unable to evaluate interactions due to a lack of time information. Secondly, this study was limited by incomplete and less informative data. For example, the type of milk, timing and rate of feeding advancement were not available. Also, missing data was one of the limitations in this study analysis. Lastly, some of the clinical factors may be confounded by unmeasured related variables.
In summary, we have described the occurrence of NEC in a large national neonatal cohort in Korea. The strengths of this study include the large cohort size, standardization of the definitions of neonatal morbidities among different units, and organization of prospective data collection. This study is the first report of national NEC data from VLBWI in Korea, allowing us to take a peek into the epidemiology and management of NEC and associated clinical variables related to NEC. If possible in the future, long- term neurodevelopmental outcomes of NEC data may allow for the assessment of additional clinical predictors. It may be interesting to investigate the long-term interaction with NEC for VLBWI in Korea. Further studies are required to search for additional relationship with NEC and a better understanding of this disease process.
Footnotes
Funding: This research was supported by a grant (2013-E63008-01) from the Research of Korea Centers for Disease Control and Prevention.
DISCLOSURE: The authors have no conflicts of interest to disclose.
References
- 1.Neu J, Walker WA. Necrotizing enterocolitis. N Engl J Med. 2011;364:255–264. doi: 10.1056/NEJMra1005408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schnabl KL, Van Aerde JE, Thomson AB, Clandinin MT. Necrotizing enterocolitis: a multifactorial disease with no cure. World J Gastroenterol. 2008;14:2142–2161. doi: 10.3748/wjg.14.2142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thompson AM, Bizzarro MJ. Necrotizing enterocolitis in newborns: pathogenesis, prevention and management. Drugs. 2008;68:1227–1238. doi: 10.2165/00003495-200868090-00004. [DOI] [PubMed] [Google Scholar]
- 4.Guthrie SO, Gordon PV, Thomas V, Thorp JA, Peabody J, Clark RH. Necrotizing enterocolitis among neonates in the United States. J Perinatol. 2003;23:278–285. doi: 10.1038/sj.jp.7210892. [DOI] [PubMed] [Google Scholar]
- 5.Toltzis P. 50 years ago in The Journal of Pediatrics: Necrotizing enterocolitis in premature infants. J Pediatr. 2015;166:883. doi: 10.1016/j.jpeds.2014.11.005. [DOI] [PubMed] [Google Scholar]
- 6.Choi YY. Necrotizing enterocolitis in newborns: update in pathophysiology and newly emerging therapeutic strategies. Korean J Pediatr. 2014;57:505–513. doi: 10.3345/kjp.2014.57.12.505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gephart SM, Spitzer AR, Effken JA, Dodd E, Halpern M, McGrath JM. Discrimination of GutCheck (NEC): a clinical risk index for necrotizing enterocolitis. J Perinatol. 2014;34:468–475. doi: 10.1038/jp.2014.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fanaroff AA, Stoll BJ, Wright LL, Carlo WA, Ehrenkranz RA, Stark AR, Bauer CR, Donovan EF, Korones SB, Laptook AR, et al. Trends in neonatal morbidity and mortality for very low birthweight infants. Am J Obstet Gynecol. 2007;196:147.e1–147.e8. doi: 10.1016/j.ajog.2006.09.014. [DOI] [PubMed] [Google Scholar]
- 9.Stoll BJ, Hansen NI, Bell EF, Shankaran S, Laptook AR, Walsh MC, Hale EC, Newman NS, Schibler K, Carlo WA, et al. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics. 2010;126:443–456. doi: 10.1542/peds.2009-2959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Horbar JD, Badger GJ, Carpenter JH, Fanaroff AA, Kilpatrick S, LaCorte M, Phibbs R, Soll RF Members of the Vermont Oxford Network. Trends in mortality and morbidity for very low birth weight infants, 1991-1999. Pediatrics. 2002;110:143–151. doi: 10.1542/peds.110.1.143. [DOI] [PubMed] [Google Scholar]
- 11.Wilson-Costello D, Friedman H, Minich N, Siner B, Taylor G, Schluchter M, Hack M. Improved neurodevelopmental outcomes for extremely low birth weight infants in 2000-2002. Pediatrics. 2007;119:37–45. doi: 10.1542/peds.2006-1416. [DOI] [PubMed] [Google Scholar]
- 12.Yee WH, Soraisham AS, Shah VS, Aziz K, Yoon W, Lee SK Canadian Neonatal Network. Incidence and timing of presentation of necrotizing enterocolitis in preterm infants. Pediatrics. 2012;129:e298–e304. doi: 10.1542/peds.2011-2022. [DOI] [PubMed] [Google Scholar]
- 13.Llanos AR, Moss ME, Pinzòn MC, Dye T, Sinkin RA, Kendig JW. Epidemiology of neonatal necrotising enterocolitis: a population-based study. Paediatr Perinat Epidemiol. 2002;16:342–349. doi: 10.1046/j.1365-3016.2002.00445.x. [DOI] [PubMed] [Google Scholar]
- 14.Stoll BJ, Kanto WP, Jr, Glass RI, Nahmias AJ, Brann AW., Jr Epidemiology of necrotizing enterocolitis: a case control study. J Pediatr. 1980;96:447–451. doi: 10.1016/s0022-3476(80)80696-2. [DOI] [PubMed] [Google Scholar]
- 15.Dollberg S, Lusky A, Reichman B. Patent ductus arteriosus, indomethacin and necrotizing enterocolitis in very low birth weight infants: a population-based study. J Pediatr Gastroenterol Nutr. 2005;40:184–188. doi: 10.1097/00005176-200502000-00019. [DOI] [PubMed] [Google Scholar]
- 16.Casserly B, Phillips GS, Schorr C, Dellinger RP, Townsend SR, Osborn TM, Reinhart K, Selvakumar N, Levy MM. Lactate measurements in sepsis-induced tissue hypoperfusion: results from the Surviving Sepsis Campaign database. Crit Care Med. 2015;43:567–573. doi: 10.1097/CCM.0000000000000742. [DOI] [PubMed] [Google Scholar]
- 17.Stevenson DK, Blakely ML. Historical perspective: necrotizing enterocolitis: an inherited or acquired condition? NeoReviews. 2006;7:e125–e134. [Google Scholar]
- 18.Robel-Tillig E, Vogtmann C, Faber R. Postnatal intestinal disturbances in small-for-gestational-age premature infants after prenatal haemodynamic disturbances. Acta Paediatr. 2000;89:324–330. [PubMed] [Google Scholar]
- 19.Israel EJ. Necrotizing enterocolitis. In: Long SA, editor. Principles and practice of pediatric infectious disease. 2nd ed. Philadelphia: Churchill Livingstone; 2003. [Google Scholar]
- 20.Hintz SR, Kendrick DE, Stoll BJ, Vohr BR, Fanaroff AA, Donovan EF, Poole WK, Blakely ML, Wright L, Higgins R, et al. Neurodevelopmental and growth outcomes of extremely low birth weight infants after necrotizing enterocolitis. Pediatrics. 2005;115:696–703. doi: 10.1542/peds.2004-0569. [DOI] [PubMed] [Google Scholar]
- 21.Simon NP, Brady NR, Stafford RL, Powell RW. The effect of abdominal incisions on early motor development of infants with necrotizing enterocolitis. Dev Med Child Neurol. 1993;35:49–53. doi: 10.1111/j.1469-8749.1993.tb11551.x. [DOI] [PubMed] [Google Scholar]
- 22.Tobiansky R, Lui K, Roberts S, Veddovi M. Neurodevelopmental outcome in very low birthweight infants with necrotizing enterocolitis requiring surgery. J Paediatr Child Health. 1995;31:233–236. doi: 10.1111/j.1440-1754.1995.tb00792.x. [DOI] [PubMed] [Google Scholar]
- 23.Chacko J, Ford WD, Haslam R. Growth and neurodevelopmental outcome in extremely-low-birth-weight infants after laparotomy. Pediatr Surg Int. 1999;15:496–499. doi: 10.1007/s003830050648. [DOI] [PubMed] [Google Scholar]
- 24.Shah DK, Doyle LW, Anderson PJ, Bear M, Daley AJ, Hunt RW, Inder TE. Adverse neurodevelopment in preterm infants with postnatal sepsis or necrotizing enterocolitis is mediated by white matter abnormalities on magnetic resonance imaging at term. J Pediatr. 2008;153:170–175. doi: 10.1016/j.jpeds.2008.02.033. [DOI] [PubMed] [Google Scholar]
- 25.Luig M, Lui K. Epidemiology of necrotizing enterocolitis-- Part I: Changing regional trends in extremely preterm infants over 14 years. J Paediatr Child Health. 2005;41:169–173. doi: 10.1111/j.1440-1754.2005.00582.x. [DOI] [PubMed] [Google Scholar]
- 26.Abdullah F, Zhang Y, Camp M, Mukherjee D, Gabre-Kidan A, Colombani PM, Chang DC. Necrotizing enterocolitis in 20,822 infants: analysis of medical and surgical treatments. Clin Pediatr (Phila) 2010;49:166–171. doi: 10.1177/0009922809349161. [DOI] [PubMed] [Google Scholar]