Abstract
Introduction
Rupture of the extensor pollicis longus (EPL) tendon has been reported in the setting of distal radius fracture, chronic inflammatory arthritis, following steroid injection, and with excessive or repetitive activities. Truly, spontaneous EPL rupture, without an identifiable predisposing factor, has rarely been reported.
Methods
We present a retrospective case series of eight patients with spontaneous EPL rupture who were treated in our institution.
Results
The majority of the cases were female (75 %, n = 6), and the nondominant (75 %, n = 6) hand was most commonly involved. No identifiable predisposing factor could be identified in four patients. While four patients reported a history of a fall, radiographs failed to demonstrate skeletal abnormality in all four cases. No additional pathology could be identified at the time of surgery. Patients were treated using tendon transfer (n = 7) or interpositional graft (n = 1). There has been no case of clinical recurrence in the mean of 74.8 months (range 23–140 months) follow-up period.
Conclusion
The EPL tendon is at risk for spontaneous rupture even in the absence of identifiable predisposing risk factor. Rather than pure mechanical irritation, vascular and metabolic factors may also play a substantial role in the etiology of this uncommon diagnosis.
Keywords: Spontaneous, EPL, Tendon rupture, Tendon transfer
Introduction
Rupture of the extensor pollicis longus (EPL) tendon is uncommon but has been reported in the literature following several precipitating factors. Nondisplaced fracture of the distal radius is a well-established risk factor with an incidence of EPL rupture of 0.2–5 % [22]. Other predisposing factors that have been reported in the literature include chronic inflammatory conditions such as rheumatoid arthritis [2, 4, 8, 14, 20, 24], systemic or local steroid injections, and repetitive or excessive abnormal motion of the wrist [6, 16]. Several factors are thought to contribute to EPL rupture in these clinical settings. These fall grossly into mechanical and vascular categories [4, 8, 9, 13]. The EPL is particularly susceptible to mechanical irritation due to its close anatomic relationship to the dorsal radius and particularly the Lister tubercle [9, 13]. Cortical irregularities from distal radius fractures or osteophytes easily abrade the tendon, causing gradual attrition and ultimately rupture. An impaired vascular contribution to EPL rupture has also been supported by microcirculatory anatomic studies [8, 12]. In this model, we showed that a watershed zone with limited blood supply leaves the tendon at risk for ischemia and resultant tendon degeneration.
Spontaneous EPL rupture without an identifiable predisposing factor has rarely been reported [22]. In the present study, we report a series of eight such cases in which spontaneous rupture of the EPL was successfully managed without recurrence. These cases challenge our current concepts of the relative contribution of mechanical and vascular factors in the etiology of EPL rupture.
Materials and Methods
Between August 2003 and December 2012, eight patients (six women, two men) were diagnosed with and treated for spontaneous rupture of the EPL in the Plastic Surgery Department of Chang Gung Memorial Hospital. We performed a retrospective chart review to record demographic data including patient age, sex, occupation, and hand dominance. History of trauma, steroid injection symptoms, or diagnosis of inflammatory arthritis were also recorded. All radiographic data were reviewed by two radiologists. The patients were contacted by the latest clinical follow-up to determine if there had been any recurrence of preoperative symptoms or further surgical management of the operative hand.
After clinical confirmation of the diagnosis of EPL rupture by physical examination and the proximal EPL stump might be contractured, our preferred surgical management consists of a standard extensor indicis proprius (EIP) to EPL transfer using a Pulvertaft weave technique. When variants of the extensor digitorum communis (EDC) of the index finger and EIP were noted, the defect was <2 cm, and both of the disrupted stumps were out of the tunnel of the extensor retinaculum, our next preferred reconstruction utilizes a palmaris longus (PL) interposition graft. Debrided tendon edges were sent for pathological analysis.
After surgery, the patient’s operated wrist was immobilized in a short-arm splint with the wrist in a neutral position and the thumb in abduction and extension for 4–6 weeks. Gentle range-of-motion exercises were then started with intermittent splint protection under the supervision of a physical therapist. Night-time splint protection was applied for the following 2 weeks. At 6 weeks postoperatively, the splint was completely removed.
Results
Table 1 summarizes the patient demographic data, operative findings, management, and clinical follow-up. Six patients presented with EPL rupture of their nondominant hand. Only one patient had an occupation that routinely involved heavy labor (police officer), four patients were housewife, one patient was a student, and the other two were businessmen. The average patient age was 47 years (range, 24–66 years). In the cohort of eight patients, four patients had no identifiable trauma, preceding wrist pain, repetitive activity, or history of injection around the wrist. The other four patients reported a recent history of falling onto an outstretched hand. However, in all four cases, radiographic evaluation of the affected wrist was interpreted as without fracture or other abnormality by two radiologists. In cases in which a history of trauma was present (n = 4), EPL rupture was diagnosed at an average of 48 days after trauma (range, 10–90 days).
Table 1.
Summary of clinical cases
| Patient | Age | Sex | Occupation | Dominant hand injury? | History | Time to rupture | Operative findings | Surgical management | Follow-up (months) | Latest ROM extension | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| IPJ | MPJ | ||||||||||
| 1 | 61 | F | Housewife | No | Fall, no radiographic evidence of fracture | 10 days | Retinaculum intact. Degenerative and inflammatory tendon ends | EIP to EPL transfer | 136 | +10° | 0° |
| 2 | 47 | F | Housewife | No | Fall, no radiographic evidence of fracture | 3 months | Retinaculum intact. Tenosynovitis and degenerative tendon ends | EIP to EPL transfer | 57 | +10° | 0° |
| 3 | 24 | F | Student | No | Denied preceding pain, injury or injection | – | Retinaculum intact. Degenerative and inflammatory tendon ends | EIP to EPL transfer | 140 | +10° | 0° |
| 4 | 49 | M | Businessman | No | Fall, no radiographic evidence of fracture | 1 month | Retinaculum intact. Degenerative and inflammatory tendon ends | EIP to EPL transfer | 24 | +10° | 0° |
| 5 | 43 | F | Businessman | Yes | Fall, no radiographic evidence of fracture | 2 months | Retinaculum intact. Degenerative and inflammatory tendon ends | PL interposition graft | 133 | 0° | 0° |
| 6 | 66 | F | Housewife | No | Denied preceding pain, injury, or injection | – | Retinaculum intact. Degenerative and inflammatory tendon ends | EIP to EPL transfer | 23 | 0° | 0° |
| 7 | 29 | M | Police officer | Yes | Denied preceding pain, injury, or injection | – | Retinaculum intact. Degenerative and inflammatory tendon ends | EDC index to EPL transfera | 30 | 0° | 0° |
| 8 | 56 | F | Housewife | No | Denied preceding pain, injury, or injection. Radiograph with prominent Lister tubercle | – | Retinaculum and synovial sheath intact. Degenerated tendon edges | EIP to EPL transfer | 56 | 0° | 0° |
EPL extensor pollicis longus, EIP extensor indicis proprius, PL palmaris longus, EDC extensor digitorum communis
aSecond MCPJ extension lag < 10
Operative findings revealed complete disruption of the EPL tendon around the Lister tubercle with an intact extensor retinaculum in all cases. No obvious mechanical irritants such as cortical disruption or osteophytes were found in any case. The typical clinical appearance included varying degrees of synovitis surrounding the frayed tendon ends of the EPL. In one patient, substantial invasive synovitis was present. Six patients underwent an EIP to EPL transfer, one patient underwent a PL interpositional graft, and one patient underwent extensor digitorum communis index to EPL transfer. The pathological diagnosis in all cases revealed fibrosis and signs of chronic inflammation. Recurrence was assessed at the most recent clinic follow-up at an average of 74.8 months (range, 23–140 months) postoperatively. At that point, all eight patients had an extensor lag <10° with unrestricted thumb interphalangeal joint motion.
Case Report
Patient 4
A 49-year-old right-handed man presented with a history of falling onto an outstretched hand 4 weeks prior to noting onset of thumb extension restrictions. He is a businessman who had no occupational need to repetitively or excessively use his wrist. He had no associated pain and no preceding symptoms to suggest tendon irritation. A physical examination revealed that he could not actively extend the left interphalangeal joint of his thumb (Fig. 1). Radiographic findings were normal (Fig. 2). During the operation, the extensor retinaculum was found to be intact. The proximal and distal portions of the ruptured EPL tendon were found near the Lister tubercle. There was no evidence of a bony cortical irregularity on the dorsum of the wrist or carpus. Although the retinaculum was intact, distal EPL stump curling and the appearance of degenerative and inflammatory changes were noted (Fig. 3). To reconstruct the EPL tendon, the EIP tendon was identified and harvested within the surgical incision. The EIP was transected distally and interwoven with the distal stump of the EPL tendon using the Pulvertaft technique at the level of the carpometacarpal joint (Fig. 3). Tension was established by suturing the EIP tendon to the distal portion of the EPL tendon with the thumb IP and MCP joints held in 0° of extension and with the wrist in a neutral position. The patient was immobilized postoperatively in a short-arm splint with the wrist in a neutral position and the thumb in abduction and extension for 6 weeks. Gentle range-of-motion exercises were then started, and the splint use was gradually weaned. At 4 months postoperatively, he showed the ability to extend the interphalangeal joint of the thumb without an extension lag (Fig. 1).
Fig. 1.
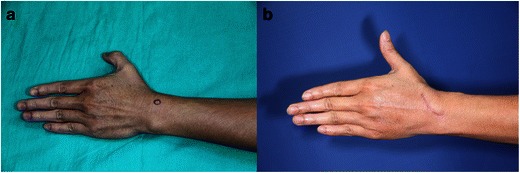
a Preoperative clinical photograph of patient 4 who presented with an inability to extend the interphalangeal joint of the left thumb. b Postoperative clinical photograph showing full extension at the interphalangeal joint of left thumb
Fig. 2.

Patient 4. Radiograph of the right wrist was interpreted as normal
Fig. 3.

Patient 4. Intra-operative findings. a Distal EPL stump with curled appearance of degenerative and inflammatory change (black arrow). EIP was identified (black arrowhead). b EIP was transferred to EPL tendon using the Pulvertaft technique at the level of the carpometacarpal (CMC) joint
Patient 8
A 56-year-old right hand-dominant woman visited our clinic with the chief complaint of the inability to move her left thumb. She was a housewife. She denied a history of trauma, symptoms consistent with rheumatoid or other inflammatory arthritis, or steroid injection. Physical examination revealed loss of full extension of the interphalangeal (IP) joint in the left thumb but preserved IP flexion (Fig. 4). The patient was not able to recall any fall or trauma either recently or remotely. At the time of surgery, EPL tendon was disrupted but synovial sheath was in continuity (Fig. 4). Radiography revealed no fracture, but prominent Lister tubercle was noted. There was no evidence of rheumatoid arthritis, distal radius, or carpal fracture nor was significant tenosynovitis or synovitis noted. Additionally, there was no evidence of a bony cortical irregularity on the dorsum of the wrist or carpus. This appearance lacks substantial inflammatory changes and with an intact synovial sheath suggests the chronicity of a pathological process that may have been impacted by the Lister tubercle. To reconstruct the EPL tendon, we excised the disrupted end and transferred the EIP to the EPL distal stump using the Pulvertaft technique. The patient wore a short-arm splint for 6 weeks and followed the same rehabilitation protocol as patient 4. At 56 months postoperatively in clinical follow-up, she demonstrated no limitation of extending the interphalangeal joint of the thumb and reported good daily activity.
Fig. 4.

a Preoperative clinical photograph of patient 8 who presented with an inability to extend the interphalangeal joint of the left thumb. b Intra-operative finding revealed EPL was disrupted with synovial sheath in continuity
Discussion
Rupture of the EPL tendon is uncommon, but when reported, a predisposing factor such as distal radius fracture [12], blunt trauma [4], repetitive and excessive abnormal motion [6, 16], inflammatory disease [24], and systemic or local steroid injection [4] can generally be identified. In this study, we presented eight cases in which none of these classical precipitating factors could be identified. Distal radius fracture is the most well-established risk factor associated with EPL rupture. In such cases, direct mechanical shearing force from the disrupted cortex of the dorsal radius is thought to be the main cause [9]. Interestingly, EPL rupture has been reported more commonly following nondisplaced, rather than displaced, distal radius fracture [10, 12, 17, 20, 22, 23]. In this setting, the extensor retinaculum is generally not disrupted and is thought to contribute to mechanical irritation as it maintains the EPL closely approximated to the dorsum of the radius and Lister tubercle. These mechanical factors are thought to be compounded by the EPL tendon’s relatively poor blood supply in the region of the Lister tubercle. Microangiographic studies have revealed that the EPL has a distal and proximal blood supply with a relatively avascular zone in the area of the Lister tubercle [4, 8]. When pressure increases in the surrounding tendon sheath due to inflammation following distal radius fracture or other trauma, the direct blood supply may be compromised, leaving only diffusion through the synovial fluid to supply adequate nutrition. This is thought to cause ischemia and delayed tendon rupture. Additional mechanisms were recently described. One cadaveric study suggested that a direct crush injury to the EPL can occur by contact between the Lister tubercle and the base of the third metacarpal bone in a simulated fall onto an outstretched hand [9]. Additionally, case reports of occupation and sports-associated spontaneous EPL rupture exist [6, 11, 16].
In our study, four patients had a history of falling onto an outstretched wrist. While no fracture was identified on plain radiographs, it is possible that an occult distal radius fracture was present. Additionally, although patient 8 could not recall a fall or trauma, we suspect a remote history of trauma that led to a prominent Lister tubercle. However, a prominent Lister tubercle was not found on the radiographs of the other three patients with a falling history by either radiologist. To identify any occult fracture, we tried to arrange CT scans for all patients; however, we faced difficulty convincing patients of the need for it when the radiographic findings were normal. Moreover, the treatment remains unchanged despite positive findings on CT scans. With regard to the lack of CT scans, it is possible that occult distal radius fracture was present in patients with history of trauma.
When a distal radius fracture is complicated by an EPL rupture, the timing is generally somewhat delayed. A retrospective case–control study by Roth et al. [22] found the average time from injury to EPL rupture in three cases to be 46 days, while others have reported rupture anywhere from 7 days to 18 months [10, 17, 23]. These findings grossly correlate with ours. In the four patients with a history of fall, the average time to EPL rupture was 48 days with a range of 10 days to 3 months. For the patients in whom no predisposing factor could be identified, explanations that do not include mechanical irritation due to fracture must be explored. No substantial occupation-related repetitive or excessive activity of the wrist could be identified that may have precipitated the EPL rupture (Table 1). Further evidence supporting that excessive use did not precipitate EPL rupture is the fact that the majority of patients (75 %) sustained a rupture in their nondominant hand. In these cases, vascular rather than mechanical contributions may explain the tendon rupture.
Six of eight (75 %) patients in our cohort were women. Studies have suggested that EPL rupture following distal radius fracture is more common in women [6, 14, 16, 22, 24, 25]. In the Roth study mentioned above, three of three cases of EPL rupture following distal radius fracture occurred in women. One classical reference reported the female predominance of EPL rupture after distal radius fracture of 60 % [15]. Stenosing tenosynovitis, also known as de Quervain’s disease, is a common tendonopathy with a known predilection for women, particularly those who are pregnant or lactating. In de Quervain’s disease, in addition to repetitive activities, hormonal factors are thought to contribute to the increased prevalence in women [3]. This association has yet to be studied with regard to EPL rupture, but it may be worth exploration considering idiopathic cases such as the ones presented here. Furthermore, rupture of both the abductor pollicis longus and extensor pollicis brevis has been reported following distal radius fracture and conservative management of de Quervain’s disease [1, 26]. Given the related anatomy and risk factors, it is possible that these two processes (de Quervain’s disease and spontaneous EPL rupture) share a common pathological pathway. Unfortunately, in this is a retrospective study, we failed to conduct hormone levels as an endpoint. For the above reasons, we suggest complete hormone study for spontaneous EPL rupture in female patient in the future.
Although not statistically significant, our clinical experience led us to suspect that the intact extensor retinaculum contributes substantially to mechanical attrition and circulatory compromise of the EPL tendon, because we found the thick synovial sheath with frayed tendon ends along with chronic inflammatory changes on path reports which was compatible to the literatures of EPL synovitis around the Lister tubercle. However, the definite etiology of synovitis in our patient was still unknown. Knowing both mechanical irritation and synovitis within the intact extensor retinaculum can cause symptoms, we have heightened awareness of dorsal-side wrist symptoms following even minor trauma or repetitive activity. If physical examination elicits pain with direct palpation over the course of the EPL tendon or with thumb motion, we routinely obtain an ultrasound to identify inflammation in the third extensor compartment. When inflammation is found, we recommend prophylactic surgical release of the third compartment similar to the management of recalcitrant de Quervain’s disease. The same recommendation is reported by Navaratnam et al. [19].
By reviewing the treatment of spontaneous EPL rupture, the surgical options tried have included direct repair, tendon transfer, and tendon grafting. Direct end-to-end repair is difficult, because the rupture end is usually fragile and thin. After removing unhealthy part, there is always a gap between proximal and distal end. Tendon transfer or tendon grafting has become the standard procedure. As for tendon transfer, EIP transfer is the standard technique for spontaneous EPL rupture. It is important to note that anatomic variations in the EIP tendon have been reported and we encountered one such case in this series. Patient 7 underwent an EDC index transfer due to such an anatomic variation. In normal anatomy, the EIP arises from the posterior surface of the distal third of the ulna and the adjacent interosseous membrane. It passes distally within the fourth dorsal compartment deep to the EDC tendons and inserts into the dorsal expansion of the index finger on the ulnar side of the EDC. In this case, the EIP was on the radial side of the insertion of EDC and the EDC of the index was used for transfer to the EPL distal stump. Variations of the extensor tendons of the hand are common. In a study of 263 cadaveric specimens, a 4 % incidence of anomalous EIP muscles was found [5]. Other anatomic variants of the EIP include absence, duplication, or with anomalous insertions to the thumb, the ring finger, or, more often, the middle finger [25]. The incidence of EIP absence was reported around 1–4 % in a literature review [7, 18, 27]. In the setting of anomalous anatomy that precludes EIP transfer, we may use an PL tendon transfer. It is important to note that there were no cases of recurrence in this study. During surgical management, the extensor retinaculum of the third compartment is opened and the EPL is transposed. This alleviates the mechanical irritation from the tight retinaculum and the Lister tubercle.
As a small retrospective case series, this study is inherently limited. We are unable to report an incidence of spontaneous EPL rupture or draw conclusions about what additional risk factors may be present. Nonetheless, only few reports of spontaneous EPL rupture without a classical predisposing factor have previously been described in a case series such as this one [21]. Several risk factors and possible mechanisms for EPL rupture have been described. However, our study suggests that we should continue following the hypothesis of the relative contributions that mechanical, vascular, and potentially metabolic or hormonal factors have in this process.
Conclusion
Spontaneous rupture of the EPL tendon has generally been reported in the setting of predisposing risk factors. The cases presented in this study demonstrate that the EPL may be at risk for rupture even in the absence of classic risk factors.
Acknowledgments
Conflict of Interest
Ching-Hsuan Hu has no conflicts of interest to disclose.
Duretti Fufa has no conflicts of interest to disclose.
Chung-Chen Hsu has no conflicts of interest to disclose.
Yu-Te Lin has no conflicts of interest to disclose.
Chih-Hung Lin has no conflicts of interest to disclose.
Statement of Human and Animal Rights
This article does not contain any studies with human or animal subjects.
Statement of Informed Consent
Informed consent was obtained from all individual participants included in the study.
Contributor Information
Ching-Hsuan Hu, Email: Chinghsuanhu@yahoo.com.tw.
Duretti Fufa, Email: duretti.fufa@gmail.com.
Chung-Chen Hsu, Email: hsu.chungchen@gmail.com.
Yu-Te Lin, Email: linutcgmh@gmail.com.
Chih-Hung Lin, Email: Chinghsuanhu@hotmail.com.tw, Email: profchlin@gmail.com.
References
- 1.Al-Najjim M, Fenton C, Scott T. Closed rupture of abductor pollicis longus and extensor pollicis brevis associated with fracture of the distal radius. J Hand Surg Eur Vol. 2012;37:176–7. doi: 10.1177/1753193411424703. [DOI] [PubMed] [Google Scholar]
- 2.Apard T, Moui Y. Spontaneous rupture of extensor pollicis longus in systemic lupus erythematosus. Chir Main. 2004;23:254–6. doi: 10.1016/j.main.2004.08.004. [DOI] [PubMed] [Google Scholar]
- 3.Avci S, Yilmaz C, Sayli U. Comparison of nonsurgical treatment measures for de Quervain’s disease of pregnancy and lactation. J Hand Surg Am. 2002;27:322–4. doi: 10.1053/jhsu.2002.32084. [DOI] [PubMed] [Google Scholar]
- 4.Bjorkman A, Jorgsholm P. Rupture of the extensor pollicis longus tendon: a study of aetiological factors. Scand J Plast Reconstr. 2004;38:32–5. doi: 10.1080/02844310310013046. [DOI] [PubMed] [Google Scholar]
- 5.Cauldwell EW, Anson BJ, Wright RR. The extensor indicis proprius muscle. A study of 263 consecutive specimens. Q Bull Northwest Univ Med Sch. 1943;17:267–79. [Google Scholar]
- 6.Choi JC, Kim WS, Na HY, et al. Spontaneous rupture of the extensor pollicis longus tendon in a tailor. Clin Orthop Surg. 2011;3:167–9. doi: 10.4055/cios.2011.3.2.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.el-Badawi MG, Butt MM, al-Zuhair AG, et al. Extensor tendons of the fingers: arrangement and variations—II. Clin Anat. 1995;8:391–8. doi: 10.1002/ca.980080604. [DOI] [PubMed] [Google Scholar]
- 8.Engkvist O, Lundborg G. Rupture of the extensor pollicis longus tendon after fracture of the lower end of the radius—a clinical and microangiographic study. Hand. 1979;11:76–86. doi: 10.1016/S0072-968X(79)80015-7. [DOI] [PubMed] [Google Scholar]
- 9.Ferreres A, Llusa M, Garcia-Elias M, et al. A possible mechanism of direct injury to the EPL tendon at Lister’s tubercle during falls with the wrist fully extended. J Hand Surg Eur Vol. 2008;33:149–51. doi: 10.1177/1753193407087575. [DOI] [PubMed] [Google Scholar]
- 10.Fm S. Late rupture of extensor policis longus tendon following Colles’s fracture. J Bone Joint Surg Am. 1946;29:49–59. [PubMed] [Google Scholar]
- 11.Fujita N, Doita M, Yoshikawa M, et al. Spontaneous rupture of the extensor pollicis longus tendon in a professional skier. Knee Surg Sport Traumatol Arthrosc. 2005;13:489–91. doi: 10.1007/s00167-004-0539-z. [DOI] [PubMed] [Google Scholar]
- 12.Hirasawa Y, Katsumi Y, Akiyoshi T, et al. Clinical and microangiographic studies on rupture of the E.P.L. tendon after distal radial fractures. J Hand Surg Br. 1990;15:51–7. doi: 10.1016/0266-7681(90)90048-9. [DOI] [PubMed] [Google Scholar]
- 13.Kim CH. Spontaneous rupture of the extensor pollicis longus tendon. Arch Plast Surg. 2012;39:680–2. doi: 10.5999/aps.2012.39.6.680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kurklu M, Bilgic S, Yurttas Y, et al. Spontaneous rupture of the extensor pollicis longus tendon due to a small osteophyte. Acta Reumatol Port. 2009;34:555–6. [PubMed] [Google Scholar]
- 15.Kwedar AT, Mitchell CL. Late rupture of extensor pollicis longus tendon following Colles’ fracture. J Bone Joint Surg Am. 1940;22A:429–35. [Google Scholar]
- 16.Lloyd TW, Tyler MP, Roberts AH. Spontaneous rupture of extensor pollicis longus tendon in a kick boxer. Br J Sport Med. 1998;32:178–9. doi: 10.1136/bjsm.32.2.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McKay SD, MacDermid JC, Roth JH, et al. Assessment of complications of distal radius fractures and development of a complication checklist. J Hand Surg Am. 2001;26:916–22. doi: 10.1053/jhsu.2001.26662. [DOI] [PubMed] [Google Scholar]
- 18.Mestdagh H, Bailleul JP, Vilette B, et al. Organization of the extensor complex of the digits. Anat Clin. 1985;7:49–53. doi: 10.1007/BF01654629. [DOI] [PubMed] [Google Scholar]
- 19.Navaratnam AV, Ball S, Eckersley R. Prophylactic decompression of extensor pollicis longus to prevent rupture. BMJ Case Rep. 2013. doi:10.1136/bcr-2013-010196. [DOI] [PMC free article] [PubMed]
- 20.Perry DC, Machin DMG, Casaletto JA, et al. Minimising the risk of extensor pollicis longus rupture following volar plate fixation of distal radius fractures: a cadaveric study. Ann Roy Coll Surg. 2011;93:57–60. doi: 10.1308/003588411X12851639107151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rada EM, Shridharani SM, Lifchez SD. Spontaneous atraumatic extensor pollicis longus rupture in the nonrheumatoid population. Eplasty [Electron Resour] 2013;13:e11. [PMC free article] [PubMed] [Google Scholar]
- 22.Roth KM, Blazar PE, Earp BE, et al. Incidence of extensor pollicis longus tendon rupture after nondisplaced distal radius fractures. J Hand Surg-Am. 2012;37:942–7. doi: 10.1016/j.jhsa.2012.02.006. [DOI] [PubMed] [Google Scholar]
- 23.Skoff HD. Postfracture extensor pollicis longus tenosynovitis and tendon rupture: a scientific study and personal series. Am J Orthop. 2003;32:245–7. [PubMed] [Google Scholar]
- 24.Straub LR, Wilson EH., Jr Spontaneous rupture of extensor tendons in the hand associated with rheumatoid arthritis. J Bone Joint Surg Am. 1956;38-A:1208–17. [PubMed] [Google Scholar]
- 25.Tountas Chris P, Bergman R. Anatomic variations of the upper extremity. New York: Churchill Livingstone; 1993. pp. 117–35. [Google Scholar]
- 26.Yuen A, Coombs CJ. Abductor pollicis longus tendon rupture in De Quervain’s disease. J Hand Surg Br. 2006;31:72–5. doi: 10.1016/j.jhsb.2005.09.020. [DOI] [PubMed] [Google Scholar]
- 27.Zilber S, Oberlin C. Anatomical variations of the extensor tendons to the fingers over the dorsum of the hand: a study of 50 hands and a review of the literature. Plast Reconstr Surg. 2004;113:214–21. doi: 10.1097/01.PRS.0000091163.86851.9C. [DOI] [PubMed] [Google Scholar]


