Abstract
Background
Malaysia has been experiencing significant drug abuse problems since the 1970s, and drug abuse is the major driver of HIV transmission in Malaysia. We investigated risk factors for HIV associated with use of amphetamine type stimulants (ATS) among not-in-treatment opiate injectors in Malaysia.
Methods
Between October of 2006 and May of 2008, we conducted a series of surveys in three major urban areas of Malaysia. A total of 732 opiate IDUs (679 males and 53 females) were enrolled in the three surveys. The survey instruments consisted of a structured interview on demographic characteristics, drug use history (including year of first use, and past month history of use of illicit drugs; lifetime and past month history of IDU or needle or equipment sharing), and HIV status.
Results
There were 194/704 (27.6%) HIV positive participants in the sample. Two factors were significantly associated with HIV infection in this sample: lifetime history of ATS use (OR [95%CI]: 2.3 [1.5–3.6]) and lifetime history of sharing of injection equipment (OR [95% CI]: 4.2 [1.8–9.8]). Both HIV-positive and HIV-negative participants reported high levels of current needle/equipment sharing practices: 82% vs. 75%, respectively.
Conclusions
ATS use spread rapidly in the study sample after 1997 and is associated with an increased risk of HIV infection in this population already at high risk because of opiate IDU. Out-of-treatment IDUs in Malaysia engage in high risk behaviors regardless of their HIV status. Increased education and public health prevention measures are needed to reduce HIV transmission risks in this population.
Keywords: ATS use, HIV transmission risk, Malaysia, Poly substance abuse
1. Introduction
Malaysia has been experiencing significant drug abuse problems since the 1970s, and drug abuse is the major driver of HIV transmission in Malaysia. The prevalence of HIV infection among drug users in Malaysia ranges from 25% to 45% (Kamarulzaman, 2009) and injection drug use (IDU) accounts for majority of all HIV infections in Malaysia (91,362 HIV cases registered between 1986 and 2010; Department of Public Health, Ministry of Health Malaysia). Historically, heroin (injected or smoked) has been the dominant drug of abuse in Malaysia, in part due to its geographic proximity to the Golden Triangle. More recently, amphetamine type stimulants (ATS), including crystal methamphetamine and various other methamphetamine and/or amphetamine containing substances/pills, has been identified as a growing problem in Malaysia and throughout East and South-East Asia (McKetin et al., 2008; Sutcliffe et al., 2009; UNODC, 2010, 2011). Laboratories producing ATS, including large scale laboratories capable of industrial-scale manufacture, have been identified in most countries in the region and the UNODC’s 2010 assessment estimated that up to 20.7 million individuals in Asia and the Pacific have used ATS in the past year (Global SMART Programme, 2010). In our previous research, we found that approximately 60% of opioid IDUs in many regions in Malaysia report lifetime use of ATS with 29% also reporting lifetime injection of ATS (Vicknasingam et al., 2010).
Despite recent widespread media attention to ATS problems in Malaysia and other countries in Asia, very limited data are available to date the onset of ATS problems in Malaysia and other countries. Additionally, although ATS use has been identified as a risk factor for HIV in some populations (Colfax et al., 2010; Degenhardt et al., 2010; Martin et al., 2010; Plankey et al., 2007; Strathdee and Stockman, 2010), its impact on HIV transmission among heroin IDUs has not been extensively studied (Colfax et al., 2010).
Consequently, we evaluated the temporal onset of ATS use and its association with HIV transmission risk behaviors in this population, using data collected in a series of surveys of not-in-treatment opiate IDUs in three major urban areas of Malaysia.
2. Methods
2.1. Subjects
Between October of 2006 and May of 2008, we conducted three successive surveys of not-in-treatment opiate injectors in Kuala Lumpur, Johor Bharu, and Penang, Malaysia. In each city, we recruited outreach collaborators (ex-drug users and/or staff of local NGOs working with active drug users) to identify areas frequented by active drug users and to engage, screen, and recruit survey participants. All engaged survey participants were asked to inform other active drug users about the survey and to encourage their participation and/or introduce them to our research staff (chain referral sampling). The inclusion criterion for participation in all survey interviews was current (past week) opiate IDU, based on self-report and verified by examination of recent injection marks. A total of 732 participants were interviewed in all three surveys.
2.2. Survey instruments
The survey instruments consisted of a structured interview (self-report) on demographic characteristics, drug use history (including year of first use, and past month history of use of illicit opiates and ATS; lifetime and past month history of IDU or needle or equipment sharing) and HIV status. The survey instruments included questions from clinical and research instruments previously used by our research team in Malaysia and included both multiple choice and open ended questions regarding both lifetime and current or recent (in the past 30 days) behaviors. No identifying data were collected and all participants were assured anonymity of their responses. Survey participants received 15 RM (approximately $4.5 USD) for taking time to participate in the interviews (see Vicknasingam et al., 2010 for description of the study procedures and findings of two of the three surveys). Approval for the surveys was obtained from the Human Research and Ethical Committee of Universiti Sains Malaysia.
2.3. Interviewers
Interviewers were trained before engaging in any study related activities and supervised throughout the surveys by an experienced research assistant and the study investigators.
2.4. Data/statistical analyses
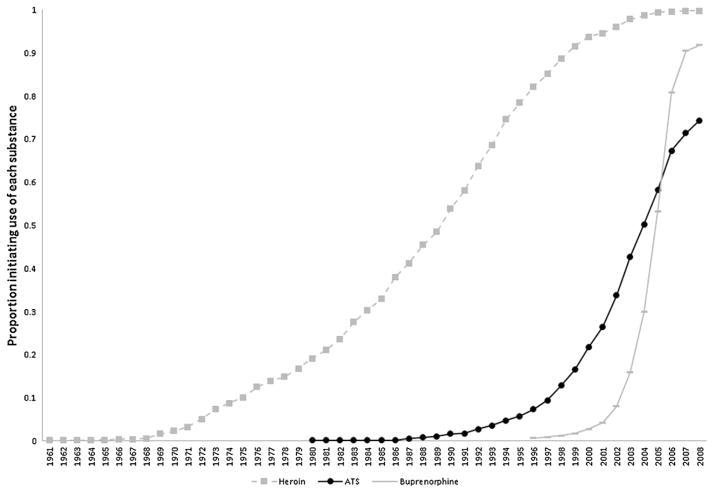
Data analyses included descriptive statistics to summarise demographics, drug use history, and risk behaviors data. We used an exploratory stepwise logistic regression to evaluate the association between the prevalence of HIV and the collected demographic, drug use, and risk behaviors data in the sample. To evaluate timeline trends for the initiation of illicit use of heroin, ATS, and buprenorphine, we plotted cumulative proportion curves of survey participants who initiated their illicit use of each illicit drug between 1961 and 2008 (Fig. 1) based on the reported ages of onset of illicit use of these drugs.
Fig. 1.
Timeline of drug abuse onset in a sample of 732 not-in-treatment active opiate injectors in Kuala Lumpur, Johor Bahru, and Penang, Malaysia.
3. Results
A total of 732 participants (679 males and 53 females) were enrolled in the three surveys. Their mean (SD) age was 38.14 (8.7); 612 (84%) were of Malay, 50 (7%) of Chinese, 64 (9%) of Indian, and 6 (1%) of other/unknown ethnicity; 441 (63%) had less than high school education; 232 (33%) were unemployed; 83 (12%) were married; 194/732 (27%) reported being HIV positive, 510/732 (70%) reported being HIV negative, and 28/732 (4%) did not know their HIV status.
All survey participants (732) reported lifetime and current (past month) opiate abuse; 728 (99.5%) reported lifetime history of opiate IDU, including 710 (97%) heroin IDU and 572 (78%) buprenorphine IDU. Lifetime history of ATS use was reported by 551 (75%) and 167 (23%) reported lifetime ATS IDU. Current (past month) opiate IDU was reported by 715 (97.7%) and current ATS IDU was reported by 87 (12%). The mean (SD) of duration of heroin, ATS, and buprenorphine use were reported respectively as: 18.1 (8.7), 5.1 (4.1), and 2.1 (2.0) years.
Drug-related risks of HIV infection: 664 (91%) of survey participants reported lifetime history of sharing of injection equipment and 561 (77%) reported current (past month) sharing practices. The prevalence of current injection equipment sharing did not differ significantly between respondents who reported being HIV-positive (159/194, 82%) and those who reported being HIV-negative (384/510, 75%).
In the multivariate exploratory stepwise logistic regression, lifetime history of ATS use (B = 2.4, p < 0.001, OR (95%CI): 2.3 (1.5–3.6)) and lifetime history of sharing of injection equipment (B = 4.5, p < 0.001, OR (95%CI): 4.2 (1.8–9.8)) were the only statistically significant factors associated with an increased risk of HIV infections in this sample. Participants who reported the lifetime history of ATS use were younger than those without ATS use history (37(8.1) vs. 42(9.5), p < 0.01), and did not differ significantly on other variables.
The cumulative proportions of respondents initiating heroin, ATS, or buprenorphine use beginning in the 1960s, the earliest onset of heroin use among the survey respondents, through 2008, is shown in Fig. 1. As illustrated in Fig. 1, the cumulative proportion of study participants initiating heroin use increased steadily beginning in the late 1960s. On the other hand, ATS use was negligible until 1987 (only one person reported initiation of ATS before 1987). The number of participants initiating ATS use increased slowly over the next several years before rising rapidly after 1997. By 2008, 75% of the participants had initiated ATS use. Initiation of buprenorphine use was reported very infrequently before 2000, but the proportion initiating buprenorphine use increased rapidly after 2002, the year when buprenorphine became available in Malaysia as a medication to treat opiate dependence.
4. Discussion
The study findings point to the relatively recent and rapid emergence over the past decade of ATS use in the study sample and identify lifetime ATS use as an additional risk factor for HIV transmission in this population of heroin IDUs who are already at increased risk for HIV because of long histories of opiate IDU and a high prevalence of sharing of injection equipment. Similar findings regarding the relationship between stimulant use or abuse and HIV infection among heroin IDUs have been reported previously for cocaine abuse (Meandzija et al., 1994) but not for ATS use. Although the results from this cross-sectional study should not be interpreted as proving a causal relationship between ATS use and HIV infections, as suggested by the findings of earlier studies among IDUs and men who have sex with men (MSM) populations in the U.S., ATS use might contribute to increased HIV infection by a number of behavioral and biological pathways, including increased energy and interest in sexual activities; impaired judgment leading to increased frequency of unsafe sexual practices; increased frequency of IDU or equipment sharing; or more impulsive sharing in particularly high risk situations (see Colfax et al., 2010; Degenhardt et al., 2010 for review).
Of additional importance are the study findings that participants who know that they were HIV-infected reported comparably high rates of continued sharing of injection equipment as those without HIV infection. Despite intensive education efforts among drug users in Malaysia over the past two decades to increase their knowledge about HIV/AIDS transmission and to reduce their risky behaviors and introduction of needle exchange programs in Malaysia in 2005 (Kamarulzaman, 2009), we found that out-of-treatment heroin IDUs persisted in high rates of injection equipment sharing and that knowledge of HIV infection is not associated with reduction in rates of needle and/or equipment sharing.
4.1. Limitations
Survey participants were a non-random sample of active drug users in selected areas of three large cities with a high prevalence of IDU and may not be representative of all IDUs in the country. Notably, however, the sociodemographic characteristics of survey participants are similar to the characteristics of registered drug users in Malaysia (National Anti Drug Agency, Malaysia, 2007). The study findings are based on self-report data regarding HIV status and drug use history, and the survey assessed a limited range of behavioral risk factors (some drug-related risks, but no sexual risk behaviors). Self-reported HIV infection is likely to underestimate the actual prevalence, because of underreporting or lack of awareness of seroconversion since last testing, but the observed prevalence is consistent with verifiable health statistics in Malaysia. The close correspondence between self-reported data regarding timing of initiation of buprenorphine use and the formal approval and introduction of buprenorphine into Malaysia in 2002 supports the validity of self-reported data regarding the onset of different drug use problems by survey participants.
4.2. Implications
The study findings document the emergence over the past decade of problems with ATS use among long-term heroin IDUs in Malaysia and the significant contribution of lifetime ATS use as an additional risk factor for HIV infection. Especially because of its association with increased HIV transmission risk, the emergence of ATS use in this population threatens to interfere with the effectiveness of public health efforts underway in Malaysia and throughout the region calling for a rapid expansion of medically assisted treatments for opiate dependence to reduce the intertwined problems of heroin addiction and HIV/AIDS. The study results also point to the potential utility of incorporating surveys of not-in-treatment drug users as part of a surveillance system to monitor emerging drug use problems. As the substance abuse treatment systems expand in Malaysia and other countries in the region, routine monitoring of drug use timeline histories of individuals entering substance abuse treatments may also provide a relatively low cost and feasible approach for identifying emerging drug use patterns and potential scope of drug use problems. In this approach, reports by newly enrolling patients serve as the “canary in the coal mine” to help identify new trends in illicit drug use, since the uptake of newly emerging drugs of abuse may be most rapid among current drug users.
The study finding that knowledge of HIV serostatus (or HIV infection) is not associated with significant reduction in HIV risk behaviors underscores the importance of intensifying the educational, prevention, and treatment outreach efforts to reach populations of not-in treatment active drug users with targeted and more extensive HIV risk reduction interventions in order to effectively curtail the spread of HIV and other blood borne and infectious diseases.
Acknowledgments
Role of funding sources
A series of surveys that collected data used in this manuscript were funded by Research University Grant Scheme from Universiti Sains Malaysia in Penang. Richard S. Schottenfeld’s and Marek Chawarski’s work is supported in part by NIDA K24 DA00445 award (PI: Richard S. Schottenfeld). Their work is also supported in part by the State of Connecticut and the Connecticut Mental Health Center. None of these funding sources had any roles in study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
Footnotes
Contributors
Authors Chawarski, Vicknasingam, Mazlan, and Schottenfeld designed the study, wrote the protocol, and oversaw the implementation of the study. Authors Vicknasingam and Mazlan served as the Project Directors at Malaysia sites. Authors Chawarski, Vicknasingam, and Mazlan trained and supervised the research staff involved in the study. Authors Chawarski and Schottenfeld undertook the statistical analysis, and author Chawarski wrote the first draft of the manuscript. All authors contributed to and have approved the final manuscript.
Conflict of interest
No conflict declared.
References
- Colfax G, Santos GM, Chu P, Vittinghoff E, Pluddemann A, Kumar S, Hart C. Amphetamine-group substances and HIV. Lancet. 2010;376:458–474. doi: 10.1016/S0140-6736(10)60753-2. [DOI] [PubMed] [Google Scholar]
- Degenhardt L, Mathers B, Guarinieri M, Panda S, Phillips B, Strathdee SA, Tyndall M, Wiessing L, Wodak A, Howard J. Reference Group to the United Nations on HIV and injecting drug use Meth/amphetamine use and associated HIV: implications for global policy and public health. Int J Drug Policy. 2010;21:347–358. doi: 10.1016/j.drugpo.2009.11.007. [DOI] [PubMed] [Google Scholar]
- Department of Public Health, Ministry of Health Malaysia. [accessed 16.02.11]; Available at: http://www.dph.gov.my/aids.
- Global SMART Programme. Patterns and Trends of Amphetamine-Type Stimulants and Other Drugs: Asia and the Pacific. 2010 http://www.unodc.org/documents/scientific/ATSReport2010web.pdf.
- Kamarulzaman A. Impact of HIV prevention programs on drug users in Malaysia. J Acquir Immune Defic Syndr. 2009;S2:17–19. doi: 10.1097/QAI.0b013e3181bbc9af. [DOI] [PubMed] [Google Scholar]
- Martin M, Vanichseni S, Suntharasamai P, Mock PA, van Griensven F, Pitisuttithum P, Tappero JW, Chiamwongpaet S, Sangkum U, Kitayaporn D, Gurwith M, Choopanya K Bangkok Vaccine Evaluation Group. Drug use and the risk of HIV infection amongst injection drug users participating in an HIV vaccine trial in Bangkok, 1999–2003. Int J Drug Policy. 2010;21:296–301. doi: 10.1016/j.drugpo.2009.12.002. [DOI] [PubMed] [Google Scholar]
- McKetin R, Kozel N, Douglas J, Ali R, Vicknasingam B, Lund J, Li JH. The rise of methamphetamine in Southeast and East Asia. Drug Alcohol Rev. 2008;27:220–228. doi: 10.1080/09595230801923710. [DOI] [PubMed] [Google Scholar]
- Meandzija B, O’Connor PG, Fitzgerald B, Rounsaville BJ, Kosten TR. HIV infection and cocaine use in methadone maintained and untreated intravenous drug users. Drug Alcohol Depend. 1994;36:109–113. doi: 10.1016/0376-8716(94)90092-2. [DOI] [PubMed] [Google Scholar]
- National Anti Drug Agency, Malaysia. 2007 Available at: http://www.adk.gov.my.
- Plankey MW, Ostrow DG, Stall R, Cox C, Li X, Peck JA, Jacobson LP. The relationship between methamphetamine and popper use and risk of HIV seroconversion in the multicenter AIDS cohort study. J Acquir Immune Defic Syndr. 2007;45:85–92. doi: 10.1097/QAI.0b013e3180417c99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strathdee SA, Stockman JK. Epidemiology of HIV among injecting and non-injecting drug users: current trends and implications for interventions. Curr HIV/AIDS Rep. 2010;7:99–106. doi: 10.1007/s11904-010-0043-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutcliffe CG, Apinun Aramrattana A, Sherman SG, Sirirojn B, German D, Wongworapat K, Quan V, Keawvichit R, Celentano DD. Incidence of HIV and sexually transmitted infections and risk factors for acquisition among young methamphetamine users in northern Thailand. Sex Transm Dis. 2009;36:284–289. doi: 10.1097/OLQ.0b013e318191ba17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations Office on Drugs and Crime (UNODC) UNODC World Drug Report. United Nations Publication; 2010. Sales No. E.10.XI.13.2010. [Google Scholar]
- United Nations Office on Drugs and Crime (UNODC) UNODC World Drug Report. United Nations Publication; 2011. Sales No. E.11.XI.10.2011. [Google Scholar]
- Vicknasingam B, Mazlan M, Schottenfeld RS, Chawarski MC. Injection of buprenorphine and buprenorphine/naloxone tablets in Malaysia. Drug Alcohol Depend. 2010;111:44–49. doi: 10.1016/j.drugalcdep.2010.03.014. [DOI] [PubMed] [Google Scholar]