Abstract
Objective:
To evaluate whether microsurgery gains better result in root coverage compared to conventional surgical techniques.
Methods:
A number of databases were searched to identify eligible studies from January 1992 to January 2015.
The following outcomes were evaluated:
number of sites exhibiting complete root coverage and patients’ esthetic satisfaction.
Results:
Four Randomized Clinical Trials (RCTs) fulfilled the inclusion criteria. A pooled estimate from the two RCTs regarding sub-epithelial connective tissue grafts (SCTG) showed significant achievement in complete root coverage in the microsurgical group [relative risk (RR):1.63; 95% confidence interval (CI): 1.12 to 2.36; P=0.01] with acceptable heterogeneity. The other two studies were about coronal advanced flap (CAF) with enamel matrix derivative or free rotated papilla autograft and did not qualify for meta-analysis. Patients’ esthetic satisfaction was analyzed only by one study.
Conclusions:
Using microsurgical technique for treating gingival recessions may be effective in achieving complete root coverage for SCTG.
KEY WORDS: Gingival Recession, Microscopy, Surgery, Surgical Flaps
INTRODUCTION
Gingival recession, is defined as apical shift of gingival margin towards cementoenamel junction and consequently results in tooth root surface exposure. Gingival recession is usually associated with anatomic factors, inflammatory conditions, and trauma, and is one of the most common esthetic complaints of patients in periodontal clinics. Esthetic improvement, dentinal hypersensitivity, root caries are all indications for surgical treatment.1
A variety of surgical techniques have been used for root coverage; such as sub-epithelial connective tissue grafts (SCTG), guided tissue regeneration and coronal advanced flap (CAF).1 The microsurgical technique involves microscope and fine instruments that allow high-level of accuracy. Microsurgery was introduced in the specialty of periodontics in 1992.2 Clinical and histological evidence showed that microsurgical technique may result in primary wound closure,3-5 which could lead to better esthetic appearance and less postoperative discomfort. Though the microsurgical technique have some benefits, not all randomized clinical trials (RCTs) comparing microsurgery with conventional surgery showed clinical efficacy of the microsurgery. A systematic review was carried out to provide the best level of evidence and summarize the existing studies.
METHODS
Inclusion and Exclusion criteria
Types of studies
Only RCTs with a follow-up of ≥6 months were included (including split-mouth studies randomized by quadrants). However, trials that randomized individual teeth or alternate teeth, with the initial selection of the teeth sequence being randomized, were not included.
Types of participants
Healthy adult patients with a localized gingival recession (no limitation on Miller classifications6) who had undergone surgical treatment.
Types of interventions and comparison
Plastic surgery for root coverage of gingival recession defects comparing microsurgical procedure (using operational microscope and microsurgical instruments) with conventional procedure (without using microscope).
Types of outcome measures
Primary outcomes: The number of sites exhibiting complete root coverage. Secondary outcomes: Patients’ esthetic evaluation.
Literature Search
Electronic search
MEDLINE (via PubMed), EMBASE (via OVID), CENTRAL (for the Cochrane Central Register of Controlled Trials), Cochrane Oral Health Group’s Specialized Register database, and CNKI in China were searched for identifying RCTs, to be included or considered for this systematic review. For dissertations and grey literature, ProQuest and OpenGrey database were searched. Google Scholar was another source of search. Articles from January 1992 to January 2015 without limitation to any language were searched. Following key words were used:
Gingival recession
(recession NEAR gingiva*) or (recession NEAR defect*)
(exposure NEAR root*) or (exposed NEAR root*)
1 or 2 or 3
Microsurgery
Microscop*
Minimal* NEAR invasive
5 or 6 or 7
4 and 8
Manual search
Journal of Periodontology, Journal of Periodontal Research, Journal of Clinical Periodontology, and International Journal of Periodontics & Restorative Dentistry were manually searched for articles published through January 1992 to January 2015. References of the eligible studies were further browsed for identification of relevant articles.
Study selection and data extraction
The title and abstract of each article were screened by two of the authors (JK and SM). Full texts of relevant articles were obtained and then assessed for inclusion also by the same two authors (JK and SM). Disagreements were resolved by discussion with a third author (SJG). Finally, studies fulfilling the inclusion criteria underwent data extraction by two authors (JK and SM) independently using data-extraction forms. Unpublished data and details about the trials were obtained by contacting the concerned researchers.
Risk of bias assessment
Two authors (JK and SM) assessed the risk of bias in included studies. Random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other biases were considered.7 In case of disagreement, the dispute was resolved through a discussion with a third author (SJG).
Data synthesis
For continuous data, mean differences (MDs), standard errors (SEs), and 95% confidence intervals (CIs) were calculated for all studies to combine data from parallel and split-mouth studies.8
For dichotomous data, pooled relative risks (RRs) and associated 95% CIs were used. Number needed to treat (NNT) was calculated for sites exhibiting complete root coverage when the pooled estimate was statistical significant (P<0.05). Heterogeneity between studies was analyzed through heterogeneity test and I2 statistic. P>0.1 and I2<50% were taken as acceptable heterogeneity, in which case, a fixed-effects model was employed; otherwise a random-effects model was adopted. Meta-analysis was conducted by Review Manager (RevMan) software (Version 5.1).
RESULTS
The results of the search from databases provided 201 records. Six additional records including one dissertation were found by screening the references and Google Scholar. After eliminating the duplicate records, 163 records remained. By screening the titles and abstracts, 137 irrelevant articles were discarded, leaving 26 articles for further evaluation. Full texts of these 26 articles were obtained; of which 20 articles were excluded for not being RCTs.9-29 One RCT was excluded because the surgical strategies were different in the microsurgical and control groups.5 The dissertation by Pandey Suraj Devendra30 and the article by Pandey and Mehta31 described the same study. The dissertation and article were merged into one.31 Finally, four RCTs in five records were included in this review.3,4,31,32 A flow chart summarizing the results of the search and reasons for exclusion are listed in Fig.1.
Fig.1.
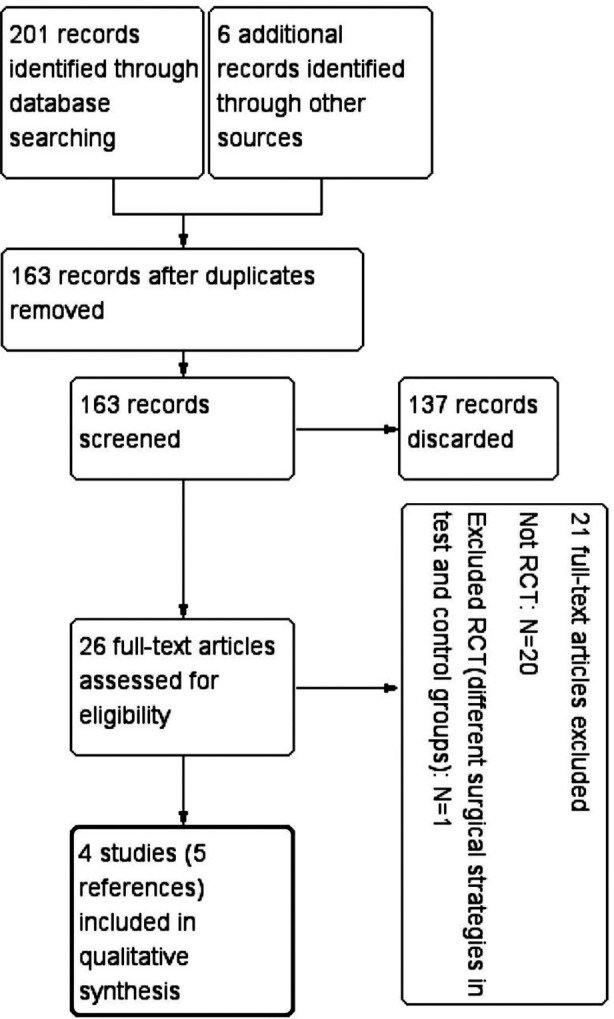
Flow chart of articles screened through the review process.
Characteristics of included studies
Burkhardt and Lang and Bittencourt et al. performed SCTG combined with double papilla flap or a repositioned flap,3,4 while Andrade performed CAF with enamel matrix derivative.32 Pandey and Mehta performed CAF combined with free rotated papilla autograft.31 The characteristics of the included studies are summarized as Table-I.
Table-I.
Characteristics of RCTs.
| Study ID | Study design | Participants (n) | Miller class | Interventions | Outcomes | Follow-up (month) |
|---|---|---|---|---|---|---|
| Burkhardt and Lang, 2005 | RCT; split-mouth study | 10 (Two were lost to follow-up) | I or II | Test group: SCTG+double-pedicle papilla flap under 5× and 15× magnification | 1. Postsurgical vascularization; 2. PD; 3. GR; 4. CAL; 5. GI and PI |
12 |
| Control group: SCTG+double-pedicle papilla flap by conventional approach | ||||||
| Anderade et al. 2010 | RCT; parallel study | 30 | I or III | Text group: CAF+EMD by microsurgical approach | 1. GR; 2. PD; 3. CAL; 4. WKT;5. TKT 6. Pain evaluation |
6 |
| Control group: CAF+EMD by conventional approach | ||||||
| Bittencourt et al. 2012 | RCT; split-mouth study | 24 | I or II | Test group: SCTG with a microscope under 8× to 12× magnification | 1.GR; 2. WKT; 3. RW; 4. PD; 5. CAL; 6. TKT; 7. Postoperative pain; 8. Patients’ satisfaction (relative to esthetics, root sensitivity before and after surgery) |
12 |
| Control group: SCTG performed without a microscope but employing fine instruments | ||||||
| Pandey and Mehta, 2013 | RCT; split-mouth study | 10 | I or II | Text group: CAF+free rotated papilla autograft under 10× magnification | 1.Plaque index; 2.Gingival index; 3.GR; 4.RW; 5.CAL; 6.WKT |
6 |
| Control group: CAF+free rotated papilla autograft by conventional approach |
CRC: complete root coverage; CAF: coronally advanced flaps; CAL: clinical attachment level; EMD: enamel matrix derivative; GI: gingival index; GR: gingival recession; PD: probing depth; PI: plaque index; RCT: randomized controlled trial; RW: recession width; SCTG: subepithelial connective tissue graft; TKT: thickness of keratinized tissue; WKT: width of keratinized tissue; NR: not reported.
Risk of bias in included studies
Risk of bias in the included studies is summarized in Fig.2. All the included trials were categorized as high risk of bias due to the difficulties in blinding patients and surgeons while using operational microscope. Concealment of random sequence was poorly reported by most of the studies.4,31,32 Bittencourt et al were contacted; they responded and explained that they adequately concealed the random allocation scheme.3 Lack of details about random sequence generation31 and masking of outcome assessors4,31,32 were the other sources of bias. In one study, two patients out of ten could not be followed-up because of relocation.4 There might not be great effect on the risk of attrition bias for split-mouth studies due to the balanced dropout numbers with the same reason across groups.33 Data for these two patients in the study4 were excluded from the analysis. The trial by Pandey and Mehta31 had unclear risk of reporting bias for not reporting the sites of complete root coverage which is considered to be an important outcome.
Fig.2.
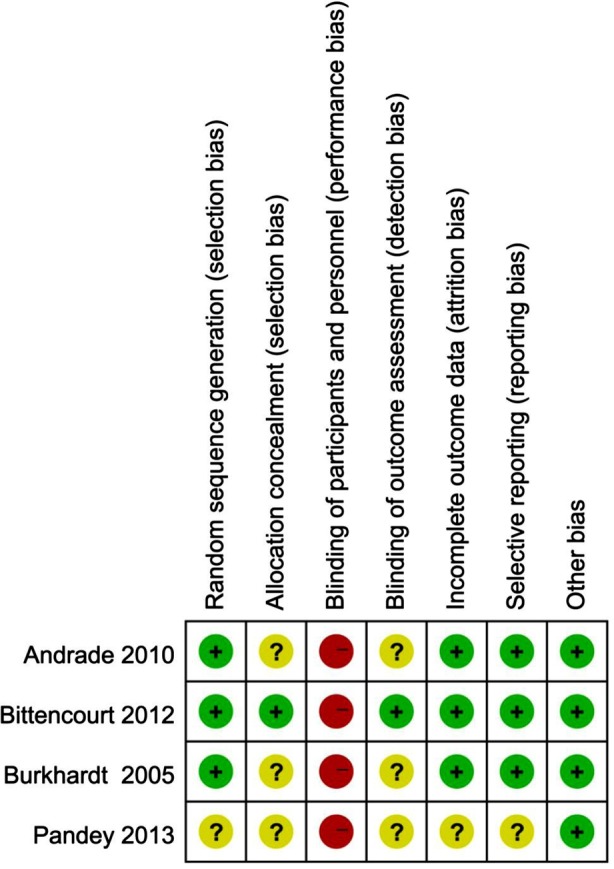
Risk of bias summary: review authors’ judgments about each risk of bias item for each included study.
Effects of interventions
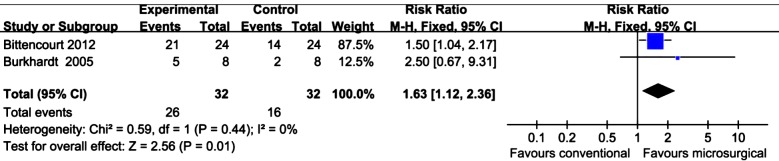
Number of sites exhibiting complete root coverage
Two split-mouth studies3,4 employing SCGT and one parallel study32 combining CAF with enamel matrix derivative reported the results of complete root coverage. For SCTG, a pooled estimate showed significant achievement in complete root coverage in the microsurgery group (RR: 1.63; 95% CI: 1.12 to 2.36; P=0.01) with acceptable heterogeneity (Fig.3). Additionally, the number needed to treat was 4 (95%CI: 1.88 to 10.78), implying that one additional person will gain complete root coverage for every four participants receiving the microsurgical intervention rather than conventional approach. For CAF with enamel matrix derivative microsurgical group achieved 73.3% complete root coverage versus 46.7% in control group (P=0.26).
Fig.3.
Meta-analysis for complete root coverage by SCTG comparing microsurgery and conventional surgery.
Patients’ esthetic satisfaction
Patients’ satisfaction about esthetic improvement was reported only by one study3 that was collected through a questionnaire. All patients in microsurgery group were satisfied from the gingival appearance, comparing with 79.1% in the conventional surgery group.
DISCUSSION
This systematic review evaluated the effectiveness of root coverage operation through microsurgical technique. Four trials met the proposed inclusion criteria, providing data from patients treated with SCTG, CAF combined with enamel matrix derivative, or free rotated papilla autograft.
Complete root coverage is the ultimate goal of gingival recession treatment. By achieving this goal, periodontist can not only get the greatest degree of improvement in appearance, but also reduce the extent of dentinal hypersensitivity.34,35 The available evidence, stemming from 2 RCTs3,4 indicate that complete root coverage can be more predictably achieved by SCTG performed with a microscope. This can be explained by accurately mapped incisions, finely elevated flaps, and precisely closed wound without tension leading to primary wound healing.22 Nevertheless, very limited data about complete root coverage are available in the literature for other root coverage techniques such as CAF with enamel matrix derivative or free rotated papilla autograft and guided tissue regeneration. The scarcity of data makes meta-analyses difficult and prevent making conclusive evidence-based statements.
Despite the fact that esthetics is considered as a main reason for opting microsurgery,3 few studies evaluated the patients’ satisfaction. Even with complete root coverage; the incision scar, gingival color, and gingival margin contour also affect the esthetic appearance. It is the patients who should primarily evaluate the esthetic success of root coverage. There is a need to investigate patients’ own evaluation on esthetic condition of microsurgical technique in future research.
All the trials included in this study were categorized as high risk of bias. The lack of details about randomization, allocation concealment and blinding, can act as sources of bias and affect the accuracy of the results. Knowledge of the intervention by participants may also impact on patients’ esthetic evaluation. Although it is impossible to mask the surgeons; participants’ blinding could be improved by blindfolding during operation.
This systematic review has the following limitations with regard to the robustness of the results: the paucity of RCTs, small sample size, and methodological flaws within the included studies. Microsurgery might be a promising technique in gingival recession treatment. However, further research is required in this area.
CONCLUSION
The application of magnification and finer instruments in the treatment of gingival recession may predict greater opportunities of achieving complete root coverage for SCTG.
Footnotes
Source of funding: This study was supported by funding from the National Key Clinical Specialty Program of China to Department of Periodontics, West China Hospital of Stomatology (2010).
Declaration of interests: All authors declare that they have no conflict of interests.
Authors’ Contribution
Jian Kang: Drafting the article; Responsible for study selection, data extraction and risk of bias assessment, data analysis and interpretation.
Shu Meng: Revising this article critically for important intellectual content; Responsible for study selection, data extraction and risk of bias assessment, data analysis and interpretation.
Chunjie Li: Providing methodological advice; contributions to data analysis and interpretation
Zhenhua Luo: Revising the manuscript for improvement of English language.
Shujuan Guo: Providing methodological advice; Responsible for study selection, data extraction and risk of bias assessment.
Yafei Wu: Corresponding author, substantial contributions to conception & design; Final approval of the version to be published.
REFERENCES
- 1.Bouchard P, Malet J, Borghetti A. Decision-making in aesthetics: root coverage revisited. Periodontol 2000. 2001;27:97–120. doi: 10.1034/j.1600-0757.2001.027001097.x. doi: 10.1034/j.1600-0757.2001.027001097.x. [DOI] [PubMed] [Google Scholar]
- 2.Shanelec DA, Tibbetts LS. 78th American Academy of Periodontology annual meeting, Nov 19. Orlando, FL: 1992. Periodontal microsurgery, continuing education course. [Google Scholar]
- 3.Bittencourt S, Del Peloso Ribeiro E, Sallum EA, Nociti FH, Jr, Casati MZ. Surgical microscope may enhance root coverage with subepithelial connective tissue graft: a randomized-controlled clinical trial. J Periodontol. 2012;83(6):721–730. doi: 10.1902/jop.2011.110202. doi: 10.1902/jop.2011.110202. [DOI] [PubMed] [Google Scholar]
- 4.Burkhardt R, Lang NP. Coverage of localized gingival recessions: comparison of micro- and macrosurgical techniques. J Clin Periodontol. 2005;32(3):287–293. doi: 10.1111/j.1600-051X.2005.00660.x. doi: 10.1111/j.1600-051X.2005.00660.x. [DOI] [PubMed] [Google Scholar]
- 5.Francetti L, Del Fabbro M, Calace S, Testori T, Weinstein RL. Microsurgical treatment of gingival recession: a controlled clinical study. Int J Periodontics Restorative Dent. 2005;25(2):181–188. [PubMed] [Google Scholar]
- 6.Miller PD., Jr A classification of marginal tissue recession. Int J Periodontics Restorative Dent. 1985;5(2):8–13. [PubMed] [Google Scholar]
- 7.Julian PT, Higgins SG. Collaboration TC, editor. Cochrane Handbook for Systematic Reviews of Interventions. 5.1.0 ed2011. [Google Scholar]
- 8.Lesaffre E, Garcia Zattera MJ, Redmond C, Huber H, Needleman I. Reported methodological quality of split-mouth studies. J Clin Periodontol. 2007;34(9):756–761. doi: 10.1111/j.1600-051X.2007.01118.x. doi: 10.1111/j.1600-051X.2007.01118.x. [DOI] [PubMed] [Google Scholar]
- 9.Belcher JM. A perspective on periodontal microsurgery. Int J Periodontics Restorative Dent. 2001;21(2):191–196. [PubMed] [Google Scholar]
- 10.Burkhardt R, Hurzeler MB. Utilization of the surgical microscope for advanced plastic periodontal surgery. Pract Periodontics Aesthet Dent. 2000;12(2):171–180. [PubMed] [Google Scholar]
- 11.de Campos GV, Bittencourt S, Sallum AW, Nociti FH, Junior, Sallum EA, Casati MZ. Achieving primary closure and enhancing aesthetics with periodontal microsurgery. Pract Proced Aesthet Dent. 2006;18(7):449–454. [PubMed] [Google Scholar]
- 12.Dhir V, Jha A. Microsurgical treatment of gingival recession by subepithelial connective tissue graft: a case report. Med J Armed Forces India. 2011;67(3):293–295. doi: 10.1016/S0377-1237(11)60066-X. doi: 10.1016/S0377-1237(11)60066-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Francetti L, Del Fabbro M, Testori T, Weinstein RL. Periodontal microsurgery: report of 16 cases consecutively treated by the free rotated papilla autograft technique combined with the coronally advanced flap. Int J Periodontics Restorative Dent. 2004;24(3):272–279. [PubMed] [Google Scholar]
- 14.Hegde R, Sumanth S, Padhye A. Microscope-enhanced periodontal therapy: a review and report of four cases. J Contemp Dent Pract. 2009;10(5):E088–E096. [PubMed] [Google Scholar]
- 15.Kahn S, Rodrigues WJ, Barceleiro Mde O. Periodontal plastic microsurgery in the treatment of deep gingival recession after orthodontic movement. Case Rep Dent. 2013;2013:851413. doi: 10.1155/2013/851413. doi: 10.1155/2013/851413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kapadia JA, Bhedasgoankar SY, Bhandari SD. Periodontal microsurgery: A case report. J Indian Soc Periodontol. 2013;17(6):790–792. doi: 10.4103/0972-124X.124511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Latha TA, Sudarsan S, Arun KV, Talwar A. Root coverage in class I gingival recession defects, combining rotated papillary pedicle graft and coronally repositioned flap, using a micro surgical approach: A clinical evaluation. J Indian Soc Periodontol. 2009;13(1):21–26. doi: 10.4103/0972-124X.51890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mamoun JS. A rationale for the use of high-powered magnification or microscopes in general dentistry. Gen Dent. 2009;57(1):18–26. [PubMed] [Google Scholar]
- 19.Michaelides PL. Connective-tissue root coverage using microsurgery. Dent Today. 1996;15(10):74. 76, 78-79. [PubMed] [Google Scholar]
- 20.Nordland WP. The role of periodontal plastic microsurgery in oral facial esthetics. J California Dent Assoc. 2002;30(11):831–837. [PubMed] [Google Scholar]
- 21.Rossi R, Pilloni A, Morales RS. Qualitative assessment of connective tissue graft with epithelial component. A microsurgical periodontal plastic surgical technique for soft tissue esthetics. Euro J Esthetic Dent. 2009;4(2):118–128. [PubMed] [Google Scholar]
- 22.Shanelec DA. Periodontal microsurgery. J Esthetic Restorative Dent. 2003;15(7):402–407. doi: 10.1111/j.1708-8240.2003.tb00965.x. discussion 8. doi: 10.1111/j.1708-8240.2003.tb00965.x. [DOI] [PubMed] [Google Scholar]
- 23.Shanelec DA, Tibbetts LS. A perspective on the future of periodontal microsurgery. Periodontol 2000. 1996;11:58–64. doi: 10.1111/j.1600-0757.1996.tb00183.x. doi: 10.1111/j.1600-0757.1996.tb00183.x. [DOI] [PubMed] [Google Scholar]
- 24.Tibbetts LS, Shanelec D. Current status of periodontal microsurgery. Curr Opin Periodontol. 1996;3:118–125. [PubMed] [Google Scholar]
- 25.Tibbetts LS, Shanelec D. Periodontal microsurgery. Dent Clin North Am. 1998;42(2):339–359. [PubMed] [Google Scholar]
- 26.Tibbetts LS, Shanelec DA. An overview of periodontal microsurgery. Curr Opin Periodontol. 1994:187–193. [PubMed] [Google Scholar]
- 27.Tibbetts LS, Shanelec DA. A review of the principles and practice of periodontal microsurgery. Tex Dent J. 2007;124(2):188–204. [PubMed] [Google Scholar]
- 28.Zuhr O, Fickl S, Wachtel H, Bolz W, Hurzeler MB. Covering of gingival recessions with a modified microsurgical tunnel technique: case report. Int J Periodontics Restorative Dent. 2007;27(5):457–463. [PubMed] [Google Scholar]
- 29.Belcher JM. A perspective on periodontal microsurgery. Int J Periodontics Restorative Dent. 2001;21(2):191–196. [PubMed] [Google Scholar]
- 30.Pandey S. Treatment of localized gingival recession using the free rotated papilla autograft combined with coronally advanced flap by conventional and microsurgical technique-a comparative clinical study dissertation: Rajiv Gandhi University of Health Sciences. 2009 doi: 10.4103/0972-124X.124500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pandey S, Mehta DS. Treatment of localized gingival recession using the free rotated papilla autograft combined with coronally advanced flap by conventional (macrosurgery) and surgery under magnification (microsurgical) technique: A comparative clinical study. J Indian Soc Periodontol. 2013;17(6):765–770. doi: 10.4103/0972-124X.124500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Andrade PF, Grisi MF, Marcaccini AM, Fernandes PG, Reino DM, Souza SL, et al. Comparison between micro- and macrosurgical techniques for the treatment of localized gingival recessions using coronally positioned flaps and enamel matrix derivative. J Periodontol. 2010;81(11):1572–1579. doi: 10.1902/jop.2010.100155. doi: 10.1902/jop.2010.100155. [DOI] [PubMed] [Google Scholar]
- 33.Higgins JPT, Altman DG, Sterne JAC, editors; Higgins JPT, Green S, editors. Chapter 8: Assessing risk of bias in included studies. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration. 2011. Available from www.cochrane-handbook.org .
- 34.Nieri M, Rotundo R, Franceschi D, Cairo F, Cortellini P, Pini Prato G. Factors affecting the outcome of the coronally advanced flap procedure: a Bayesian network analysis. J Periodontol. 2009;80(3):405–410. doi: 10.1902/jop.2009.080146. doi: 10.1902/jop.2009.080146. [DOI] [PubMed] [Google Scholar]
- 35.Chambrone L, Pannuti CM, Tu YK, Chambrone LA. Evidence-based periodontal plastic surgery. II. An individual data meta-analysis for evaluating factors in achieving complete root coverage. J Periodontol. 2012;83(4):477–490. doi: 10.1902/jop.2011.110382. doi: 10.1902/jop.2011.110382. [DOI] [PubMed] [Google Scholar]