Abstract
Hepatocellular carcinoma (HCC) is the 5th most common malignancy which is responsible for more than half million annual mortalities; also, it is the third leading cause of cancer related death. Unfavorable systemic side-effects of chemotherapeutic agents and susceptibility to the degradation of small interfering RNAs (siRNAs), which can knock down a specific gene involved in the disease, have hampered their clinical application. So, it could be beneficial to develop an efficient carrier for the stabilization and specific delivery of drugs and siRNA to cells. Targeted nanoparticles have gained considerable attention as an efficient drug and gene delivery system, which is due to their capability in achieving the highest accumulation of cytotoxic agents in tumor tissue, modifiable drug pharmacokinetic- and bio-distribution, improved effectiveness of treatment, and limited side-effects. Recent studies have shed more light on the advantages of novel drug loaded carrier systems vs free drugs. Most of the animal studies have reported improvement in treatment efficacy and survival rate using novel carrier systems. Targeted delivery may be achieved passively or actively. In passive targeting, no ligand as homing device is used, while targeting is achieved by incorporating the therapeutic agent into a macromolecule or nanoparticle that passively reaches the target organ. However, in active targeting, the therapeutic agent or carrier system is conjugated to a tissue or cell-specific receptor which is over-expressed in a special malignancy using a ligand called a homing device. This review covers a broad spectrum of targeted nanoparticles as therapeutic and non-viral siRNA delivery systems, which are developed for enhanced cellular uptake and targeted gene silencing in vitro and in vivo and their characteristics and opportunities for the clinical applications of drugs and therapeutic siRNA are discussed in this article. Asialoglycoprotein receptors, low-density lipoprotein, ganglioside GM1 cell surface ligand, epidermal growth factor receptor receptors, monoclonal antibodies, retinoic acid receptors, integrin receptors targeted by Arg-Gly-Asp peptide, folate, and transferrin receptors are the most widely studied cell surface receptors which are used for the site specific delivery of drugs and siRNA-based therapeutics in HCC and discussed in detail in this article.
Keywords: Small interfering RNA, Targeted delivery, Nanoparticle, Hepatocellular carcinoma, Chemotherapeutic agents
Core tip: Targeted nanoparticles have gained considerable attention as an efficient drug and gene delivery system in hepatocellular carcinoma owing to their capability for achieving the highest accumulation of cytotoxic agents in tumor tissue, modifiable drug pharmacokinetic- and bio-distribution, improved effectiveness of treatment, and limited side-effects. This review covers a broad spectrum of targeted nanoparticles as therapeutic and non-viral small interfering RNA (siRNA) delivery systems, which are developed for enhanced cellular uptake and targeted gene silencing in vitro and in vivo. Their characteristics and opportunities for the clinical applications of drugs and therapeutic siRNA are discussed in this article.
EPIDEMIOLOGY
Hepatocellular carcinoma (HCC) as the 5th most common malignancy is the most common primary liver cancer and is responsible for more than half million annual mortalities, which makes it the third leading cause of cancer related deaths[1]. This disease more dominantly affects males than females, the ratio of which is usually around 3:1 or 4:1 in most populations[2]. At the moment, HCC is most prevalent in East Asia; but, it is rapidly pervading through most of the Western nations and the number of diagnosed patients is rapidly increasing[1,3].
Etiology
Several risk factors are held responsible for the occurrence of HCC, but with varying importance levels in different regions. This disease mostly occurs in persons with a history of other liver diseases such as cirrhosis, which is the unique nature of HCC and points to the most important risk factors as Hepatitis C and B as well as alcoholic and non-alcoholic fatty liver. Other important risk factors are toxic exposure to aflatoxins and vinyl chloride, diabetes mellitus, obesity, diet, hemochromatosis, Wilson’s disease, type 2 diabetes, hemophilia, and genetic factors[4]. The overall average 5-year survival rate of HCC is estimated as 70% for the patients undergoing surgery[5].
SIGNS AND SYMPTOMS
There are several staging systems for HCC which determine the course of treatment and treatment prognosis[6]. HCC patients may show jaundice, bloating from fluid in the abdomen, easy bruising from coagulopathy, loss of appetite, unintentional weight loss, nausea, vomiting, or fatigue. Patients usually complain about right upper quadrant pain, weight loss, and deterioration of liver function in cirrhotic cases. Most symptoms are unspecific such as abdominal pain, malaise, fever, jaundice, and anorexia. Ascites, hemorrhage, and encephalopathy may also occur; but, a large number of population may remain asymptomatic[7].
DIAGNOSIS
HCC screening is recommended for high risk patients and the most frequently used surveillance methods are testing serum α-fetoprotein (AFP) and abdominal ultrasound in 6 mo intervals[8,9]. Ultrasound is often the first imaging and screening modality which is used. In the patients with higher suspicion of HCC (such as rising alpha-fetoprotein and des-gamma carboxyprothrombin levels), the best method of diagnosis involves a computed tomography (CT) scan of the abdomen using intravenous contrast agent. A biopsy is not needed to confirm the diagnosis of HCC if certain imaging criteria are met. An alternative to a CT imaging study would be magnetic resonance imaging (MRI)[8,9].
MANAGEMENT AND TREATMENT MODALITIES FOR HCC
Non-medicinal managements of HCC
If benefits outweigh surgery risks, the patient is a candidate for surgical modalities such as liver resection in the case of early-stage non-cirrhotic patients and liver transplantation in the case of chronic disease and cirrhosis. However, early-stage HCC patients that are not qualified for surgical interventions can alternatively benefit from minimally invasive treatments such as percutaneous ablation and intermediate-stage HCC cases that have not shown vascular invasion and cancer related symptoms could undergo trans catheter arterial chemoembolization (TACE), which is usually performed for unresectable tumors or as a temporary treatment while waiting for liver transplant[10]. Other managements include: interventional radiology; http://en.wikipedia.org/wiki/File:HepatoCellular_Ca.JPG; radiofrequency ablation (RFA) using high frequency radio-waves to destroy tumor by local heating; selective internal radiation therapy (SIRT) used to destroy the tumor and thus minimize exposure of healthy tissue; intra-arterial iodine-131-lipiodol administration and percutaneous ethanol injection (PEI) as well-tolerated methods; combined PEI and TACE for the tumors of larger than 4 cm in diameter; and portal vein embolization as a method using a percutaneous trans hepatic approach in which an interventional radiologist embolizes the portal vein supplying the side of the liver and the tumor. There are currently two products of embolic microspheres: SIR-Spheres and Thera Sphere. The latter is an FDA approved treatment for primary HCC. SIR-Spheres are FDA approved for the treatment of metastatic colorectal cancer, but outside the United States. Cryosurgery is also another management of HCC that is a new technique and can destroy tumors in the liver. High intensity focused ultrasound is another therapeutic treatment of HCC[10]. Figure 1 summarizes various treatment strategies for HCC at different stages according to the Barcelona Clinic Liver Cancer algorithm.
Figure 1.
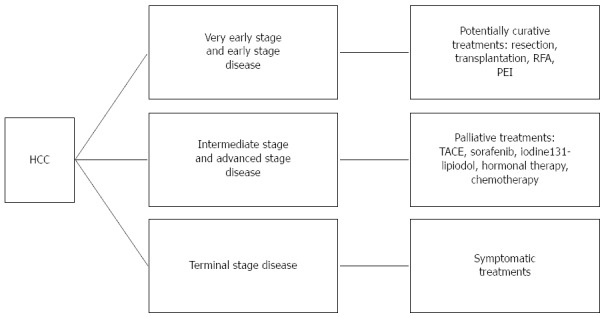
Schematic representation of various treatment strategies for hepatocellular carcinoma at different stages according to the Barcelona Clinic Liver Cancer algorithm. RFA: Radiofrequency ablation, PEI: Percutaneous ethanol injection; TACE: Trans catheter arterial chemoembolization.
Therapeutics of HCC
Palliative and restricted therapy to a localized region of the body could also be used in intermediate- to advanced-stage patients, for whom embolization is not feasible. Some examples of locoregional therapy methods are internal radiation and hormonal therapy including antiestrogen therapy with tamoxifen (usually considered ineffective), octreotide (somatostatin analogue), and adjuvant chemotherapy. No randomized trial has shown the benefit of neoadjuvant or adjuvant systemic therapy in HCC. Single trial has shown a decrease in new tumors among the patients receiving oral synthetic retinoid for 12 mo after resection/ablation. Results have not been reproduced[11].
Since systemic chemotherapy is not proved to significantly increase survival rate in HCC patients and due to the overall side-effects of chemotherapeutic agents, their dose limitation, and possibly the expression of multi drug resistance gene (MDR-1) in HCC, chemotherapy is now considered one of the palliative therapies for HCC, while the survival rate of incurable HCC patients remains poor[12].
Doxorubicin is one of the most frequently used cytotoxic agents for the chemotherapy of non-resectable HCC tumors, even though it has high toxic side-effects and has shown no increased survival rate[13]. Randomized phase II and III studies have also compared the response rates of doxorubicin vs the frequently used PIAF regimen consisting of cisplatin/interferonα-2b/doxorubicin/5-fluorouracil; while the response rates have been slightly enhanced, the survival rates are not significantly improved[14,15]. Gemcitabine has been found to be more effective in hepatic cancers and the combination regimen of gemcitabine and oxaliplatin (GEMOX) along with bevacizumab has slightly increased the survival time in a phase II study[16].
Studies on interferon-α (IFN-α) immunotherapies have suggested that IFN-α could have survival benefits for non-curable HCC patients when used in combination with other agents[17].
Many molecular targeted therapies are also under phase II and III studies. A receptor tyrosine kinase inhibitor, sorafenib, as an FDA approved drug, may be used in the patients with advanced HCC. Sorafenib is a small molecule that inhibits tumor-cell proliferation and tumor angionesis. It correspondingly increases the rate of apoptosis in other tumor models. Sorafenib is one of the molecular targeted small molecule agents, which blocks vascular epithelial growth factor receptors (VEGFRs) 1, 2 and 3 and platelet derived growth factor receptor β (PDGFR-β) through multikinase inhibition and leads to the inhibition of tumor growth and angiogenesis[18,19]. Results of meta-analysis based on phase II and III trials have suggested that sorafenib-based chemotherapy is superior to placebo-based chemotherapy in terms of overall survival without considerable increase in toxicity[20].
Bevacizumab is another molecular drug which is, in fact, a humanized monoclonal antibody against VEGF and, hence, results in the blockade of angiogenesis. Findings of phase II clinical trials have suggested that bevacizumab might increase the survival rate of patients with nonmetastatic HCC[21]. Erlotinib and sunitinib are also other small molecules for the inhibition of thyrosine kinase that have been found effective in phase II trials[22,23]. Cetuximab and lapatinib are other molecular therapeutics that are currently under phase II studies for non-resectable HCC[24].
Small interfering RNA-based treatment of HCC
Small interfering RNA (siRNA) is a double-strand RNA molecule which is also named short interfering RNA or silencing RNA with 20-25 base pairs in length. siRNA interferes with the expression of specific genes with complementary nucleotide sequences. It causes mRNA to get broken down after transcription and result in no translation[25]. RNA interference (RNAi) may represent a powerful strategy to interfere in key molecular pathways involved in cancer and has established a new area of clinical therapy for HCC. siRNA induced RNAi presents an effective and simple method to silence a wide range of cancer-associated genes. A number of siRNAs have been established that are capable of silencing some different types of human HCC gene targets, such as livin, cyclin E, VEGF, COP9 signalosome subunit 5, c-Myc, and so on[26-29]. The most important molecular and biochemical markers of human hepatocellular carcinoma effective in progression and poor prognosis include glypican-3, Dickkopf-1, S100A4, S100A14, SOX6, SUOX, AKR1B10, and CD34, cystine/glutamic acid transporter, GRK6, GPR87, metallothioneins, retinoic acid-induced protein 3, synovial sarcoma X breakpoint 2, protein phosphatase magnesium-dependent 1 delta, BCL9, interferon regulatory factor-1 and 2, CDK4, LASP-1, PTP4A3, fatty acids, PAK5, hnRNPL, cylindromatosis gene, melanoma-associated antigen family protein D-4, EphA3, and Flotillin-1[30]. Knocking down of the genes of these biomarkers by siRNA may be used for the treatment of HCC. Li et al[31] presented the development of TetR siRNA therapeutics for HCC using an integrated approach, including the development of an efficient lipid nanoparticle (NP) delivery system, the identification of a robust therapeutic target that does not trigger liver toxicity upon target knock down, and the selection of potent and non-immunogenic siRNA molecules against the target. The TetR-ODC-Luc, HepG2, or HuH7 cells were inoculated into the liver of 6 to 8 wk old severe combined immune-deficient female mice to create various orthotopic HCC liver tumor models. The resulting siRNA-containing lipid NPs produced significant antitumor efficacy in orthotopic HCC models and, thus, represented a promising starting point for the development of siRNA therapeutics for HCC.
Kinesin spindle protein (KSP) plays a critical role in mitosis. Inhibition of KSP function leads to cell cycle arrest at mitosis and, ultimately, cell death. In the study done by Doan et al[32], KSP expression was suppressed by specific siRNA in Hep3B cells and evaluated its anti-tumor activity. KSP-siRNA transfection induced apoptosis and could increase chemo sensitivity to DOX in Hep3B cells, even at low doses compared to the control. This method may yield promising results for eradicating HCC cells in vitro.
Another important siRNA type in HCC is the specific gene silencing siRNA of AFP which is an oncoembryonal protein highly expressed in the majority of HCCs. AFP may be involved in multiple cell growth regulating, differentiating, and immunosuppressive activities. Effects of AFP gene silencing by siRNA on the apoptosis and proliferation of HCC cell line EGHC-9901, which highly expresses AFP has been investigated. Western blot and RT-PCR assay have demonstrated that siRNA-AFP induces high expression of caspase-3, caspase-8, caspase-9, and Bcl-2[33].
p28GANK is an HCC oncogene. The adenovirus-delivered siRNA (AdsiRNA) is applied to inhibit this oncogene in HCC cell lines and the antitumor effect is investigated. The T7-RNA polymerase system is used to screen the specific target site. AdSiRNA could suppress p28GANK expression by up to 80% in HCC cells. Depletion of p28GANK induces caspase-8- and caspase-9-mediated apoptosis of HCC cells. Finally, targeting p28GANK by adenovirus injection inhibits the growth of established tumors in nude mice. This study shows that the T7-RNA polymerase system screening-based AdSiRNA can be used successfully to silence an oncogene. p28GANK may serve as a novel therapeutic target for treating HCC[34].
NANOPARTICLE-BASED DRUG DELIVERY
Nanoparticulate drug delivery systems are solid, colloidal particles with the particle size of 10 to 1000 nm. However, in nanomedicine, they often refer to devices < 200 nm (i.e., the width of microcapillaries). There are two types of NPs: nanocapsules and nanospheres. Nanocapsules are vesicular systems in which a drug is confined to a cavity surrounded by a polymeric membrane, whereas nanospheres are matrix systems in which the drug is physically and uniformly dispersed. NPs can load the active ingredients in different forms of dissolved, entrapped, adsorbed, attached, and/or encapsulated into or onto a nanomatrix. Systemic unfavorable side-effects of chemotherapeutic agents and other drugs have led to research on the development of new agents or therapeutic strategies. The main objectives are to achieve the highest accumulation of cytotoxic agents in tumor tissue, modify drug pharmacokinetic- and bio-distribution, improve effectiveness of treatment, and limit the side-effects.
Targeted delivery may be achieved passively or actively (Figure 2). In the passive targeting, no ligand is used as a homing device and targeting is achieved by incorporating the therapeutic agent into a macromolecule or nanoparticle that passively reaches the target organ. In this strategy, the leaky nature of vessels in cancer tissue and lack of well-defined lymphatic system can enhance the permeation and retention of NPs, which is called the enhanced permeation and retention (EPR) effect. However, in active targeting, the therapeutic agent or carrier system is conjugated to a tissue or cell specific receptor which is over-expressed in special malignancy using a ligand called homing device[35].
Figure 2.
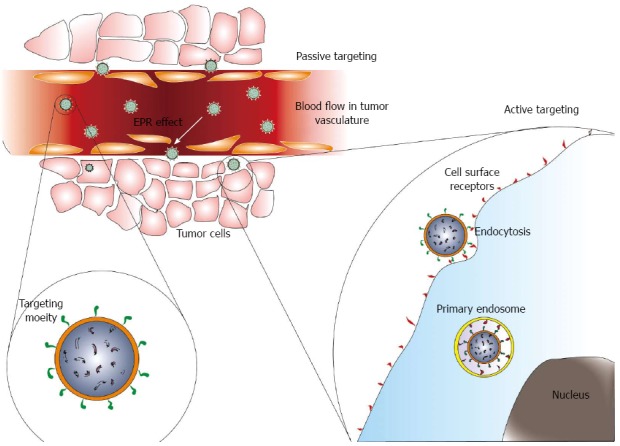
Different methods of targeted delivery of nanoparticles by passive or active mechanism. EPR: Enhanced permeation and retention.
CELL SURFACE RECEPTORS IN HCC
HCC has one of the worst prognoses for survival as it is poorly responsive to both conventional chemotherapy and mechanism-directed therapy. This issue is due to the lack of therapeutic concentration in the tumor tissue coupled with the highly toxic off-site effects exhibited by these compounds. Consequently, the best packaging for the therapy of HCC will involve three components: a potent therapeutic, a rationally designed drug delivery vehicle to enrich the target site concentration of the drug, and a surface ligand that can lead to greater propensity for internalization by tumor cells compared to parenchyma. Before addressing the variety of targeted drug delivery systems used in HCC, an introduction to the different receptors that are over-expressed in this disease and may be used for the active targeting of chemotherapeutic agents loaded in NPs may be useful. Serotonin is a well-known neurotransmitter and vasoactive substance. Recent studies have indicated that serotonin contributes to liver regeneration and promotes tumor growth of human HCC. The serotonin receptors 1B and 2B are expressed, respectively, in 32% and 35% of the patients with hepatocellular cancer. Both receptors are associated with an increased proliferation index in Huh7 and HepG2 cell lines[36].
Gamma-aminobutyric acid and gamma-aminobutyric acid A receptor θ subunit play important roles in HCC development and progression and could be a promising molecular target for the development of new diagnostic and therapeutic strategies for HCC[37].
Over-expression of fibroblast growth factor receptor 3 (FGFR3), which is a signal transduction and cell proliferation related gene in HCC, is another important receptor with an important role in liver carcinogenesis. FGFR3 may be an ideal candidate as a molecular marker in the diagnosis of HCC and a potential therapeutic target[38]. Epidermal growth factor receptor (EGFR) is frequently over-expressed in HCC. EGFR expression has shown borderline association with cirrhosis, but not with other examined clinicopathologic parameters. EGFR over-expression is present in a majority of HCC types, which suggests a role for EGFR antagonists in therapy[39].
Somatostatin receptor related alterations are potentially novel prognostic and predictive biomarkers for HCC with a special emphasis on the therapeutic potential of somatostatin analogues in HCC management[40].
Insulin receptor (IR) exists as two isoforms resulting from the alternative splicing of IR pre-mRNA. IR-B promotes the metabolic effects of insulin, while IR-A rather signals proliferative effects. IR-B is predominantly expressed in the adult liver. Alternative splicing of IR pre-mRNA is dysregulated in HCC, while it is normal in adjacent non-tumor liver tissue. Increased expression of IR-A during the neoplastic transformation of hepatocytes could mediate some of the adverse effects of hyperinsulinemia on HCC[41].
Prostaglandin E2 (PGE2) has been implicated in cell invasion in HCC via increased β1-integrin expression and cell migration by activating the PKC/NF-κB signaling pathway. Targeting PGE2/EP1/PKC/NF-κB/FoxC2/β1-integrin pathway may represent a new therapeutic strategy for the prevention and treatment of this cancer[42]. High levels of adenosine accumulate in hypoxic tissues during the rapid growth of tumors, suggesting that the activation of adenosine receptors may facilitate tumor progress. A2b expression is up-regulated in HCC and its expression level is correlated to tumor progression in HCC, which suggest that A2b may be a novel target for HCC therapeutic strategy[43]. The insulin-like growth factor (IGF) pathway is implicated in the pathogenesis of HCC and may be important in nonalcoholic fatty liver disease. Significant associations have been seen between IGF-1 expression and liver cirrhosis and survival after resection in patients with HCC, independent from their underlying liver disease[44].
Galactosamine-mediated targeted delivery of anti-cancer drugs in the liver has been tested, because its receptor, asialoglycoprotein receptor 1 (ASGPR1), is expressed in the liver and not in other human tissues. Mammalian hepatic ASGPRs mediate the binding, internalization, and degradation of extracellular glycoproteins with exposed terminal galactose, lactose, or N-acetyl-galactosamine residues[45].
Androgen (AR) signaling has also been shown to suppress the metastasis of HCC among the patients with late-stage disease. In addition, there is evidence that therapy comprising Sorafenib and agents that enhance the functional expression of AR may suppress the progression of late-stage HCC[46].
Another surface receptor which is over-expressed in HCC is the folate receptor (FR). Folate is a basic component of cell metabolism and DNA synthesis and repair. Rapidly dividing cancer cells have an increased requirement for folate to maintain DNA synthesis, an observation supported by the widespread use of anti-folates in cancer chemotherapy. FR levels are high in specific malignant tumors of epithelial origin compared to normal cells and are positively associated with tumor stage and grade, which raises the questions of its role in tumor etiology and progression. Although the precise mechanism of pathway(s) for FR uptake has not been exploited, phagocytosis is proposed from the observation that FR recycles between an acid-resistant (intracellular) and acid-sensitive (extracellular) pool. GPI-anchored proteins are diffusely distributed at the cell surface and it is proposed that FR is cross-linked by these proteins and then concentrated in clusters at the cell membrane surfaces called Caveolae, whereby the membrane would transiently close and internalize the folate-bound receptor complex. When the internal compartment of the cell shows increased acidification folate is separated from the receptor and using the energy generated from the acidic gradient moves across the membrane into the cytoplasm of the cell, then, the next cycle would be started at the cell surface membrane by the exposure of the receptors[47].
Transferrin receptor (TfR) is also over-expressed in many malignant cells, including breast cancer, pancreatic cancer, prostate cancer, colon cancer, lung cancer, and leukaemia[48-50] cells. It is also over-expressed in some cell lines of HCC including HepG2, J5, Bel-7402, Huh7, and SK-Hep-1. It is a carrier protein for Tf, imports iron into the cell by internalizing the Tf-iron complex through receptor-mediated endocytosis, and is regulated in response to intracellular iron concentration[51].
Retinoid analogues have been reported to inhibit the growth of HCC. Sano et al[52]’s study showed that retinoic acid receptor-alpha is the dominant receptor in HCC, which suggests that selective retinoid analogues of this receptor may be useful for chemotherapy.
TARGETED NANOPARTICLE-BASED DRUGS AND SIRNA DELIVERY IN HCC
In different works aiming to reduce undesirable side-effects of therapeutic agents in non-target organs, scientists have tried to sign up one of these over-expressed receptors for the active targeting of drugs to HCC by the conjugation of a specific ligand to the NPs which fit to the receptor and facilitate the endocytosis of the drug loaded carrier to the cells. In the following sections, it is attempted to illustrate the potentials of novel strategies based on targeted nanoparticulate delivery systems used in the treatment of HCC incorporating drugs or siRNA through different over-expressed cell surface receptors. Table 1 summarizes some of the different targeted nanocarriers used for the delivery of therapeutic agents and in HCC, while Table 2 shows the reported delivery systems of targeted NPs for siRNA in this disease.
Table 1.
Summary of studied targeted nanoparticles used in vitro/in vivo for drug delivery in hepatocellular carcinoma using different targeting moieties
| Type of nanocarrier | NPs composition | Targeted for receptor | Active moiety | Specific Remarks | Ref. |
| Synthetic or natural polymeric NPs | Polyethylenglycol (PEG), dithiodipropionate, hyaluronic acid | Asialogycoprotein receptor (ASGPR) , no receptor (EPR effect) | Doxorubicin (DOX) | The NPs were sensitive to acidic environment of endosomes and high intracellular Glutathion concentrations | [62] |
| Synthetic or natural polymeric NPs | poly(caprolactone), PEG | no receptor (EPR effect) | Docetaxel | The NPs had a long circulating characteristic and longer retention time in tumor cells | [63] |
| Synthetic or natural polymeric NPs | Galactose (GA), chitosan, | ASGPR | 5-FU | - | [66,74,75] |
| Synthetic or natural polymeric NPs | O-carboxymethyl chitosan, GA | ASGPR | Paclitaxel (PTX) | - | [68] |
| Synthetic or natural polymeric NPs | Hyaluronic acid (HA), GA | ASGPR | PTX | The dual targeting allows for the NPs to get internalized by tumor cells more specifically | [69] |
| Synthetic or natural polymeric NPs | Hematoporphyrin, Bovine serum albumin (BSA) | LDL | DOX | The photosensitizing properties of hematoporphyrin allowed for an accurate monitoring of NP uptake by imaging | [88] |
| Synthetic or natural polymeric NPs | Heat-liable enterotoxin subunite B (LTB), BSA | Ganglioside GM1 receptor | 5-FU | - | [92] |
| Synthetic or natural polymeric NPs | Galactosylated chitosan, polycaprolactone | ASGPR | Curcumin | - | [72] |
| Synthetic or natural polymeric NPs | Galactosylated chitosan, mPEG-SH | ASGPR | Norcantharidin (NCTD) | The drug was actually loaded using ionic cross linkage between NCTD and chitosan | [76] |
| Synthetic or natural polymeric NPs | SM5-1, PLA | Membrane antigens | 5-FU | - | [96] |
| Synthetic or natural polymeric NPs | Apotransferin, BSA | transferrin receptor | DOX | - | [138] |
| Synthetic or natural polymeric NPsSynthetic or natural polymeric NPs | Apotransferrin, LactoferrinChitosan, retinoic acid (RA), Albumin | Transferrin receptorRA receptor | DOXDOX | -- | [139][105] |
| Mixed NPs | GA, DOX, Alginate | ASGPR | DOX | - | [70] |
| Mesoporous high surface area silica core fused to a liposome (protocell) | Silica, PEG, Zwitterionic lipids, phosphatidylethanolamine | SP94 receptor, no receptor (EPR effect) | DOX | The fusogenic peptide used allows for more efficient internalization. The nanoporous silica core also gives the NPs, a significantly higher surface area | [64] |
| Nano micelle | PEG, polycaprolactone, SPION, folate | Folate receptor | Sorafenib | The SPION loaded NPs could be efficiently monitored using MR imaging | [128] |
| Nano micelle | RGD, PEG, stearic acid, chitosan | Integrins | DOX | - | [112] |
| Nano liposome | egg phosphatidylcholine, cholesterol, monomethoxy PEG-distearoyl phosphatidylethanolamine, and Lactose - dioleyl phosphatidylethanolamine (DOPE) | ASGPR | DOX | - | [73] |
| Nano liposome | Anti CD44 antibody, cholesterol, DOPE, DSPC, DSPE-(PEO)4-cRGDfK, DSPE-mPEG | CD44 | DOX | - | [97] |
| Lipid nanocarriers | Lactobionic acid, Stearyl amine, lecithin, glyceryl monostearate, oleic acid | AGPR | 5-FU | - | [71] |
| Magnetic NPs | FeCl2, FeCl3, CMC, EpCAM aptamer | Epithelial cell adhesion molecule | DOX | These magnetic nanoparticles were suggested as a candidate for MR imagine of HCC | [113] |
| Magnetic NPs | Fe3O4/Fe, silica | no receptor (EPR effect) | ABT-888, Temozolamide | The co-delivery of the two drugs both inhibits transcription of survival genes and has cytotoxic effect | [65] |
| BSA NPs | Glycyrrhizic acid (GA), BSA, 10-hydroxycamptothecin (HCPT) | ASGPR | FITC | - | [67] |
| Gold NP | Gold, cetuximab | EGFR | gemcitabine | When coupled with RF-hyperthermia, these NPs were significantly effective at tumor growth inhibition | [94] |
| Nanosuspension | DSPE, PEG, FA, soy lecithin | Folate receptor | Docetaxel | - | [136] |
| Dendrimer | poly(methacryloyl sulfadimethoxine) (PSD), PEG, Lactose | ASGPR | DOX | - | [77] |
| Virus-like NP | MS2 capsid, Ricin toxin A chain, SP94, H5WYG fusogenic peptide, PEG | SP94 receptor | DOX, cisplatin, 5-FU | - | [142] |
| Core-shell NP | Poly(vinyl alcohol), albumin | Transferrin receptor | DOX, sorafenib | The synergistic effect of DOX and sorafenib here increased tumor inhibition more significantly | [141] |
| Miscellaneous | PLGA, PVA, chitosan, Asialofetuin | ASGPR | EPI | Co-delivery of EPI with tocotrienols as anti-oxidative agents, resulted in significantly lower cardiotoxicity and higher apoptosis level | [85] |
| Miscellaneous | Benzyl malolactonate, PEG, Fluorescein amine, Biotin, cyclic Biotin-RGD peptide, streptavidin | Biotin Receptor, integrins | DOX | The use of streptavidin for grafting a peptide suggests that a number of peptides could be grafted in NPs without needing any additional chemistry | [115] |
NP: Nanoparticle; LDL: Low-density lipoprotein; EPR: Enhanced permeation and retention; FITC: Fluorescein isothiocyanate.
Table 2.
Summary of studied targeted nanoparticles used in vitro/in vivo for small interfering RNA delivery in hepatocellular carcinoma using different targeting moieties
| Type of nanocarrier | Active moiety | Targeted receptor | Suggested Mechanism | Ref. |
| Lipid nanoparticle | TetR siRNA | - | - | [31] |
| Novel nonocarrier consisting of a silica core fused to liposomes (called protocell) | Model siRNA | SP94 protein and EPR | - | [64] |
| Galactose mediated trimethylchitosan cysteine NPs | VEGF-siRNA and Survivin shRNA-expression pDNA (iSUR-pDNA) | ASGPR | Silencing of tumor growth genes | [86] |
| A phospholipid-cholesterol nanocomplex | Pokemon siRNA | LDL receptor | Cell growth inhibition | [89] |
| A SPION called SilenceMag | Human VEGF siRNA | EGFR | Tumor growth inhibition | [95] |
| PEGylated Polyethyleneamine SPION | Survivin siRNA | Integrin | Induction of apoptosis | [114] |
| Virus-like nanoparticle of bacteriophage MS2 | Anti-cyclin siRNA | Folic acid receptor, SP94, transferrin receptor | Induction of apoptosis | [142] |
| Lipid nanoparticle | Integrin b1 siRNA | integrin | Inhibition of proliferation and tumor cell death | [116] |
SPION: Superparamagnetic iron oxide nanoparticle; siRNA: Small interfering RNA; LDL: Low-density lipoprotein; EPR: Enhanced permeation and retention; EGFR: Epidermal growth factor receptor; ASGPR: Asialoglycoprotein receptor.
Passive targeting by pegylated NPs
As mentioned before, targeted drug delivery may be achieved by EPR effect via passive targeting. For this purpose, it is necessary for the carrier to have enough time to reach the affected area. Surface-modification of delivery vehicles with polyethylene glycol (PEG), i.e., PEGylation, is a promising method for enhancing in vivo stability and performance of various non-viral drug and gene vectors, which results in the production of stealth NPs[53-59]. In addition, PEGylation can dramatically improve particle transport through biological obstacles, such as mucus[60]. The efficacy of nucleus-targeted drug- or gene-carrying NPs may be limited by slow transport through the molecularly crowded cytoplasm following endosome escape. NPs may stick to cytoskeletal elements and cellular organelles may be steric obstacles for the efficient intracellular transport of NPs. Therefore, surface coating of NPs with PEG can potentially reduce the adhesive interactions of colloids with intracellular components[61]. In this attempt, the dual sensitive spherical NPs of PEGylated dithiodipropionate-hyaluronic acid copolymer (PEG-SS-HA) was produced and loaded with DOX by Xu et al[62]. This NP is prone to releasing its DOX content in response to the acidic pH of intracellular lysosomes and reduction by high intracellular glutathion (GSH) concentration. Due to PEGylation, NPs have a stealth circulation and are finally uptaken by liver cells because of the HA content. The in vitro studies have demonstrated that these NPs are effectively internalized by HepG2 cell line and cause the inhibition of cell growth.
Docetaxel loaded poly ethyleneglycol-poly (caprolactone) (mPEG-PCL) NPs are another example of passive targeted NPs used on hepatic cancer cell line H22 in vitro. This study results in the same cytotoxic effect as the free commercial Docetaxel. NPs have a long circulation, higher accumulation inside tumor parenchyma, longer retention time in tumor cells in vivo, and hence effective tumor growth inhibition[63].
Pegylation along with peptide targeted NPs have been used for efficient co-delivery of therapeutic and siRNA in HCC, one of which is a spherical, nanoporous high surface area silica core fused to liposomes. The obtained hybrid and supported lipid bilayer, named protocell, is then modified using a targeting SP94 peptide, PEG, and fusogenic peptide. This novel nanocarrier has a much higher surface area that results in higher capacity for therapeutic loading as well as enhanced stability and selectivity compared to the liposomes with the same size. DOX, a low molecular weight model drug, and a siRNA model are loaded into these protocells. The protocells are demonstrated to be internalized rapidly by Hep3B cells and DOX is released in an efficient manner in physiological mimicking environments. The protocells designed here are potential candidates for the delivery of a disparate set of cargoes and therapeutic and siRNA cocktails with the flexibility of selecting several targeting ligands and other characteristics[64].
Sometimes, passive targeting is potentiated by an external magnetic field to concentrate the NPs in the affected area. An example of this method of targeting is a study in which a poly (ADP-ribose) polymerase 1 (PARP-1) inhibitor (ABT-888) in conjunction with the alkylating agent temozolomide (TMZ) is used as a therapeutic strategy to increase the cytotoxic effect of drug on HCC. Fe3O4/Fe core with a silica shell is prepared for the dual delivery of ABT-888 and TMZ. This nanosystem is tested in vitro on three tumoral and one non-cancerous cell lines of the liver. An extended release kinetic is achieved and the NPs are accumulated in tumor cells and show higher efficacy in apoptotic cell death compared to free drug[65].
Asialoglycoprotein receptors
Although PEGylation has been widely used to enhance the accumulation of NPs in tumor tissues through EPR effect, it still inhibits cellular uptake and affects intracellular trafficking of carriers. On the other hand, active targeting of molecules displays better cell selectivity and enhances the poor tumor penetration effect. As mentioned before, asialoglycoprotein receptors are another type of receptors over-expressed on HCC cells. They are lectins which bind asialoglycoprotein; glycoproteins from which a sialic acid has been removed to expose galactose residues. The receptors, which are located on liver cells, remove the target glycoproteins from circulation. Glycyrrhetinic acid (GA) is one of the sugar type ligands, which is used for the targeted delivery of NPs to HCC. GA modified chitosan NPs are produced and loaded with 5-FU. The NPs provide a sustained release system that halts tumor cell growth in vitro in a time and dose dependent manner. The in vivo studies on an ortothopic model of liver cancer in mouse have demonstrated significant tumor growth inhibition and prolonged life span[66].
In another study, glycyrrhizic acid modified NPs of bovine serum albumin are synthesized by different concentrations of each agent and loaded with 10-hydroxycamptothecin. These NPs have higher affinity for hepatic tumor cells and the treatment group shows a higher amount of tumor growth inhibition than the control group[67].
Use of glycyrrhizin modified O-carboxymethyl chitosan NPs loaded with paclitaxel is another example of targeted NPs toward ASGPRs, which are tested on HCC cell line of SMMC-7721. The blank NPs show complete biocompatibility and no toxicity. The cell internalization of glycyrrhizin conjugated NPs is almost 10 times higher than the non-targeted NPs. Furthermore, the tumor growth inhibition is significantly higher than non-targeted NPs and free paclitaxel[68].
A double target nanocarrier containing glycyrrhetinic acid-grafted-hyaluronic acid (GAHA) NPs is also synthesized. This double target nanocarrier against liver tumor cells consist of a hyaluronic acid shell with glycyrrhetinic acid grafts encapsulating paclitaxel and is tested on two different cell lines of human HCC. The uptake of NPs is high in HepG2, which has both receptors for HA and GA. The carrier itself has a low cytotoxicity level and in vivo imaging studies have demonstrated a high accumulation level in tumor cells[69].
GA was also used as the targeting moiety to target ASGPRs by Guo et al[70]. A pH sensitive nanocarrier system consisting of GA modified alginate/doxorubicin (DOX) modified alginate is prepared and tested on the model of HCC. The release profile of DOX from NPs is prolonged compared to the half-life of free agent and responds to the pH of endosomes. The nanosystem could successfully decrease tumor growth in mice without any mortality.
Varshosaz et al[71] also developed galactosylated nanostructured lipid carriers (NLC) for the targeted delivery of 5-FU in HCC. They conjugated lactobionic acid to stearyl amine by chemical reaction. The targeted NLCs of 5-FU contained lecithin, glyceryl monostearate, oleic acid, or Labrafac as the oil phase and was dispersed in an aqueous phase containing Tween 80 or Solutol HS15 as the surfactants. NLCs were prepared by an emulsification-solvent diffusion method. The galactosylated NLCs of 5-FU were cytotoxic at the concentration of half dose of free 5-FU on HepG2 cell line and seemed promising in reducing 5-FU dose in HCC.
Galactosylated chitosan-polycaprolactone (Gal-CH-PCL) NPs loaded with curcumin are another type of the NPs targeted to ASGPRs. NPs have a controlled release and their PCL content is found to be a key factor for the release mechanism. NPs are efficiently uptaken by HepG2 cells in vitro and the curcumin loaded into NPs has a 6-fold higher cytotoxic effect than free curcumin. This issue suggests improved bioavailability by Gal-CH-PCL NPs[72].
Another reported example of the targeted nananoparticulate delivery systems is a lactosylated lipid called dioleylphosphatidylethanolamine (Lac-DOPE), which is utilized as the targeting ligand on the modified liposome of methoxy pegylated distearoeylphosphatidylethanolamine (mPEG-DSPE) loaded with DOX which targets ASGPR of hepatocytes in HCC. The Lac-L-DOX nanoliposomes show a higher uptake by HepG2 hepatocellular cells and an enhanced cytotoxicity rate compared with the non-targeted liposomal DOX in conjunction with the longer circulation time due to PEG modification. The in vivo studies have also demonstrated increased tumor growth inhibition in nude mice compared to both free and non-targeted liposomal drugs[73].
Galactosylated chitosan (GC) NPs are synthesized encapsulating 5-FU and tested in vivo and in vitro to HCC cells. Studies have demonstrated higher apoptosis induction through p53 pathway by GC/5-FU and the test group has no such 5-FU related side-effects as liver injury or bone marrow suppression. These NPs also show a sustained release mechanism for 5-FU, which carrier could be promising for 5-FU delivery to hepatic cells without the usual immunosuppressive effects of this chemotherapeutic agent[74,75]. Another form of these NPs is prepared by cross-linking the GC using norcantharidin as the active pharmaceutical ingredient, whose in vivo antitumor activity is better than either the free norcantharidin or norcantharidin attached to CS NPs, but without galactose residue in mice bearing H22 liver tumors[76].
Lactose is another sugar used for targeting ASGPRs. In a study, lactose modified PEGylated poly (amido amine) (PAMAM) dendrimer that is turned into a pH sensitive system by poly (methacryloyl sulfadimethoxine) (LA-PEG-b-PSD-PAMAM) and DOX is loaded in PAMAM. The drug release is significantly higher at pH 6.5 compared to pH 7.4 in PBS. The modified dendrimers have a specific cellular uptake by hepatoma cells at pH 6.5 and in vivo studies show a higher tumor growth inhibition rate by the modified dendrimers[77].
Asialofetuin (AF) is a glycoprotein that possesses three asparagine-linked triantennary complex carbohydrate chains with terminal N-acetylgalactosamine residues. This protein has high affinity to ASGPR on hepatocytes and enters the cells through this receptor[78,79]. Thus, AF has been used as a ligand to deliver drugs to hepatocytes and a competitive inhibitor to ASGPR[80,81]. AF-appended liposomes have widespread use as a hepatocyte-selective gene transfer carrier[82-84].
Epirubicin (EPI) loaded chitosan-poly(lactide-co-glicolide) (PLGA) NPs were designed by Nasr et al[85] to target hepatocytes using asialofetuin and the NPs were tested on HepG2 cell line and HCC induced mouse model. Also, in an attempt for decreasing cardiotoxicity, these delivery systems were co-administered with tocotrienols. The developed NPs reduced cell proliferation and tumor angiogenesis and also, when co-administered with tocotrienols, further enhanced apoptosis and decreased VEGF level dose dependently. The cardiotoxicity assessment demonstrated that EPI-NPs decreased the level of TNF-alfa induced inflammation, nitric oxide (NO), lipid peroxidation product of oxidative stress, and restored superoxide desmutase levels and also reduced glutathione levels in the heart. All these effects were enhanced when co-administered with tocotrienols.
The ASGPRs are not only used for the targeted delivery of therapeutic agents but also for siRNA based drug delivery. For example, NPs of galactose mediated trimethyl chitosan cystein (GTC) are developed for the oral delivery of VEGF-siRNA and Survivin shRNA-expression pDNA (iSUR-pDNA). Co-administration of a pDNA and siRNA allows for both prompt and long-lasting silencing effects on tumor growth genes. The NPs with moderate galactose density could effectively enter the tumor tissue both in vitro and in vivo and result in Survivin and VEGF gene silencing and, hence, decreased cell growth and angiogenesis and increased induction of apoptosis. Co-delivery of these two RNAs has a synergistic effect on halting tumor growth compared to single gene delivery[86].
Low-density lipoprotein receptors
HCC is frequently associated with paraneoplastic hypercholesterolemia. In familial hypercholesterolemia, the genetic mutation of low-density lipoprotein (LDL) receptor gene has been recognized as a pathogenesis of the disease[87].
In the study conducted by Chang et al[88], hematoporphyrin was used as an LDL target and photo-sensitizing agent in the treatment of HCC. Hematoporphyrin modified bovine serum albumin NPs were loaded with DOX. The designed NPs were evaluated in vitro on HepG2 cells and in vivo on mice inoculated by HCC. In both cases, efficacy was enhanced according to photodynamic toxicity session and eradiation time.
Cholestrol can also target LDL receptors. Therefore, a nanocomplex consisting of soybean phospholipids and cholesterol conjugated siRNA (Chol-siRNA) for Pokemon gene silencing mediated by reconstituted HDL (rHDL) for targeting HepG2 liver cancer cells was prepared. Pokemone protein is held responsible for oncogenesis in liver cells in vivo. NPs have a sustained release kinetic and highly efficient and specific delivery to HepG2 cell line. The in vitro studies have shown significant cell growth inhibition and reduction of Pokemon and Bcl-2 proteins (responsible for the inhibition of cell apoptosis) in the treated cells, whereas in vivo studies have demonstrated high uptake of carriers by tumor cells of HCC bearing nude mice upon iv administration as well as significant cell growth inhibition. Hereby rHDL is suggested as a superior liver cell delivery vector, which facilitates the specific transfection with siRNA[89].
Another reported delivery system which can target LDL receptors is the sterol containing solid lipid nanoparticles (SLNs) that is used for quercetin delivery, a potential chemotherapeutic drug. Low solubility of quercetin seriously limits its clinical use. Therefore, SLNs are designed for enhancing its cellular penetration using cholesterol analogues, i.e., sterols which make bilayers fluent for targeting HCC cells. Three sterol types including cholesterol, stigmasterol, and stigmastanol are used for the preparation of quercetin SLNs by emulsification solvent evaporation method. The IC50 of quercetin in cholesterol containing SLNs is about six and twice less than the free drug and phytosterol containing SLNs, respectively, and it causes more accumulation of the drug in HepG2 cells[90].
Ganglioside GM1 cell surface ligand
The branched pentasaccharide chain of ganglioside GM1 is a prominent cell surface ligand, for example, for cholera toxin or tumor growth-regulatory homodimeric galectins[91]. Zhao et al[92] used heat-liable enterotoxin subunit B (LTB) as a ganglioside GM1 binding ligand for the targeted treatment of HCC. NPs of the mixture of LTB and bovine serum albumin are prepared and their internalization to hepatocellular cancer cell line SMMC-7721 is tested. 5-FU is loaded in these NPs and cytotoxicity is proved to be much higher than that of the untargeted NPs.
EGFR receptors
Hyperthermia is almost always used along with other forms of cancer therapy, such as radiation therapy and chemotherapy. Hyperthermia may make some cancer cells more sensitive to radiation or harm other cancer cells that cannot be damaged by radiation. There are 2 very different types of hyperthermia: local hyperthermia or thermal ablation in which very high temperatures are used for destroying a small area of cells, such as a tumor. The other way is regional hyperthermia or whole-body hyperthermia in which the temperature of a part of the body (or even the whole body) is raised to a few degrees higher than normal. This type of hyperthermia helps other cancer treatments such as radiation, immunotherapy, or chemotherapy work properly. Local hyperthermia is most commonly done using high-energy radio waves and, consequently, is named RFA to treat tumors up to about 2 inches (5 cm) across. This method is used for the patients in whom surgery is not possible to remove the tumor or for those who have recurrent tumors. It can also be added to other treatments like surgery, radiation therapy, chemotherapy, hepatic arterial infusion therapy, alcohol ablation, or chemoembolization. In this technique, a thin, needle-like probe is put into the tumor for about 10 to 30 min under the guidance of ultrasound, MRI, or CT scans. The high-frequency current produced in the tip of the probe creates heat between 122 °F-212 °F, which destroys the cells within the affected tumor area[93]. In this regard, Raoof et al[94] produced some gold NPs loaded with anticancer drug gemcitabin and tested them on the xenograft model of HCC. They used EGFR for the targeted delivery of gemcitabin. As mentioned before, this receptor is expressed on some HCC cell lines such as Hep3B and is specifically targeted by cetuximab as a monoclonal antibody. Using radiofrequency (RF), it induces a non-invasive hyperthermia in targeted cells, but not in normal cells, which results in reduced growth and induction of apoptosis. This study suggests that an Au NP-gemcitabin system could be as effective as the conventional dosage of gemcitabine, but with the almost 275 times less dosage.
VEGF, a sub-family of growth factors, is a signal protein produced by the cells that stimulate vasculogenesis and angiogenesis. When VEGF is over-expressed, it can contribute to the disease. Solid cancers cannot grow beyond a limited size without an adequate blood supply; cancers that can express VEGF are able to grow and metastasize. The influence of siRNA-VEGF on endothelial cell proliferation, apoptosis, and tube formation was analyzed in vitro by Raskopf et al[28]. Their results showed that two days after transfection, the VEGF expression was inhibited 70% in Hepa129 and 48% in SVEC4-10 cell lines. In vitro endothelial cell proliferation and tube formation were reduced by 23% and 38%, respectively. Reduced pAKT in hepatoma cells interfered in VEGF signaling. Intraperitoneal application of siRNA-VEGF inhibited the tumor growth by 83% or 63% in orthotopic tumors within 14 d. VEGF protein was reduced in both models by 29% and 44%. Microvessel density dropped to 34% for the tumors from ex vivo transfected cells and 39% for systemic treated tumors.
Human VEGF (hVEGF) siRNA was labeled with 131I using the Bolton-Hunter method and conjugated to a type of SPIOs named SilenceMag. Nude mice with HCC tumors were injected subcutaneously with 131I-hVEGF siRNA/SilenceMag and were then exposed to an external magnetic field (EMF). External application of an EMF attracted and retained more 131I-hVEGF siRNA/SilenceMag in HCC tumors as shown by MRI and biodistribution studies. The tumors treated with 131I-hVEGF siRNA/SilenceMag grew nearly 50% slower in the presence of EMF than those without EMF and the control. Immunohistochemical assay confirmed that the tumor targeted by 131I-hVEGF siRNA/SilenceMag guided by an EMF had a lower VEGF protein level than the one without EMF exposure and the control. The synergic therapy of 131I-hVEGF siRNA/SilenceMag might be a promising future treatment option against HCC with the dual functional properties of tumor therapy and imaging[95].
Specific surface antigens targeted by monoclonal antibodies
One of the most successful therapeutic strategies for solid tumors and hematologic malignancies is based on treatment with the monoclonal antibodies of cancer in the last 20 years. For cancer cell surface antigen discovery, a combination of serological techniques with hybridoma technology leads to a series of landmark clinical trials that paves the way for new generation antibodies and subsequent clinical success. Therapeutic monoclonal antibodies target specific antigens found on the cell surface, such as transmembrane receptors or extracellular growth factors. In some cases, monoclonal antibodies are conjugated to radio-isotopes or toxins to allow the specific delivery of these cytotoxic agents to the intended cancer cell target. One of these therapeutic monoclonal antibodies is Sorafenib (Nexavar), which targets VEGFR, PDGFR, KIT, and RAF antigens and is FDA approved for HCC. Another antibody with specificity for liver tumor cells is SM5-1 which is a humanized mouse antibody. NPs of PLGA are prepared, conjugated with SM5-1, and loaded with 5-fluorouracil. They are then tested in vitro and in vivo on subcutaneous and liver tumor HCC-LM3-fLuc cells. In both occasions, the targeted NPs have better efficacy in terms of inhibiting tumor cell growth[96].
Another reported antibody targeted NPs used to specifically target HCC was designed by Wang et al[97] who prepared a liposomal NP, mediated by CD44 antibody and loaded with herpes simples virus-truncated thymidine kinase (HSV-ttk), renilla luciferase (Rluc), and red fluorescent protein (RFP) in an attempt to evaluate targeting efficacy by non-invasive molecular imaging. HepG2 cells were injected into the liver of NOD/SCID mice to model in situ liver cancer. Then, the growth status of tumor was monitored.
Retinoic acid receptors
Retinoid analogues have been reported to inhibit the growth of HCC. They strongly affect embryogenesis and carcinogenesis. The biological activity of retinoids is exerted through binding to specific nuclear receptors in the steroid/thyroid hormone family. Two major classes of retinoid receptors, RARs and retinoic X, have been identified, each of which consists of three distinct receptor subtypes: α, β, and γ[98]. Retinoic acid receptor-α, is reported as the dominant receptor in HCC and its mRNA has been shown to be at low levels in the normal liver, but at high levels in HCC[52,99]. Retinoic acid is a derivative of vitamin A with an important role in the regulation of cell proliferation and differentiation[100] and its inhibitory effect on cancer cell growth is well established[101-104]. This receptor has been used to target doxorubicin in HCC by Varshosaz et al[105]. They graft retinoic acid to chitosan and synthesize copolymers with different degrees of substitution of retinoic acid on the chitosan. Then, the conjugate of retinoic acid-chitosan is grafted to albumin NPs for the targeted delivery of doxorubicin in HCC. NPs are produced by coacervation method. Cytotoxicity of doxorubicin loaded NPs on HepG2 cells using MTT assay shows that IC50 of drug loaded in these NPs is reduced to half and one third compared to the non-targeted NPs and free drug, respectively.
Integrin receptors targeted by Arg-Gly-Asp peptide
The tripeptide Arg-Gly-Asp (RGD) was originally identified as the sequence within fibronectin that mediates cell attachment. This tripeptide has been found in numerous proteins, including integrins, a family of cell-surface proteins, which act as receptors for cell adhesion molecules. RGD adheres to integrin receptors, especially αvβ3 and αvβ5, which are over-expressed on the angiogenic endothelium in diseased tissues and various malignant tumors. RGD sequence is the cell attachment site of a large number of adhesive extracellular matrix (ECM), blood and cell surface proteins, and nearly half of more than 20 known integrins recognize this sequence in their adhesion protein ligands. Integrins are transmembrane receptors which act like bridges for cell-cell and ECM interactions. When integrins are triggered, chemical pathways to the interior are activated. Some of these signals include chemical composition and mechanical status of ECM, which result in a response such as the regulation of cell cycle, cell shape, and/or motility or new receptors are added to the cell membrane. This issue allows rapid and flexible responses to events at the cell surface, for example, signal platelets to initiate an interaction with coagulation factors. Proteins that contain RGD attachment site, together with the integrins that serve as receptors for them, constitute a major recognition system for cell adhesion. When RGD peptides are insolubilized onto a surface, they can promote cell adhesion and inhibit it when presented to cells in solution. There are several types of integrins which may be present on the cell surface. Fibronectin, vitronectin, collagen, and laminin (http://en.wikipedia.org/wiki/Ligands) are some of the common ligands for integrins[106]. The binding of a subset of the integrins which recognizes RGD motif within their ligands mediates both cell-substratum and cell-cell interactions. By cyclizing peptides with the selected sequences around the RGD and by synthesizing RGD mimics, it is possible to design reagents that bind selectively to only one or a few of the RGD-directed integrins. Integrin-mediated cell attachment influences and regulates many functions in various biological systems such as cell migration, growth, differentiation, and apoptosis. Therefore, drug design based on RGD structure may provide new treatments for diseases such as thrombosis, osteoporosis, and cancer[107].
Dual-ligand system may possess a synergistic effect and create a more ideal drug delivery effect. Based on the above factors, Mei et al[108] designed a multistage liposome system co-modified by RGD, TAT peptide, and cleavable PEG, which combined the advantages of PEG, specific ligand, and penetrating peptide (TAT). TAT is the basic region of the trans-activating transcriptional activator protein from HIV-1[109], which is able to transport different molecules and even 200 nm nanocarriers across biological barriers to be taken up by various cell lines like HCC[110,111]. The cleavable PEG could increase the stability and circulation time of liposomes during circulation. After the passive extravasation to tumor tissues, RGD specifically recognizes the integrins over-expressed on HepG2 cells of HCC and mediates efficient internalization in the synergistic effect of RGD and TAT. In vitro cellular uptake and 3D tumor spheroid penetration studies have demonstrated that the system could not only be selectively and efficiently taken up by the cells’ over-expressing integrins, but also penetrate into the tumor cells to reach the depths of the avascular tumor spheroids. In vivo imaging and fluorescent images of tumor section have further demonstrated that this system achieves profoundly improved distribution within tumor tissues.
Studies of Cai et al[112] demonstrated that the targeting of RGD-coupled to poly(ethylene glycol)-modified stearic acid-grafted chitosan (PEG-CS-SA) micelles to HCC tumor vasculature is a promising strategy for tumor-targeting treatment. DOX was entrapped in the micelles as a model anticancer drug. Qualitative and quantitative analyses of drug-loaded RGD-PEG-CS-SA micelles indicated significant increase of cellular uptake of DOX in HCC cell line (BEL-7402) that over-expressed integrins ανβ3 and ανβ5, but not in human epithelial carcinoma cell line (Hela). The competitive cellular-uptake test showed that the cellular uptake of RGD-modified micelles in BEL-7402 cells was significantly inhibited in the presence of excess free RGD peptides. In vitro cytotoxicity tests demonstrated that DOX-loaded RGD-modified micelles could specifically enhance cytotoxicity against BEL-7402 compared to DOX-loaded PEG-CS-SA and free DOX.
Carboxy methyl cellulose-magnetic NPs have been synthesized using epithelial cell adhesion molecule (EpCAM) as a target on HCC cells. The in vitro MR imaging shows a higher uptake of the targeted magnetic NPs by cancer cells. DOX is loaded to these NPs and the accumulation of DOX in cancer cells is proved higher than that of free DOX or untargeted NPs. This nanoprobe is suggested to be useful for the delivery of therapeutics and imaging compounds[113].
PEG is grafted to polyethylenimine (PEI), modified by RGD tripeptide and functionalized by super paramagnetic iron oxide NPs (RGD-PEG-g-PEI-SPION) for the targeted delivery of Survivin siRNA to human HCC cell line Bel-7402. RGD conjugated NPs have higher efficacy in silencing Survivin gene in cancer cells compared to the non-targeted carriers. This gene suppression in conjunction with induced cell apoptosis leads to tumor growth inhibition in the mouse model of HCC. The SPION functionalized NPs also allow for the efficacious MIR imaging of targeted cells in vitro and in vivo, which suggests that this specific carrier might be a potential candidate for imaging and treatment purposes in human HCC[114].
Degradable and biocompatible building blocks of amphiphilic derivatives of poly(benzyl malate) are synthesized for the production of functional NPs bearing biotin molecules for the targeted delivery of an anti-cancer model drug, DOX. These NPs target the biotin receptors over-expressed on the surface of several cancer cells. Some of these biotinylated NPs are grafted to cyclic RGD peptide to produce biotinylated cyclic RGD NPs using the strong and highly specific interactions between biotin and the streptavidin protein. The fluorescent NPs grafted with cyclic RGD had A more efficient uptake by the HepaRG hepatoma cells compared to biotinylated fluorescent NPs. Furthermore, the targeting of HepaRG hepatoma cells with NPs bearing cyclic RGD is a very efficient and suitable targeting agent for liver cells[115]. Figure 3 shows the schematic representation of the biotinylated cyclic RGD NPs loaded with DOX.
Figure 3.
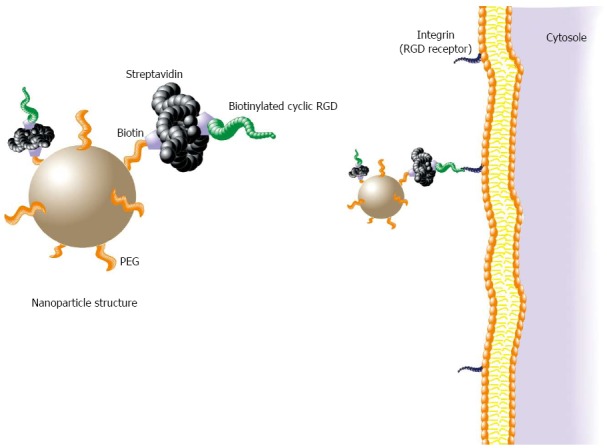
Schematic representation of the biotinylated cyclic Arg-Gly-Asp nanoparticles loaded with doxorubicin. PEG: Polyethylene glycol; RGD: Arg-Gly-Asp.
Knocking down of integrin subunits slows down the progression of HCC, which is due to the significant retardation of HCC progression, reduced proliferation, and increased tumor cell death accompanied by the reduced activation of the MET oncogene as well as expression of its mature form on the cell surface. MET is a receptor tyrosine kinase located at the membrane that is essential for embryonic development and wound healing. Hepatocyte growth factor (HGF) is the only known ligand of the MET receptor. MET is normally expressed by the cells of epithelial origin, while HGF expression is restricted to the cells of mesenchymal origin. Upon HGF stimulation, MET induces several biological responses that collectively give rise to a program known as invasive growth. Transformed proliferating cells from HCC are more sensitive to the knock-down of integrins than normal hepatocytes, which highlights the potential of small interfering RNA-mediated inhibition of integrins as an anti-cancer therapeutic approach. All integrin receptors in hepatocytes are down-regulated using the nanoparticulate delivery of short interfering RNAs targeting β1 and αv integrin subunits. Short-term (2 wk) integrin knock-down does not cause apparent structural or functional perturbations of normal liver tissue. However, sustained integrin down-regulation for 7 wk alters liver morphology[116].
Folate receptors
Folate is a basic component of cell metabolism, DNA synthesis, and repair, and rapidly dividing cancer cells have an increased requirement for folate to maintain DNA synthesis, an observation supported by the widespread use of antifolates in cancer chemotherapy. Because folate receptors (FR) are over-expressed in tumor cells, folate is frequently conjugated with different nanocarriers like polymeric micelles for targeted drug delivery to improve drug efficacy and safety of antitumor drugs[117,118]. FR is a glycosyl phosphatidinositol-anchored membrane protein which is over-expressed in 90% ovarian carcinomas and many types of other epithelial cancers like HCC. Folate receptors (FRα, FRβ, and FRγ) are cysteine-rich cell-surface glycoproteins that bind folate with high affinity to mediate the cellular uptake of folate[119-123].
The expression levels of FR in normal tissues are much lower than in tumor tissues. FRα are especially expressed at high levels in numerous cancers to meet the folate demand of rapidly dividing cells under low folate conditions. FR is an ideal target for drug delivery thanks to its distinct expression between normal and malignant tissues. Folate dependency of many tumors has been therapeutically and diagnostically exploited by the administration of anti-FRα antibodies, high-affinity antifolates, folate-based imaging agents, and folate-conjugated drugs and toxins. Folate, the natural ligand of FR, has been extensively investigated for chemotherapeutic NP delivery considering its inherent high affinity, small size, and non-toxicity[124-127].
The effect of targeted folate-functionalized polyethyleneglycol-block-poly (e-caprolactone) (PEG-PCL) micelles containing superparamagnetic iron oxide NPs (SPIONs) and sorafenib on the human hepatic carcinoma (HepG2) cells has been studied in vitro to observe the feasibility of the surveillance of this targeting therapeutic effect by magnetic resonance imaging. Magnetic resonance imaging using a clinical 1.5 T scanner is performed to detect changes in the signal intensity of cells after incubation with the targeted micelles. The apoptotic rate in the targeted cells is significantly higher than that in the non-targeted cells (P = 0.043). The T2 signal intensity on magnetic resonance imaging of the cells treated with the targeted micelles is significantly decreased with increasing the concentrations of sorafenib in the cell culture medium; but, there is no obvious decrease in signal intensity in the cells treated with the non-targeted micelles. The results of this study show that polymeric micelles functionalized with folate and loaded with SPIONs and sorafenib inhibit proliferation and induce the apoptosis in HepG2 cells in vitro. The inhibitory events caused by targeted micelles could be monitored using magnetic resonance[128].
Although the expression of FR on HCC has been proved and its different cell lines like Bel-7402[129-131], Hep3B[132], PLC/PRF/5[133], and HepG2[134,135] have been reported to be FR positive, the last one is controversial and, in some references, it has been used as a FR negative cell line. For example, biodegradable DTX lipid-based nanosuspension (LNS) prepares as the base nanocarrier system. NPs of LNS which are loaded with DTX are either conjugated with folate (fLNS) or coated with PEG (pLNS). These two nanocarriers are tested on the tumor cell line of B16 as an over-expressing folate receptor (FR+) and HepG2 as its under-expressing (FR-). In vitro studies have shown no difference between the antitumor effect of tLNS and pLNS in HepG2 cells, whereas in vivo studies in B16 bearing mice have demonstrated a higher tumor inhibition level with fLNS compared to pLNS and free agent. Expectedly, the uptake of fLNS is found to be higher after biodistribution studies[136].
Transferrin receptors
Cytotoxicity enhancement of two synthetic derivatives of temozolomide encapsulated in nanostructured lipid carriers (NLC) has been demonstrated for HCC cell lines of HuH-6 and HuH-7[137]. Two types of NPs were designed by Krishna et al[138]: one was the NPs of apotransferrin and the second was BSA conjugated to apotransferrin. Both were loaded with DOX and comparative studies were performed. The direct NPs of apotransferrin had a higher uptake by HCC cell’s nucleus, even though both were efficiently internalized by TfR mediated endocytosis. The direct nanodrug showed an improved circulation and kinetic via intraperitoneal route and reduced the drug accumulation in the heart via iv route; therefore, lower DOX related cardiotoxicity was seen.
Decreased cardiotoxicity of DOX has been also reported by apotransferrin and lactoferrin modified NPs loaded with DOX which are applied in the rat HCC model induced by diethylnitrosamine. Enhancement of drug bioavailability and efficacy in a target-specific mode is also achieved by these NPs[139]. Apo-human serum transferrin coupled with cisplatin could specifically deliver cisplatin to HepG2 cells in vitro, minimize the side-effects, and then stimulate apoptosis[140].
In the study by Malarvizhi et al[141], DOX was loaded to poly(vinyl alcohol) nano-cores and sorafenib was encapsulated in albumin nanoshell over the nanocore. Sofarenib inhibited the oncogenic signaling and hence a cytostatic effect, while DOX resulted in cytotoxicity. When targeted with transferrin ligand, the cellular uptake and cytotoxicity were enhanced. This core-shell nanoparticle with two relevant medications caused synergistic anti-cancer effects for the treatment of liver cancer.
CONCLUSION AND OUTLOOK
In this article, we highlighted the recent progress of utilizing targeted NPs as delivery system for therapeutic agents and siRNA in the treatment of HCC. According to these studies, targeted NPs have the potential to be used in the delivery of therapeutic agents to the tumor and effective delivery of siRNA to silence the corresponding genetic component involved in this disease. Various materials are used in modifying the physicochemical properties of targeted NPs to increase their stability, loading efficiency, and intracellular delivery, which have led to efficient targeted drug delivery and gene silencing. To prolong blood circulation time, the pegylated version of these nanocarriers can be developed. Surface functionalizing with targeting moiety has been shown to increase tissue accumulation and reduce adverse effects. Great efforts have been made to the coupling of polymer chains to NPs, especially in the context of the so-called bioconjugation for biomedical applications. On the contrary, few works have been reported on the attachment of NPs with different natures for functionalizing agents for efficient co-delivery of siRNA and therapeutic agents. This field certainly needs to be further explored in the upcoming years in order to open very interesting possibilities for the preparation of novel materials through the assembly of functionalized NPs as nonviral inorganic/organic hybrid carriers. At the same time, the pharmacokinetic, pharmacodynamics, safety, and toxicity profiles of these carriers should be considered in preclinical and clinical studies to prove the efficacy of these materials as effective non-viral vectors in gene delivery.
Footnotes
Conflict-of-interest statement: The authors report no conflict of interest.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: May 6, 2015
First decision: June 23, 2015
Article in press: September 30, 2015
P- Reviewer: Zhang L S- Editor: Yu J L- Editor: A E- Editor: Liu XM
References
- 1.Gomaa AI, Khan SA, Toledano MB, Waked I, Taylor-Robinson SD. Hepatocellular carcinoma: epidemiology, risk factors and pathogenesis. World J Gastroenterol. 2008;14:4300–4308. doi: 10.3748/wjg.14.4300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bosch FX, Ribes J, Cléries R, Díaz M. Epidemiology of hepatocellular carcinoma. Clin Liver Dis. 2005;9:191–211, v. doi: 10.1016/j.cld.2004.12.009. [DOI] [PubMed] [Google Scholar]
- 3.Altekruse SF, Henley SJ, Cucinelli JE, McGlynn KA. Changing hepatocellular carcinoma incidence and liver cancer mortality rates in the United States. Am J Gastroenterol. 2014;109:542–553. doi: 10.1038/ajg.2014.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.El-Serag HB, Rudolph KL. Hepatocellular carcinoma: epidemiology and molecular carcinogenesis. Gastroenterology. 2007;132:2557–2576. doi: 10.1053/j.gastro.2007.04.061. [DOI] [PubMed] [Google Scholar]
- 5.Bruix J, Llovet JM. Prognostic prediction and treatment strategy in hepatocellular carcinoma. Hepatology. 2002;35:519–524. doi: 10.1053/jhep.2002.32089. [DOI] [PubMed] [Google Scholar]
- 6.Llovet JM, Burroughs A, Bruix J. Hepatocellular carcinoma. Lancet. 2003;362:1907–1917. doi: 10.1016/S0140-6736(03)14964-1. [DOI] [PubMed] [Google Scholar]
- 7.Befeler AS, Di Bisceglie AM. Hepatocellular carcinoma: diagnosis and treatment. Gastroenterology. 2002;122:1609–1619. doi: 10.1053/gast.2002.33411. [DOI] [PubMed] [Google Scholar]
- 8.Trevisani F, De Notariis S, Rapaccini G, Farinati F, Benvegnù L, Zoli M, Grazi GL, Del PP, Di N, Bernardi M. Semiannual and annual surveillance of cirrhotic patients for hepatocellular carcinoma: effects on cancer stage and patient survival (Italian experience) Am J Gastroenterol. 2002;97:734–744. doi: 10.1111/j.1572-0241.2002.05557.x. [DOI] [PubMed] [Google Scholar]
- 9.Zhang B, Yang B. Combined alpha fetoprotein testing and ultrasonography as a screening test for primary liver cancer. J Med Screen. 1999;6:108–110. doi: 10.1136/jms.6.2.108. [DOI] [PubMed] [Google Scholar]
- 10.Bruix J, Hessheimer AJ, Forner A, Boix L, Vilana R, Llovet JM. New aspects of diagnosis and therapy of hepatocellular carcinoma. Oncogene. 2006;25:3848–3856. doi: 10.1038/sj.onc.1209548. [DOI] [PubMed] [Google Scholar]
- 11.Forner A, Hessheimer AJ, Isabel Real M, Bruix J. Treatment of hepatocellular carcinoma. Crit Rev Oncol Hematol. 2006;60:89–98. doi: 10.1016/j.critrevonc.2006.06.001. [DOI] [PubMed] [Google Scholar]
- 12.Bruix J, Sherman M. Management of hepatocellular carcinoma. Hepatology. 2005;42:1208–1236. doi: 10.1002/hep.20933. [DOI] [PubMed] [Google Scholar]
- 13.Chlebowski RT, Brzechwa-Adjukiewicz A, Cowden A, Block JB, Tong M, Chan KK. Doxorubicin (75 mg/m2) for hepatocellular carcinoma: clinical and pharmacokinetic results. Cancer Treat Rep. 1984;68:487–491. [PubMed] [Google Scholar]
- 14.Nerenstone SR, Ihde DC, Friedman MA. Clinical trials in primary hepatocellular carcinoma: current status and future directions. Cancer Treat Rev. 1988;15:1–31. doi: 10.1016/0305-7372(88)90007-2. [DOI] [PubMed] [Google Scholar]
- 15.Yeo W, Mok TS, Zee B, Leung TW, Lai PB, Lau WY, Koh J, Mo FK, Yu SC, Chan AT, et al. A randomized phase III study of doxorubicin versus cisplatin/interferon alpha-2b/doxorubicin/fluorouracil (PIAF) combination chemotherapy for unresectable hepatocellular carcinoma. J Natl Cancer Inst. 2005;97:1532–1538. doi: 10.1093/jnci/dji315. [DOI] [PubMed] [Google Scholar]
- 16.Zhu AX, Blaszkowsky LS, Ryan DP, Clark JW, Muzikansky A, Horgan K, Sheehan S, Hale KE, Enzinger PC, Bhargava P, et al. Phase II study of gemcitabine and oxaliplatin in combination with bevacizumab in patients with advanced hepatocellular carcinoma. J Clin Oncol. 2006;24:1898–1903. doi: 10.1200/JCO.2005.04.9130. [DOI] [PubMed] [Google Scholar]
- 17.Kim RD, Reed AI, Fujita S, Foley DP, Mekeel KL, Hemming AW. Consensus and controversy in the management of hepatocellular carcinoma. J Am Coll Surg. 2007;205:108–123. doi: 10.1016/j.jamcollsurg.2007.02.025. [DOI] [PubMed] [Google Scholar]
- 18.Chang YS, Adnane J, Trail PA, Levy J, Henderson A, Xue D, Bortolon E, Ichetovkin M, Chen C, McNabola A, et al. Sorafenib (BAY 43-9006) inhibits tumor growth and vascularization and induces tumor apoptosis and hypoxia in RCC xenograft models. Cancer Chemother Pharmacol. 2007;59:561–574. doi: 10.1007/s00280-006-0393-4. [DOI] [PubMed] [Google Scholar]
- 19.Wilhelm SM, Carter C, Tang L, Wilkie D, McNabola A, Rong H, Chen C, Zhang X, Vincent P, McHugh M, et al. BAY 43-9006 exhibits broad spectrum oral antitumor activity and targets the RAF/MEK/ERK pathway and receptor tyrosine kinases involved in tumor progression and angiogenesis. Cancer Res. 2004;64:7099–7109. doi: 10.1158/0008-5472.CAN-04-1443. [DOI] [PubMed] [Google Scholar]
- 20.Zhang T, Ding X, Wei D, Cheng P, Su X, Liu H, Wang D, Gao H. Sorafenib improves the survival of patients with advanced hepatocellular carcinoma: a meta-analysis of randomized trials. Anticancer Drugs. 2010;21:326–332. doi: 10.1097/CAD.0b013e3283350e26. [DOI] [PubMed] [Google Scholar]
- 21.Siegel AB, Cohen EI, Ocean A, Lehrer D, Goldenberg A, Knox JJ, Chen H, Clark-Garvey S, Weinberg A, Mandeli J, et al. Phase II trial evaluating the clinical and biologic effects of bevacizumab in unresectable hepatocellular carcinoma. J Clin Oncol. 2008;26:2992–2998. doi: 10.1200/JCO.2007.15.9947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Huether A, Höpfner M, Sutter AP, Schuppan D, Scherübl H. Erlotinib induces cell cycle arrest and apoptosis in hepatocellular cancer cells and enhances chemosensitivity towards cytostatics. J Hepatol. 2005;43:661–669. doi: 10.1016/j.jhep.2005.02.040. [DOI] [PubMed] [Google Scholar]
- 23.Zhu AX, Sahani DV, Duda DG, di Tomaso E, Ancukiewicz M, Catalano OA, Sindhwani V, Blaszkowsky LS, Yoon SS, Lahdenranta J, et al. Efficacy, safety, and potential biomarkers of sunitinib monotherapy in advanced hepatocellular carcinoma: a phase II study. J Clin Oncol. 2009;27:3027–3035. doi: 10.1200/JCO.2008.20.9908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Llovet JM, Bruix J. Novel advancements in the management of hepatocellular carcinoma in 2008. J Hepatol. 2008;48 Suppl 1:S20–S37. doi: 10.1016/j.jhep.2008.01.022. [DOI] [PubMed] [Google Scholar]
- 25.Devi GR. siRNA-based approaches in cancer therapy. Cancer Gene Ther. 2006;13:819–829. doi: 10.1038/sj.cgt.7700931. [DOI] [PubMed] [Google Scholar]
- 26.Lee YH, Judge AD, Seo D, Kitade M, Gómez-Quiroz LE, Ishikawa T, Andersen JB, Kim BK, Marquardt JU, Raggi C, et al. Molecular targeting of CSN5 in human hepatocellular carcinoma: a mechanism of therapeutic response. Oncogene. 2011;30:4175–4184. doi: 10.1038/onc.2011.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li K, Lin SY, Brunicardi FC, Seu P. Use of RNA interference to target cyclin E-overexpressing hepatocellular carcinoma. Cancer Res. 2003;63:3593–3597. [PubMed] [Google Scholar]
- 28.Raskopf E, Vogt A, Sauerbruch T, Schmitz V. siRNA targeting VEGF inhibits hepatocellular carcinoma growth and tumor angiogenesis in vivo. J Hepatol. 2008;49:977–984. doi: 10.1016/j.jhep.2008.07.022. [DOI] [PubMed] [Google Scholar]
- 29.Zhao Y, Jian W, Gao W, Zheng YX, Wang YK, Zhou ZQ, Zhang H, Wang CJ. RNAi silencing of c-Myc inhibits cell migration, invasion, and proliferation in HepG2 human hepatocellular carcinoma cell line: c-Myc silencing in hepatocellular carcinoma cell. Cancer Cell Int. 2013;13:23. doi: 10.1186/1475-2867-13-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Scaggiante B, Kazemi M, Pozzato G, Dapas B, Farra R, Grassi M, Zanconati F, Grassi G. Novel hepatocellular carcinoma molecules with prognostic and therapeutic potentials. World J Gastroenterol. 2014;20:1268–1288. doi: 10.3748/wjg.v20.i5.1268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Li L, Wang R, Wilcox D, Sarthy A, Lin X, Huang X, Tian L, Dande P, Hubbard RD, Hansen TM, et al. Developing lipid nanoparticle-based siRNA therapeutics for hepatocellular carcinoma using an integrated approach. Mol Cancer Ther. 2013;12:2308–2318. doi: 10.1158/1535-7163.MCT-12-0983-T. [DOI] [PubMed] [Google Scholar]
- 32.Doan CC, Doan NT, Nguyen QH, Nguyen MH, Do MS, Le VD. Downregulation of Kinesin spindle protein inhibits proliferation, induces apoptosis and increases chemosensitivity in hepatocellular carcinoma cells. Iran Biomed J. 2015;19:1–16. doi: 10.6091/ibj.1386.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhang L, He T, Cui H, Wang Y, Huang C, Han F. Effects of AFP gene silencing on apoptosis and proliferation of a hepatocellular carcinoma cell line. Discov Med. 2012;14:115–124. [PubMed] [Google Scholar]
- 34.Li H, Fu X, Chen Y, Hong Y, Tan Y, Cao H, Wu M, Wang H. Use of adenovirus-delivered siRNA to target oncoprotein p28GANK in hepatocellular carcinoma. Gastroenterology. 2005;128:2029–2041. doi: 10.1053/j.gastro.2005.03.001. [DOI] [PubMed] [Google Scholar]
- 35.Steichen SD, Caldorera-Moore M, Peppas NA. A review of current nanoparticle and targeting moieties for the delivery of cancer therapeutics. Eur J Pharm Sci. 2013;48:416–427. doi: 10.1016/j.ejps.2012.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Soll C, Riener MO, Oberkofler CE, Hellerbrand C, Wild PJ, DeOliveira ML, Clavien PA. Expression of serotonin receptors in human hepatocellular cancer. Clin Cancer Res. 2012;18:5902–5910. doi: 10.1158/1078-0432.CCR-11-1813. [DOI] [PubMed] [Google Scholar]
- 37.Li YH, Liu Y, Li YD, Liu YH, Li F, Ju Q, Xie PL, Li GC. GABA stimulates human hepatocellular carcinoma growth through overexpressed GABAA receptor theta subunit. World J Gastroenterol. 2012;18:2704–2711. doi: 10.3748/wjg.v18.i21.2704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Qiu WH, Zhou BS, Chu PG, Chen WG, Chung C, Shih J, Hwu P, Yeh C, Lopez R, Yen Y. Over-expression of fibroblast growth factor receptor 3 in human hepatocellular carcinoma. World J Gastroenterol. 2005;11:5266–5272. doi: 10.3748/wjg.v11.i34.5266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Buckley AF, Burgart LJ, Sahai V, Kakar S. Epidermal growth factor receptor expression and gene copy number in conventional hepatocellular carcinoma. Am J Clin Pathol. 2008;129:245–251. doi: 10.1309/WF10QAAED3PP93BH. [DOI] [PubMed] [Google Scholar]
- 40.Abdel-Rahman O, Lamarca A, Valle JW, Hubner RA. Somatostatin receptor expression in hepatocellular carcinoma: prognostic and therapeutic considerations. Endocr Relat Cancer. 2014;21:R485–R493. doi: 10.1530/ERC-14-0389. [DOI] [PubMed] [Google Scholar]
- 41.Chettouh H, Fartoux L, Aoudjehane L, Wendum D, Clapéron A, Chrétien Y, Rey C, Scatton O, Soubrane O, Conti F, et al. Mitogenic insulin receptor-A is overexpressed in human hepatocellular carcinoma due to EGFR-mediated dysregulation of RNA splicing factors. Cancer Res. 2013;73:3974–3986. doi: 10.1158/0008-5472.CAN-12-3824. [DOI] [PubMed] [Google Scholar]
- 42.Bai X, Wang J, Guo Y, Pan J, Yang Q, Zhang M, Li H, Zhang L, Ma J, Shi F, et al. Prostaglandin E2 stimulates β1-integrin expression in hepatocellular carcinoma through the EP1 receptor/PKC/NF-κB pathway. Sci Rep. 2014;4:6538. doi: 10.1038/srep06538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Xiang HJ, Liu ZC, Wang DS, Chen Y, Yang YL, Dou KF. Adenosine A(2b) receptor is highly expressed in human hepatocellular carcinoma. Hepatol Res. 2006;36:56–60. doi: 10.1016/j.hepres.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 44.Chun YS, Huang M, Rink L, Von Mehren M. Expression levels of insulin-like growth factors and receptors in hepatocellular carcinoma: a retrospective study. World J Surg Oncol. 2014;12:231. doi: 10.1186/1477-7819-12-231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Shi B, Abrams M, Sepp-Lorenzino L. Expression of asialoglycoprotein receptor 1 in human hepatocellular carcinoma. J Histochem Cytochem. 2013;61:901–909. doi: 10.1369/0022155413503662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ma WL, Lai HC, Yeh S, Cai X, Chang C. Androgen receptor roles in hepatocellular carcinoma, fatty liver, cirrhosis and hepatitis. Endocr Relat Cancer. 2014;21:R165–R182. doi: 10.1530/ERC-13-0283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kelemen LE. The role of folate receptor alpha in cancer development, progression and treatment: cause, consequence or innocent bystander? Int J Cancer. 2006;119:243–250. doi: 10.1002/ijc.21712. [DOI] [PubMed] [Google Scholar]
- 48.Högemann-Savellano D, Bos E, Blondet C, Sato F, Abe T, Josephson L, Weissleder R, Gaudet J, Sgroi D, Peters PJ, et al. The transferrin receptor: a potential molecular imaging marker for human cancer. Neoplasia. 2003;5:495–506. doi: 10.1016/s1476-5586(03)80034-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Niitsu Y, Kohgo Y, Nishisato T, Kondo H, Kato J, Urushizaki Y, Urushizaki I. Transferrin receptors in human cancerous tissues. Tohoku J Exp Med. 1987;153:239–243. doi: 10.1620/tjem.153.239. [DOI] [PubMed] [Google Scholar]
- 50.Nakamaki T, Kawabata H, Saito B, Matsunawa M, Suzuki J, Adachi D, Tomoyasu S, Phillip Koeffler H. Elevated levels of transferrin receptor 2 mRNA, not transferrin receptor 1 mRNA, are associated with increased survival in acute myeloid leukaemia. Br J Haematol. 2004;125:42–49. doi: 10.1111/j.1365-2141.2004.04866.x. [DOI] [PubMed] [Google Scholar]
- 51.Yan JJ, Liao JZ, Lin JS, He XX. Active radar guides missile to its target: receptor-based targeted treatment of hepatocellular carcinoma by nanoparticulate systems. Tumour Biol. 2015;36:55–67. doi: 10.1007/s13277-014-2855-3. [DOI] [PubMed] [Google Scholar]
- 52.Sano K, Takayama T, Murakami K, Saiki I, Makuuchi M. Overexpression of retinoic acid receptor alpha in hepatocellular carcinoma. Clin Cancer Res. 2003;9:3679–3683. [PubMed] [Google Scholar]
- 53.Lenter MC, Garidel P, Pelisek J, Wagner E, Ogris M. Stabilized nonviral formulations for the delivery of MCP-1 gene into cells of the vasculoendothelial system. Pharm Res. 2004;21:683–691. doi: 10.1023/b:pham.0000022416.33048.81. [DOI] [PubMed] [Google Scholar]
- 54.Mishra S, Webster P, Davis ME. PEGylation significantly affects cellular uptake and intracellular trafficking of non-viral gene delivery particles. Eur J Cell Biol. 2004;83:97–111. doi: 10.1078/0171-9335-00363. [DOI] [PubMed] [Google Scholar]
- 55.Ogris M, Walker G, Blessing T, Kircheis R, Wolschek M, Wagner E. Tumor-targeted gene therapy: strategies for the preparation of ligand-polyethylene glycol-polyethylenimine/DNA complexes. J Control Release. 2003;91:173–181. doi: 10.1016/s0168-3659(03)00230-x. [DOI] [PubMed] [Google Scholar]
- 56.Pun SH, Tack F, Bellocq NC, Cheng J, Grubbs BH, Jensen GS, Davis ME, Brewster M, Janicot M, Janssens B, et al. Targeted delivery of RNA-cleaving DNA enzyme (DNAzyme) to tumor tissue by transferrin-modified, cyclodextrin-based particles. Cancer Biol Ther. 2004;3:641–650. doi: 10.4161/cbt.3.7.918. [DOI] [PubMed] [Google Scholar]
- 57.Sanders NN, De Smedt SC, Cheng SH, Demeester J. Pegylated GL67 lipoplexes retain their gene transfection activity after exposure to components of CF mucus. Gene Ther. 2002;9:363–371. doi: 10.1038/sj.gt.3301663. [DOI] [PubMed] [Google Scholar]
- 58.Suh J, Wirtz D, Hanes J. Real-time intracellular transport of gene nanocarriers studied by multiple particle tracking. Biotechnol Prog. 2004;20:598–602. doi: 10.1021/bp034251y. [DOI] [PubMed] [Google Scholar]
- 59.Zahr AS, de Villiers M, Pishko MV. Encapsulation of drug nanoparticles in self-assembled macromolecular nanoshells. Langmuir. 2005;21:403–410. doi: 10.1021/la0478595. [DOI] [PubMed] [Google Scholar]
- 60.Lai SK, O’Hanlon DE, Harrold S, Man ST, Wang YY, Cone R, Hanes J. Rapid transport of large polymeric nanoparticles in fresh undiluted human mucus. Proc Natl Acad Sci USA. 2007;104:1482–1487. doi: 10.1073/pnas.0608611104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Suh J, Choy KL, Lai SK, Suk JS, Tang BC, Prabhu S, Hanes J. PEGylation of nanoparticles improves their cytoplasmic transport. Int J Nanomedicine. 2007;2:735–741. [PMC free article] [PubMed] [Google Scholar]
- 62.Xu M, Qian J, Suo A, Wang H, Yong X, Liu X, Liu R. Reduction/pH dual-sensitive PEGylated hyaluronan nanoparticles for targeted doxorubicin delivery. Carbohydr Polym. 2013;98:181–188. doi: 10.1016/j.carbpol.2013.05.077. [DOI] [PubMed] [Google Scholar]
- 63.Liu Q, Li R, Zhu Z, Qian X, Guan W, Yu L, Yang M, Jiang X, Liu B. Enhanced antitumor efficacy, biodistribution and penetration of docetaxel-loaded biodegradable nanoparticles. Int J Pharm. 2012;430:350–358. doi: 10.1016/j.ijpharm.2012.04.008. [DOI] [PubMed] [Google Scholar]
- 64.Ashley CE, Carnes EC, Phillips GK, Padilla D, Durfee PN, Brown PA, Hanna TN, Liu J, Phillips B, Carter MB, et al. The targeted delivery of multicomponent cargos to cancer cells by nanoporous particle-supported lipid bilayers. Nat Mater. 2011;10:389–397. doi: 10.1038/nmat2992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Muñoz-Gámez JA, López Viota J, Barrientos A, Carazo Á, Sanjuán-Nuñez L, Quiles-Perez R, Muñoz-de-Rueda P, Delgado Á, Ruiz-Extremera Á, Salmerón J. Synergistic cytotoxicity of the poly (ADP-ribose) polymerase inhibitor ABT-888 and temozolomide in dual-drug targeted magnetic nanoparticles. Liver Int. 2015;35:1430–1441. doi: 10.1111/liv.12586. [DOI] [PubMed] [Google Scholar]
- 66.Cheng M, Gao X, Wang Y, Chen H, He B, Xu H, Li Y, Han J, Zhang Z. Synthesis of glycyrrhetinic acid-modified chitosan 5-fluorouracil nanoparticles and its inhibition of liver cancer characteristics in vitro and in vivo. Mar Drugs. 2013;11:3517–3536. doi: 10.3390/md11093517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Zu Y, Meng L, Zhao X, Ge Y, Yu X, Zhang Y, Deng Y. Preparation of 10-hydroxycamptothecin-loaded glycyrrhizic acid-conjugated bovine serum albumin nanoparticles for hepatocellular carcinoma-targeted drug delivery. Int J Nanomedicine. 2013;8:1207–1222. doi: 10.2147/IJN.S40493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Shi L, Tang C, Yin C. Glycyrrhizin-modified O-carboxymethyl chitosan nanoparticles as drug vehicles targeting hepatocellular carcinoma. Biomaterials. 2012;33:7594–7604. doi: 10.1016/j.biomaterials.2012.06.072. [DOI] [PubMed] [Google Scholar]
- 69.Zhang L, Yao J, Zhou J, Wang T, Zhang Q. Glycyrrhetinic acid-graft-hyaluronic acid conjugate as a carrier for synergistic targeted delivery of antitumor drugs. Int J Pharm. 2013;441:654–664. doi: 10.1016/j.ijpharm.2012.10.030. [DOI] [PubMed] [Google Scholar]
- 70.Guo H, Lai Q, Wang W, Wu Y, Zhang C, Liu Y, Yuan Z. Functional alginate nanoparticles for efficient intracellular release of doxorubicin and hepatoma carcinoma cell targeting therapy. Int J Pharm. 2013;451:1–11. doi: 10.1016/j.ijpharm.2013.04.025. [DOI] [PubMed] [Google Scholar]
- 71.Varshosaz J, Hassanzadeh F, Sadeghi H, Khadem M. Galactosylated nanostructured lipid carriers for delivery of 5-FU to hepatocellular carcinoma. J Liposome Res. 2012;22:224–236. doi: 10.3109/08982104.2012.662653. [DOI] [PubMed] [Google Scholar]
- 72.Zhou N, Zan X, Wang Z, Wu H, Yin D, Liao C, Wan Y. Galactosylated chitosan-polycaprolactone nanoparticles for hepatocyte-targeted delivery of curcumin. Carbohydr Polym. 2013;94:420–429. doi: 10.1016/j.carbpol.2013.01.014. [DOI] [PubMed] [Google Scholar]
- 73.Zhou X, Zhang M, Yung B, Li H, Zhou C, Lee LJ, Lee RJ. Lactosylated liposomes for targeted delivery of doxorubicin to hepatocellular carcinoma. Int J Nanomedicine. 2012;7:5465–5474. doi: 10.2147/IJN.S33965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Cheng M, He B, Wan T, Zhu W, Han J, Zha B, Chen H, Yang F, Li Q, Wang W, et al. 5-Fluorouracil nanoparticles inhibit hepatocellular carcinoma via activation of the p53 pathway in the orthotopic transplant mouse model. PLoS One. 2012;7:e47115. doi: 10.1371/journal.pone.0047115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Cheng MR, Li Q, Wan T, He B, Han J, Chen HX, Yang FX, Wang W, Xu HZ, Ye T, et al. Galactosylated chitosan/5-fluorouracil nanoparticles inhibit mouse hepatic cancer growth and its side effects. World J Gastroenterol. 2012;18:6076–6087. doi: 10.3748/wjg.v18.i42.6076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Wang Q, Zhang L, Hu W, Hu ZH, Bei YY, Xu JY, Wang WJ, Zhang XN, Zhang Q. Norcantharidin-associated galactosylated chitosan nanoparticles for hepatocyte-targeted delivery. Nanomedicine. 2010;6:371–381. doi: 10.1016/j.nano.2009.07.006. [DOI] [PubMed] [Google Scholar]
- 77.Liu D, Hu H, Zhang J, Zhao X, Tang X, Chen D. Drug pH-sensitive release in vitro and targeting ability of polyamidoamine dendrimer complexes for tumor cells. Chem Pharm Bull (Tokyo) 2011;59:63–71. doi: 10.1248/cpb.59.63. [DOI] [PubMed] [Google Scholar]
- 78.Kamimoto Y, Tanabe D, Tashiro S, Hiraoka T, Miyauchi Y. Changes in receptor-mediated endocytosis in liver sinusoidal cells after partial hepatectomy in the rat. Liver. 1994;14:141–147. doi: 10.1111/j.1600-0676.1994.tb00063.x. [DOI] [PubMed] [Google Scholar]
- 79.Roseng L, Tolleshaug H, Berg T. Uptake, intracellular transport, and degradation of polyethylene glycol-modified asialofetuin in hepatocytes. J Biol Chem. 1992;267:22987–22993. [PubMed] [Google Scholar]
- 80.Becker S, Spiess M, Klenk HD. The asialoglycoprotein receptor is a potential liver-specific receptor for Marburg virus. J Gen Virol. 1995;76(Pt 2):393–399. doi: 10.1099/0022-1317-76-2-393. [DOI] [PubMed] [Google Scholar]
- 81.Chang AG, Wu GY. Gene therapy: applications to the treatment of gastrointestinal and liver diseases. Gastroenterology. 1994;106:1076–1084. doi: 10.1016/0016-5085(94)90771-4. [DOI] [PubMed] [Google Scholar]
- 82.Hara T, Kuwasawa H, Aramaki Y, Takada S, Koike K, Ishidate K, Kato H, Tsuchiya S. Effects of fusogenic and DNA-binding amphiphilic compounds on the receptor-mediated gene transfer into hepatic cells by asialofetuin-labeled liposomes. Biochim Biophys Acta. 1996;1278:51–58. doi: 10.1016/0005-2736(95)00205-7. [DOI] [PubMed] [Google Scholar]
- 83.Ishihara H, Hayashi Y, Hara T, Aramaki Y, Tsuchiya S, Koike K. Specific uptake of asialofetuin-tacked liposomes encapsulating interferon-gamma by human hepatoma cells and its inhibitory effect on hepatitis B virus replication. Biochem Biophys Res Commun. 1991;174:839–845. doi: 10.1016/0006-291x(91)91494-w. [DOI] [PubMed] [Google Scholar]
- 84.Motoyama K, Nakashima Y, Aramaki Y, Hirayama F, Uekama K, Arima H. In Vitro Gene Delivery Mediated by Asialofetuin-Appended Cationic Liposomes Associated with γ-Cyclodextrin into Hepatocytes. J Drug Deliv. 2011;2011:476137. doi: 10.1155/2011/476137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Nasr M, Nafee N, Saad H, Kazem A. Improved antitumor activity and reduced cardiotoxicity of epirubicin using hepatocyte-targeted nanoparticles combined with tocotrienols against hepatocellular carcinoma in mice. Eur J Pharm Biopharm. 2014;88:216–225. doi: 10.1016/j.ejpb.2014.04.016. [DOI] [PubMed] [Google Scholar]
- 86.Han L, Tang C, Yin C. Oral delivery of shRNA and siRNA via multifunctional polymeric nanoparticles for synergistic cancer therapy. Biomaterials. 2014;35:4589–4600. doi: 10.1016/j.biomaterials.2014.02.027. [DOI] [PubMed] [Google Scholar]
- 87.Sohda T, Iwata K, Kitamura Y, Suzuki N, Takeyama Y, Irie M, Anan A, Nakane H, Yoshikane M, Watanabe H, et al. Reduced expression of low-density lipoprotein receptor in hepatocellular carcinoma with paraneoplastic hypercholesterolemia. J Gastroenterol Hepatol. 2008;23:e153–e156. doi: 10.1111/j.1440-1746.2007.05115.x. [DOI] [PubMed] [Google Scholar]
- 88.Chang JE, Yoon IS, Sun PL, Yi E, Jheon S, Shim CK. Anticancer efficacy of photodynamic therapy with hematoporphyrin-modified, doxorubicin-loaded nanoparticles in liver cancer. J Photochem Photobiol B. 2014;140:49–56. doi: 10.1016/j.jphotobiol.2014.07.005. [DOI] [PubMed] [Google Scholar]
- 89.Ding Y, Wang W, Feng M, Wang Y, Zhou J, Ding X, Zhou X, Liu C, Wang R, Zhang Q. A biomimetic nanovector-mediated targeted cholesterol-conjugated siRNA delivery for tumor gene therapy. Biomaterials. 2012;33:8893–8905. doi: 10.1016/j.biomaterials.2012.08.057. [DOI] [PubMed] [Google Scholar]
- 90.Varshosaz J, Jafarian A, Salehi G, Zolfaghari B. Comparing different sterol containing solid lipid nanoparticles for targeted delivery of quercetin in hepatocellular carcinoma. J Liposome Res. 2014;24:191–203. doi: 10.3109/08982104.2013.868476. [DOI] [PubMed] [Google Scholar]
- 91.Siebert HC, Born K, André S, Frank M, Kaltner H, von der Lieth CW, Heck AJ, Jiménez-Barbero J, Kopitz J, Gabius HJ. Carbohydrate chain of ganglioside GM1 as a ligand: identification of the binding strategies of three 15 mer peptides and their divergence from the binding modes of growth-regulatory galectin-1 and cholera toxin. Chemistry. 2005;12:388–402. doi: 10.1002/chem.200500505. [DOI] [PubMed] [Google Scholar]
- 92.Zhao L, Su R, Cui W, Shi Y, Liu L, Su C. Preparation of biocompatible heat-labile enterotoxin subunit B-bovine serum albumin nanoparticles for improving tumor-targeted drug delivery via heat-labile enterotoxin subunit B mediation. Int J Nanomedicine. 2014;9:2149–2156. doi: 10.2147/IJN.S60764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Bull JM, Scott GL, Strebel FR, Nagle VL, Oliver D, Redwine M, Rowe RW, Ahn CW, Koch SM. Fever-range whole-body thermal therapy combined with cisplatin, gemcitabine, and daily interferon-alpha: a description of a phase I-II protocol. Int J Hyperthermia. 2008;24:649–662. doi: 10.1080/02656730802104740. [DOI] [PubMed] [Google Scholar]
- 94.Raoof M, Corr SJ, Zhu C, Cisneros BT, Kaluarachchi WD, Phounsavath S, Wilson LJ, Curley SA. Gold nanoparticles and radiofrequency in experimental models for hepatocellular carcinoma. Nanomedicine. 2014;10:1121–1130. doi: 10.1016/j.nano.2014.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Chen J, Zhu S, Tong L, Li J, Chen F, Han Y, Zhao M, Xiong W. Superparamagnetic iron oxide nanoparticles mediated (131)I-hVEGF siRNA inhibits hepatocellular carcinoma tumor growth in nude mice. BMC Cancer. 2014;14:114. doi: 10.1186/1471-2407-14-114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Ma X, Cheng Z, Jin Y, Liang X, Yang X, Dai Z, Tian J. SM5-1-conjugated PLA nanoparticles loaded with 5-fluorouracil for targeted hepatocellular carcinoma imaging and therapy. Biomaterials. 2014;35:2878–2889. doi: 10.1016/j.biomaterials.2013.12.045. [DOI] [PubMed] [Google Scholar]
- 97.Wang L, Su W, Liu Z, Zhou M, Chen S, Chen Y, Lu D, Liu Y, Fan Y, Zheng Y, et al. CD44 antibody-targeted liposomal nanoparticles for molecular imaging and therapy of hepatocellular carcinoma. Biomaterials. 2012;33:5107–5114. doi: 10.1016/j.biomaterials.2012.03.067. [DOI] [PubMed] [Google Scholar]
- 98.De Luca LM. Retinoids and their receptors in differentiation, embryogenesis, and neoplasia. FASEB J. 1991;5:2924–2933. [PubMed] [Google Scholar]
- 99.Sever CE, Locker J. Expression of retinoic acid alpha and beta receptor genes in liver and hepatocellular carcinoma. Mol Carcinog. 1991;4:138–144. doi: 10.1002/mc.2940040209. [DOI] [PubMed] [Google Scholar]
- 100.Schug TT, Berry DC, Shaw NS, Travis SN, Noy N. Opposing effects of retinoic acid on cell growth result from alternate activation of two different nuclear receptors. Cell. 2007;129:723–733. doi: 10.1016/j.cell.2007.02.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Altucci L, Gronemeyer H. The promise of retinoids to fight against cancer. Nat Rev Cancer. 2001;1:181–193. doi: 10.1038/35106036. [DOI] [PubMed] [Google Scholar]
- 102.Recchia F, Saggio G, Cesta A, Candeloro G, Di Blasio A, Amiconi G, Lombardo M, Nuzzo A, Lalli A, Alesse E, et al. Phase II study of interleukin-2 and 13-cis-retinoic acid as maintenance therapy in metastatic colorectal cancer. Cancer Immunol Immunother. 2007;56:699–708. doi: 10.1007/s00262-006-0224-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Singh B, Murphy RF, Ding XZ, Roginsky AB, Bell RH, Adrian TE. On the role of transforming growth factor-beta in the growth inhibitory effects of retinoic acid in human pancreatic cancer cells. Mol Cancer. 2007;6:82. doi: 10.1186/1476-4598-6-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Tsimberidou AM, Tirado-Gomez M, Andreeff M, O’Brien S, Kantarjian H, Keating M, Lopez-Berestein G, Estey E. Single-agent liposomal all-trans retinoic acid can cure some patients with untreated acute promyelocytic leukemia: an update of The University of Texas M. D. Anderson Cancer Center Series. Leuk Lymphoma. 2006;47:1062–1068. doi: 10.1080/10428190500463932. [DOI] [PubMed] [Google Scholar]
- 105.Varshosaz J, Hassanzadeh F, Sadeghi H, Ghelich Khan Z, Rostami M. Retinoic Acid Decorated Albumin-Chitosan Nanoparticles for Targeted Delivery of Doxorubicin Hydrochloride in Hepatocellular Carcinoma. J Nanomaterials. 2013;2013:12. [Google Scholar]
- 106.Hynes RO. Integrins: bidirectional, allosteric signaling machines. Cell. 2002;110:673–687. doi: 10.1016/s0092-8674(02)00971-6. [DOI] [PubMed] [Google Scholar]
- 107.Ruoslahti E. RGD and other recognition sequences for integrins. Annu Rev Cell Dev Biol. 1996;12:697–715. doi: 10.1146/annurev.cellbio.12.1.697. [DOI] [PubMed] [Google Scholar]
- 108.Mei L, Fu L, Shi K, Zhang Q, Liu Y, Tang J, Gao H, Zhang Z, He Q. Increased tumor targeted delivery using a multistage liposome system functionalized with RGD, TAT and cleavable PEG. Int J Pharm. 2014;468:26–38. doi: 10.1016/j.ijpharm.2014.04.008. [DOI] [PubMed] [Google Scholar]
- 109.Torchilin VP. Tat peptide-mediated intracellular delivery of pharmaceutical nanocarriers. Adv Drug Deliv Rev. 2008;60:548–558. doi: 10.1016/j.addr.2007.10.008. [DOI] [PubMed] [Google Scholar]
- 110.Duchardt F, Fotin-Mleczek M, Schwarz H, Fischer R, Brock R. A comprehensive model for the cellular uptake of cationic cell-penetrating peptides. Traffic. 2007;8:848–866. doi: 10.1111/j.1600-0854.2007.00572.x. [DOI] [PubMed] [Google Scholar]
- 111.Pappalardo JS, Quattrocchi V, Langellotti C, Di Giacomo S, Gnazzo V, Olivera V, Calamante G, Zamorano PI, Levchenko TS, Torchilin VP. Improved transfection of spleen-derived antigen-presenting cells in culture using TATp-liposomes. J Control Release. 2009;134:41–46. doi: 10.1016/j.jconrel.2008.11.006. [DOI] [PubMed] [Google Scholar]
- 112.Cai LL, Liu P, Li X, Huang X, Ye YQ, Chen FY, Yuan H, Hu FQ, Du YZ. RGD peptide-mediated chitosan-based polymeric micelles targeting delivery for integrin-overexpressing tumor cells. Int J Nanomedicine. 2011;6:3499–3508. doi: 10.2147/IJN.S26670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Pilapong C, Sitthichai S, Thongtem S, Thongtem T. Smart magnetic nanoparticle-aptamer probe for targeted imaging and treatment of hepatocellular carcinoma. Int J Pharm. 2014;473:469–474. doi: 10.1016/j.ijpharm.2014.07.036. [DOI] [PubMed] [Google Scholar]
- 114.Wu C, Gong F, Pang P, Shen M, Zhu K, Cheng D, Liu Z, Shan H. An RGD-modified MRI-visible polymeric vector for targeted siRNA delivery to hepatocellular carcinoma in nude mice. PLoS One. 2013;8:e66416. doi: 10.1371/journal.pone.0066416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Loyer P, Bedhouche W, Huang ZW, Cammas-Marion S. Degradable and biocompatible nanoparticles decorated with cyclic RGD peptide for efficient drug delivery to hepatoma cells in vitro. Int J Pharm. 2013;454:727–737. doi: 10.1016/j.ijpharm.2013.05.060. [DOI] [PubMed] [Google Scholar]
- 116.Bogorad RL, Yin H, Zeigerer A, Nonaka H, Ruda VM, Zerial M, Anderson DG, Koteliansky V. Nanoparticle-formulated siRNA targeting integrins inhibits hepatocellular carcinoma progression in mice. Nat Commun. 2014;5:3869. doi: 10.1038/ncomms4869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Agarwal A, Saraf S, Asthana A, Gupta U, Gajbhiye V, Jain NK. Ligand based dendritic systems for tumor targeting. Int J Pharm. 2008;350:3–13. doi: 10.1016/j.ijpharm.2007.09.024. [DOI] [PubMed] [Google Scholar]
- 118.Yap TA, Carden CP, Kaye SB. Beyond chemotherapy: targeted therapies in ovarian cancer. Nat Rev Cancer. 2009;9:167–181. doi: 10.1038/nrc2583. [DOI] [PubMed] [Google Scholar]
- 119.Elwood PC. Molecular cloning and characterization of the human folate-binding protein cDNA from placenta and malignant tissue culture (KB) cells. J Biol Chem. 1989;264:14893–14901. [PubMed] [Google Scholar]
- 120.Lacey SW, Sanders JM, Rothberg KG, Anderson RG, Kamen BA. Complementary DNA for the folate binding protein correctly predicts anchoring to the membrane by glycosyl-phosphatidylinositol. J Clin Invest. 1989;84:715–720. doi: 10.1172/JCI114220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Parker N, Turk MJ, Westrick E, Lewis JD, Low PS, Leamon CP. Folate receptor expression in carcinomas and normal tissues determined by a quantitative radioligand binding assay. Anal Biochem. 2005;338:284–293. doi: 10.1016/j.ab.2004.12.026. [DOI] [PubMed] [Google Scholar]
- 122.Ross JF, Chaudhuri PK, Ratnam M. Differential regulation of folate receptor isoforms in normal and malignant tissues in vivo and in established cell lines. Physiologic and clinical implications. Cancer. 1994;73:2432–2443. doi: 10.1002/1097-0142(19940501)73:9<2432::aid-cncr2820730929>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 123.Wu M, Gunning W, Ratnam M. Expression of folate receptor type alpha in relation to cell type, malignancy, and differentiation in ovary, uterus, and cervix. Cancer Epidemiol Biomarkers Prev. 1999;8:775–782. [PubMed] [Google Scholar]
- 124.Leamon CP. Folate-targeted drug strategies for the treatment of cancer. Curr Opin Investig Drugs. 2008;9:1277–1286. [PubMed] [Google Scholar]
- 125.Varshosaz J, Hassanzadeh F, Sadeghi Aliabadi H, Nayebsadrian M, Banitalebi M, Rostami M. Synthesis and characterization of folate-targeted dextran/retinoic acid micelles for doxorubicin delivery in acute leukemia. Biomed Res Int. 2014;2014:525684. doi: 10.1155/2014/525684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Varshosaz J, Taymouri S, Hassanzadeh F, Javanmard SH, Rostami M. Folated synperonic-cholesteryl hemisuccinate polymeric micelles for the targeted delivery of docetaxel in melanoma. Biomed Res Int. 2015;2015:746093. doi: 10.1155/2015/746093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Yang T, Li B, Qi S, Liu Y, Gai Y, Ye P, Yang G, Zhang W, Zhang P, He X, et al. Co-delivery of doxorubicin and Bmi1 siRNA by folate receptor targeted liposomes exhibits enhanced anti-tumor effects in vitro and in vivo. Theranostics. 2014;4:1096–1111. doi: 10.7150/thno.9423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Zhang L, Gong F, Zhang F, Ma J, Zhang P, Shen J. Targeted therapy for human hepatic carcinoma cells using folate-functionalized polymeric micelles loaded with superparamagnetic iron oxide and sorafenib in vitro. Int J Nanomedicine. 2013;8:1517–1524. doi: 10.2147/IJN.S43263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Cao N, Cheng D, Zou S, Ai H, Gao J, Shuai X. The synergistic effect of hierarchical assemblies of siRNA and chemotherapeutic drugs co-delivered into hepatic cancer cells. Biomaterials. 2011;32:2222–2232. doi: 10.1016/j.biomaterials.2010.11.061. [DOI] [PubMed] [Google Scholar]
- 130.Li X, Li H, Yi W, Chen J, Liang B. Acid-triggered core cross-linked nanomicelles for targeted drug delivery and magnetic resonance imaging in liver cancer cells. Int J Nanomedicine. 2013;8:3019–3031. doi: 10.2147/IJN.S45767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Xu Z, Zhang Z, Chen Y, Chen L, Lin L, Li Y. The characteristics and performance of a multifunctional nanoassembly system for the co-delivery of docetaxel and iSur-pDNA in a mouse hepatocellular carcinoma model. Biomaterials. 2010;31:916–922. doi: 10.1016/j.biomaterials.2009.09.103. [DOI] [PubMed] [Google Scholar]
- 132.Maeng JH, Lee DH, Jung KH, Bae YH, Park IS, Jeong S, Jeon YS, Shim CK, Kim W, Kim J, et al. Multifunctional doxorubicin loaded superparamagnetic iron oxide nanoparticles for chemotherapy and magnetic resonance imaging in liver cancer. Biomaterials. 2010;31:4995–5006. doi: 10.1016/j.biomaterials.2010.02.068. [DOI] [PubMed] [Google Scholar]
- 133.Viota JL, Carazo A, Munoz-Gamez JA, Rudzka K, Gómez-Sotomayor R, Ruiz-Extremera A, Salmerón J, Delgado AV. Functionalized magnetic nanoparticles as vehicles for the delivery of the antitumor drug gemcitabine to tumor cells. Physicochemical in vitro evaluation. Mater Sci Eng C Mater Biol Appl. 2013;33:1183–1192. doi: 10.1016/j.msec.2012.12.009. [DOI] [PubMed] [Google Scholar]
- 134.Fan L, Li F, Zhang H, Wang Y, Cheng C, Li X, Gu CH, Yang Q, Wu H, Zhang S. Co-delivery of PDTC and doxorubicin by multifunctional micellar nanoparticles to achieve active targeted drug delivery and overcome multidrug resistance. Biomaterials. 2010;31:5634–5642. doi: 10.1016/j.biomaterials.2010.03.066. [DOI] [PubMed] [Google Scholar]
- 135.Jin H, Yang P, Cai J, Wang J, Liu M. Photothermal effects of folate-conjugated Au nanorods on HepG2 cells. Appl Microbiol Biotechnol. 2012;94:1199–1208. doi: 10.1007/s00253-012-3935-1. [DOI] [PubMed] [Google Scholar]
- 136.Wang L, Li M, Zhang N. Folate-targeted docetaxel-lipid-based-nanosuspensions for active-targeted cancer therapy. Int J Nanomedicine. 2012;7:3281–3294. doi: 10.2147/IJN.S32520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Li JC, Sha XY, Zhang LJ, Fang XL. [9-nitrocamptothecin nanostructured lipid carrier system: in vitro releasing characteristics, uptake by cells, and tissue distribution in vivo] Yao Xue Xue Bao. 2005;40:970–975. [PubMed] [Google Scholar]
- 138.Krishna AD, Mandraju RK, Kishore G, Kondapi AK. An efficient targeted drug delivery through apotransferrin loaded nanoparticles. PLoS One. 2009;4:e7240. doi: 10.1371/journal.pone.0007240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Golla K, Cherukuvada B, Ahmed F, Kondapi AK. Efficacy, safety and anticancer activity of protein nanoparticle-based delivery of doxorubicin through intravenous administration in rats. PLoS One. 2012;7:e51960. doi: 10.1371/journal.pone.0051960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Luo LZ, Jin HW, Huang HQ. Transferrin-cisplatin specifically deliver cisplatin to HepG2 cells in vitro and enhance cisplatin cytotoxicity. J Proteomics. 2012;77:237–250. doi: 10.1016/j.jprot.2012.08.023. [DOI] [PubMed] [Google Scholar]
- 141.Malarvizhi GL, Retnakumari AP, Nair S, Koyakutty M. Transferrin targeted core-shell nanomedicine for combinatorial delivery of doxorubicin and sorafenib against hepatocellular carcinoma. Nanomedicine. 2014;10:1649–1659. doi: 10.1016/j.nano.2014.05.011. [DOI] [PubMed] [Google Scholar]
- 142.Ashley CE, Carnes EC, Phillips GK, Durfee PN, Buley MD, Lino CA, Padilla DP, Phillips B, Carter MB, Willman CL, et al. Cell-specific delivery of diverse cargos by bacteriophage MS2 virus-like particles. ACS Nano. 2011;5:5729–5745. doi: 10.1021/nn201397z. [DOI] [PMC free article] [PubMed] [Google Scholar]


