Abstract
Context
A comprehensive systematic literature review of the health-related quality-of-life (HRQOL) differences among individuals with chronic ankle instability (CAI), ankle-sprain copers, and healthy control participants has not been conducted. It could provide a better indication of the self-reported deficits that may be present in individuals with CAI.
Objective
To systematically summarize the extent to which HRQOL deficits are present in individuals with CAI.
Data Sources
We searched for articles in the electronic databases of EBSCO Host and PubMed Central using key words chronic, functional, mechanical, coper, instability, sprains, and patient-assessed. We also performed a hand search of reference lists, authors, and patient-reported outcomes (PROs) of the articles screened for inclusion.
Study Selection
Studies were included if they (1) incorporated a PRO as a participant descriptor or as a study outcome to compare adults with CAI to ankle-sprain copers or healthy controls, (2) were written in English, and (3) were published in peer-reviewed journals.
Data Extraction
Two authors independently assessed methodologic quality using the modified Downs and Black Index. Articles were filtered into 3 categories based on between-groups comparisons: CAI and copers, CAI and healthy control participants, copers and healthy participants. We calculated Hedges g effect sizes and 95% confidence intervals to examine PRO group differences.
Data Synthesis
Of the 124 studies assessed for eligibility, 27 were included. A total of 24 articles compared PROs in individuals with CAI and healthy controls, 7 compared individuals with CAI and copers, and 4 compared copers and healthy controls. Quality scores on the modified Downs and Black Index ranged from 52.9% to 88.2%, with 8 high-, 16 moderate-, and 3 low-quality studies. Overall, we observed moderate to strong evidence that individuals with CAI displayed deficits on generic and region-specific PROs compared with copers and healthy controls. However, evidence that differences exist between copers and healthy controls was conflicting. In addition, for dimension-specific outcomes, evidence to suggest that fear of reinjury is heightened in individuals with CAI was limited.
Conclusions
The evidence suggested that CAI is associated with functional and HRQOL deficits, particularly when examined with region-specific PROs. However, PROs do not appear to differ between copers and healthy controls.
Key Words: region-specific outcomes, ankle sprains, patient-centered care
Key Points
Chronic ankle instability (CAI) is most likely associated with decreased health-related quality of life as measured by patient-reported outcomes.
Patient-reported outcomes did not appear to be affected in ankle-sprain copers.
Given that region-specific outcomes were worse in individuals with CAI than in ankle-sprain copers and healthy control participants, they should be considered when treating CAI and ankle sprains.
Ankle sprains are the most commonly reported injury in collegiate and high school athletics, accounting for roughly 16% of all injuries1,2; however, other estimates have indicated that ankle sprains compose up to 45% of all athletic injuries.3,4 These injuries have placed an enormous burden on the health care industry, with an estimated $4.4 billion spent annually on treatment.5 Not only are ankle sprains prevalent and costly injuries, at least one third of individuals who sustain acute ankle sprains will develop chronic ankle instability (CAI).6–8 This condition is characterized by residual symptoms that include feelings of “giving way” and instability, recurrent ankle sprains, and functional loss after 1 or more acute ankle sprains.9 Residual symptoms associated with CAI can persist for decades,10 making it difficult for an individual to lead an active, healthy lifestyle. Furthermore, the repetitive trauma associated with recurrent ankle sprains often contributes to more advanced conditions, such as ankle osteoarthritis,11 for which effective treatments are lacking.
Traditionally, CAI research has focused primarily on the pathophysiology of this condition by concentrating efforts on identifying mechanical and functional insufficiencies from a disease-oriented perspective.12–14 In the last decade, researchers15 have expanded their efforts to include the patient's perception of his or her health status, as patient-based outcomes are increasingly recognized in health care. These changes have led to the development of several patient-reported outcomes (PROs) to measure functional limitations in patients with CAI, including the Ankle Joint Functional Assessment Tool (AJFAT),16 Foot and Ankle Ability Measure (FAAM),17 and Chronic Ankle Instability Scale.18 These 3 instruments are self-reported and have been used for many ankle conditions. Their development has enabled researchers and clinicians to collect outcomes that examine a range of activities of daily living (ADLs) and sport tasks from the patient's perspective.
In the CAI literature, both discriminative (eg, Ankle Instability Instrument,19 Cumberland Ankle Instability Tool [CAIT])20 and evaluative (eg, FAAM) PROs have been used. Discriminative instruments are used to identify individuals with a particular pathologic condition (eg, CAI), whereas evaluative instruments measure an individual's perceived level of function.21 Donahue et al22 reviewed 7 instruments used to discriminate between participants with and without CAI and recommended both the CAIT and Ankle Instability Instrument to determine ankle-stability status. Furthermore, Eechaute et al23 assessed the clinimetric qualities of 4 evaluative instruments and concluded that the Foot and Ankle Disability Index (FADI) and FAAM were the most appropriate tools for quantifying functional limitations in patients with CAI. Despite these findings, the use of PROs has been inconsistent in the CAI literature. To strengthen the reporting of CAI participant information and to further our knowledge about the limitations associated with this condition, the International Ankle Consortium24 recently released a position statement in which it endorsed specific patient-selection criteria for CAI research and advocated for the use of PROs to better describe this population. In addition to the discriminatory and evaluative instruments used to quantify region-specific function in individuals with CAI, other investigators25,26 have used PROs to measure health-related quality of life (HRQOL) via generic and dimension-specific instruments. Therefore, further examining PROs used in the CAI literature may allow us to better describe the population and improve our understanding of the condition for future research and clinical practice.
A variety of PROs have been used to compare HRQOL in individuals with CAI and ankle-sprain copers (ie, individuals with a history of 1 ankle sprain and no residual symptoms) or healthy control participants. Compared with ankle-sprain copers and healthy populations, individuals with CAI appear to exhibit HRQOL deficits.25 However, to our knowledge, a comprehensive review of the differences among groups has not been conducted. Providing a comprehensive systematic review that critically appraises the research literature may offer a better indication of the self-reported deficits that may be present in those with CAI. Therefore, the purpose of our systematic review was to determine the extent to which HRQOL deficits are present in individuals with CAI.
METHODS
Literature Search Strategy
In March 2014, 2 investigators (M.N.H., M.C.H.) conducted a computerized search of EBSCO Host (CINAHL, MEDLINE, SPORTDiscus) and PubMed Central entries from their inception through March 15, 2014, to identify studies that compared HRQOL outcomes in individuals with CAI and ankle-sprain copers or healthy control participants (Table 1). Search strategies were limited to studies that were written in English, reported in peer-reviewed journals, and involved humans. In addition to the electronic search, a hand search of reference lists, authors, and PROs of the articles screened for inclusion was performed to identify pertinent articles.
Table 1.
Search Strategy
| Step |
Search Terms |
Boolean Operator |
EBSCO Host |
PubMed |
| 1 | Chronic, functional, mechanical, recurrent | OR | 1 339 297 | 1 187 097 |
| 2 | Ankle | 13 487 | 35 904 | |
| 3 | Instability, insufficiency, sprains | OR | 12 804 | 149 136 |
| 4 | 1, 2, 3 | AND | 1113 | 1631 |
| 5 | Coper, healthy, uninjured | OR | 622 314 | 397 729 |
| 6 | Assessment, form, function, instrument, measure, outcome, patient-assessed, patient-report, questionnaire, self-report, scale, score | OR | 5 176 268 | 6 339 137 |
| 7 | 4, 5, 6 | AND | 187 | 213 |
| Duplicates removed | NA | NA | 56 | 0 |
| Total | NA | NA | 131 | 213 |
| Duplicates | NA | NA | 86a |
Abbreviation: NA, not applicable.
Indicates total number of duplicates between EBSCO Host and PubMed.
Selection Criteria
All authors reviewed the articles obtained by the systematic search for inclusion. We were not blinded to study author, place of publication, or results. Titles and abstracts of all articles were screened for eligibility based on the inclusion and exclusion criteria. If we could not tell from the title and abstract whether the study met the criteria, we screened the full text of the manuscript.
Inclusion Criteria
We included articles in which researchers compared PROs in adults with CAI and ankle-sprain copers or healthy control participants. In these articles, participants in CAI groups were described as having CAI, functional ankle instability or insufficiency, mechanical ankle instability or insufficiency, or recurring ankle sprains. Participants in the ankle-sprain–coper group were described as having a history of at least 1 lateral ankle sprain more than 12 months before testing, experiencing no residual symptoms, and having resumed all preinjury activities without limitation. Participants in the healthy group were described as having no history of ankle sprain. Articles were included if the investigators used PROs (eg, AJFAT, CAIT, FAAM) as a participant descriptor or as an outcome, if they were published in the English language, and if they were published in peer-reviewed journals.
Exclusion Criteria
We excluded articles in which researchers required a minimal score for the PRO (ie, FAAM score <90%, CAIT score <24) as inclusionary criteria and articles that contained duplicate data from a previously published study. Editorials, commentaries, case studies, guidelines, conference proceedings, and review articles were also excluded.
Methodologic Quality
An adapted, 16-item version of the original Downs and Black27 Quality Index described by Munn et al28 was used to assess the methodologic quality of the included studies. The index encompasses components of the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement and has demonstrated high internal consistency and interrater reliability.27 Based on the recommendations of Munn et al,28 studies meeting less than 60% of criteria were deemed low quality; 60% to 74.9%, moderate quality; and more than 75%, high quality. Average quality index scores were calculated for all studies and within individual comparisons. Two reviewers (M.N.H., M.C.H.) independently assessed the quality of each included study, and disagreement was resolved either by discussion or a third reviewer (J.M.H.). Percentage of agreement between the reviewers was calculated.
Data Extraction
After the literature search, we initially filtered the articles into 2 categories based on the between-groups comparisons in each study (CAI and ankle-sprain copers, CAI and healthy control participants). A third comparison was conducted between ankle-sprain copers and healthy controls when the data were available. Each category compared HRQOL scores between the participant pools. If a study consisted of more than 1 between-groups comparison, each was included in all appropriate categories. The categories were subdivided into the 3 HRQOL components: generic, region specific, and dimension specific. Generic outcomes are not specific to body region or condition and are designed to assess the patient's overall health (eg, Short Form-36 [SF-36]).29 However, region-specific outcomes (eg, FAAM) are specific to a joint or region of the body, and dimension-specific outcomes (eg, Tampa Scale of Kinesiophobia-17 [TSK-17]) are specific to a disease or health dimension, such as fear of reinjury. In the region-specific category, all FADI-Sport scores identified in the literature are reported as FAAM-Sport scores because the PROs are identical instruments. Whereas similar, the FADI-ADL has 5 more items than the FAAM-ADL; thus, those scores are reported separately.
Statistical Analysis
Hedges g effect sizes and 95% confidence intervals (CIs) were calculated to examine the magnitude and precision of differences between groups.30 The Hedges g effect size is a unitless measure and represents an effect that exists on a parametric distribution.30 A positive effect size indicated lower HRQOL in the CAI group than in the coper or healthy control group. A positive effect size for the coper-to-healthy-group comparison indicated lower HRQOL in the coper group. Effect sizes were interpreted as weak (≤0.40), moderate (0.41–0.69), or strong (≥0.70).31 To further describe trends in the data, we performed a qualitative assessment of effect sizes and CIs by examining the differences in effect-size estimates between groups and determining if the CI crossed zero.
Level of Evidence
We assessed level of evidence for the included studies using method guidelines for systematic reviews adapted from the Cochrane Collaboration Back Review Group.32 The guidelines suggest using 5 levels ranging from strong to no evidence. The levels were modified to include moderate-quality studies. Consistent findings among multiple high-quality studies were classified as strong evidence. Consistent findings among multiple moderate-quality or low-quality studies were considered moderate evidence. One moderate-quality or 1 low-quality study was categorized as limited evidence. Inconsistent findings among multiple studies were classified as conflicting evidence. If no studies had been conducted, the classification was no evidence.
RESULTS
Search Strategy
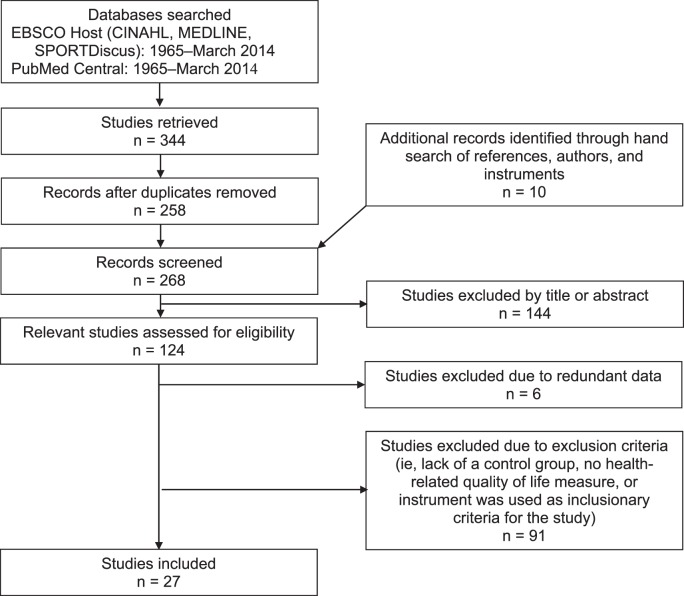
The initial search strategy retrieved 344 articles (Figure 1). Ten additional articles were obtained through a hand search of references, authors, and PROs. Of the 124 articles assessed for eligibility, 27 studies met the inclusion criteria for this systematic review.16,25,26,33–56 Six articles were excluded due to duplicate data, and 91 were excluded because researchers did not include a control group, did not report an HRQOL outcome, or used the HRQOL instrument as inclusionary criteria for the study with minimal scores required for participation. The 27 studies were classified into the following categories based on group comparison: CAI and healthy control participants, CAI and ankle-sprain copers, and ankle-sprain copers and healthy control participants. In 24 articles, authors reported HRQOL outcomes between individuals with CAI and healthy control participants.16,25,26,33,35–51,54–56 Researchers reported HRQOL outcomes between individuals with CAI and copers in 7 articles34,36,45,52–55 and between copers and healthy control participants in 4 articles.36,45,54,56 A summary of inclusion criteria, population, sample size, PRO, and study design is provided in Table 2.
Figure 1.
Flow chart of articles reviewed for inclusion.
Table 2.
Methodologic Summary of the Included Studies Continued on Next Page
| Study |
Inclusion Criteria |
Population |
Chronic Ankle Instability, No. |
Ankle-Sprain Copers, No. |
Healthy Controls, No. |
Patient-Reported Outcomes |
Study Design |
| Arnold et al,25 2011 | FAI defined as ≥1 ankle sprain, ≥1 episode of giving way per month, and a CAIT score <28. | Physically active | 34 | NA | 34 | FAAM-ADL, FAAM-Sport, Short Form-36 | Cross-sectional |
| Brown et al,34 2008 | History of acute ankle sprain within the past 5 y that required immobilization for ≥3 d. MAI and FAI groups reported ≥2 episodes of giving way in the last year. MAI group had positive anterior drawer or talar tilt. FAI and coper groups had negative anterior drawer and talar tilt. | Recreationally active | 21 MAI, 21 FAI | 21 | NA | FAAM-ADL, FAAM-Sport | Case control |
| Brown et al,33 2010 | CAI defined as a history of ≥1 moderate to severe ankle sprain that required ≥3 d of immobilization or non-weight bearing, with ≥2 episodes of giving way in the last year. Control participants reported 1 mild to moderate sprain and did not report episodes of giving way. | Recreationally active | 24 | 24 | NA | CAIT | Case control |
| Carcia et al,35 2008 | CAI defined as ≥2 ankle sprains, episodes of giving way, and residual symptoms during functional activities that limited their ability to participate. | National Collegiate Athletic Association Division II Athletes | 15 | NA | 15 | FAAM-ADL, FAAM-Sport | Cross-sectional |
| Croy et al,36 2012 | CAI defined as a history of recurrent ankle sprains and reported instability on ≥2 AII questions. Coper defined as a history of 1 ankle sprain ≥1 y ago with no residual symptoms of instability or episodes of giving way. | Recreationally active | 20 | 20 | 20 | FAAM-ADL, FAAM-Sport | Cross-sectional |
| Feger et al,37 2015 | CAI defined as a history of >1 ankle sprain with the initial sprain occurring >1 y ago and current self-reported functional deficits (FAAM-Sport <85%). | Physically active | 15 | NA | 15 | FAAM-ADL | Case control |
| Hale and Hertel,38 2005 | CAI defined as a history of ankle sprain with pain or limping for >1 d; chronic weakness, pain, or instability attributed to the initial injury; and giving way in the last 6 mo. | Recreationally active | 29 | NA | 12 | FAAM-ADL, FAAM-Sport | Repeated measures |
| Houston et al,26 2014 | CAI defined by a history of ≥1 ankle sprain, ≥2 episodes of giving way in the past 3 mo, and ≥4 questions answered yes on the AII. | Physically active | 25 | NA | 25 | Disablement in the Physically Active Scale, FAAM-ADL, FAAM-Sport, Fear-Avoidance Beliefs Questionnaire, Tampa Scale of Kinesiophobia-11 | Case control |
| Hubbard et al,39 2005 | CAI defined by the Ankle History Questionnaire. | NA | 15 | NA | 15 | FAAM-ADL, FAAM-Sport | Case control |
| Hubbard et al,41 2006 | CAI defined by the Functional Ankle Instability Questionnaire. | NA | 30 | NA | 30 | FAAM-ADL, FAAM-Sport | Case control |
| Hubbard and Cordova,40 2010 | CAI as defined by the Ankle Instability Questionnaire. | NA | 20 | NA | 20 | FAAM-ADL, FAAM-Sport | Case control |
| Kipp and Palmieri-Smith,42 2012 | CAI defined as having sustained ≥1 ankle sprain and repeated episodes of instability. | Recreationally active | 11 | NA | 11 | FAAM-ADL, FAAM-Sport | Case control |
| Marshall et al,43 2009 | CAI defined as ≥1 ankle sprain in the last year that required medical treatment and ≥1 d of missed work or training, episodes of giving way or instability of the ankle, and no current pain. | NA | 12 | NA | 12 | CAIT, FAAM-ADL, FAAM-Sport | Case control |
| Nauck and Lohrer,44 2011 | CAI defined by the Ankle Injury History Questionnaire. | Not applicable | 17 Conservative treatment, 24 preoperative | NA | 31 Sports students, 37 volley- ballers | FAAM-ADL, FAAM-Sport | Cross-sectional |
| Plante and Wikstrom,45 2013 | CAI defined as an initial ankle sprain that required immobilization or non-weight bearing for ≥3 d, multiple episodes of giving way in the past year, ≥1 recurrent sprain 3–6 mo before participation, and an AJFAT score >22. Coper defined as having an initial ankle sprain that required immobilization or non-weight bearing for ≥3 d but having resumed physical activity without limitation for ≥12 mo before participation and an AJFAT score >22. | Active adults | 25 | 21 | 20 | FAAM-ADL, FAAM-Sport | Case control |
| Ross et al,51 2005 | FAI defined as ≥2 ankle sprains (1 of which required ≥3 d of immobilization) and ≥2 episodes of giving way. | Not applicable | 10 | NA | 10 | AJFAT | Case control |
| Ross and Guskiewicz,50 2006 | FAI defined as ≥2 ankle sprains (1 of which required ≥3 d of immobilization) and ≥2 episodes of giving way. | Physically active | 10 Conventional coordination training, 10 stimulation coordination training, 10 control | NA | 10 | AJFAT | Case control |
| Ross et al,47 2008 | FAI defined as ≥2 ankle sprains (1 of which required ≥3 d of immobilization) and ≥2 episodes of giving way. | NA | 15 | NA | 15 | AJFAT | Case control |
| Ross et al,48 2009 | FAI defined as ≥2 ankle sprains (1 of which required ≥3 d of immobilization) and ≥2 episodes of giving way. | NA | 22 | NA | 22 | AJFAT | Case control |
| Ross et al,46 2011 | FAI defined as ≥1 ankle sprain and ≥2 episodes of giving way in the last year. | NA | 17 | NA | 17 | AJFAT | Case control |
| Ross et al,49 2013 | FAI defined as a history of ankle sprains and ≥2 episodes of giving way in the last year. | Recreationally active | 12 | NA | 12 | AJFAT | Case control |
| Rozzi et al,16 1999 | FAI defined as ≥2 unilateral ankle sprains and a current sense of weakness or instability. | Active university students | 13 | NA | 13 | AJFAT | Repeated measures |
| Steib et al,52 2013 | FAI defined as ≥1 moderate to severe ankle sprain within 5 y of the study and reported ≥2 episodes of giving way within the last 12 mo. Coper defined as 1 moderate to severe ankle sprain within 5 y, no residual symptoms, and a full return to preinjury activity >6 mo before testing. | Athletes from university sports programs | 19 | 19 | NA | FAAM-ADL, FAAM-Sport | Case control |
| Wikstrom et al,54 2009 | CAI defined as an ankle sprain that required immobilization or non-weight bearing for ≥3 d, multiple episodes of giving way, ≥1 recurrent sprain 3–6 mo before study participation, and an AJFAT score >22. Coper defined as having the same ankle-sprain criteria but having resumed all preinjury physical activity without limitation for ≥12 mo and an AJFAT score >22. | Recreationally active | 24 | 24 | 24 | FAAM-ADL, Self-Report Questionnaire of Ankle Function | Case control |
| Wikstrom,53 2011 | CAI defined as an ankle sprain that required immobilization or non-weight bearing for ≥3 d, multiple episodes of giving way, ≥1 recurrent sprain 3–6 mo before study participation, and an AJFAT score >22. Coper defined as having the same ankle-sprain criteria but having resumed all preinjury physical activity without limitation for ≥12 mo and an AJFAT score >22. | NA | 29 | 29 | NA | Tampa Scale of Kinesiophobia-17 | Cross-sectional |
Abbreviations: AII, Ankle Instability Instrument; AJFAT, Ankle Joint Functional Assessment Tool; CAI, chronic ankle instability; CAIT, Cumberland Ankle Instability Tool; FAAM-ADL, Foot and Ankle Ability Measure-Activities of Daily Living; FAAM-Sport, Foot and Ankle Ability Measure-Sport; FAI, functional ankle instability; MAI, mechanical ankle instability; NA, not applicable.
Methodologic Quality
Initially, the 2 reviewers agreed on 91.7% (396/432) of the items on the modified Downs and Black Index. Disagreements were resolved by discussion among the reviewers. Overall, quality scores for the studies ranged from 52.9% to 88.2%, with 8 high-quality studies (>75%), 16 moderate-quality studies (60% to 74.9%), and 3 low-quality studies (<60%). Individual item and quality index scores can be found in Table 3.
Table 3.
Adapted Downs and Black Quality Index Scores for the Included Articles
| Study |
Quality Index Score, % |
| Arnold et al,25 2011 | 70.59 |
| Brown et al,34 2008 | 70.59 |
| Brown et al,33 2010 | 64.71 |
| Carcia et al,35 2008 | 88.24 |
| Croy et al,36 2012 | 88.24 |
| Feger et al,37 2015 | 64.71 |
| Hale and Hertel,38 2005 | 52.94 |
| Houston et al,26 2014 | 70.59 |
| Hubbard et al,39 2005 | 70.59 |
| Hubbard et al,41 2006 | 82.35 |
| Hubbard and Cordova,40 2010 | 70.59 |
| Kipp and Palmieri-Smith,42 2012 | 64.71 |
| Marshall et al,43 2009 | 70.59 |
| Nauck and Lohrer,44 2011 | 52.94 |
| Plante and Wikstrom,45 2013 | 82.35 |
| Ross et al,51 2005 | 70.59 |
| Ross and Guskiewicz,50 2006 | 64.71 |
| Ross et al,47 2008 | 64.71 |
| Ross et al,48 2009 | 64.71 |
| Ross et al,46 2011 | 70.59 |
| Ross et al,49 2013 | 64.71 |
| Rozzi et al,16 1999 | 70.59 |
| Steib et al,52 2013 | 76.47 |
| Wikstrom et al,54 2009 | 82.35 |
| Wikstrom,53 2011 | 52.94 |
| Wright et al,56 2013 | 82.35 |
| Wright and Arnold,55 2012 | 76.47 |
Data Synthesis
Chronic Ankle Instability and Healthy Control Groups
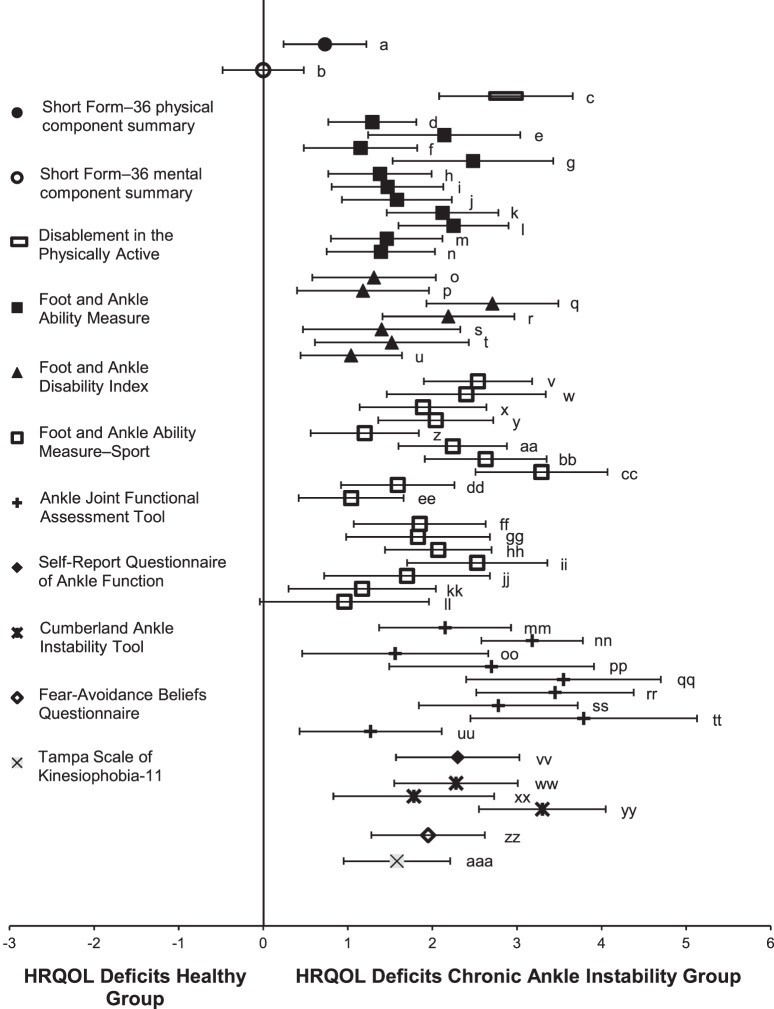
All 24 articles provided sufficient data for the calculation of effect sizes.16,25,26,33,35–51,54–56 Table 4 summarizes effect sizes and 95% CIs for the HRQOL comparison between the CAI and healthy control groups. The mean Downs and Black score for these articles was 70.8% ± 9.6%. Effect sizes and 95% CIs for HRQOL outcomes between the CAI and healthy control groups are presented in Figure 2. Of the 53 comparisons examined, 52 point estimates indicated that HRQOL was lower in the CAI group; however, the CIs of 2 point estimates crossed zero.
Table 4.
Effect Size and 95% Confidence Intervals for the Comparison Between the Chronic Ankle Instability and Healthy Control Groups
| Study |
Patient-Reported Outcome |
Hedges g |
95% Confidence Interval |
| Generic instrument | |||
| Arnold et al,25 2011 | Short Form-36 physical component summarya | 0.73 | (0.24, 1.22) |
| Arnold et al,25 2011 | Short Form-36 mental component summaryb | 0.00 | (−0.48, 0.48) |
| Houston et al,26 2014 | Disablement in the Physically Active Scalec | 2.87 | (2.08, 3.66) |
| Region-specific instrument | |||
| Arnold et al,25 2011 | FAAMd | 1.29 | (0.77, 1.81) |
| Carcia et al,35 2008 | FAAMe | 2.14 | (1.25, 3.04) |
| Croy et al,36 2012 | FAAMf | 1.15 | (0.48, 1.82) |
| Feger et al,37 2015 | FAAMg | 2.48 | (1.53, 3.43) |
| Houston et al,26 2014 | FAAMh | 1.38 | (0.76, 1.99) |
| Nauck and Lohrer (conservative treatment versus sports students),44 2011 | FAAMi | 1.47 | (0.81, 2.13) |
| Nauck and Lohrer (conservative treatment versus volleyballers),44 2011 | FAAMj | 1.58 | (0.94, 2.23) |
| Nauck and Lohrer (preoperative versus sports students),44 2011 | FAAMk | 2.12 | (1.46, 2.79) |
| Nauck and Lohrer (preoperative versus volleyballers),44 2011 | FAAMl | 2.25 | (1.60, 2.90) |
| Plante and Wikstrom,45 2013 | FAAMm | 1.46 | (0.80, 2.13) |
| Wright et al,56 2013 | FAAMn | 1.39 | (0.74, 2.03) |
| Hale and Hertel,38 2005 | FADI° | 1.31 | (0.58, 2.04) |
| Hubbard et al,39 2005 | FADIp | 1.18 | (0.41, 1.96) |
| Hubbard et al,41 2006 | FADIq | 2.71 | (2.01, 3.41) |
| Hubbard and Cordova,40 2010 | FADIr | 2.19 | (1.41, 2.97) |
| Kipp and Palmieri-Smith,42 2012 | FADIs | 1.40 | (0.47, 2.34) |
| Marshall et al,43 2009 | FADIt | 1.52 | (0.61, 2.43) |
| Wikstrom et al,54 2009 | FADIu | 1.04 | (0.43, 1.64) |
| Arnold et al,25 2011 | FAAM-Sportv | 2.54 | (1.90, 3.18) |
| Carcia et al,35 2008 | FAAM-Sportw | 2.40 | (1.46, 3.34) |
| Croy et al,36 2012 | FAAM-Sportx | 1.89 | (1.15, 2.640 |
| Houston et al,26 2014 | FAAM-Sporty | 2.04 | (1.36, 2.73) |
| Nauck and Lohrer (conservative treatment versus sports students),44 2011 | FAAM-Sportz | 1.20 | (0.56, 1.83) |
| Nauck and Lohrer (conservative treatment versus volleyballers),44 2011 | FAAM-Sportaa | 2.24 | (1.53, 2.95) |
| Nauck and Lohrer (preoperative versus sports students),44 2011 | FAAM-Sportbb | 2.63 | (1.90, 3.35) |
| Nauck and Lohrer (preoperative versus volleyballers),44 2011 | FAAM-Sportcc | 3.29 | (2.52, 4.07) |
| Plante and Wikstrom,45 2013 | FAAM-Sportdd | 1.59 | (0.92, 2.27) |
| Wright et al,56 2013 | FAAM-Sportee | 1.04 | (0.42, 1.65) |
| Hale and Hertel,38 2005 | FAAM-Sportff | 1.85 | (1.07, 2.63) |
| Hubbard et al,39 2005 | FAAM-Sportgg | 1.83 | (0.98, 2.69) |
| Hubbard et al,41 2006 | FAAM-Sporthh | 2.07 | (1.45, 2.70) |
| Hubbard and Cordova,40 2010 | FAAM-Sportii | 2.53 | (1.69, 3.36) |
| Kipp and Palmieri-Smith,42 2012 | FAAM-Sportjj | 1.70 | (0.73, 2.68) |
| Marshall et al,43 2009 | FAAM-Sportkk | 1.17 | (0.30, 2.03) |
| Wikstrom et al,54 2009 | FAAM-Sportll | 0.96 | (−0.04, 1.96) |
| Ross et al,51 2005 | AJFATmm | 2.15 | (1.05, 3.26) |
| Ross and Guskiewicz (conventional coordination training),50 2006 | AJFATnn | 3.18 | (1.86, 4.50) |
| Ross and Guskiewicz (stimulation coordination training),50 2006 | AJFAToo | 1.56 | (0.56, 2.56) |
| Ross and Guskiewicz (control),50 2006 | AJFATpp | 2.70 | (1.48, 3.91) |
| Ross et al,47 2008 | AJFATqq | 3.55 | (2.40, 4.70) |
| Ross et al,48 2009 | AJFATrr | 3.45 | (2.52, 4.39) |
| Ross et al,46 2011 | AJFATss | 2.78 | (1.84, 3.72) |
| Ross et al,49 2013 | AJFATtt | 3.79 | (2.45, 5.12) |
| Rozzi et al,16 1999 | AJFATuu | 1.27 | (0.43, 2.12) |
| Wikstrom et al,54 2009 | Self-Report Questionnaire of Ankle Functionvv | 2.30 | (1.57, 3.03) |
| Brown et al,33 2010 | CAITww | 2.28 | (1.55, 3.00) |
| Marshall et al,43 2009 | CAITxx | 1.78 | (0.84, 2.73) |
| Wright and Arnold,55 2012 | CAITyy | 3.30 | (2.55, 4.06) |
| Dimension-specific instrument | |||
| Houston et al,26 2014 | Fear-Avoidance Beliefs Questionnairezz | 1.95 | (1.28, 2.62) |
| Houston et al,26 2014 | Tampa Scale of Kinesiophobia-11aaa | 1.58 | (0.94, 2.21) |
Abbreviations: AJFAT, Ankle Joint Functional Assessment Tool; CAIT, Cumberland Ankle Instability Tool; FAAM, Foot and Ankle Ability Measure; FAAM-Sport, Foot and Ankle Ability Measure-Sport; FADI, Foot and Ankle Disability Index.
a–aaa Corresponds with lettering in Figure 2.
Figure 2.
Summary of Hedges g effect sizes and 95% confidence intervals for the comparison between the chronic ankle instability and healthy control groups.a–aaa Corresponds with the actual values presented in Table 4. Abbreviation: HRQOL, health-related quality of life.
Effect sizes ranged from 0.00 to 3.79, suggesting that individuals with CAI reported HRQOL deficits compared with healthy control participants. For generic outcomes, a strong effect (g = 0.73) was found for the SF-36 Physical Component Summary (SF-36 PCS), indicating that individuals with CAI reported decreased physical health on the SF-36; however, no effect was present for the SF-36 Mental Component Summary (SF-36 MCS). In addition, a strong effect (g = 2.87) was observed for the Disablement in the Physically Active (DPA) Scale, suggesting that individuals with CAI reported increased disablement compared with healthy control participants. A strong effect ranging from 0.96 to 3.79 was observed for region-specific outcomes. Effect sizes for the FAAM and FAAM-Sport ranged from 0.96 to 3.29, indicating that individuals with CAI reported decreased ankle function during ADLs and sport. Similarly, effect sizes for the FADI ranged from 1.04 to 2.71. In addition, strong effects were found for the AJFAT (g range = 1.27 to 3.79), Self-Report Questionnaire of Ankle Function (SRQAF; g = 2.30), and CAIT (g range = 1.78 to 3.30). Lastly, both dimension-specific outcomes, the Fear-Avoidance Beliefs Questionnaire (FABQ; g = 1.95) and the TSK-11 (g = 1.58), demonstrated strong effects, suggesting that individuals with CAI exhibited heightened fear of reinjury.
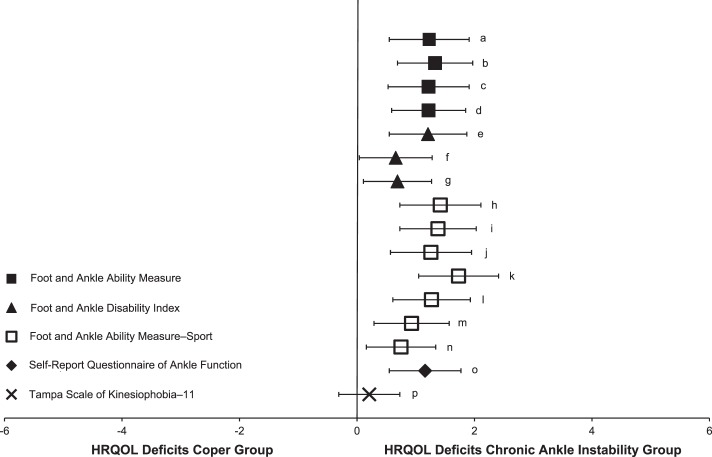
Chronic Ankle Instability and Ankle-Sprain–Coper Groups
All 7 articles provided sufficient data for the calculation of effect sizes.34,36,45,52–54,56 Table 5 summarizes effect sizes and 95% CIs for the HRQOL comparison between the CAI and ankle-sprain–coper groups. The mean Downs and Black score for these articles was 76.5% ± 11.8%. Effect sizes and 95% CIs for HRQOL outcomes between the CAI and coper groups are presented in Figure 3. All 16 comparisons indicated that HRQOL was lower in the CAI group; however, 1 of the CIs crossed zero.
Table 5.
Effect Size and 95% Confidence Intervals for the Comparison Between the Chronic Ankle Instability and Ankle-Sprain–Coper Groups
| Study |
Patient-Reported Outcome |
Hedges g |
95% Confidence Interval |
| Region-specific instrument | |||
| Croy et al,36 2012 | FAAMa | 1.23 | (0.55, 1.91) |
| Plante and Wikstrom,45 2013 | FAAMb | 1.33 | (0.69, 1.98) |
| Steib et al,52 2013 | FAAMc | 1.22 | (0.53, 1.91) |
| Wright et al,56 2013 | FAAMd | 1.22 | (0.59, 1.85) |
| Brown et al (mechanical ankle instability),34 2008 | FADIe | 1.21 | (0.55, 1.86) |
| Brown et al (functional ankle instability),34 2008 | FADIf | 0.66 | (0.04, 1.28) |
| Wikstrom et al,54 2009 | FADIg | 0.69 | (0.11, 1.27) |
| Croy et al,36 2012 | FAAM-Sporth | 1.42 | (0.73, 2.12) |
| Plante and Wikstrom,45 2013 | FAAM-Sporti | 1.38 | (0.74, 2.03) |
| Steib et al,52 2013 | FAAM-Sportj | 1.26 | (0.57, 1.96) |
| Wright et al,56 2013 | FAAM-Sportk | 1.73 | (1.05, 2.40) |
| Brown et al (mechanical ankle instability),34 2008 | FAAM-Sportl | 1.27 | (0.61, 1.94) |
| Brown et al (functional ankle instability),34 2008 | FAAM-Sportm | 0.93 | (0.29, 1.56) |
| Wikstrom et al,54 2009 | FAAM-Sportn | 0.75 | (0.16, 1.34) |
| Wikstrom et al,54 2009 | Self-Report Questionnaire of Ankle Function° | 1.16 | (0.55, 1.77) |
| Dimension-specific instrument | |||
| Wikstrom,53 2011 | Tampa Scale of Kinesiophobia-17p | 0.21 | (−0.30, 0.73) |
Abbreviations: FAAM, Foot and Ankle Ability Measure; FAAM-Sport, Foot and Ankle Ability Measure-Sport; FADI, Foot and Ankle Disability Index.
a–p Corresponds with lettering in Figure 3.
Figure 3.
Summary of Hedges g effect sizes and 95% confidence intervals for the comparison between the chronic ankle instability and ankle-sprain–coper groups.a–p Corresponds with the actual values presented in Table 5. Abbreviation: HRQOL, health-related quality of life.
Effect sizes ranged from 0.21 to 1.73, suggesting that individuals with CAI reported HRQOL deficits in comparison with ankle-sprain copers. No generic outcome scores were reported for this comparison. Moderate to strong effects (g range = 0.66 to 1.73) were found for all region-specific outcomes. A strong effect (g range = 0.75 to 1.73) was observed for the FAAM and FAAM-Sport, indicating that individuals with CAI reported decreased ankle function during ADLs and sport. However, moderate to strong effect sizes (g range = 0.66 to 1.21) were observed for the FADI. A strong effect was also reported for the SRQAF (g = 1.16). A weak effect (g = 0.21) was observed for the only dimension-specific outcome, suggesting that individuals with CAI reported increased kinesiophobia compared with copers; however, the CI crossed zero.
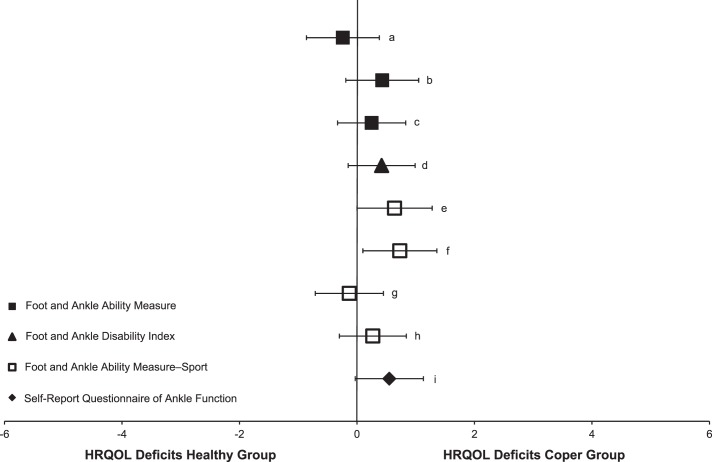
Ankle-Sprain–Coper and Healthy Control Groups
All 4 articles provided sufficient data for the calculation of effect sizes.36,45,54,56 Table 6 summarizes effect sizes and 95% CIs for the HRQOL comparison between ankle-sprain–coper and healthy control groups. The mean Downs and Black score for these articles was 83.9% ± 2.5%. Effect sizes and 95% CIs for HRQOL outcomes between the coper and healthy control groups are presented in Figure 4. Of the 9 comparisons examined, 7 point estimates indicated that HRQOL was lower in the coper group; however, 2 point estimates showed lower HRQOL in the healthy control group. In addition, 8 of 9 CIs crossed zero.
Table 6.
Effect Size and 95% Confidence Intervals for the Comparison Between the Ankle-Sprain–Coper and Healthy Control Groups
| Study |
Patient-Reported Outcome |
Hedges g |
95% Confidence Interval |
| Croy et al,36 2012 | FAAMa | −0.24 | (−0.87, 0.38) |
| Plante and Wikstrom,45 2013 | FAAMb | 0.43 | (−0.20, 1.05) |
| Wright et al,56 2013 | FAAMc | 0.25 | (−0.33, 0.83) |
| Wikstrom et al,54 2009 | Foot and Ankle Disability Indexd | 0.42 | (−0.15, 0.99) |
| Croy et al,36 2012 | FAAM-Sporte | 0.64 | (0.00, 1.27) |
| Plante and Wikstrom,45 2013 | FAAM-Sportf | 0.73 | (0.09, 1.36) |
| Wright et al,56 2013 | FAAM-Sportg | −0.13 | (−0.70, 0.45) |
| Wikstrom et al,54 2009 | FAAM-Sporth | 0.27 | (−0.29, 0.83) |
| Wikstrom et al,54 2009 | Self-Report Questionnaire of Ankle Functioni | 0.55 | (−0.02, 1.13) |
Abbreviations: FAAM, Foot and Ankle Ability Measure; FAAM-Sport, Foot and Ankle Ability Measure-Sport.
a–i Corresponds with lettering in Figure 4.
Figure 4.
Summary of Hedges g effect sizes and 95% confidence intervals for the comparison between the ankle-sprain–coper and healthy control groups.a–i Corresponds with the actual values presented in Table 6. Abbreviation: HRQOL, health-related quality of life.
Effect sizes were inconsistent, ranging from −0.24 to 0.73. No generic or dimension-specific outcomes were reported for this comparison. For region-specific outcomes, FAAM effect sizes ranged from −0.24 to 0.43. Two comparisons favored decreased FAAM scores in the coper group, and 1 comparison suggested the healthy control group exhibited decreased FAAM scores. Similar trends were identified for the FAAM-Sport, with effect sizes ranging from −0.13 to 0.73. A moderate effect (g = 0.42) was found for the FADI, indicating that the coper group exhibited decreased function compared with the healthy control group. In addition, a moderate effect was found for the SRQAF (g = 0.55), reflecting decreased function in the coper group.
Level of Evidence
For generic outcomes, moderate evidence supported differences between the CAI and healthy control groups based on consistent findings of 2 moderate-quality studies.25,26 Generic outcomes have not been used to compare HRQOL between CAI and coper groups or coper and healthy control groups. For region-specific outcomes, individuals with CAI reported lower scores than healthy control participants and ankle-sprain copers. This result was based on consistent findings in 27 studies,16,25,26,33–56 8 of which were high quality. However, evidence that differences exist between the ankle-sprain–coper and healthy control groups was conflicting based on inconsistent findings among 4 high-quality studies.36,45,54,56 For dimension-specific outcomes, evidence to suggest that fear of reinjury was heightened in the CAI group compared with the healthy control group was limited and based on the findings of 1 moderate-quality study.26 In addition, evidence to indicate that kinesiophobia scores were similar between the CAI and coper groups was limited and based on the findings of 1 low-quality study.53 Fear-of-reinjury instruments have not been used to compare ankle-sprain copers and healthy control participants.
DISCUSSION
The purpose of this systematic review was to determine the extent to which HRQOL deficits were present in individuals with CAI compared with ankle-sprain copers and healthy control participants. We also compared HRQOL deficits between ankle-sprain copers and healthy control participants when these data were available in the included studies. After reviewing the literature, our findings suggested that individuals with CAI experienced HRQOL deficits, particularly when measured using region-specific outcomes. However, limited to moderate evidence was available to support deficits on dimension-specific and generic instruments. Furthermore, evidence that HRQOL deficits are present in ankle-sprain copers compared with healthy control participants was conflicting. Consequently, we organized the following discussion by outcome type (ie, generic, region specific, and dimension specific) to generate a concise summary of each component of HRQOL.
Generic Instruments
Based on our systematic review, we found moderate evidence to suggest that individuals with CAI experienced HRQOL deficits compared with healthy control participants on generic instruments. Authors of 2 moderate-quality studies25,26 used generic instruments to compare HRQOL between CAI and healthy control groups. Arnold et al25 used the SF-36 and found a strong effect (g = 0.73) with a narrow CI for the SF-36 PCS; however, they observed no effect for the SF-36 MCS. The lack of consistency between outcome summary components may be attributed to differences in scale constructs. For example, the SF-36 PCS is a physical health summary consisting of 4 subscales: physical functioning, physical role, bodily pain, and general health. Conversely, the SF-36 MCS is a mental health summary consisting of 4 subscales: vitality, social functioning, emotional role, and mental health. Therefore, individuals with CAI may report decreased physical health but unaffected mental health. However, Houston et al26 noted a very strong effect (g = 2.87) with a narrow CI for the DPA, and 4 of the 16 DPA items pertain to the emotional well-being of the individual.
To better understand the influence of CAI on generic function, we need more research. Investigators should examine the effect of CAI on other measures of generic function, such as the Short Form-12, which offers the advantage of brevity, and should consider selecting generic instruments that are better suited for the population. For example, the DPA was designed for use in physically active individuals,57 and authors of 16 studies included in our review recruited physically active participants or athletes. Knowing that athletes exhibited better HRQOL on outcomes such as the SF-36,58,59 we must consider instrument appropriateness for the population. Studying the effect of CAI on generic function by using more than 1 outcome and outcomes appropriate for the sampled population will help us to better describe deficits associated with the condition.
Region-Specific Instruments
Overall, we found strong evidence to suggest that individuals with CAI reported lower region-specific outcomes than did healthy control participants and ankle-sprain copers. Moderate to strong effects (g range = 0.66 to 3.79) demonstrated differences between the CAI and healthy control groups and the CAI and coper groups. The evidence to support such differences among region-specific measures unique to the foot and ankle region, including the FAAM, FADI, CAIT, and AJFAT, was strong. Therefore, such measures should continue to be used in research and clinical practice to describe functional limitations in individuals with CAI. However, given the similarities between the FAAM and FADI, we highly recommend that clinicians and researchers use only the FAAM in the future. The FAAM's shortened format and the rigorous validation process the tool underwent during development17 make it the preferred PRO. Furthermore, clinicians should begin monitoring patient progress via such outcomes to ensure complete recovery after injury.
We found conflicting evidence to support region-specific differences between the ankle-sprain–coper and healthy control groups. Croy et al36 observed a weak effect (g = −0.24), suggesting that healthy control participants reported decreased function; yet Plante and Wikstrom45 identified a strong effect (g = 0.73), suggesting that ankle-sprain copers reported decreased function. The lack of consistency between studies and the broad CIs indicate that region-specific differences may not exist between ankle-sprain copers and healthy control participants. These findings further substantiate the likelihood that individuals with CAI have unique impairments that create functional limitations. In addition, ankle-sprain copers returned to similar levels of activity and involvement compared with healthy control participants. Accordingly, functional limitations should be considered when attempting to discriminate between individuals with CAI and ankle-sprain copers.
Dimension-Specific Instruments
The limited evidence regarding differences in dimension-specific outcomes makes it unclear how fear of reinjury, kinesiophobia, or other HRQOL dimensions affect individuals with CAI. Authors of 2 studies used fear-of-reinjury instruments to make comparisons. Houston et al26 used the FABQ and the TSK-11 to compare individuals with CAI and healthy control participants. Both the FABQ (g = 1.95) and the TSK-11 (g = 1.58) exhibited strong effects, indicating that individuals with CAI reported a heightened fear of reinjury. The only other comparison using a dimension-specific outcome was between individuals with CAI and copers; therefore, all participants had a history of at least 1 ankle sprain. Wikstrom53 observed a weak effect (g = 0.21) between groups, suggesting that the CAI group reported increased kinesiophobia on the TSK-17 compared with the copers, but the CI crossed zero. The weak relationship may have been due to the history of ankle sprain in both groups. Therefore, more evidence is needed to understand how CAI or the history of previous injury affects this aspect of function.
Clinical Relevance
The results of this systematic review indicated that functional limitations and HRQOL deficits were reported by individuals with CAI but not by ankle-sprain copers and healthy control participants; however, functional limitations and HRQOL deficits did not appear to be present when comparing ankle-sprain copers and healthy control participants. Whereas the evidence pertaining to generic and dimension-specific outcomes is limited, it is apparent that CAI contributes to self-reported region-specific deficits. For this reason, clinicians should consider monitoring region-specific function when treating patients with ankle sprains and CAI. Furthermore, investigating patient perceptions may reveal characteristics distinct to the individual's impairment and help guide rehabilitation. Tailoring rehabilitation efforts and treatments to the individual patient's goals and values will advance patient-centered care60 and, in turn, may improve the quality of care that rehabilitation specialists provide.
To supply clinical context and recommendations for monitoring functional limitations and HRQOL, it would be useful to compare the mean difference between groups to the minimal detectable change (MDC) or minimal clinically important difference (MCID) scores previously established in the literature. The MDC is an estimate of the smallest amount of change required to exceed measurement variability (ie, objective change),61 whereas the MCID indicates the smallest difference that a patient perceives as beneficial (ie, subjective change).62 To our knowledge, only 3 of the 12 PROs represented in this study have established MDC or MCID scores. Change scores for the other PROs either were not representative of CAI populations or have not been reported. In individuals with CAI, MDC or MCID (or both) scores have been reported for the FAAM (MDC = 7.76%,63 MCID = 9.50%17), FAAM-Sport (MDC = 15.48%,63 MCID = 28.10%17), and FADI (MDC = 7.23%38). Examining the mean differences between the CAI and healthy groups compared with MDC and MCID scores in the literature showed that 63.6% (7/11) of the point estimates observed for the FAAM exceeded both the MDC and MCID. On the FAAM-Sport, 70.6% (12/17) exceeded the MDC score, but only 17.6% (3/17) surpassed the MCID. These observations suggest that, although individuals with CAI reported functional limitations on the FAAM that appear to be beyond measurement variability, patients may not perceive those limitations related to sport tasks as relevant. Similar observations were noted between the CAI and coper groups, with 50% of the point estimates exceeding the MDC and MCID for the FAAM (2/4); however, only 28.6% exceeded the MDC for the FAAM-Sport (2/7), and none of the FAAM-Sport (0/7) point estimates surpassed the MCID. Whereas an MCID score was not available for the FADI, 57.1% (4/7) of the point estimates exceeded the MDC. Hence, the FADI appears to detect an objective difference between groups by exceeding measurement variability. The variability between the CAI and coper groups was much less, with only 33.3% (1/3) of the point estimates exceeding the MDC for the FADI. None of the point estimates exceeded MDC or MCID scores for the comparison between coper and healthy control groups. The lack of MCID scores for the FADI further substantiates the need for the FAAM to be used in future research and clinical endeavors. As stated, only 3 of the 12 (25.0%) outcome measures identified in the CAI literature had MDC or MCID values relevant to this group. Therefore, although an array of PROs are used in the CAI literature, the lack of change scores is a major confounder to clinical interpretation.
Limitations
Whereas this systematic review was designed based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses64 (PRISMA) guidelines, limitations still need to be addressed. We conducted the electronic searches in databases considered to be the most relevant to CAI and followed up with a hand search of references, authors, and PROs in the identified studies; however, other evidence is possibly available. Our search was also limited to studies published in English and peer-reviewed journals, but we do not believe any relevant articles were excluded by these search criteria. In addition, although we excluded articles that had a PRO criterion for participant inclusion, some studies may have had a PRO criterion that was not specified in the manuscript. Articles that had a PRO criterion for inclusion were excluded in an attempt to capture the entire spectrum of individuals with CAI, as individuals with CAI may meet other selection criteria24 but not report functional deficits on the FAAM. Furthermore, CAI or coper groups may have differed due to the lack of universal definitions for CAI and coper. However, participants in each study included in the CAI group were defined as having CAI, mechanical ankle instability or insufficiency, functional ankle instability or insufficiency, or recurring ankle sprain, and participants included in the ankle-sprain coper group were defined as having a history of at least 1 ankle sprain with no residual complications. Brown et al33 defined control participants as reporting no more than 1 mild to moderate sprain and no episodes of giving way and, therefore, included them as a coper group. Lastly, whereas most authors required participants to have sustained their ankle sprains at least 6 weeks before the study, it is unclear how time since injury could influence PRO scores.
CONCLUSIONS
A systematic search of the literature revealed 27 studies in which authors compared PROs in individuals with CAI, ankle-sprain copers, and healthy control participants. The evidence suggested that CAI is most likely associated with decreased HRQOL as measured by PROs. However, PROs did not appear to be affected in ankle-sprain copers, who typically had sustained 1 acute ankle sprain. It is clear that region-specific outcomes are lower in individuals with CAI than in ankle-sprain copers and healthy control participants. Therefore, region-specific outcomes should be considered when treating patients with CAI and ankle sprains. Yet the relationship between CAI and generic and dimension-specific outcomes remains unclear and warrants further investigation. By investigating the effect of CAI on patient-perceived perceptions of physical limitations and HRQOL, we may further our understanding of this multifaceted condition.
REFERENCES
- 1.Hootman JM, Dick R, Agel J. Epidemiology of collegiate injuries for 15 sports: summary and recommendations for injury prevention initiatives. J Athl Train. 2007;42(2):311–319. [PMC free article] [PubMed] [Google Scholar]
- 2.Swenson DM, Collins CL, Fields SK, Comstock RD. Epidemiology of US high school sports-related ligamentous ankle injuries, 2005/06–2010/11. Clin J Sport Med. 2013;23(3):190–196. doi: 10.1097/JSM.0b013e31827d21fe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fong DT, Hong Y, Chan LK, Yung PS, Chan KM. A systematic review on ankle injury and ankle sprain in sports. Sports Med. 2007;37(1):73–94. doi: 10.2165/00007256-200737010-00006. [DOI] [PubMed] [Google Scholar]
- 4.Ferran NA, Maffulli N. Epidemiology of sprains of the lateral ankle ligament complex. Foot Ankle Clin. 2006;11(3):659–662. doi: 10.1016/j.fcl.2006.07.002. [DOI] [PubMed] [Google Scholar]
- 5.Soboroff SH, Pappius EM, Komaroff AL. Benefits, risks, and costs of alternative approaches to the evaluation and treatment of severe ankle sprain. Clin Orthop Relat Res. 1984;183:160–168. [PubMed] [Google Scholar]
- 6.Anandacoomarasamy A, Barnsley L. Long term outcomes of inversion ankle injuries. Br J Sports Med. 2005;39(3):e14. doi: 10.1136/bjsm.2004.011676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Konradsen L, Bech L, Ehrenbjerg M, Nickelsen T. Seven years follow-up after ankle inversion trauma. Scand J Med Sci Sports. 2002;12(3):129–135. doi: 10.1034/j.1600-0838.2002.02104.x. [DOI] [PubMed] [Google Scholar]
- 8.Braun BL. Effects of ankle sprain in a general clinic population 6 to 18 months after medical evaluation. Arch Fam Med. 1999;8(2):143–148. doi: 10.1001/archfami.8.2.143. [DOI] [PubMed] [Google Scholar]
- 9.Delahunt E, Coughlan GF, Caulfield B, Nightingale EJ, Lin C, Hiller CE. Inclusion criteria when investigating insufficiencies in chronic ankle instability. Med Sci Sports Exerc. 2010;42(11):2106–2121. doi: 10.1249/MSS.0b013e3181de7a8a. [DOI] [PubMed] [Google Scholar]
- 10.Lofvenberg R, Karrholm J, Lund B. The outcome of nonoperated patients with chronic lateral instability of the ankle: a 20-year follow-up study. Foot Ankle Int. 1994;15(4):165–169. doi: 10.1177/107110079401500401. [DOI] [PubMed] [Google Scholar]
- 11.Valderrabano V, Hintermann B, Horisberger M, Fung TS. Ligamentous posttraumatic ankle osteoarthritis. Am J Sports Med. 2006;34(4):612–620. doi: 10.1177/0363546505281813. [DOI] [PubMed] [Google Scholar]
- 12.Hertel J. Sensorimotor deficits with ankle sprains and chronic ankle instability. Clin Sports Med. 2008;27(3):353–370. doi: 10.1016/j.csm.2008.03.006. vii. [DOI] [PubMed] [Google Scholar]
- 13.Hubbard TJ, Kramer LC, Denegar CR, Hertel J. Contributing factors to chronic ankle instability. Foot Ankle Int. 2007;28(3):343–354. doi: 10.3113/FAI.2007.0343. [DOI] [PubMed] [Google Scholar]
- 14.Hubbard TJ, Hertel J. Mechanical contributions to chronic lateral ankle instability. Sports Med. 2006;36(3):263–277. doi: 10.2165/00007256-200636030-00006. [DOI] [PubMed] [Google Scholar]
- 15.Parker J, Nester CJ, Long AF, Barrie J. The problem with measuring patient perceptions of outcome with existing outcome measures in foot and ankle surgery. Foot Ankle Int. 2003;24(1):56–60. doi: 10.1177/107110070302400109. [DOI] [PubMed] [Google Scholar]
- 16.Rozzi SL, Lephart SM, Sterner R, Kuligowski L. Balance training for persons with functionally unstable ankles. J Orthop Sports Phys Ther. 1999;29(8):478–486. doi: 10.2519/jospt.1999.29.8.478. [DOI] [PubMed] [Google Scholar]
- 17.Martin RL, Irrgang JJ, Burdett RG, Conti SF, Van Swearingen JM. Evidence of validity for the Foot and Ankle Ability Measure (FAAM) Foot Ankle Int. 2005;26(11):968–983. doi: 10.1177/107110070502601113. [DOI] [PubMed] [Google Scholar]
- 18.Eechaute C, Vaes P, Duquet W. The chronic ankle instability scale: clinimetric properties of a multidimensional, patient-assessed instrument. Phys Ther Sport. 2008;9(2):57–66. doi: 10.1016/j.ptsp.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 19.Docherty CL, Gansneder BM, Arnold BL, Hurwitz SR. Development and reliability of the Ankle Instability Instrument. J Athl Train. 2006;41(2):154–158. [PMC free article] [PubMed] [Google Scholar]
- 20.Hiller CE, Refshauge KM, Bundy AC, Herbert RD, Kilbreath SL. The Cumberland Ankle Instability Tool: a report of validity and reliability testing. Arch Phys Med Rehabil. 2006;87(9):1235–1241. doi: 10.1016/j.apmr.2006.05.022. [DOI] [PubMed] [Google Scholar]
- 21.Kirshner B, Guyatt G. A methodological framework for assessing health indices. J Chronic Dis. 1985;38(1):27–36. doi: 10.1016/0021-9681(85)90005-0. [DOI] [PubMed] [Google Scholar]
- 22.Donahue M, Simon J, Docherty CL. Critical review of self-reported functional ankle instability measures. Foot Ankle Int. 2011;32(12):1140–1146. doi: 10.3113/FAI.2011.1140. [DOI] [PubMed] [Google Scholar]
- 23.Eechaute C, Vaes P, Van Aerschot L, Asman S, Duquet W. The clinimetric qualities of patient-assessed instruments for measuring chronic ankle instability: a systematic review. BMC Musculoskelet Disord. 2007;8:6. doi: 10.1186/1471-2474-8-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gribble PA, Delahunt E, Bleakley C, et al. Selection criteria for patients with chronic ankle instability in controlled research: a position statement of the International Ankle Consortium. J Orthop Sports Phys Ther. 2013;43(8):585–591. doi: 10.2519/jospt.2013.0303. [DOI] [PubMed] [Google Scholar]
- 25.Arnold BL, Wright CJ, Ross SE. Functional ankle instability and health-related quality of life. J Athl Train. 2011;46(6):634–641. doi: 10.4085/1062-6050-46.6.634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Houston MN, Van Lunen B, Hoch MC. Health-related quality of life in individuals with chronic ankle instability. J Athl Train. 2014;49(6):758–763. doi: 10.4085/1062-6050-49.3.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52(6):377–384. doi: 10.1136/jech.52.6.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Munn J, Sullivan SJ, Schneiders AG. Evidence of sensorimotor deficits in functional ankle instability: a systematic review with meta-analysis. J Sci Med Sport. 2010;13(1):2–12. doi: 10.1016/j.jsams.2009.03.004. [DOI] [PubMed] [Google Scholar]
- 29.Snyder AR. Valovich McLeod TC. Selecting patient-based outcome measures. Athl Ther Today. 2007;12(6):12–15. [Google Scholar]
- 30.Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to Meta-Analysis. West Sussex, United Kingdom: John Wiley & Sons, Ltd;; 2009. pp. 21–291. [Google Scholar]
- 31.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Associates;; 1988. pp. 20–26. [Google Scholar]
- 32.Van Tulder M, Furlan A, Bombardier C, Bouter L. Updated method guidelines for systematic reviews in the Cochrane Collaboration Back Review Group. Spine (Phila Pa 1976) 2003;28(12):1290–1299. doi: 10.1097/01.BRS.0000065484.95996.AF. [DOI] [PubMed] [Google Scholar]
- 33.Brown CN, Bowser B, Orellana A. Dynamic postural stability in females with chronic ankle instability. Med Sci Sports Exerc. 2010;42(12):2258–2263. doi: 10.1249/MSS.0b013e3181e40108. [DOI] [PubMed] [Google Scholar]
- 34.Brown C, Padua D, Marshall SW, Guskiewicz K. Individuals with mechanical ankle instability exhibit different motion patterns than those with functional ankle instability and ankle sprain copers. Clin Biomech (Bristol, Avon) 2008;23(6):822–831. doi: 10.1016/j.clinbiomech.2008.02.013. [DOI] [PubMed] [Google Scholar]
- 35.Carcia CR, Martin RL, Drouin JM. Validity of the Foot and Ankle Ability Measure in athletes with chronic ankle instability. J Athl Train. 2008;43(2):179–183. doi: 10.4085/1062-6050-43.2.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Croy T, Saliba SA, Saliba E, Anderson MW, Hertel J. Differences in lateral ankle laxity measured via stress ultrasonography in individuals with chronic ankle instability, ankle sprain copers, and healthy individuals. J Orthop Sports Phys Ther. 2012;42(7):593–600. doi: 10.2519/jospt.2012.3923. [DOI] [PubMed] [Google Scholar]
- 37.Feger M, Donovan L, Hart J, Hertel J. Lower extremity muscle activation in patients with or without chronic ankle instability during walking. J Athl Train. 2015;50(4):350–357. doi: 10.4085/1062-6050-50.2.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hale SA, Hertel J. Reliability and sensitivity of the Foot and Ankle Disability Index in subjects with chronic ankle instability. J Athl Train. 2005;40(1):35–40. [PMC free article] [PubMed] [Google Scholar]
- 39.Hubbard TJ, Olmsted-Kramer LC, Hertel J, Sherbondy P. Anterior-posterior mobility of the talus in subjects with chronic ankle instability. Phys Ther Sport. 2005;6(3):146–152. [Google Scholar]
- 40.Hubbard TJ, Cordova M. Effect of ankle taping on mechanical laxity in chronic ankle instability. Foot Ankle Int. 2010;31(6):499–504. doi: 10.3113/FAI.2010.0499. [DOI] [PubMed] [Google Scholar]
- 41.Hubbard TJ, Hertel J, Sherbondy P. Fibular position in individuals with self-reported chronic ankle instability. J Orthop Sports Phys Ther. 2006;36(1):3–9. doi: 10.2519/jospt.2006.36.1.3. [DOI] [PubMed] [Google Scholar]
- 42.Kipp K, Palmieri-Smith RM. Principal component based analysis of biomechanical inter-trial variability in individuals with chronic ankle instability. Clin Biomech (Bristol, Avon) 2012;27(7):706–710. doi: 10.1016/j.clinbiomech.2012.02.005. [DOI] [PubMed] [Google Scholar]
- 43.Marshall PW, McKee AD, Murphy BA. Impaired trunk and ankle stability in subjects with functional ankle instability. Med Sci Sports Exerc. 2009;41(8):1549–1557. doi: 10.1249/MSS.0b013e31819d82e2. [DOI] [PubMed] [Google Scholar]
- 44.Nauck T, Lohrer H. Translation, cross-cultural adaption and validation of the German version of the Foot and Ankle Ability Measure for patients with chronic ankle instability. Br J Sports Med. 2011;45(10):785–790. doi: 10.1136/bjsm.2009.067637. [DOI] [PubMed] [Google Scholar]
- 45.Plante JE, Wikstrom EA. Differences in clinician-oriented outcomes among controls, copers, and chronic ankle instability groups. Phys Ther Sport. 2013;14(4):221–226. doi: 10.1016/j.ptsp.2012.09.005. [DOI] [PubMed] [Google Scholar]
- 46.Ross SE, Linens SW, Wright CJ, Arnold BL. Balance assessments for predicting functional ankle instability and stable ankles. Gait Posture. 2011;34(4):539–542. doi: 10.1016/j.gaitpost.2011.07.011. [DOI] [PubMed] [Google Scholar]
- 47.Ross SE, Guskiewicz KM, Gross MT, Yu B. Assessment tools for identifying functional limitations associated with functional ankle instability. J Athl Train. 2008;43(1):44–50. doi: 10.4085/1062-6050-43.1.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ross S, Guskiewicz K, Gross M, Yu B. Balance measures for discriminating between functionally unstable and stable ankles. Med Sci Sports Exerc. 2009;41(2):399–407. doi: 10.1249/MSS.0b013e3181872d89. [DOI] [PubMed] [Google Scholar]
- 49.Ross SE, Linens SW, Wright CJ, Arnold BL. Customized noise-stimulation intensity for bipedal stability and unipedal balance deficits associated with functional ankle instability. J Athl Train. 2013;48(4):463–470. doi: 10.4085/1062-6050-48.3.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ross SE, Guskiewicz KM. Effect of coordination training with and without stochastic resonance stimulation on dynamic postural stability of subjects with functional ankle instability and subjects with stable ankles. Clin J Sport Med. 2006;16(4):323–328. doi: 10.1097/00042752-200607000-00007. [DOI] [PubMed] [Google Scholar]
- 51.Ross SE, Guskiewicz KM, Yu B. Single-leg jump-landing stabilization times in subjects with functionally unstable ankles. J Athl Train. 2005;40(4):298–304. [PMC free article] [PubMed] [Google Scholar]
- 52.Steib S, Hentschke C, Welsch G, Pfeifer K, Zech A. Effects of fatiguing treadmill running on sensorimotor control in athletes with and without functional ankle instability. Clin Biomech (Bristol, Avon) 2013;28(7):790–795. doi: 10.1016/j.clinbiomech.2013.07.009. [DOI] [PubMed] [Google Scholar]
- 53.Wikstrom EA. Fear of re-injury does not differ between those with and without chronic ankle instability. J Sports Sci Med. 2011;10(4):771–772. [PMC free article] [PubMed] [Google Scholar]
- 54.Wikstrom EA, Tillman MD, Chmielewski TL, Cauraugh JH, Naugle KE, Borsa PA. Self-assessed disability and functional performance in individuals with and without ankle instability: a case control study. J Orthop Sports Phys Ther. 2009;39(6):458–467. doi: 10.2519/jospt.2009.2989. [DOI] [PubMed] [Google Scholar]
- 55.Wright CJ, Arnold B. Fatigue's effect on eversion force sense in individuals with and without functional ankle instability. J Sport Rehabil. 2012;21(2):127–136. doi: 10.1123/jsr.21.2.127. [DOI] [PubMed] [Google Scholar]
- 56.Wright C, Arnold B, Ross SE, Ketchum J, Ericksen J, Pidcoe P. Clinical examination results in individuals with functional ankle instability and ankle-sprain copers. J Athl Train. 2013;48(5):581–589. doi: 10.4085/1062-6050-48.3.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Vela LI, Denegar CR. The Disablement in the Physically Active Scale: part II. The psychometric properties of an outcomes scale for musculoskeletal injuries. J Athl Train. 2010;45(6):630–641. doi: 10.4085/1062-6050-45.6.630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Huffman GR, Park J, Roser-Jones C, Sennett BJ, Yagnik G, Webner D. Normative SF-36 values in competing NCAA intercollegiate athletes differ from values in the general population. J Bone Joint Surg Am. 2008;90(3):471–476. doi: 10.2106/JBJS.G.00325. [DOI] [PubMed] [Google Scholar]
- 59.McAllister DR, Motamedi AR, Hame SL, Shapiro MS, Dorey FJ. Quality of life assessment in elite collegiate athletes. Am J Sports Med. 2001;29(6):806–810. doi: 10.1177/03635465010290062201. [DOI] [PubMed] [Google Scholar]
- 60.Institute of Medicine Committee on Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press;; 2001. pp. 2–4. [Google Scholar]
- 61.Michener LA, Leggin BG. A review of self-report scales for the assessment of functional limitation and disability of the shoulder. J Hand Ther. 2001;14(2):68–76. doi: 10.1016/s0894-1130(01)80036-3. [DOI] [PubMed] [Google Scholar]
- 62.Schmitt JS, Di Fabio RP. Reliable change and minimum important difference (MID) proportions facilitated group responsiveness comparisons using individual threshold criteria. J Clin Epidemiol. 2004;57(10):1008–1018. doi: 10.1016/j.jclinepi.2004.02.007. [DOI] [PubMed] [Google Scholar]
- 63.Hoch MC, Andreatta RD, Mullineaux DR, et al. Two-week joint mobilization intervention improves self-reported function, range of motion, and dynamic balance in those with chronic ankle instability. J Orthop Res. 2012;30(11):1798–1804. doi: 10.1002/jor.22150. [DOI] [PubMed] [Google Scholar]
- 64.Moher D, Liberati A, Tetzlaff J, Altman DG. The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA Statement. Ann Intern Med. 2009;151(4):264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]