Abstract
Objective
Needle Free Jet Injection system with buffered lidocaine (J tip) has been shown to reduce pain for intravenous line (IV) insertion, but its relationship with successful IV placement has not been well studied. This study aimed to determine if J tip use is associated with improved first attempt IV placement success in children
Methods
This was a retrospective cohort study of children ages 1 to 18 years with emergent IV placement. Approximately 300 children were selected from each of three separate age groups: 1) 1 to 2 years, 2) 3 to 6 years and 3) 7 to 18 years. The standard treatment group (No Device) included children with an IV insertion from January 2009 through January 2010 with no J tip. The J tip treatment group (Device) included children with an IV insertion from December 2010 through December 2011 that received a J tip. Successful IV placement on first attempt was the primary outcome. Chi square test was used to compare the proportion of first attempt success and logistic regression was performed to assess the effect of device use and patient age, sex and race on first attempt success.
Results
A total of 958 children were enrolled, 501 in the No Device group and 457 in the Device group. The most common diagnoses were vomiting/dehydration (30.3%), trauma/burn (20.0%) and infection (15.5%). Overall, first attempt success was 69.0%; first attempt success was similar between the No Device (68.7%) and Device (69.4%) groups (p=0.81). No difference in first attempt success with the use of the Device was found in any of the age groups. Multivariate analysis found only age of 1 to 2 years was associated with lower odds of first attempt success.
Conclusion
The use of J tip was not associated with improved success on the first IV attempt for children. Treatment of pain during IV placement may not be sufficient to improve placement success.
INTRODUCTION
Venipuncture and intravenous line (IV) placement are common hospital procedures that cause pain and anxiety to pediatric patients and their families.1 A prospective study found that 36% of children aged 3 to 6 years and 13% of children aged 7 to 17 years experienced moderate to severe pain with venipuncture.2 This pain can result in crying, movement and resistance by the child that may result in multiple attempts before successful IV placement.3 Multiple attempts increase not only pain and dissatisfaction, but also time to treatment and supply costs.4
Successful IV placement has been shown to be affected by a number of patient factors including patient age, history of prematurity, vein visibility and palpability, as well as staff training and experience.5,6 For children in particular, pain experienced during IV placement can result in increased movement and lack of cooperation, making success more difficult.3 A study of topical lidocaine found improved IV placement success in children was associated with analgesic use suggesting an intervention to decrease pain may increase placement success.3
The Needle Free Jet Injection system with buffered lidocaine (J tip) (NDC: 8164-2001-25, National Medical Products, Inc. Irvine, CA) is an alternative intervention that provides local anesthetic at the site of administration in less than a minute. The device uses air, instead of a needle, to deliver 0.2 mL of 1% buffered lidocaine subcutaneously prior to IV insertion. A few studies have evaluated the effectiveness of this device for the treatment of pain in children. Studies in children ages 8 to 15 years and 7 to 19 years found the J tip was more effective than EMLA for the treatment of pain during venipuncture.7,8 A study in children 5 to 18 years found J tip was superior to no intervention in reducing needle stick pain, but found no difference between J tip with lidocaine and placebo J tip with normal saline.9
The relationship between J tip use and IV placement success was evaluated in prior studies of analgesic effectiveness. No difference was found between J tip and topical lidocaine cream, or between J tip, J tip with normal saline and no anesthetic.7,8,9 In two of these, all children received pain treatment, therefore the J tip was not compared to no anesthetic. These studies were also inadequately powered to determine the effect of J tip on IV success.
Since prior studies showed J tip more effectively reduced pain in children, we hypothesized that use of J tip would improve first attempt success for children. However, J tip leaves a wheal on the skin that may make IV placement more difficult; therefore, the alternative hypothesis that J tip would worsen first attempt success was also investigated. This is the first study to determine the effect of J tip compared to no anesthetic on the success of IV placement in children as young as 1 year of age.
METHODS
Study Design
This was retrospective cohort study. A quasi-experimental before-and-after design outlined below, used subjects from two different time periods. This study received Institutional Review Board approval and the requirement for written informed consent was waived.
Study Setting and Population
This study was performed in a tertiary care children’s hospital with 62,000 pediatric Emergency Department (ED) visits per year.
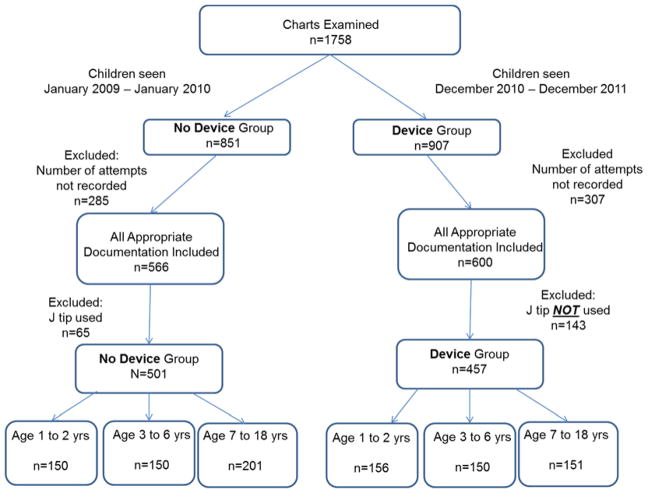
Figure 1 outlines the selection of patients. The medical records of patients evaluated in the ED with an order for intravenous line (IV) placement or IV fluids were identified during two different time periods (1) the “No Device” period, prior to widespread use of J tip in the ED (January 2009 – January 2010) and (2) the “Device” period, starting ten months after its introduction in the ED by which time it had become usual care (December 2010 – December 2011). In the “No Device” period only 11% of patients received a J tip and by the “Device” period 76% of patients received a J tip.
Figure 1.
Enrollment diagram
Duplicate records for the same patient were eliminated. Patients were stratified by age in to three groups based on developmental stages and previous research investigating characteristics associated with difficult IV access: 1 – 2 years, 3 – 6 years and 7 – 18 years.4 Records were sampled at random intervals to provide the required sample size. If inadvertent over-sampling occurred, all patients were analyzed.
Patients were included if both the IV placement and number of IV attempts were recorded in nursing documentation. Patients were excluded if documentation was illegible, an allergy to lidocaine was document, or if the patient triaged to a level 1 (the highest level of acuity). During the “No Device” period, patients were excluded if a J tip was used and in the “Device” period, patients were only included if J tip use was documented.
Study Protocol
Two trained abstractors reviewed all the written ED charts and entered the data into a standardized electronic data form. The abstractors were not blinded to the study hypothesis. Demographic characteristics of children were abstracted from ED registration information, IV placement information including placement success and number of attempts was abstracted from the written nursing documentation. Final ED discharge diagnosis, which could potentially affect IV success, was abstracted from physician documentation. Missing data was labeled as “not recorded”. Inter-rater agreement of chart abstractors was evaluated for 3% of the charts with 100% agreement.
Key outcomes measures
The primary outcome was successful first attempt IV placement. The secondary outcome was the number of documented IV attempts.
Data Analysis
Power Calculation
This study was powered to detect a 15% improvement in the primary outcome: first attempt success based on a previous studies.6 Prior to the study, first attempts success was estimated to be 55–70% and a 15% improvement was determined by experts in the field to be clinically important. 4,5,6 A change of 15% required 134 patients in each group to obtain an alpha of 0.05 (two-sided) and a beta of 0.20. An additional 10% were enrolled. Based on this priori calculation, each of the three age groups included 300 patients (150 No Device and 150 Device) for a total of 900 patients.
Statistical Analysis
Descriptive statistics were used to analyze the demographic data. Successful IV placement was reported as a percentage and compared using chi-square. Number of attempts was compared using the Wilcoxon Rank Sum for two group comparisons and Kruskal Wallis for three way comparisons. Bivariate analysis and multivariate analyses were performed to evaluate the effect of device, sex, diagnosis, race/ethnicity and age on first attempt success. A backward elimination model selection procedure was employed in multivariable analysis with forced inclusion of Device group. A statistical significance (alpha) level of 0.05 was used throughout and SAS WebEditor, version 2.5 (SAS Institute, Cary, NC) was used to perform all statistical analyses.
RESULTS
A total of 1758 charts were examined (Figure 1). Of the examined charts, 1166 charts contained required documentation about IV attempts and 958 charts met eligibility criteria and were included. The final population included 501 children with IV placement with no J tip (No Device) and 457 children with a J tip (Device) distributed amongst the three age categories.
Analysis of patient characteristics revealed significant differences in race (p=0.02) and diagnosis (p=0.02) between the No Device and Device groups, though overall groups were similar (Table 1). Comparison of the thee age groups showed younger children were more likely to be male (p=0.02) and Hispanic (p=0.01). Vomiting/Diarrhea was the most common diagnosis in children age 1 to 2 years (41.5%) and 3 to 6 years old (37.0%). The most common diagnosis in children ages 7 to 18 years was headache.
Table 1.
Patient Characteristics by Device
| Characteristic, | No Device | Device | p value |
|---|---|---|---|
| Male, n (%) | 258 (51.5) | 246 (53.8) | 0.47 |
| Race, n (%) | 0.02 | ||
| White | 242 (48.3) | 199 (43.5) | |
| Black | 176 (35.1) | 147 (32.2) | |
| Hispanic | 57 (11.4) | 68 (14.9) | |
| Other | 26 (5.2) | 43 (9.4) | |
| Diagnosis, n (%) | 0.03 | ||
| Vomiting/Diarrhea | 164 (32.7) | 126 (27.6) | |
| Trauma/Burn | 102 (20.36) | 89 (19.5) | |
| Infection | 85 (17.0) | 63 (13.8) | |
| Abdominal Pain | 31 (6.2) | 54 (11.8) | |
| Headache | 42 (8.4) | 40 (8.8) | |
| Other | 77 (15.4) | 85 (18.6) |
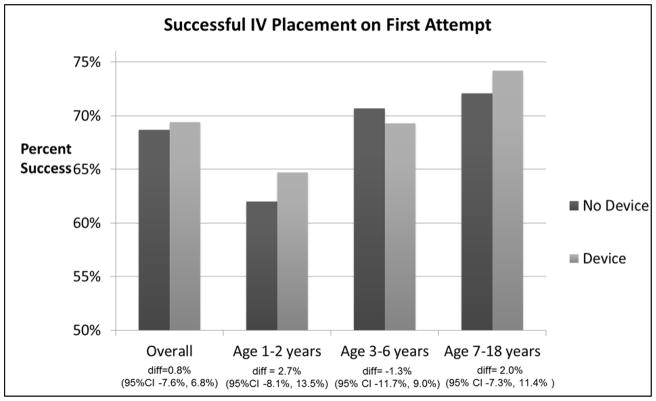
Overall, 69.0% of patients had successful first attempt IV placement. Use of the J tip was not associated with improved first attempts success (68.6% No Device v. 69.4% Device, diff +0.8%, 95% CI −6.0%, +7.6%) nor was it associated with improved first attempt success for the different age groups (Figure 2).
Figure 2.
First Attempt Success Overall and by Age Group
Analysis of the number of attempts revealed the median number of IV attempts in all patients was 1 (IQR 1, 2; range 1–7), with no difference between the No Device and Device groups. Each of the age groups also had a median of 1 attempt, but children ages 1 to 2 years had significantly more attempts (IQR 1, 2; range of 1 to 7) compared to children ages 3 to 6 years (IQR 1, 2; range 1–5) and ages 7 to 18 (IQR 1, 2; range 1– 6) (p=0.02).
Bivariate analyses were performed to evaluate patient characteristics associated with first attempt IV placement success. (Table 2) Use of the device was not associated with increased odds of first attempt success. Black children had decreased odds of first attempt success (OR 0.73, 95% CI 0.53 – 0.99) compared to white children. The youngest children, ages 1–2 years had a decreased odds of first attempts success compared to age group 7–18 years (OR 0.64, 95% CI, 0.46 – 0.89). When multivariate regression analyses was performed, only age of 1 to 2 years was found to be significantly associated with of lower odds of first attempt success (OR 0.64, 95% CI, 0.45 – 0.89) compared to children ages 7–18 years.
Table 2.
Bivariate Analysis and Multivatiate Analysis of factors associated with first attempt success for IV placement in children
| OR (95% CI) | |
|---|---|
| Bivariate Analysis | |
| Device | |
| No Device | Referent |
| Device | 1.03 (0.78, 1.36) |
| Age | |
| 1 – 2 years | 0.64 (0.46, 0.89) |
| 3 – 6 years | 0.86 (0.61, 1.22) |
| 7 – 18 years | Referent |
| Sex | |
| Male | Referent |
| Female | 0.9 (0.68, 1.19) |
| Diagnosis | |
| Trauma/Burn | Referent |
| Vomiting/Diarrhea | 0.87 (0.58, 1.30) |
| Abdominal Pain | 1.83 (0.98, 3.43) |
| Headache | 1.32 (0.73, 2.38) |
| Infection | 1.04 (0.64, 1.66) |
| Other | 0.62 (0.39, 0.96) |
| Race | |
| White | Referent |
| Black | 0.73 (0.53, 0.99) |
| Hispanic | 1.22 (0.77, 1.91) |
| Other | 1.28 (0.71, 2.29) |
| Multivariate Analysis* | |
| Device | |
| No Device | Referent |
| Device | 1.06 (0.80, 1.40) |
| Age | |
| 1 – 2 years | 0.64 (0.45, 0.89) |
| 3 – 6 years | 0.86 (0.61, 1.21) |
| 7 – 18 years | Referent |
Backwards elimination model used and only significant predictors included
DISCUSSION
This study demonstrated that 69% of children had a successful first IV attempt and use of J tip was not associated with improved first attempt success. Only age of 1 to 2 years was associated with lower success compared to older children. Further, these young children required more IV attempts to achieve IV placement.
This study does not support the hypothesis that the J tip would improve first attempt success, though there are several reasons why this may be true. These may include overall skill level of providers, patient anxiety and resistance, the use of distraction to reduce pain and other patient variables such as vein palpability and visibility that this study was unable to assess. This finding is consistent with previous smaller studies of older children that found no difference in IV placement success with J tip versus topical lidocaine cream or placebo and no anesthetic.7,8,9
The proportion of patients with an IV placed on first attempt was relatively high in this cohort at 69%. Previous studies have shown a first attempt success rate of 55–70% in children. 3,5,6 As these patients were seen in a tertiary care ED specializing in pediatric care, the nursing staff was experienced in IV placement in children. Nurses in this institution may be knowledgeable on techniques to improve cooperation, even in patients experiencing pain. The outcome may be different with providers that are not as experienced with IV placement in young children. Also, many children may be anxious and upset with IV placement, which may cause them to fight and resist placement. Treatment of pain may not significantly reduce anxiety and fighting behavior in those children.
Wide variation in the number of attempts for IV placement was found, with some children undergoing as many as seven attempts. Children ages 1 to 2 years have the lowest rate of first attempt success and were most likely to experience multiple attempts. This has been shown previously and may be due to multiple patient factors including smaller physical size, adipose tissue and developmental characteristics of this age group.5 As multiple attempts increase pain and distress, continued work is needed to determine the best treatment for pain experienced during IV placement.4
Limitations
This study has several limitations, most arising from its retrospective design. Patients without documentation of the number of IV placement attempts were excluded and may be different than patients with attempts documented. Patient factors associated with first attempt success, including palpability and visibility of the vein and prematurity, were not frequently documented in the medical record and were not included in this analysis.5 Other methods for pain reduction such as distraction or vapocoolant spray may have been used in either group and were not accounted for in this investigation due to lack of documentation.
J tip use by the nurses was discretionary. Patients for whom the nurse elected to use the J tip may have been different than patients in whom a J tip was not used. Use of the before-and-after design and inclusion of patients who received “usual care” may have minimized this effect. When all patients, regardless of J tip use, were analyzed there was still no difference in overall first attempt success between the two time periods.
Conclusion
The use of J tip is not associated with improved IV placement success. Though the device does not improve IV placement success, it has previously been shown to decrease pain with IV placement and therefore remains an option for decreasing venipuncture pain in children.7,8,9 Pain during IV placement is a significant stressor to children and families and effective interventions may reduce this stress. However, pain reduction may not independently improve IV placement success. The J tip does not change first attempt success for IV placement in children.
Acknowledgments
Funding: Support received by grant 8UL1TR000055 from the Clinical and Translational Science Award (CTSA) program of the National Center for Advancing Translational Sciences
Nicholas Philpot, MD performed data abstraction. He was a medical student at Medical College of Wisconsin and received no financial compensation.
Footnotes
Conflict of Interest: The authors have no potential conflicts of interest
Previous Presentations:
Society for Academic Emergency Medicine Annual Meeting, May 2013, Atlanta, GA Pediatric Academic Societies Annual Meeting, May 2013, Washington, DC
Contributor Information
Maren M Lunoe, Department of Pediatrics, Medical College of Wisconsin, Milwaukee, WI, USA.
Amy L Drendel, Department of Pediatrics, Medical College of Wisconsin, Milwaukee, WI, USA.
David C Brousseau, Department of Pediatrics, Medical College of Wisconsin, Milwaukee, WI, USA.
References
- 1.Smith RW, Shah V, Goldman RD, Taddio A. Caregivers’ responses to pain in their children in the emergency department. Arch Pediatr Adolesc Med. 2007;161:578–582. doi: 10.1001/archpedi.161.6.578. [DOI] [PubMed] [Google Scholar]
- 2.Fradet C, McGrath PJ, Kay J, Adams S, Luke B. A prospective survey of reactions to blood tests by children and adolescents. Pain. 1990;40:53–60. doi: 10.1016/0304-3959(90)91050-S. [DOI] [PubMed] [Google Scholar]
- 3.Taddio A, Soin HK, Schuh S, Koren G, Scolnik D. Liposomal lidocaine to improve procedural success rates and reduce procedural pain among children: a randomized controlled trial. CMAJ. 2005;172:1691–1695. doi: 10.1503/cmaj.045316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Frey AM. Success Rates for Peripheral IV Insertion in a Children’s Hospital: Financial Implications. J of Intravenous Nursing. 1998;21:160–165. [PubMed] [Google Scholar]
- 5.Yen K, Riegert A, Gorelick M. Derivation of the DIVA score: a clinical prediction rule for the identification of children with difficult intravenous access. Pediatr Emerg Care. 2008;24:143–147. doi: 10.1097/PEC.0b013e3181666f32. [DOI] [PubMed] [Google Scholar]
- 6.Riker MW, Kennedy C, Winfrey BS, Yen K, Dowd MD. Validation and Refinement of the Difficult Intravenous Access Score: A Clinical Prediction Rule for Identifying Children With Difficult Intravenous Access. Acad Emerg Med. 2011;18:1129–1134. doi: 10.1111/j.1553-2712.2011.01205.x. [DOI] [PubMed] [Google Scholar]
- 7.Spanos S, Booth R, Koenig H, Sikes K, Gracely E, Kim IK. Jet Injection of 1% Buffered Lidocaine Versus Topical ELA-Max for Anesthesia Before Peripheral Intravenous Catheterization in Children. Pediatr Emerg Care. 2008;24:511–515. doi: 10.1097/PEC.0b013e31816a8d5b. [DOI] [PubMed] [Google Scholar]
- 8.Jimenez N, Bradford H, Seidel KD, Sousa M, Lynn AM. A comparison of Needle-Free Injection System for Local Anesthesia Versus EMLA for Intravenous Catheter Insertion in the Pediatric Patient. Anesth Analg. 2006;102:411–414. doi: 10.1213/01.ane.0000194293.10549.62. [DOI] [PubMed] [Google Scholar]
- 9.Auerbach M, Tunik M, Mojica M. A randomized, double-blind controlled study of jet lidocaine compared to jet placebo for pain relief in children undergoing needle insertion in the emergency department. Acad Emerg Med. 2009;16:388–393. doi: 10.1111/j.1553-2712.2009.00401.x. [DOI] [PubMed] [Google Scholar]