Abstract
This study was conducted to describe the incidence, risk factors, and current treatment status of retinopathy of prematurity (ROP) in very-low-birth-weight (VLBW) infants registered in the Korean Neonatal Network database. Medical records of 2,009 VLBW infants born between January 2013 and June 2014 who underwent examination by an ophthalmologist were reviewed. The total incidence of ROP was 34.1%. Of the patients, 11.6% showed ROP stage ≥ 3 and 11.5% received treatment of VLBW. Among all infants who received treatment of ROP, 63.6% underwent operation only; 16.9%, anti-vascular endothelial growth factor (anti-VEGF) treatment only; and 19.5%, both operation and anti-VEGF treatment. The mean gestational age (GA) and birth weight (BW) were significantly lower and the prevalence rates of respiratory distress syndrome, patent ductus arteriosus (PDA), invasive ventilator duration, and sepsis were significantly higher in the VLBW infants with ROP than in those without ROP. In the multivariable logistic regression analysis, PDA (odd ratio [OR], 2.1; 95% confidence interval [CI], 1.11-3.79) and invasive ventilator duration (OR, 1.0; 95% CI, 1.00-1.02) were significant risk factors of ROP and ROP stage ≥ 3. In conclusion, the high incidence of ROP is associated with low GA and BW, and attempt to reduce the aforementioned risk factors could reduce the incidence of ROP stage ≥ 3 in VLBW infants.
Keywords: Retinopathy of Prematurity, Infant, Very-Low-Birth-Weight
INTRODUCTION
The morbidity and survival rates of very-low-birth-weight (VLBW) infants have increased owing to improved management of neonatal intensive care. Retinopathy of prematurity (ROP), which is a disorder involving the abnormal development of the retinal vasculature, is an important morbidity in VLBW infants. The long-term outcomes of ROP include retinal detachment, cataract, glaucoma, and strabismus (1,2,3). The incidence rate of childhood blindness caused by ROP ranges from 3% to 10% (4,5). Therefore, proper management is important for reducing or preventing the incidence of ROP in VLBW infants.
Lower gestational age (GA) and birth weight (BW) are common risk factors of ROP in preterm infants. In addition, oxygen therapy, respiratory distress syndrome (RDS), intrauterine infection, sepsis, and postnatal blood transfusion contribute to the development of ROP (1,6,7). Studies on the incidence and outcomes of ROP among VLBW infants from different nationwide world networks have been published (8,9). As nationwide data were not available in Korea before, it is nearly impossible to document the epidemiology of ROP among VLBW infants in the country. Moreover, according to the increasing survival rate of extremely low birth weight (ELBW) infants in Korea, the incidence and severity of ROP have been unavoidably increasing recently. Thus, the incidence, treatment, and risk factors of ROP should be determined in order to decrease the severe outcomes of ROP in VLBW infants.
This study was conducted to determine the current status of ROP among VLBW infants in Korea based on data collected from the Korean Neonatal Network (KNN) database (10). The incidence of ROP stage ≥ 3 and the current treatment requirement of the disease according to GA and BW were analyzed. Furthermore, the risk factors and treatment requirement of ROP stage ≥ 3 were also analyzed.
MATERIALS AND METHODS
Study population
Infants weighing < 1,500 g at birth who were born from January 2013 to June 2014 in or transferred within 28 days of birth to the participating neonatal intensive care units (NICU) of the KNN (10) were prospectively registered in the KNN database. Infants whose parents did not agree to participate in the KNN (10) were excluded.
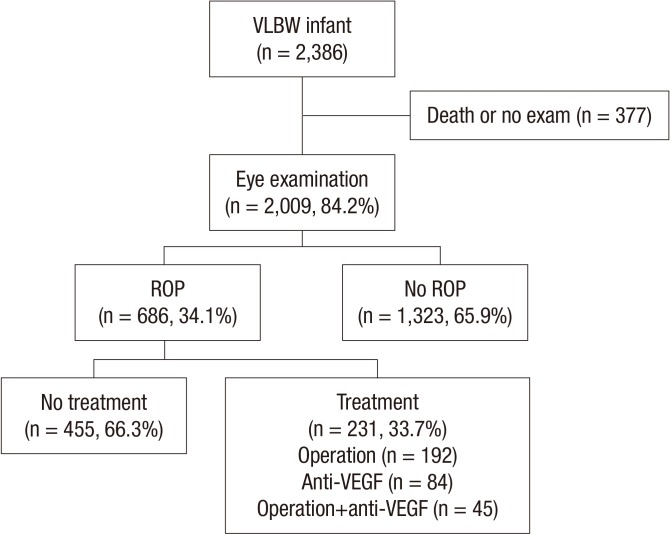
Among the 2,386 infants in 55 participating NICUs of the KNN (10), 377 were excluded because they died prior to ophthalmic examination (284 infants) or had not undergone oph-thalmic examination (93 infants). Of the 93 infants who had not undergone ophthalmic examination, 88 had not undergone ophthalmic examination during hospitalization and 5 were transferred to another hospital for reasons not related to ROP and had no available follow-up data regarding ROP. Finally, 2,009 infants were enrolled in this study (Fig. 1).
Fig. 1. Schematic diagram of the enrolled patient in the study. ROP, retinopathy of prematurity; VLBW, very-low-birth-weight infant; VEGF, vascular endothelial growth factor.
Criteria for ROP examination and treatment of ROP
The suggested criteria for the first ROP exam included infants with a BW of ≤ 1,500 g or a GA ≤ 30 weeks (11,12). The suggested indications for treatment were any stage with plus disease or stage 3 of zone I ROP and stages 2 or 3 with disease of zone II ROP (11,12). The treatment for ROP included operation (cryotherapy or laser photocoagulation and/or vitrectomy) and/or an intravitreal injection with a vascular endothelial growth factor (anti-VEGF) agent. All ophthalmic examinations and treatment were done by a qualified ophthalmologist in participating centers. However, KNN data lack informations regarding presence of plus disease or zone status. Epidemiology and ROP treatment were based on available data on stages of ROP.
Data collection
Data were collected from the KNN (10) according to a medical chart review by trained data abstractors who used the definitions and protocols contained in a standard manual of operation. The data were then sent electronically to the KNN (10) coordinating center, which is located at the Clinical Research Institute of the Samsung Medical Center, Seoul, Korea. Patient in-formation was collected until death or discharge from the NICU.
Data analysis
The 2,009 infants who received ophthalmic examinations for ROP were included in the analysis. Infants who died prior to discharge were excluded. The stages of ROP were classified from 1 to 5 according to the International Classification of Retinopathy of Prematurity (11,12). The highest stage of ROP in each infant was recorded. The incidence of ROP and treatment were analyzed according to the stages of ROP, and subgroup analysis according to GA and BW was conducted. To identify risk factors associated with ROP stage ≥ 3, the characteristics of all the infants, and maternal and neonatal variables were compared according to the severity (No ROP, ROP stage ≤ 2 and ROP stage ≥ 3) and multivariable logistic regression analysis was performed. Differences in treatment methods according to severity of ROP were analyzed. To determine differences in the clinical characteristics according to the treatment methods, a comparative analysis was performed between the 3 groups, namely 1) the infants who underwent operation only,2) the infants who underwent anti-VEGF treatment only, and 3) the infants who underwent both operation and anti-VEGF treatment.
Definitions of outcomes
The maternal and neonatal variables included GA, BW, sex, delivery mode, pregnancy-induced hypertension (PIH), maternal steroid use, gestational diabetes mellitus, premature rupture of membrane, oligohydramnios, chorioamnionitis (histologically confirmed), Apgar score at 1 and 5 min, pulmonary air leak, pulmonary hemorrhage, pulmonary hypertension, respiratory distress syndrome (RDS), duration of invasive ventilation, duration of oxygen supplementation, postnatal steroid use, symptomatic patent ductus arteriosus (PDA), red blood cell (RBC) transfusion, necrotizing enterocolitis (NEC), intraventricular hemorrhage (IVH), periventricular leukomalacia (PVL), bronchopulmonary dysplasia (BPD), sepsis, and length of hospitalization. The variables used were predefined according to the KNN standard manual of operation.
RDS was defined as respiratory distress requiring ventilator care with diagnosis based on chest radiographic findings. When RDS was diagnosed, prophylactic surfactant therapy was used at the discretion of the attending neonatologist. Invasive ventilation was defined as an endotracheal ventilatory support by conventional or high-frequency oscillation ventilation. Oxygen supplementation was defined as respiratory support with oxygen via a hood, mask, or low-flow nasal cannula. Symptomatic patent ductus arteriosus was defined as a hemodynamically significant PDA confirmed by using echocardiography plus at least one of the following symptoms: 1) systolic or continuous murmur,2) bounding pulse or hyperactive precordial pulsation,3) hypotension intractable with inotropics,4) aggravation of respiratory symptoms, and 5) heart failure evidenced by pulmonary edema, appearance of increasing pulmonary flow, and cardiothoracic ratio>60% on chest radiography.
Statistical analysis
Descriptive statistical methods were used to describe the study population. The maternal, neonatal characteristics and outcomes between three groups according to the severity of ROP were compared by using ANOVA. The risk factors were analyzed by using a multivariable logistic regression analysis adjusted for GA and BW to estimate the odds ratios (OR) with 95% confidence intervals (CI). A P value <0.05 was considered statistically significant. The statistical analyses were performed using SAS V9.4 (SAS, Cary, NC, USA).
Ethics statement
The KNN registry was approved by the institutional review board at each participating hospital and informed consent was obtained from the parents at enrollment by the NICUs partici-pating in KNN.
RESULTS
Of the 2,009 infants who had undergone ophthalmic examination, 686 (34.1%) had diagnosed ROP. None of the infants was transferred to another hospital for ROP treatment.
Distribution of incidence of ROP
Of the VLBW infants who underwent ophthalmic examination, 65.9% (1,323/2,009) did not develop ROP. In the remaining infants, ROP reached stage 1 in 11.7% (235/2,009), stage 2 in 10.9% (218/2,009), stage 3 in 11.3% (229/2,009), and stage 4 in 0.2% (4/2,009). None of the infants developed stage 5 ROP. The incidence of ROP requiring either operation and/or anti-VEGF treatment was 11.5% (231/2,009) among all the VLBW infants and 33.7% (231/686) in the ROP group (Fig. 1).
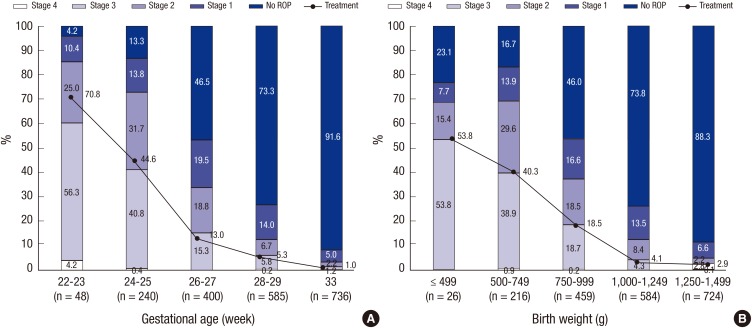
The incidence of ROP in the VLBW infants was analyzed according to GA, BW and the severity of ROP (Fig. 2). The incidence of ROP was higher with lower GA and lower BW. The incidence of ROP among the survivors at≤23 weeks of GA was 95.9% (46/48), 86.7% (208/240) among the survivors from 24 to 25 weeks of GA, 53.6% (214/400) among the survivors from 26 to 27 weeks of GA, 26.7% (156/585) among the survivors from 28 to 29 weeks of GA, and 11.9% (53/445) among the survivors from 30 to 31 weeks of GA. Among the infants <28 weeks of GA at birth, the incidence of ROP at any severity was 68.0% (468/688) and the incidence of ROP stage≥3 was 27.4% (189/688). The incidence of ROP was 76.9% (20/26) among the survivors with a BW <500 g, 83.3% (180/216) among those with a BW of 500-749 g, 54.0% (248/459) among those with a BW of 750-999 g, 26.2% (153/584) among those with a BW of 1,000-1,249 g, and 11.7% (85/724) among those with a BW≥1,250 g. Among the infants with a BW <1,000 g, the incidence of ROP at any severity was 63.9% (448/701) and the incidence of ROP stage≥3 was 26.7% (187/701).
Fig. 2. The incidences of severity of ROP and treatment according to the gestational age and birth weight in VLBW infants. (A) The incidences of severity of ROP and treatment according to gestational age. (B) The incidences of severity of ROP and treatment according to birth weight. ROP, retinopathy of prematurity; VLBW, very-low-birth-weight.
Characteristics in VLBW infants with ROP
Table 1 shows the maternal characteristics, neonatal characteristics and morbidities according to the severity of ROP. ROP stage≥3 was associated with younger GA, lower BW and Apgar scores at 1 and 5 min. Regarding maternal and obstetric factors, the incidence rate of PIH was lower and that of chorioamnionitis was higher among the infants with than among those without ROP. The incidence rates of pulmonary air leak, pulmonary hemorrhage, pulmonary hypertension, RDS, postnatal steroid use, symptomatic PDA, RBC transfusion, NEC, IVH, PVL, BPD, and sepsis were higher among the infants with than among those without ROP. ROP stage≥3 was associated with longer durations of invasive ventilation and oxygen supplementation.
Table 1. Characteristics of VLBW infants according to the staging of ROP.
| Characteristics | No ROP (n=1,323) | ROP | P value | |
|---|---|---|---|---|
| Stage ≤2 (n=453) | Stage ≥3 (n=233) | |||
| Maternal characteristics | ||||
| Vaginal delivery | 301 (22.8) | 128 (28.3) | 57 (24.5) | 0.061 |
| PIH | 294 (22.2) | 47 (10.4)* | 32 (13.7)† | < 0.001 |
| Maternal steroid use | 986 (76.0) | 358 (81.2) | 179 (78.5) | 0.075 |
| Maternal GDM | 119 (9.0) | 31 (6.8) | 13 (5.6) | 0.113 |
| Maternal PROM | 434 (32.9) | 201 (44.7)* | 89 (38.2) | < 0.001 |
| Oligohydramnios | 170 (13.7) | 64 (16.0) | 35 (16.4) | 0.386 |
| Chorioamnionitis | 328 (29.4) | 163 (44.7)* | 95 (45.5)† | < 0.001 |
| Neonatal characteristics | ||||
| Gestational age (week) | 29.8 ± 2.4 | 26.9 ± 2.2* | 25.7 ± 1.9†,‡ | < 0.001 |
| Birth weight (g) | 1,1966 ± 216 | 959 ± 244* | 821 ± 245†,‡ | < 0.001 |
| Apgar score at 1 min | 5.1 ± 1.9 | 4.2 ± 1.9* | 3.6 ± 1.7†,‡ | 0.003 |
| Apgar score at 5 min | 7.1 ± 1.6 | 6.5 ± 1.7* | 5.8 ± 1.8†,‡ | < 0.001 |
| Male | 658 (49.7) | 232 (51.2) | 115 (49.4) | 0.843 |
| Neonatal morbidities | ||||
| Pulmonary_air leak | 34 (2.6) | 25 (5.5)* | 15 (6.9)† | < 0.001 |
| Pulmonary hemorrhage | 26 (2.0) | 34 (7.5 )* | 24 (10.3)† | < 0.001 |
| Pulmonary hypertension | 30 (2.3) | 26 (5.7)* | 36 (15.5)†,‡ | < 0.001 |
| RDS | 934 (70.6) | 422 (95.6)* | 232 (99.6)†,‡ | < 0.001 |
| Invasive ventilation days | 8.1 ± 16.6 | 25.8 ± 24.4* | 44.0 ± 39.6†,‡ | < 0.001 |
| Oxygen supplement days | 7.9 ± 12.6 | 12.7 ± 17.3* | 16.6 ± 18.7†,‡ | 0.008 |
| Postnatal steroid use | 149 (11.3) | 226 (49.9)* | 122 (52.4)† | < 0.001 |
| PDA | 482 (36.4) | 283 (62.5)* | 195 (83.7)†,‡ | < 0.001 |
| RBC transfusion | 817 (61.8) | 379 (83.7)* | 219 (94.0)† | < 0.001 |
| NEC (Stage ≥ II) | 32 (2.4) | 31 (6.8)* | 29 (12.4)†,‡ | < 0.001 |
| IVH (Grade ≥ III) | 38 (2.9) | 47 (10.4)* | 43 (18.5)†,‡ | < 0.001 |
| PVL | 72 (5.5) | 68 (15.0)* | 31 (13.4 )† | < 0.001 |
| BPD | 574 (43.6) | 369 (81.6)* | 219 (94.0)†,‡ | < 0.001 |
| Sepsis | 188 (14.2) | 139 (30.7)* | 80 (34.3)† | < 0.001 |
Data are presented as n (%) or mean±standard deviation.*P<0.05, significant; between No ROP and ROP stage≤2; †P<0.05, significant; between No ROP and ROP stage≥3; ‡P<0.05, significant; between ROP stage≤2 and stage≥3. VLBW, very-low-birth-weight; ROP, retinopathy of prematurity; PIH, pregnancy induced hypertension; GDM, gestational diabetes mellitus; PROM, premature rupture of membrane; NICU, neonatal intensive care unit; RDS, respiratory distress syndrome; PDA, patent ductus arteriosus; RBC, red blood cell; NEC, necrotizing enterocolitis; IVH, intraventricular hemorrhage; PVL, periventricular leukomalacia; BPD, bronchopulmonary dysplasia.
The results of the multivariable logistic regression analysis showed that GA (OR, 0.704; 95% CI, 0.645-0.767; P<0.001), duration of invasive ventilation (OR, 1.013; 95% CI, 1.004-1.021; P=0.004), PDA (OR, 1.902; 95% CI, 1.200-3.015; P=0.006), and PDA requiring medication (OR, 1.591; 95% CI, 1.008-2.510; P= 0.046) significantly correlated with the development of ROP. The multivariable logistic regression analysis adjusted for GA and BW revealed that the duration of invasive ventilation (OR, 1.013; 95% CI, 1.004-1.023; P=0.005) and PDA (OR, 2.054; 95% CI, 1.111-3.797; P=0.022) significantly correlated with ROP stage≥3 (Table 2).
Table 2. Multivariable logistic regression analysis for factors associated with ROP stage ≥ 3 in VLBW infants.
| Variables | Odds ratio | 95% confidence interval | P value |
|---|---|---|---|
| Gestational age | 1.017 | 1.000-1.034 | 0.050 |
| Birth weight | 1.001 | 1.000-1.002 | 0.072 |
| RDS | 0.361 | 0.077-1.698 | 0.197 |
| PDA | 2.054 | 1.111-3.797 | 0.022 |
| Invasive ventilation days | 1.013 | 1.004-1.023 | 0.005 |
| Oxygen supplement days | 0.994 | 0.984-1.004 | 0.220 |
| RBC transfusion | 0.958 | 0.483-1.899 | 0.902 |
ROP, retinopathy of prematurity; VLBWI, very-low-birth-weight; RDS, respiratory distress syndrome; PDA, patent ductus arteriosus; RBC, red blood cell.
Incidence of ROP requiring treatment
Among the infants who developed ROP, the incidence rates of ROP stage≥3 and ROP requiring treatment were 34.0% (233/686) and 33.7% (231/686), respectively.
The incidence of ROP requiring treatment was 11.5% (231/2,009) among the VLBW infants in comparison to 28.1% (193/688) and 26.5% (186/701) who required treatment among the infants with GA <28 weeks and BW<1,000 g, respectively.
Among all the VLBW infants who underwent ophthalmic examination, 9.6% (192/2,009) underwent operation, 4.2% (84/2,009) underwent anti-VEGF treatment, and 2.2% (45/2,009) infants underwent both operation and anti-VEGF treatment.
Table 3 shows the incidence of ROP requiring treatment according to the severity of ROP: 10.8% (49/452) among infants with ROP stage≤2 and 78% (182/233) among those with ROP stage≥3 required treatment. Table 4 show the characteristics of infants according to the treatment methods: 83.1% (192/231) infants with ROP underwent operation. Although the incidence of ROP requiring treatment was higher with lower GA and lower BW (Fig. 2), those requiring any type of treatment were most frequently observed among 24-25 weeks of GA and 500-999 g of BW.
Table 3. Treatment according to the staging of ROP in VLBW infants.
| Treatment | No. ROP (n=1,323) | ROP | ||||
|---|---|---|---|---|---|---|
| Stage 1 (n=235) | Stage 2 (n=218) | Stage 3 (n=229) | Stage 4 (n=4) | Total (n=686) | ||
| Gestational age (week) | 29.8 ± 2.4 | 27.4 ± 2.2 | 27.9 ± 2.1 | 27.4 ± 2.2 | 26.9 ± 2.2 | 26.5 ± 2.2 |
| Birth weight (g) | 1,197 ± 216 | 959 ± 244 | 1,025 ± 241 | 959 ± 244 | 912 ± 252 | 913 ± 252 |
| Length of hospitalization (d) | 59 ± 25 | 83 ± 36 | 98 ± 34 | 116 ± 42 | 154 ± 84 | 98 ± 38 |
| ROP_treatment (No. %) | - | 8 (3.4) | 41 (18.8) | 178 (78.4) | 4 (100) | 231 (33.7) |
| Operation | - | 6 (2.6) | 32 (14.7) | 150 (66.1) | 4 (100) | 192 (28.0) |
| Anti-VEGF | - | 3 (1.3) | 15 (6.9) | 65 (28.6) | 1 (25) | 84 (12.2) |
| Operation+anti-VEGF | - | 1 (0.4) | 6 (2.8) | 37 (16.3) | 1 (25) | 45 (6.6) |
Data are presented as n (%) or mean±standard deviation. ROP, retinopathy of prematurity; VEGF, vascular endothelial growth factor.
Table 4. Characteristics of VLBW infants with ROP requiring treatment according to the treatment methods.
| Characteristics | Only ROP operation (n = 147) | Only anti-VEGF treatment (n = 39) | Operation+ anti-VEGF (n = 45) |
|---|---|---|---|
| Treatment proportion (%) | 63.6 | 16.9 | 19.5 |
| Gestational age | |||
| Mean (week) | 25.5 ± 3.3 | 25.5 ± 3.4 | 25.0 ± 3.3 |
| 22-23 | 19 (12.9%) | 4 (10.3%) | 11 (24.4%) |
| 24-25 | 69 (46.9%) | 18 (46.2%) | 20 (44.4%) |
| 26-27 | 35 (23.8%) | 9 (23.1%) | 8 (18.2%) |
| ≥ 28 | 24 (16.3%) | 8 (20.5%) | 6 (13.6%) |
| Birth weight | |||
| Mean (g) | 828 ± 254 | 814 ± 238 | 761 ± 239 |
| ≤ 499 | 7 (4.8%) | 3 (7.7%) | 4 (8.9%) |
| 500-749 | 55 (37.4%) | 13 (33.3%) | 19 (42.2%) |
| 750-999 | 53 (36.1%) | 17 (43.6%) | 15 (33.3%) |
| ≥ 1,000 | 32 (21.8%) | 6 (15.4%) | 7 (15.6%) |
| Male | 61 (52.6%) | 13 (46.4%) | 26 (68.4%) |
| ROP severity | |||
| Stage ≤ 2 (%) | 31 (21.0) | 11 (28.2) | 7 (15.6) |
| Stage ≥ 3 (%) | 116 (79.0) | 28 (71.8) | 38 (84.4) |
Data are presented as n (%) or mean±standard deviation. ROP, retinopathy of prematurity; VEGF, vascular endothelial growth factor.
DISCUSSION
This study is the first to use a national cohort to investigate the incidence of ROP in Korea. The overall incidence of ROP among the VLBW infants examined in this study was 34.1%. In the United States, the National Institute of Child Health and Human Development Neonatal Research Network (NICHD NRN) found that the incidence of ROP was 59% among VLBW infants of GA≤28 weeks between 2003 and 2007 (8). The present study found that the VLBW infants with GA≤28 weeks showed a similar incidence of ROP of 58.9%.
In this study, the incidence rate of ROP ≥stage 3 among the examined VLBW infants was 11.6%. This incidence rate was higher than the 6% reported by the Canadian Neonatal Network (CNN) (13), similar to the 10% reported by the Neonatal Research Network of Japan (NRNJ) (8,14), and lower than the 19% reported in Taiwan (15).
The overall incidence of treated ROP in VLBW infants in the present study was higher than that reported by other authors; that is, 11.5% (231/2,009) in our study, 8.1% in the study of Turkey (16). In VLBW infants of GA≤28 weeks, the incidence of treated ROP was 22.2% in our study in comparison to 16% in the study of the NICHD NRN (8). The incidence of ROP requiring treatment among VLBW infants even with mild ROP (stage 1 or 2) was 10.9% as shown on Table 3, however, a detailed information regarding indication for treatment such as zone, plus sign, and final stage at the time of operation were not available from KNN database.
Several studies documented the efficacy of intravitreal anti-VEGF (17,18) especially in those with zone 1 or zone 2 posterior as stage 3+ ROP or aggressive posterior ROP. Our study showed that the total incidence of infants who underwent for anti-VEGF treatment was 36.4% with inter-institutional variability. The proportion of VLBW infants requiring anti-VEGF was highest at 45.2% among 24-25 weeks of gestational age in accordance to those presenting with most ROP stage≥3. In the future, we would need a standard guideline to treat ROP with anti-VGEF
The American Academy of Pediatrics Section on Ophthalmology and the American Academy of Ophthalmology recommend the screening of all infants with a BW≤1,500 g or a GA≤30 weeks and selected infants between 1,500 and 2,000 g or with a GA>30 weeks with an unstable clinical course (3). Interestingly, our data showed that the incidence of ROP of VLBW infant at GA≥31 weeks was 8.4% (62/763) including those with stage 3, emphasizing the importance of screening even older gestational aged infants when indicated.
In our study, 15.8% (377/2,386) of all the infants were excluded from the ROP screening, of whom 3.9% (93/2,386) had an unknown cause of the missed examination. Other reports have documented missed ROP screening at range of 8%-13% especially for larger and older infants (19,20). Van Sorge et al. (21) found that the major factor of failure to screen was the transfer to another facility. Hence, meticulous screening and assessment should be achieved in order not to miss developing ROP and ROP stage≥3
Several studies have reported (15,22,23,24,25) that GA, BW, maternal preeclampsia, anemia, septicemia, oxygen therapy, and mechanical ventilation were the risk factors of the predisposition to ROP. In this study, PDA and invasive ventilator duration were important factors of the development of ROP stage≥3. Speculation for these findings may have arisen owing to pulmonary deterioration necessitating ventilator support in those with PDA. The predefined definition of oxygen therapy does not require reporting the level of inspired fraction of oxygen and the duration of oxygen supplementation during ventilator use. This may have erroneously led to the conclusion that duration of oxygen therapy is not a risk factor of ROP stage≥3.
ROP stage≥3 is associated with increasing ophthalmologic morbidity. In long-term outcomes, ELBW infants with ROP stage≥3 had more impairments, including visual processing, visual-motor integration, visual learning, and lower intelligence quotients, than those without ROP stage≥3 (26,27,28). The ulti-mate goal of the KNN (10) is to facilitate the improvement of the quality of care provided in NICUs, which would lead to improved prognoses of high-risk newborns through the development of evidence-based neonatal medicine.
In summary, the incidence of overall ROP in Korea is higher than that in highly developed countries (29,30,31,32), and risk factors for ROP stage≥3 in VLBW infants were PDA and invasive ventilator. The limitation of this study includes the lack of ROP information on location (zone), extent (clock hours) of disease, and vascular changes in the posterior pole vessels (plus disease). In addition, the comparison of the incidence and severity of ROP between different countries may not be accurate because of differences in GA and BW, especially that of extreme preterm infants≤25 weeks.
Follow-up studies on morbidities associated with ROP that use long-term data from the KNN are in progress (10). Meanwhile, multidisciplinary teams, including neonatologists, obstetricians, ophthalmologists, and nurses should attempt to reduce the risk factors for ROP. Furthermore, research should focus on developing practical guidelines and preventive strategies for reducing the incidence of ROP in order to improve its status in VLBW infants in Korea.
Footnotes
Funding: This research was supported by a fund (2013-E63008-01) from the Research of Korea Centers for 252 Disease Control and Prevention.
DISCLOSURE: The authors have no conflicts of interest to disclose.
AUTHOR CONTRIBUTION: Conception and design of the study: Hwang, JH, Lee EH, and Kim Ellen AR, Acquisition of data: Hwang JH, Statistical Analysis: Hwang JH and Lee KB, First Draft of the manuscript: Hwang JH, Lee EH, Kim Ellen AR.
References
- 1.Malcolm W. Retinopathy of prematurity and ophthalmologic issue. In: Malcolm WF, editor. Beyond the NICU: comprehensive care of the high-risk infant. New York: McGraw Hill Professional; 2015. pp. 347–365. [Google Scholar]
- 2.Casteels I, Cassiman C, Van Calster J, Allegaert K. Educational paper: retinopathy of prematurity. Eur J Pediatr. 2012;171:887–893. doi: 10.1007/s00431-011-1610-7. [DOI] [PubMed] [Google Scholar]
- 3.Fierson WM American Academy of Pediatrics Section on Ophthalmology; American Academy of Ophthalmology; American Association for Pediatric Ophthalmology and Strabismus; American Association of Certified Orthoptists. Screening examination of premature infants for retinopathy of prematurity. Pediatrics. 2013;131:189–195. doi: 10.1542/peds.2012-2996. [DOI] [PubMed] [Google Scholar]
- 4.Goggin M, O'Keefe M. Childhood blindness in the Republic of Ireland: a national survey. Br J Ophthalmol. 1991;75:425–429. doi: 10.1136/bjo.75.7.425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Darlow BA. Retinopathy of prematurity: new developments bring concern and hope. J Paediatr Child Health. 2015;51:765–770. doi: 10.1111/jpc.12860. [DOI] [PubMed] [Google Scholar]
- 6.Isaza G, Arora S, Bal M, Chaudhary V. Incidence of retinopathy of prematurity and risk factors among premature infants at a neonatal intensive care unit in Canada. J Pediatr Ophthalmol Strabismus. 2013;50:27–32. doi: 10.3928/01913913-20121127-02. [DOI] [PubMed] [Google Scholar]
- 7.Nair PM, Ganesh A, Mitra S, Ganguly SS. Retinopathy of prematurity in VLBW and extreme LBW babies. Indian J Pediatr. 2003;70:303–306. doi: 10.1007/BF02723585. [DOI] [PubMed] [Google Scholar]
- 8.Stoll BJ, Hansen NI, Bell EF, Shankaran S, Laptook AR, Walsh MC, Hale EC, Newman NS, Schibler K, Carlo WA, et al. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics. 2010;126:443–456. doi: 10.1542/peds.2009-2959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Isayama T, Lee SK, Mori R, Kusuda S, Fujimura M, Ye XY, Shah PS Canadian Neonatal Network. Comparison of mortality and morbidity of very low birth weight infants between Canada and Japan. Pediatrics. 2012;130:e957–e965. doi: 10.1542/peds.2012-0336. [DOI] [PubMed] [Google Scholar]
- 10.Korean Neonatal Network database. Very low birth weight infants in 2013. [accessed on 1 July 2014]. Available at http://www.knn.or.kr/index.jsp.
- 11.An international classification of retinopathy of prematurity: Prepared by an international committee. Br J Ophthalmol. 1984;68:690–697. doi: 10.1136/bjo.68.10.690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.The International Committee for the Classification of the Late Stages of Retinopathy of Prematurity. An international classification of retinopathy of prematurity. II. The classification of retinal detachment. Arch Ophthalmol. 1987;105:906–912. [PubMed] [Google Scholar]
- 13.Statistics Canada. Births 2008 (Catalogue no. 84F0210X) [accessed on 3 March 2015]. Available at http://www.statcan.gc.ca/pub/84f0210x/84f0210x2008000-eng.
- 14.Ministry of Health Labour and Welfare in Japan. Vital Statistics in 2008. [accessed on 5 January 2015]. Available at http://www.mhlw.go.jp/toukei/saikin/hw/jinkou/kakutei08/index.html.
- 15.Yang CY, Lien R, Yang PH, Chu SM, Hsu JF, Fu RH, Chiang MC. Analysis of incidence and risk factors of retinopathy of prematurity among very-low-birth-weight infants in North Taiwan. Pediatr Neonatol. 2011;52:321–326. doi: 10.1016/j.pedneo.2011.08.004. [DOI] [PubMed] [Google Scholar]
- 16.Bas AY, Koc E, Dilmen U ROP Neonatal Study Group. Incidence and severity of retinopathy of prematurity in Turkey. Br J Ophthalmol. 2015;99:1311–1314. doi: 10.1136/bjophthalmol-2014-306286. [DOI] [PubMed] [Google Scholar]
- 17.Menke MN, Framme C, Nelle M, Berger MR, Sturm V, Wolf S. Intravitreal ranibizumab monotherapy to treat retinopathy of prematurity zone II, stage 3 with plus disease. BMC Ophthalmol. 2015;15:20. doi: 10.1186/s12886-015-0001-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mintz-Hittner HA, Kennedy KA, Chuang AZ BEAT-ROP Cooperative Group. Efficacy of intravitreal bevacizumab for stage 3+ retinopathy of prematurity. N Engl J Med. 2011;364:603–615. doi: 10.1056/NEJMoa1007374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Darlow BA, Hutchinson JL, Simpson JM, Henderson-Smart DJ, Donoghue DA, Evans NJ. Variation in rates of severe retinopathy of prematurity among neonatal intensive care units in the Australian and New Zealand Neonatal Network. Br J Ophthalmol. 2005;89:1592–1596. doi: 10.1136/bjo.2005.073650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bain LC, Dudley RA, Gould JB, Lee HC. Factors associated with failure to screen newborns for retinopathy of prematurity. J Pediatr. 2012;161:819–823. doi: 10.1016/j.jpeds.2012.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.van Sorge AJ, Termote JU, Simonsz HJ, Kerkhoff FT, van Rijn LJ, Lemmens WA, Schalij-Delfos NE. Outcome and quality of screening in a nationwide survey on retinopathy of prematurity in The Netherlands. Br J Ophthalmol. 2014;98:1056–1060. doi: 10.1136/bjophthalmol-2013-304493. [DOI] [PubMed] [Google Scholar]
- 22.Bassiouny MR. Risk factors associated with retinopathy of prematurity: a study from Oman. J Trop Pediatr. 1996;42:355–358. doi: 10.1093/tropej/42.6.355. [DOI] [PubMed] [Google Scholar]
- 23.Akkoyun I, Oto S, Yilmaz G, Gurakan B, Tarcan A, Anuk D, Akgun S, Akova YA. Risk factors in the development of mild and severe retinopathy of prematurity. J AAPOS. 2006;10:449–453. doi: 10.1016/j.jaapos.2006.05.007. [DOI] [PubMed] [Google Scholar]
- 24.Chaudhari S, Patwardhan V, Vaidya U, Kadam S, Kamat A. Retinopathy of prematurity in a tertiary care center--incidence, risk factors and outcome. Indian Pediatr. 2009;46:219–224. [PubMed] [Google Scholar]
- 25.Shah VA, Yeo CL, Ling YL, Ho LY. Incidence, risk factors of retinopathy of prematurity among very low birth weight infants in Singapore. Ann Acad Med Singapore. 2005;34:169–178. [PubMed] [Google Scholar]
- 26.Molloy CS, Anderson PJ, Anderson VA, Doyle LW. The long-term outcome of extremely preterm (<28 weeks' gestational age) infants with and without severe retinopathy of prematurity. J Neuropsychol. 2015 doi: 10.1111/jnp.12069. [DOI] [PubMed] [Google Scholar]
- 27.VanderVeen DK, Bremer DL, Fellows RR, Hardy RJ, Neely DE, Palmer EA, Rogers DL, Tung B, Good WV Early Treatment for Retinopathy of Prematurity Cooperative Group. Prevalence and course of strabismus through age 6 years in participants of the early treatment for retinopathy of prematurity randomized trial. J AAPOS. 2011;15:536–540. doi: 10.1016/j.jaapos.2011.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Saldir M, Sarici SU, Mutlu FM, Mocan C, Altinsoy HI, Ozcan O. An analysis of neonatal risk factors associated with the development of ophthalmologic problems at infancy and early childhood: a study of premature infants born at or before 32 weeks of gestation. J Pediatr Ophthalmol Strabismus. 2010;47:331–337. doi: 10.3928/01913913-20100218-08. [DOI] [PubMed] [Google Scholar]
- 29.Hoogerwerf A, Schalij-Delfos NE, van Schooneveld MJ, Termote JU. Incidence of retinopathy of prematurity over the last decade in the Central Netherlands. Neonatology. 2010;98:137–142. doi: 10.1159/000280386. [DOI] [PubMed] [Google Scholar]
- 30.Allegaert K, Casteels I, Cossey V, Devlieger H. Retinopathy of prematurity: any difference in risk factors between a high and low risk population? Eur J Ophthalmol. 2003;13:784–788. doi: 10.1177/1120672103013009-1009. [DOI] [PubMed] [Google Scholar]
- 31.George I, Mekahli D, Rayyan M, Levtchenko E, Allegaert K. Postnatal trends in creatinemia and its covariates in extremely low birth weight (ELBW) neonates. Pediatr Nephrol. 2011;26:1843–1849. doi: 10.1007/s00467-011-1883-0. [DOI] [PubMed] [Google Scholar]
- 32.Larsson E, Carle-Petrelius B, Cernerud G, Ots L, Wallin A, Holmström G. Incidence of ROP in two consecutive Swedish population based studies. Br J Ophthalmol. 2002;86:1122–1126. doi: 10.1136/bjo.86.10.1122. [DOI] [PMC free article] [PubMed] [Google Scholar]