Abstract
Background
The role of subluxation in staging of the severity of osteoarthritic changes remains unclear. The aim of this study was to evaluate the influence of subluxation of symptomatic osteoarthritic trapeziometacarpal (TMC) joint regarding severity of symptoms, disability, and results of operative treatment in TMC osteoarthritis with total joint arthroplasty.
Methods
We included 172 hands in 137 patients (32 males and 105 females), mean age 59 years (44–74 years), with a combination of radiological signs of TMC osteoarthritis and clinical symptoms in the study. All patients were operated in general anaesthesia where a ball and socket joint implant was used. Disability of the Arm, Shoulder and Hand (DASH) score, visual analog scale, grip strength, and abduction deficiency were recorded and subluxation was measured on computed tomography.
Results
The mean subluxation in males was 5.2 mm (SD 1.2) and in females 5.3 mm (SD 1.3) (p = 0.95). We found a weak positive correlation between grip strength and subluxation both at the preoperative examination and at 3 and 12 months after the operation, but no other correlations with subluxation were found.
Conclusions
This study indicates that radial subluxation may not be an important factor in symptoms and function in patients with symptomatic TMC osteoarthritis without severe scaphotrapezio (ST) joint degeneration. In addition, preoperative subluxation seems not to be important for the result after total joint arthroplasty.
Keywords: Trapeziometacarpal osteoarthritis, Total joint arthroplasty, Subluxation, Radiology, Computed tomography
Introduction
Trapeziometacarpal (TMC) osteoarthritis of the first digit is a common condition [1, 6, 21] often leading to disability and the need of treatment in form of non-steroid anti-inflammatory drugs, splinting, steroid injection, or, in more severe cases, operation such as trapeziectomy or total joint arthroplasty [14, 23]. In the classification of the severity of TMC osteoarthritis, Eaton and Littler in 1973 [11] described a radiological classification system based on changes in joint space, osteophytes, subchondral sclerosis, and subluxation. Later, in 1987, Eaton and Glickel modified the classification system [10] and added degenerative changes in the scaphotrapezio (ST) joint. Subluxation was no longer included in stage II as in the Eaton–Littler version and only contributed to a minor part of stages III and IV. This classification system is now widely used in the radiological staging of TMC osteoarthritis. However, both the Eaton–Littler and the Eaton–Glickel classification systems have been evaluated leading to concerns regarding the reliability in daily use [3, 4, 9, 12, 16, 22].
Generally, there is no direct correlation between radiological findings in TMC osteoarthritis and symptoms and disability of the patient [6, 10, 15, 24], but there seems to be some correlation to hand function, especially in maximal grip strength, writing, handling, or fingering small objects [24]. The role of subluxation in the staging of the severity of osteoarthritic changes, however, still remains unclear. In a study by de Raedt et al. [7], normal TMC joints were compared with osteoarthritic TMC joints by comparing quantitative geometrical measurements in computed tomography (CT) scans of healthy and pathological joints in various stages of osteoarthritis. They found subluxation in the dorsoradial direction and changes in the center of rotation of the symptomatic osteoarthritic TMC joints compared to normal anatomy in the asymptomatic TMC joints. The clinical relevance of these findings is so far unclear and has not been tested in clinical studies.
The aim of this study was to evaluate the influence of subluxation of the symptomatic osteoarthritic TMC joint regarding the severity of symptoms, disability, and the results of operative treatment in TMC osteoarthritis with total joint arthroplasty.
Materials and Methods
Subjects
We prospectively included 172 hands in 137 patients (32 males and 105 females) with a mean age of 59 years (44–74 years) in the period of January 2008 to April 2013 with a combination of radiological signs of TMC osteoarthritis Eaton stage II–IV [10] and clinical symptoms in the study. All patients were referred to our clinic from general practitioners or other hospitals for operative treatment after failure of conservative treatment, and in all patients, plain radiographs had confirmed the clinical diagnosis of TMC osteoarthritis.
Indications for total joint arthroplasty were confirmed osteoarthritis of the TMC joint on plain radiographs plus CT and a history of pain at activity at the TMC joint limiting activities of daily living. Contraindications and exclusion criteria were severe osteoarthritic changes in the scaphoid-trapezoid (ST) joint and/or loss of trapezium height, hyperextension contracture at the metacarpophangeal (MP) joint of the thumb, or known osteoporosis.
Further exclusion criterion from the study was re-operation of any kind in the operated hand during the 12-month observation period.
Operative Procedure
All patients were operated in general anaesthesia using a tourniquet. At the operation, a ball and socket joint implant was used in all patients and the cup was placed in the anatomical center of the trapezium to correct subluxation and restore the normal rotation center of the TMC joint. The implants used were in 62 hands an Elektra cementless stem and cup (Small Bone Innovations Inc., Les Bruyères, France), in 17 hands an Elektra cementless stem combined with a cemented DLC cup (Small Bone Innovations Inc., Les Bruyères, France), in 17 hands a Motec cementless stem and cup (Swemac AB, Linköbing, Sweden), and in 37 hands a cementless Motec stem and a cemented Motec polyethylene cup (Swemac AB, Linköbing, Sweden).
At the operation, the soft tissue tension was balanced with stripping of the capsule around the base of the metacarpal to avoid the effect of a tight capsule after replacing the center of rotation and removing the subluxation. All patients were immobilized in a plaster of Paris splint for 3 weeks after the operation and allowed to do light exercises after removal of the splint. Unlimited use was allowed after 3 months. The patients received no occupational therapy.
Measurement Parameters
As part of the preoperative evaluation, a supplementary CT scan was performed in all patients and a Disability of the Arm, Shoulder and Hand (DASH) score was recorded using a validated Danish translation [13] together with measurements of grip strength in kilograms with a Jamar hand dynamometer, thumb abduction deficiency (the distance between the tip of finger 1 and 2 in full abduction compared to the contralateral hand), and recording of pain at rest and at activity using a visual analog scale (VAS).
All measurements were performed by an independent observer (outpatient clinic nurse) and were repeated at 3 months after the operation and again after 12 months.
The measurements of the subluxation were performed by one observer based on CT scans and calculated as the mean of two measurements made on two different occasions with at least 4 weeks in between.
The subluxation was defined as the radial deviation of the long axis of the first metacarpal compared to the axis of the trapezium. The measurement (mm) was done on CT as follows: The coronal plan in which the TMC joint of the thumb was best depicted was selected. Two right angles were drawn to represent the axes of the bones, and the distance (a) between the axes was measured in level of the joint (Fig. 1). The reliability of the measurements of the subluxation was measured using all scans (172 hands), and we found the correlation between measurements 1 and 2 good with a correlation coefficient of 0.66.
Fig. 1.
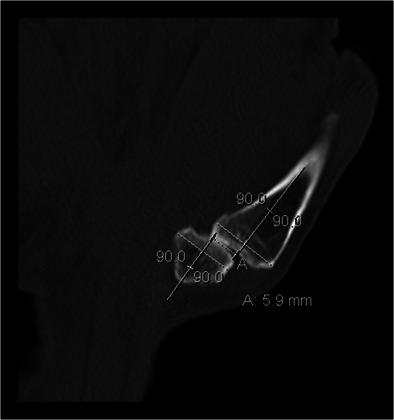
The subluxation (a) measured as the radial deviation of the long axis of the first metacarp compared to the axis of the trapezium
Pearson’s correlation coefficient was used to test for correlation between subluxation and the measured variables in each patient.
Student’s t test was used for comparison of mean values.
Results
Nineteen hands were excluded from the clinical follow-up part of the study due to cancellation of the planned operative treatment with total joint arthroplasty by any reason (treatment with trapeziectomy instead or regression of symptoms), 15 hands were excluded due to some kind of revision surgery (luxation, fracture, implant loosening, or infection) during the 12-month study period, and 5 patients were excluded due to missing data leaving 133 hands in 114 patients in the study.
There was no difference (p = 0.75) concerning the subluxation in the 133 included hands with a mean of 5.3 mm (SD 1.4) compared to all scans (172 hands) with a mean of 5.3 mm (SD 1.5). Also, we found no difference in subluxation comparing the 133 hands without reoperation (mean subluxation 5.3 mm (SD 1.4)) with the 15 hands with reoperation (mean subluxation 5.1 mm (SD 1.6), p = 0.79). The mean subluxation in males was 5.2 mm (SD 1.2) and in females 5.3 mm (SD 1.3) (p = 0.95).
Grip strength and DAS score improved after the operation, and VAS both at rest and at activity was reduced (Table 1).
Table 1.
Grip strength, pain at rest/activity (VAS (0–10)), and DASH score in 133 hands before and after trapeziometacarpal total joint arthoplasty
| Preoperative | 3 months | 12 months | |
|---|---|---|---|
| Grip strength (mean) | 22.6 kg (SD 13.6) | 22.4 kg (SD 11.3) | 27.8 kg (SD 12.1) |
| VAS at rest (mean) | 3.1 (SD 2.2) | 0.8 (SD 1.6) | 0.6 (SD 1.3) |
| VAS at activity (mean) | 7.8 (SD 1.8) | 2.5 (SD 2.4) | 1.8 (SD 2.4) |
| DASH score (mean) | 39.1 (SD 17.0) | 21.1 (SD 18.0) | 13.6 (SD17.1) |
SD standard deviation, VAS visual analog scale, DASH Disability of the Arm, Shoulder and Hand score
We found no correlation between subluxation and patient age, DASH score, pain VAS score at rest, pain VAS score with activity, or restriction in abduction preoperatively or at 3 and 12 months after total joint arthroplasty (Table 2). The only positive findings were a weak positive correlation between grip strength and subluxation both at the preoperative examination and at 3 and 12 months after the operation. Including only the first operated hand in bilateral cases or only including unilateral cases did not change the results (Table 2).
Table 2.
Pearson’s correlation coefficient in test for correlation between subluxation and the measured variables preoperatively and 3 and 12 months after total joint arthroplasty
| Variable | Hands (n = 133) | Patientsa (n = 114) | Unilateral cases (n = 95) |
|---|---|---|---|
| Age | −0.05 | −0.07 | −0.03 |
| Preoperative | |||
| Grip strength | 0.29 | 0.21 | 0.22 |
| Grip strengthb | 0.07 | 0.07 | 0.08 |
| Restriction abduction | 0.05 | 0.05 | 0.08 |
| VAS at rest | 0.01 | −1.13 | 0.06 |
| VAS at activity | −0.04 | −0.06 | 0.05 |
| DASH | −0.06 | −0.02 | −0.06 |
| 3 months | |||
| Grip strength | 0.22 | 0.24 | 0.21 |
| VAS at rest | −0.13 | −0.13 | −0.07 |
| VAS at activity | 0.10 | −0.013 | −0.14 |
| DASH | 0.00 | −0.05 | −0.14 |
| 12 months | |||
| Grip strength | 0.30 | 0.32 | 0.34 |
| Restriction abduction | −0.05 | 0.07 | 0.06 |
| VAS at rest | −0.03 | −0.08 | −0.09 |
| VAS at activity | 0.10 | 0.07 | 0.03 |
| DASH | −0.03 | −0.09 | −0.19 |
VAS visual analog scale, DASH Disability of the Arm, Shoulder and Hand score
aOnly first operated hand in bilateral cases
bGrip strength of the operated hand divided with the grip strength of the opposite hand
Discussion
The most important finding in this study is that subluxation of the TMC joint only had very little influence on the preoperative symptoms and function in a group of patients with TMC osteoarthritis without fixed MP joint hyperextension contracture and severe degenerative changes in the ST joint. Also, it seems not to influence the result after total joint arthroplasty with a ball and socket joint replacement, where the cup is placed in the anatomical center of the trapezium and a soft tissue release is made to avoid uneven capsular tension due to the preoperative subluxation.
The study may be flawed by using a nonvalidated method to measure the abduction of the thumb, and comparing abduction with the opposite thumb abduction, as the opposite hand may have similar degenerative changes. However, the results were the same if looking at unilateral cases, where the opposite hand had not been treated due to lack of symptoms. Also, based on the very low correlation values, we believe that an alternative measurement method of thumb abduction would not have lead to another result.
In the study by de Raedt et al. [7], normal TMC joints were compared with osteoarthritic TMC joints in a three-dimensional model, and they found dorsoradial subluxation and changes in the center of rotation of the symptomatic osteoarthritic TMC joints. In our study, we did not use a three-dimensional model for assessment of the subluxation, as this method is not available for normal daily use. Instead, we focused on radial subluxation alone, but the results of our study may have been different if using three-dimensional assessment of the subluxation instead. The lack of an indication of a positive correlation between symptoms and subluxation in the present study with very low correlation coefficients in a relatively large number of patients, however, gives a strong indication of a missing correlation between subluxation and symptoms.
The symptoms from TMC osteoarthritis vary and are influenced by several other factors [2]. We excluded patients with fixed hyperextension contracture of the MP joint because fixed hyperextension contracture of the MP joint remains a challenge regardless of using total joint arthroplasty or trapeziectomy [8, 17] and often needs supplementary surgery to the MP joint [18–20]. This condition is often combined with severe subluxation of the TMC joint, and the results of our study may have been different if this patient category had been included. Also, we excluded patients with severe ST joint degeneration as these patients were not suitable for treatment with total joint arthroplasty of the TMC joint limiting the generalization of the results of our study.
Spaans et al. [22] evaluated the Eaton–Littler classification and found only a moderate interobserver reliability using radiologists and hand surgeons as observers. Kubik and Lubahn [16] evaluated the Eaton–Glickel classification using hand surgeons and orthopaedic residents and found only a moderate intraobserver and interobserver reliability in hand surgeons. Dela Rosa et al. [9] also evaluated the Eaton–Glickel classification and used only highly experienced hand surgeons but found that the overall interobserver reliability was only moderate. Hansen et al. [12] compared the reliability of the Eaton–Glickel classification using plain radiographs or using CT and found that adding CT scans improved the intraobserver reliability of the classification, but still interobserver classification reliability was a problem, especially in the evaluation of the degenerative changes in the ST joint. Choa et al. [4] used weighed Kappa analysis and improved the reliability, but still the Eaton–Littler and Eaton–Glickel classifications seem to be problematic in communicating the staging of the degenerative disease [3], especially as they are purely radiological classifications and do not include clinical information such as deformity of the MP joint. The classification system suggested by Comtet et al. [5] is more focused on classifying the patients into possible treatments compared to the Eaton–Littler or Eaton–Glickel classification.
There seems to be a need of a more simple and reliable classification system, if the severity of the degenerative changes seen on plain radiographs or CT scans should be used in the assessment of the patient and staging of the osteoarthritic joint changes prior to the specific choice of treatment. This study indicates that radial subluxation may not be an important factor in symptoms and function in patients with TMC osteoarthritis without severe ST joint degeneration. In addition, preoperative subluxation seems not to be important for the result after total joint arthroplasty. The ideal classification system of TMC osteoarthritis should precisely stage the preoperative symptoms and predict the outcome of surgery. We suggest that future studies should aim at refining the staging systems combining clinical symptoms and radiological findings and that radial subluxation based on this study may not need to play an important role in the classification of TMC joint degenerative changes.
Acknowledgments
Conflict of interest
Solveig K. A. Larsen declares that she has no conflict of interests.
Ann Mai Østergaard declares that she has no conflict of interests.
Torben B. Hansen declares that he has no conflict of interests.
Statement of Human and Animal Rights
All procedures were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5).
Statement of Informed Consent
Informed consent was obtained from all patients for being included in the study.
Study approval and registration
The study needed no approval from The Regional Committee of Biomedical Research Ethics as the data was collected, as part of our normal pre- and postoperative clinical pathway, but the study is part of an outcome study of the results after total joint arthroplasty of the TMC joint registered in Clinicaltrials.gov (NCT01554748).
References
- 1.Armstrong AL, Hunter JB, Davis TR. The prevalence of degenerative arthritis of the base of the thumb in post-menopausal women. J Hand Surg. 1994;19:340–341. doi: 10.1016/0266-7681(94)90085-X. [DOI] [PubMed] [Google Scholar]
- 2.Becker SJ, Makarawung DJ, Spit SA, et al. Disability in patients with trapeziometacarpal joint arthrosis: incidental versus presenting diagnosis. J Hand Surg. 2014;39:2009–2015. doi: 10.1016/j.jhsa.2014.07.009. [DOI] [PubMed] [Google Scholar]
- 3.Berger AJ, Momeni A, Ladd AL. Intra- and interobserver reliability of the Eaton classification for trapeziometacarpal arthritis: a systematic review. Clin Orthop Relat Res. 2014;472:1155–1159. doi: 10.1007/s11999-013-3208-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Choa RM, Giele HP. Inter- and intrarater reliability of osteoarthritis classification at the trapeziometacarpal Joint. J Hand Surg. 2014. [DOI] [PubMed]
- 5.Comtet JJ, Gazarian A, Fockens W. Definition and classification of basal joint osteoarthritis. A critical analysis and proposals. Treatment options. Chir Main. 2001;20:5–10. doi: 10.1016/S1297-3203(01)00009-9. [DOI] [PubMed] [Google Scholar]
- 6.Dahaghin S, Bierma-Zeinstra SM, Ginai AZ, et al. Prevalence and pattern of radiographic hand osteoarthritis and association with pain and disability (the Rotterdam study) Ann Rheum Dis. 2005;64:682–687. doi: 10.1136/ard.2004.023564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.de Raedt S, Stilling M, van de Giessen M, et al. A three-dimensional analysis of osteoarthritic changes in the thumb carpometacarpal joint. J Hand Surg, Eur. 2013;38:851–859. doi: 10.1177/1753193412466764. [DOI] [PubMed] [Google Scholar]
- 8.Degreef I, De Smet L. Predictors of outcome in surgical treatment for basal joint osteoarthritis of the thumb. Clin Rheumatol. 2006;25:140–142. doi: 10.1007/s10067-005-1108-7. [DOI] [PubMed] [Google Scholar]
- 9.Dela Rosa TL, Vance MC, Stern PJ. Radiographic optimization of the Eaton classification. J Hand Surg. 2004;29:173–177. doi: 10.1016/j.jhsb.2003.09.003. [DOI] [PubMed] [Google Scholar]
- 10.Eaton RG, Glickel SZ. Trapeziometacarpal osteoarthritis. Staging as a rationale for treatment. Hand Clin. 1987;3:455–471. [PubMed] [Google Scholar]
- 11.Eaton RG, Littler JW. Ligament reconstruction for the painful thumb carpometacarpal joint. J Bone Joint Surg Am. 1973;55:1655–1666. [PubMed] [Google Scholar]
- 12.Hansen TB, Sorensen OG, Kirkeby L, et al. Computed tomography improves intra-observer reliability, but not the inter-observer reliability of the Eaton-Glickel classification. J Hand Surg, Eur. 2013;38:187–191. doi: 10.1177/1753193412443502. [DOI] [PubMed] [Google Scholar]
- 13.Herup A, Merser S, Boeckstyns M. Validation of questionnaire for conditions of the upper extremity. Ugeskr Laeger. 2010;172:3333–3336. [PubMed] [Google Scholar]
- 14.Hochberg MC, Altman RD, April KT, et al. American College of R. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res. 2012;64:465–474. doi: 10.1002/acr.21596. [DOI] [PubMed] [Google Scholar]
- 15.Jones G, Cooley HM, Bellamy N. A cross-sectional study of the association between Heberden’s nodes, radiographic osteoarthritis of the hands, grip strength, disability and pain. Osteoarthr Cartil / OARS, Osteoarthr Res Soc. 2001;9:606–611. doi: 10.1053/joca.2001.0460. [DOI] [PubMed] [Google Scholar]
- 16.Kubik NJ, 3rd, Lubahn JD. Intrarater and interrater reliability of the Eaton classification of basal joint arthritis. J Hand Surg. 2002;27:882–885. doi: 10.1053/jhsu.2002.35310. [DOI] [PubMed] [Google Scholar]
- 17.Moineau G, Richou J, Liot M, et al. Prognostic factors for the recovery of hand function following trapeziectomy with ligamentoplasty stabilisation. Orthop Traumatol, Surg Res: OTSR. 2009;95:352–358. doi: 10.1016/j.otsr.2009.03.015. [DOI] [PubMed] [Google Scholar]
- 18.Poulter RJ, Davis TR. Management of hyperextension of the metacarpophalangeal joint in association with trapeziometacarpal joint osteoarthritis. J Hand Surg, Eur. 2011;36:280–284. doi: 10.1177/1753193411400359. [DOI] [PubMed] [Google Scholar]
- 19.Qadir R, Duncan SF, Smith AA, et al. Volar capsulodesis of the thumb metacarpophalangeal joint at the time of Basal joint arthroplasty: a surgical technique using suture anchors. J Hand Surg. 2014;39:1999–2004. doi: 10.1016/j.jhsa.2014.07.045. [DOI] [PubMed] [Google Scholar]
- 20.Raskolnikov D, White NJ, Swart E, et al. Volar plate capsulodesis for metacarpophalangeal hyperextension with basal joint arthritis. Am J Orthop. 2014;43:354–358. [PubMed] [Google Scholar]
- 21.Sodha S, Ring D, Zurakowski D, et al. Prevalence of osteoarthrosis of the trapeziometacarpal joint. J Bone Joint Surg Am. 2005;87:2614–2618. doi: 10.2106/JBJS.E.00104. [DOI] [PubMed] [Google Scholar]
- 22.Spaans AJ, van Laarhoven CM, Schuurman AH, et al. Interobserver agreement of the Eaton-Littler classification system and treatment strategy of thumb carpometacarpal joint osteoarthritis. J Hand Surg. 2011;36:1467–1470. doi: 10.1016/j.jhsa.2011.06.017. [DOI] [PubMed] [Google Scholar]
- 23.Vermeulen GM, Slijper H, Feitz R, et al. Surgical management of primary thumb carpometacarpal osteoarthritis: a systematic review. J Hand Surg. 2011;36:157–169. doi: 10.1016/j.jhsa.2010.10.028. [DOI] [PubMed] [Google Scholar]
- 24.Zhang Y, Niu J, Kelly-Hayes M, et al. Prevalence of symptomatic hand osteoarthritis and its impact on functional status among the elderly: the Framingham Study. Am J Epidemiol. 2002;156:1021–1027. doi: 10.1093/aje/kwf141. [DOI] [PubMed] [Google Scholar]


