Abstract
Context
In its best-practices recommendation, the Inter-Association Task Force for Preventing Sudden Death in Secondary School Athletics Programs urged all high schools to have a certified athletic trainer (AT) on staff. Despite the recommendation, many high schools lack the medical services of an AT.
Objective
To examine the barriers that athletic directors (ADs) face in hiring ATs in public high schools and in providing medical coverage for their student-athletes.
Design
Qualitative study.
Setting
Semistructured telephone interviews.
Patients or Other Participants
Twenty full-time public high school ADs (17 men, 3 women) from various geographical regions of the United States (6 North, 4 South, 4 Midwest, 6 West) participated. Data saturation guided the total number of participants.
Data Collection and Analysis
We completed telephone interviews guided by a semistructured questionnaire with all participants. Interviews were recorded and transcribed verbatim. Multiple-analyst triangulation and peer review were included as steps to establish data credibility. We analyzed the data using the principles of the general inductive approach.
Results
We identified 3 themes. Lack of power represented the inability of an AD to hire an AT, which was perceived to be a responsibility of the superintendent and school board. Budget concerns pertained to the funding allocated to specific resources within a school, which often did not include an AT. Nonbudget concerns represented rural locations without clinics or hospitals nearby; misconceptions about the role of an AT, which led to the belief that first-aid–trained coaches are appropriate medical providers; and community support from local clinics, hospitals, and volunteers.
Conclusions
Many ADs would prefer to employ ATs in their schools; however, they perceive that they are bound by the hiring and budgeting decisions of superintendents and school boards. Public school systems are experiencing the consequences of national budget cuts and often do not have the freedom to hire ATs when other school staff are being laid off.
Key Words: medical care, secondary school, staffing
Key Points
Budgeting concerns influenced the decisions of athletic directors about employing athletic trainers.
The athletic director is only 1 member of the administration who can influence the hiring of athletic trainers.
Misconceptions regarding the value and role of the athletic trainer in the secondary school setting were barriers to hiring.
Researchers have estimated that more than 7 million high school students currently participate in organized sports.1 Approximately 1.4 million sport-related injuries occur among high school athletes each year.2 American football alone has been projected to produce 12.04 injuries per 1000 exposures during competitions and 2.54 injuries per 1000 exposures during practices.3 Whereas most athletic injuries are relatively minor, potentially limb-threatening or life-threatening emergencies can occur. One medical emergency that can affect athletes is exertional heat stroke, which is consistently among the top 3 causes of death in sport.4 On October 12, 2010, Tyler Davenport died of exertional heat stroke that occurred during a football practice in August (Douglas J. Casa, oral communication, June 3, 2014). Although Davenport's coaches provided assistance at practice before transporting him to the hospital, their level of emergency medical training was limited to basic emergency care and focused on cardiopulmonary resuscitation (CPR) and automated external defibrillator (AED) training. Several deaths are reported each year, and they often result from a failure to recognize or implement appropriate care.5 Prompt and appropriate management of these injuries is critical to the patient's outcome and should be carried out by trained health care personnel, such as a certified athletic trainer (AT), to minimize the risk of further injury or death.6
The Inter-Association Task Force for Preventing Sudden Death in Secondary School Athletics Programs urged all high schools to have an AT on staff to take charge of emergency situations and provide care for student-athletes.7,8 The AT can evaluate and properly treat injuries, including sprains, strains, contusions, and abrasions, as well as more serious conditions, such as exertional heat stroke and hyponatremia. The AT can also facilitate and manage athletic health care at the high school, referring as needed and treating many patients in house. The presence of an AT can help reduce health care costs for the school and for the parents of student-athletes. In addition to heat illnesses, emergencies involving asthma, brain and cervical spine injuries, diabetes, sudden cardiac death, exertional illnesses, and environmental dangers have resulted in the deaths of athletes of all ages.4 In 1994, only 35% of high schools used the services of an AT, and in 1997, only 13 states reported employing ATs in greater than 50% of high schools.9 By 2009, the national average of schools employing ATs had risen to only 42%.10 Whereas the prevalence of ATs in high schools is improving, some high schools still lack the appropriate medical personnel to institute guidelines for preventing sudden death in youth athletics.11 In these settings, the responsibility to save young athletes may fall to coaches, athletic directors (ADs), or bystanders who are not trained in discerning similar signs and symptoms of potentially fatal circumstances.7 Specific and prompt care is critical for a patient to have the best chance of a positive outcome. In some situations, waiting until emergency medical services arrive to provide care can result in catastrophic injury or death, as demonstrated in Davenport's case. Having onsite medical coverage provided by an AT can in many cases reduce the number of deaths that occur in high school athletes; yet in some cases, an AT is not available to provide such care.
The importance of having an AT onsite has been well documented by various outlets but most prominently in the best-practices recommendation of the Inter-Association Task Force for Preventing Sudden Death in Secondary School Athletics Programs.7,8 However, many high schools do not meet this recommendation. The Collaboration for Athletic Training Coverage in High Schools–An Ongoing National Study (CATCH-ON) provided preliminary data on the prevalence of ATs in public high schools across the United States; this study was designed to gain a better understanding of the medical coverage provided by US high schools.11 After attempting to contact every public high school in the United States, the researchers observed that 70% of public high schools, which account for 86% of all student-athletes at this level, have some access to an AT. As part of the CATCH-ON project, initial data emerged about reasons for not having an AT.11 Those barriers included budgetary concerns and the belief that an AT was not needed, mostly due to the CPR, AED, and first-aid training of coaches.11 Therefore, the purpose of our study was to focus on the barriers that ADs face in providing medical coverage for their student-athletes and hiring ATs for public high schools. By examining these barriers more thoroughly, we hoped to find ways to help ADs initiate positive change by seeking AT coverage.
METHODS
To facilitate organizational changes within secondary school athletics, the current environment and its potential resistance to change must first be assessed. In this study, we used data from the CATCH-ON project to gain a more holistic and in-depth explanation for the lack of AT coverage at the secondary school level. In this case, we chose qualitative methods, as they afford the flexibility to examine a phenomenon without much data and to expand on the themes found in the CATCH-ON project.11 The CATCH-ON project was a research project initiated by the Korey Stringer Institute at the University of Connecticut in conjunction with the National Athletic Trainers' Association (NATA) aimed at identifying the level of athletic training services in the public secondary school setting.11 The study quantified the services provided but did not fully capture the reasons for not having or providing medical services by an AT. Telephone interviews, therefore, would enable us to gain a better understanding of the barriers to and reasons for public schools not hiring ATs. The researchers conducting the CATCH-ON project obtained data from 4688 public high schools about their medical coverage and observed that 70% provided some degree of services through an AT.11
Participants
Schools that participated in the CATCH-ON project11 and reported not employing an AT (N = 1504) served as the initial recruitment pool for our study. We wanted to recruit ADs from schools that indicated in the CATCH-ON project that they did not provide medical services using an AT. From this pool, we randomly selected public high schools using numeric coding and a random-number–generating Web site (https://www.random.org) to begin our recruitment process. For the purposes of our study, the United States was divided into 4 regions: North (n = 100 schools), South (n = 218 schools), Midwest (n = 617 schools), and West (n = 568 schools; Table). We then randomly selected schools by region (n = 20). Each randomly selected school received an initial telephone call from 1 of the authors; if the AD was not available, a second telephone call was made later. Two e-mails were sent to schedule specific interview appointments if the AD could not be reached with 2 calls. When ADs could not be reached or refused to participate, additional schools were selected randomly. We used data saturation as our recruitment-sampling procedure, which was reached with a total of 20 ADs. The University of Connecticut-Storrs Institutional Review Board granted an exempt status because we were not collecting personal information.
Table.
Regional Division of Participants
| Region |
State |
No. of Participants |
| North | Connecticut | 1 |
| Maryland | 1 | |
| New Hampshire | 1 | |
| Rhode Island | 2 | |
| Vermont | 1 | |
| South | North Carolina | 2 |
| South Carolina | 1 | |
| West Virginia | 1 | |
| Midwest | Indiana | 3 |
| Iowa | 1 | |
| West | Arizona | 1 |
| Colorado | 1 | |
| Idaho | 2 | |
| Utah | 1 | |
| Washington | 1 |
Instrumentation
We developed a semistructured interview guide based on the current research11 and topics in the field of athletic training, including availability of medical care for high school athletes, emergency preparedness, and the initial CATCH-ON project results.11 Before data collection was initiated, 3 ATs (not authors) reviewed the interview guide for content and clarity. Two of the ATs were researchers with experience in qualitative research methodology, and 1 AT had athletic training experience within the high school setting. All 3 were knowledgeable about risk management in athletics and sudden death in sports. We made minor changes for verbiage and clarity after evaluating their feedback. The final guide included qualitative discussion questions and specific probes regarding the ADs' views on ATs, medical care provided for student-athletes, and the risk of catastrophic injury or death for student-athletes.
Data Collection
Data collection was conducted by telephone, with each call lasting approximately 20 minutes. Telephone interviewing allowed the participants to speak freely on the topics that the researcher asked, promoted discourse between the researcher and the participant to gain further insights, and permitted follow-up questioning when necessary.12 For consistency, 1 researcher (S.R.R.) conducted all interviews. Before data collection, an experienced qualitative researcher (S.M.M.) trained and mentored her. S.R.R. called participants and made additional calls based on the convenience and availability of participants. Conversation was based on the semistructured interview guide, but the researcher could modify the line of questioning based on the participant's responses. The researcher took field notes while conducting the interview sessions. All interviews were recorded digitally and transcribed verbatim by an outside transcription company to avoid researcher bias.
Data Analysis
We selected a general inductive approach to analysis as described by Thomas,13 which included constant comparisons of all transcripts and qualitative content analysis. The initial reading of the transcripts allowed us to gain a general understanding of the data. Secondary reading of the transcripts was intended to initiate the formulation of inductive coding. Predominant themes were identified and coded with a term to represent the meaning. These codes were compared and sorted into categories, which were organized into themes, based on the research questions. Throughout the reading process, the codes, categories, and themes were compared and evaluated based on the data and in relation to the current literature on medical coverage in athletics.
Data Credibility
Credibility of the procedures and trustworthiness of the data analysis were established using data-source triangulation, peer review, and intercoder reliability.14 Sampling participants nationally enhanced the credibility of the data by providing multiple regional perspectives, which we compared to find more generally applicable themes. An athletic training researcher (K.D.P.), who was not directly involved in the data-collection process but had experience in qualitative methodology and analysis, ensured the credibility and trustworthiness of the data. We provided the peer reviewer with the final analysis of the data and the transcripts to confirm the findings. Our peer review yielded agreement. To complete the multiple-analyst triangulation, 2 researchers (S.M.M., S.R.R.) independently analyzed the data as described by Thomas.13 After this analysis, the researchers met and reached agreement on the themes through discussion. The general meaning of the themes was similar, and the discussions between the 2 researchers centered on terminology and wording of the results.
RESULTS
Our participants included 6 ADs from the North, 4 from the South, 4 from the Midwest, and 6 from the West (Table). Nine ADs reported that their schools had employed an AT in the past but no longer did. Thirteen ADs stated that they had worked with an AT during their careers as either ADs or as coaches. Ten ADs reported attempts to address the possibility of hiring an AT and sending proposals to their school boards. Budget was directly stated as a limiting factor by 18 ADs. Between the initial CATCH-ON project and the telephone interviews we conducted, 3 schools (2 in the North, 1 in the South) had been approved to hire an AT.
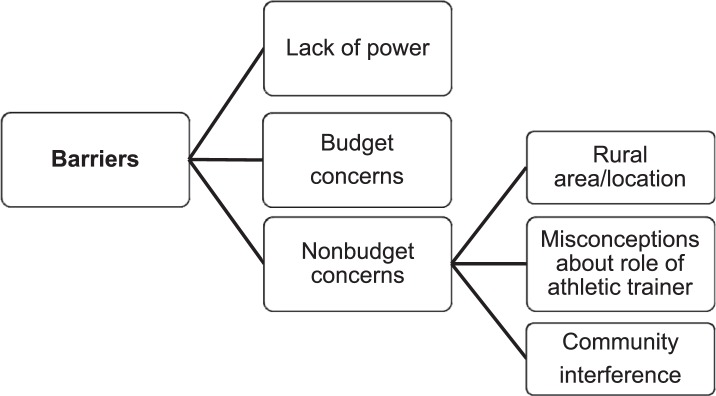
Three major themes emerged from the data: lack of power, budget concerns, and nonbudget concerns (Figure). We discuss each theme with supporting quotes from the participants.
Figure.
Barriers to hiring an athletic trainer in the high school setting.
Lack of Power
The data demonstrated that public school ADs perceived that they lacked the power to make hiring and budgetary decisions. Sixteen participants spoke candidly about the limited role they had in hiring and creating positions within their school districts. An AD from the North stated:
I definitely think the school board needs to think about, you know, ATs as almost another position in the school. You know, as we have our teachers, we have our nurses. . . there should be an athletic training position.
When discussing the possibility of hiring an AT and whether it was worth his efforts with his school board, an AD from the Midwest said: “You know, I see it as a need, at least a part-time person that is here, you know, set hours every day, but I'm not ready to fight that battle yet.” When asked if any way existed to persuade their school departments to hire ATs, an AD from the South commented: “Zero chance. I mean, there's no way we could hire an athletic trainer and get rid of teachers at the same time. And that's what our district's kind of in the mode of right now.” Another AD from the Midwest explained: “Honestly, no. I don't think that that's something that, quite honestly, my superintendent or my school board would entertain.” In response to the question about reasons they do not have ATs, an AD from the West noted:
I believe that they [my school board] already understand the value of it [employing an AT]. But to persuade them to shift the monies from another area to that won't happen. It's been attempted on several occasions. It's placed in our budget every single year, and it's cut every single year.
The same AD continued discussing his struggles with hiring an AT:
I have presented on probably 3 or 4 different occasions, but in the end, when they [the school board] get to the last week before the town financial meeting and the town vote, it is one that goes—especially as they get closer and closer to the end, when the pressures get greater and greater for the approval or nonapproval of the school budget.
These statements by the AD from the West showcase the concept of lack of power in decision making and the relationship it may have with budgets, allocation of funds, and final approval of spending. Athletic directors in our study illustrated that a lack of support from supervisors in the school hierarchy could be present, and they did not believe they could overcome it.
Budget Concerns
The funds allocated to specific departments or projects within a school can be a leading factor in the services and programs that a school can provide for its student-athletes. All but 1 AD directly attributed not employing an AT to a lack of funding. Eighteen of the 20 participants discussed budgetary concerns as the major barrier to providing AT services at their high schools. An AD from the South who had an AT employed in the school until recently described the reason for the change:
It was financial, period, financial. Everything that evolves at this school relates to money, nothing more than that. They understand the value of everything that's there for us, but the question is the ability to pay. Therefore, they prioritize, and they felt as though that was one that wasn't important, which is untrue, but they didn't feel as though they could afford it, so they cut it.
Another AD from the South shared his struggle with budget approval:
We have already been told that, if the budget gets voted down this year, then we have to revert back to the last budget, which means we would have to cut probably $44 000 from our athletic program, as part of overall cuts for everything. It is really just a budgetary issue. I would love to have an athletic trainer, but unfortunately, we just. . . for me to put in a. . . that into our budget. . . we're probably. . . that is just not going to happen.
An AD from the West reported:
One is cost. Two, we're a B school. We have just a little over—well, our K through 12 school district is only 700 kids, but our high school is only about 220 kids in the high school, and the school just runs a sports program under what's called the bare minimum amount of money that we can come up with and stuff. There has just never been the ability to afford to have somebody on staff as a sports trainer.
Reflecting on the effects of widespread funding deficits in public education, an AD from the Midwest observed:
I know it's important. I've reflected that to our school board, but once again, we're in a time right now where schools just don't have any money. I don't know what it's like in Connecticut, but in Indiana schools. . . I mean, we're laying off teachers; so if you're laying off teachers, it's hard to hire an athletic trainer even though one lawsuit will cover the cost of an athletic trainer, but it's hard for a school board to justify that when they're laying off teachers.
Limited resources and budgetary concerns were the primary factors prohibiting hiring ATs in secondary schools, as these statements illustrated.
Nonbudget Concerns
Several challenges beyond lack of power and budget were represented in the data. Nonbudget concerns comprised 3 categories: rural area/location, misconception about the role of an AT, and community interference. In 14 interviews, participants also discussed these secondary factors as contributing to the themes of lack of power and budget concerns.
Rural Area/Location
Professional resources in rural areas can be substantially limited, as 7 participants discussed. One AD from the South commented that his school cannot employ an AT because its location is problematic: “We are 26 miles from the nearest traffic signal.” Many rural ADs reported relying heavily on services of the local emergency medical system (EMS) in lieu of ATs. The ADs believed that little incentive existed for an AT to accept positions in their schools for various reasons but mostly due to the location of the school. For example, 1 AD explained this restriction of location:
You know, we've never had an athletic trainer. We've had like physician's assistants that have helped us out and things like that, but I mean, we're pretty rural out here, and we don't have athletic trainers. . . We do have 1 small school that's, oh, about 110 miles away, and they have a volunteer athletic trainer. It's just that I don't know how we'd get someone to come out here.
Another AD relied on traveling physicians from major cities in the absence of ATs, sharing
Yeah, we are a very small community of about 3500 in our community, so we do have a hospital but the majority of the doctors do come from out of town in the Tucson and Phoenix area. They travel every weekend, so 2 to 4 hours away they travel.
Rural schools present constraints for hiring an AT due to limitations related to location and resources.
Misconceptions About the Role of an AT
Whereas most of the ADs in our study understood the role of an AT in the high school setting, it was apparent that others believed the secondary school coach had sufficient knowledge and training to address the medical needs of student-athletes without an AT. All 20 participants stated that their coaches received training in first aid, CPR, and concussion recognition and were expected to use this training in practices and games. One AD from the West who was confident in the abilities of the high school coaches noted:
We send all of our coaches to get the required training that the [state high school association] and the National Federation of High Schools require [for coaches]. Yeah, they go through concussion training. They also go through first aid, which is first aid, CPR, AED, and stuff. They also go to coaches' camps to learn how to tape, fix sprains, and stuff like that too, but the biggest one we do every year annually is the concussion training.
This admission by the AD demonstrated misconceptions about the training that ATs receive and a failure to recognize certification and licensure regulations.
High school interscholastic leagues often only mandate medical personnel for football games; therefore, high schools that do not employ ATs must rely on their coaching staff, in addition to the local EMS, to act in emergency situations. Seventeen ADs reported that they had football teams and did not employ ATs. In reference to emergency preparedness and the training of coaches, 1 AD from the North stated:
If anything, common sense I hope would prevail, if that makes sense. Well, I mean, they have to be first-aid–CPR certified. The State Association does require the NFHS [National Federation of High Schools] concussion course every 2 years.
An AD from the West said that a coach could provide basic care if necessary and, for emergency situations, the local fire department and emergency medical system would provide it:
Well, at football games, we have EMT [emergency medical technician], you know, ambulance on standby. They're at the field. They're there in case something serious or even minor happens. You know, during basketball games. . . I mean, all of our coaches are CPR certified, first-aid certified, so I mean, minor injuries, you know, we handle onsite ourselves.
Several of the ADs believed that, given CPR and first-aid training, their coaching staffs provided an adequate substitution for an AT and, thus, did not believe they needed to advocate for hiring one at their respective schools. The misconception of the role of the AT extended into the belief that other health care providers, such as EMTs or physical therapists, could be appropriate substitutes for ATs. An AD from the West commented:
We have EMTs onsite, you know, for games, but not for practices. We have a local guy [EMT] that will donate his services for us. A physical therapist will also help us out in some of those other situations.
The use of community resources appeared to facilitate misconceptions that their availability reduced the need to have an AT onsite regularly. Another AD from the West demonstrated the continued misconception of the AT's role compared with that of other health care providers. While discussing medical coverage at the high school, the AD reported:
Well, the hospital obviously has a person. . . I don't know if it's like a pure athletic trainer. It's probably more of a physical therapist type of position, and the hospital does bring one over to us from time to time. Usually like on Mondays, they'll try to stop in, but it's not. . . it hasn't been super consistent, if that makes sense.
Athletic directors at high schools without ATs appeared to believe that coaches who are trained in CPR, AED, and first aid, along with local emergency response personnel, can provide sufficient medical care to their student-athletes. The misconceptions related to the role of the AT were manifested in their beliefs related to those who serve the local community and the confidence in coaches to care for their student-athletes.
Community Interference
This category encompassed local school resources and, in some cases, medical coverage that can be provided free of charge. Interference was based on the notion that other medical care providers who were community members or local to the high school were sufficient to provide onsite coverage for games. Ten participants without ATs mentioned volunteer medical coverage from local EMS or other providers as filling the void of athletic training services. An AD from the West explained the absence of an AT:
In this school district here in [my city], there are 5 people who work for the district as teachers and principals and myself as an AD who are all EMTs. We are at every sporting event that takes place, where there is soccer, baseball, softball, basketball, and volleyball, whatever. We always have at least 1 to 2 EMTs on scene with a kit.
This statement illustrated the ADs' assumptions that medical coverage of games is most important, and local emergency response provides adequate coverage instead of having an AT onsite. The AD also suggested, among the misconceptions about the role of an AT category, that an administrator can replace the AT in providing medical coverage. An AD from the South offered a similar scenario in which community members could supply the care in place of an AT:
Volunteers [are a way to get coverage], but like I said, we [myself and my wife] are both certified EMTs. The fire hall is right across the street [from our school], so we also have a program where we allow 2 members of our fire hall in free to all our athletic games with the understanding that, if we need an ambulance, they are going to get it.
Community interference was a barrier to hiring an AT because ADs who relied on it believed it was a way to provide appropriate coverage in lieu of an AT, or minimally, it was a sufficient means of medical coverage. Our data suggested that ADs believed local community members could fill in for the lack of the AT services at the high school level and showcased the misconception of the AT's value and the need for continued care rather than onsite medical coverage only. Furthermore, the data indicated that ADs viewed medical coverage from EMTs as free and, thus, an easier, more practical option to provide medical care at the secondary school level.
In contrast, community support also can be a catalyst for positive change. Three participants reported approval for hiring an AT after participation in the CATCH-ON project. The driving force behind this approval was commonly found to be support from local hospitals and clinics, as well as from parents. For example, a school in the North received a grant from a local hospital to pay an AT for 5 sports seasons. The intent of the grant was to facilitate the continuation of AT services by the school board after the funding ended; ultimately, witnessing the importance of the AT would encourage the school board to allocate funding in the future. At the time the interview was conducted, the AT was fulfilling his second sports season (spring). An AD from the Midwest had a similar experience with the resources of a local hospital:
I was told that the AT was an employee of the hospital. The AT was paid through a grant or something, and the hospital paid their salary. The AT came to the high school to cover many of our games. Then, of course, any injuries or whatever would be rehabbed [rehabilitated] through the hospital. That's how the hospital recouped their money, according to what I was told.
Two other ADs described the concept of community support from local hospitals providing access to an AT without a direct cost to the high school itself. An AD from the North discussed his experiences with community support despite not being on the receiving end:
We have a lot of our parents ask, you know, “There are some other schools in our area that are smaller than us, but they have athletic trainers, why don't we?” Well, it's because they have a county hospital that provides that service for them, and ours doesn't. A lot of them think it's because we are too cheap to pay for one, but that's not the case.
Community resources not only inhibited the hiring of an AT but also facilitated it. Parents and other local community members either served as care providers or sought resources to provide an AT for their student-athletes.
DISCUSSION
The purpose of our study was to examine the barriers that ADs face when hiring ATs in public high schools. The NATA has recommended employing ATs in high schools, yet many high schools do not follow this recommendation. Limited data exist, however, on the barriers to hiring or reasons why many high schools, unlike colleges, do not hire ATs. The barriers that emerged from our study included lack of power, budget concerns, and nonbudget concerns. These findings were triangulated back to the initial CATCH-ON results, in which ADs briefly mentioned barriers to employing ATs.11 Our observations supported anecdotal reports that budgetary concerns often prevent high schools from hiring ATs. Our data also illustrated that the barriers to hiring an AT can be multifaceted and can include reliance on other health care providers, misconceptions about the role of the AT in health care, and school location and resources.
Lack of Power
The responsibilities of a high school AD frequently include but are not limited to hiring coaches, ensuring that coaches and athletes adhere to athletic department bylaws, scheduling competitions, scheduling transportation and officials for competition, purchasing equipment and uniforms, overseeing athletic facilities, and monitoring athlete academic eligibility.15 However, based on our results, it seems that high school ADs believe they have little control over the health care provided to their student-athletes, as many recognized the need for the services of an AT but were limited by having no control over decision making and budget planning. These responsibilities are seemingly juxtaposed with those of collegiate ADs, who have both fiscal and operational control over their departments.16
All high schools must adhere to the standard of care that their state athletic associations set forth; however, Hawaii is the only state that specifically requires the employment of ATs.17 The CATCH-ON project showed that, although 64% of public high schools employed ATs, only 38% employed full-time ATs.11 Many of our ADs responded that their states require an unspecified health care provider to be onsite only for football competitions, which was fulfilled by having EMTs or volunteer physicians on the sidelines. Our data indicated that, although this may be viewed as adequate, not all ADs agreed this was sufficient medical coverage. However, they were still limited by the organizational infrastructure within the public school sector.
Lack of power led directly to high school ADs being unable to initiate organizational changes for approving the hiring of an AT through an increase in or allocation of budget resources. Not addressing necessary change, such as providing the medical services of an AT, can be dangerous in the high school setting because it puts the wellbeing of the student-athlete at risk, which increases the risk for liability.18 One example is a pending lawsuit in Georgia. The parents of Donteria J. Searcy are suing various entities of Ben Hill County for the death of their son during football training camp in the summer of 2011. The school did not employ an AT, and the parents are asserting that the coaches did not provide appropriate care.19 Regulatory agencies, including state advisory boards, professional organizations, or interest groups, typically dictate appropriate and necessary methods of organization and act as catalysts for institutional change.20 By acting on collectively valued standards and changing their structures to conform to the expectations of an institutional environment, organizations increase the legitimacy of their programs and ensure necessary resource flow.21,22 As public awareness about health and safety in athletics increases, schools must adapt to meet new expectations.
When asked why their schools did not employ ATs, many ADs cited that their school boards did not believe an AT was a necessity despite the ADs' opposing views on that need. Our ADs struggled to find the means to facilitate hiring of an AT when the school board members did not see value in adding those services to the budget. Organizations including the American Medical Association, the American Academy of Pediatrics, and the NATA have recommended hiring ATs in high schools for decades.9,23 The recommendation seemed largely anecdotal until 2010. Wham24 used the Appropriate Care Index based on the “Appropriate Medical Care for Secondary School-Aged Athletes” consensus statement to quantitatively correlate higher levels of medical care with the employment of ATs.23,24 High schools that directly contracted with ATs had higher levels of care based on Appropriate Care Index scores than schools that contracted with ATs through outside sources (ie, clinics, hospitals).24 This observation was attributed to differences in hours of availability to student-athletes; those hired directly by the high school were not restricted to hours spent working for the contracting agency.24,25 These results showed a clear value in employing an AT in a high school. However, administrators (school boards and superintendents) with the power to hire staff need to become more aware of this benefit. Whereas ADs are not in the direct position to hire ATs, they must continue to advocate for the health and safety of their student-athletes, as many demonstrated in our study. Presenting the need for ATs in high schools at school board meetings and to other city councils may be a necessary step in educating higher-level administrators, which is a possible means to overcome the ADs' barrier of lack of power. Efforts by ATs and the NATA to educate superintendents and school boards on the importance of ATs also may help to overcome this barrier. For example, the “Appropriate Medical Care for the Secondary School-Aged Athletes” statement could provide the support needed to employ ATs.23 The statement was developed by a collaboration of several sports medicine associations and the NATA and can provide the necessary information for those decision makers to approve the hiring of ATs.
Budget Concerns
Budget, as often suspected, was the major barrier to hiring ATs in high schools. National recession and shifts in governing philosophy have led to major changes in public school funding and cutbacks in states' general funds over the past several years.26 The general fund is based on state tax revenue and pays for the bulk of educational operations, which includes the salaries and benefits of teachers and support staff, teaching supplies, and most student programming. Between 2008 and 2011, the states and the District of Columbia were forced to make major cuts ($115.6 million to $700 million annually) to public education based on declining tax revenue.27 Jarman and Boyland26 estimated that, due to reductions in the general fund, approximately 2608 teachers and 1357 instructional assistants were cut from Indiana's public schools in the 2009–2010 academic year. The economic climate and its effect on school budgets concerned our participants, especially when they discussed attempts to include AT services in their budgets each year. In fact, when we asked our participants if they had addressed the importance of hiring an AT with their school boards, most believed that creating an AT position would not be considered when more teachers are being laid off each year.
It is interesting that even in the current economic crisis, the number of schools using AT services has continued to rise. Clearly, ways exist to overcome this challenge, and budgets are potentially perceived as a larger barrier than they truly might be. The prevalence of part-time ATs whom larger medical facilities have provided to high schools seems to be the simplest adaptation to the budget. Several ADs expressed concern over the financial and legal liability that could be associated with a major injury to a student-athlete. However, it seems that the hypothetical worst-case scenario holds very little weight against the difficult and sometimes controversial cuts that certain schools already must make.
It is evident that public education departments nationally are trying to preserve academic programs by eliminating extracurricular activities and services. Even if an AD presents a case for hiring an AT, the school board frequently votes against it due to the current state of public education funding. Identifying budget as a major qualitative theme or barrier to hiring an AT combined with the data of Wham24 in 2010 may provide enough support for administrators and state legislators to justify the allocation of funds to employing ATs in high schools. Athletic directors need to continue to advocate for hiring ATs despite budgetary constraints and continue to educate parents, school boards, and superintendents about the effects that an AT can have on the student-athlete's wellbeing and medical care. The NATA can aid in the process by developing educational programs geared toward superintendents and school board members. Concussion researchers have begun to investigate the effect of educational interventions for promoting awareness and compliance with concussion protocols. Similar research could be conducted to evaluate the influence of education on promoting AT services in the secondary and high school settings.
Nonbudget Concerns
Rural Area/Location
Seven participants mentioned rural location and small school size as limitations to hiring ATs. Whereas rural populations are considered a minority in the United States, Brown and Swanson28 estimated that more than 56 million people reside in rural communities. Rural education researchers commonly recognized rural schools as being located in small communities (population < 2500) and being relatively isolated geographic areas (at least 2 hours from a major metropolitan area or 1 hour from a 4-year college or university). The residents of these communities typically have average family incomes of less than $23 000 per year, a prevalence of low-end jobs (agricultural or low-skill industrial), and low median level of education (most without formal postsecondary education). Various levels of diversity also exist within the population. Some include large percentages of ethnic minorities, and others do not.29 High school ATs are sometimes contracted through private clinics or hospitals, and the distance from such facilities represents a large limiting factor for certain schools. This also correlates with budgeting concerns. If a school does not have the funding to directly contract with an AT, the only option may be community outreach from larger medical institutions. Rural ADs stated that they believed they could provide little incentive for ATs to come to their towns. One roadblock may be the need for a team physician to oversee the AT and the difficulty gaining consistent access to a rural school. That is, if the physician is employed or has a practice that is not close to the school, frequent onsite visits may be a challenge. Whereas the physician may agree to and develop standing orders with the AT, he or she may not be comfortable assuming the role of the team physician due to time conflicts or inability to attend games.
To help combat some of the problems of medically underserved areas, Ohio University supplies graduate-assistant ATs to rural Appalachian high schools.30 The graduate assistants provide community service in managing the health care of student-athletes while raising public awareness about the profession of athletic training and advancing their own professional development. This program offers a great resource to schools that may not have the funding to support a full-time AT, supplies more consistent medical coverage, and as mentioned, assists in overcoming the budget barrier. We encourage more universities to develop similar programs to place ATs in rural schools. Programs could also be established through hospitals and clinics. Although ATs practice in isolation in these rural locations, they are enrolled in a postprofessional or graduate degree program and, thus, continue to have interactions with peers and faculty members who support and mentor them early in their careers. Another suggestion is for rural secondary schools to recruit newly credentialed ATs as they would recruit new teachers. The schools would capitalize by giving them an opportunity to gain real-world experience in their trade while providing a supportive environment. Newly credentialed ATs are often excited about their careers and bring passion and enthusiasm for their new roles, and therefore, could be a strong fit for the positions.
Interestingly, participants in the North did not discuss concerns pertaining to location and proximity of resources. This is likely due to regional population-density distributions. Northern school ADs were more likely to describe urban school issues, including transient populations, low-income families, and high percentages of students enrolled in free or reduced-price lunch programs. This result showed similarities with the socioeconomic status described in rural schools and suggests that university or hospital outreach may also be a viable option for providing ATs in urban schools.
Misconceptions About the Role of an AT
As participants noted, schools frequently use EMS for supplemental coverage in the absence of an AT. This supplemental care, which meets minimum state athletic association standards, offers a sense of security in medical care but may not be adequate to fit the needs of student-athletes. Emergency medical technicians are trained in providing basic medical care and transportation for patients with critical and emergency conditions and intervening with the equipment found on an ambulance.31 They are not specifically trained to evaluate athletic injuries, and the decision to return an athlete to participation is out of the EMT's scope of practice. Researchers32 have shown a disconnect with evidence-based practice in the treatment of conditions such as exertional heat stroke and the protocols of EMTs due to limitations in both education and scope of practice. In a national survey, Decoster et al33 reported that 42% of ATs have had on-field disputes with EMTs over the treatment of an injured football athlete. Specifically, these disputes have centered on spine-boarding procedures and equipment removal.33
Participants also stated that, in the absence of ATs, their coaching staffs were responsible for athlete health care during practices and competitions for all sports except football. Many believed that the training their coaches received in first aid and concussion recognition was adequate because it met state standards. However, considering basic first-aid training comparable with the skills of an AT shows substantial misconceptions about the scope of practice of ATs. Moreover, and possibly more disconcerting, is the belief that a coach can be trained through a weekend course to manage the medical care of student-athletes. In contrast, the AT receives a minimum of 2 years of postsecondary education.
No ADs addressed concern about conflicts of interest during competitive events. Ransone and Dunn-Bennett34 observed that 64% of athletic coaches surveyed could not adequately complete the American Red Cross first-aid assessment. They also reported that, when losing a close game, 63% of coaches would return an injured starter to the game.34 Whereas education standards for coaching have changed in recent years, especially for concussion management, an unbiased, objective professional must provide medical care to student-athletes.
Community Interference
This category can be both a barrier and a solution. Although it can be a driving force behind positive change, lack of community support can be a barrier to the employment of an AT. As we know, many ATs are outsourced to public high schools through hospitals or private clinics and are frequently expected to generate referrals. One Midwest AD reported that the local hospital discontinued the school AT's contract due to a lack of referrals. As mentioned earlier, rural schools without close proximity to hospitals and clinics have difficulty benefiting from such community outreach. Another Midwest AD expressed frustration because the school is located on the town lines of 3 cities but is a lengthy distance from the heart of each city. The AD stated that none of the major city's medical institutions were willing to outsource an AT over that distance, but they provided AT services to most of the schools in closer proximity.
Three participants were able to approve the hiring of an AT since the initial CATCH-ON project.11 We included them in the data set to examine how some schools have been able to overcome the barriers that we identified, including budget. Two schools were located in the North, and 1 was located in the South. The Southern school had a history of providing a volunteer AT at high-risk competitions; however, it was able to directly hire an AT for both practice and game coverage only after a local hospital presented an unsolicited contract. A Northern school was able to fund the hiring directly through the school board. The school previously had a full-time AT, but the position was revised to cover only football due to budget concerns in 2010. In the 2013–2014 academic year, the position was reestablished as full time. The school is in 1 of the states with the highest percentage of ATs in public schools based on the CATCH-ON data.11 The high saturation level of ATs in the state and community awareness of the role and value of an AT in other local schools may have assisted in the approval.
One Northern school secured a grant from a local health service for 5 sport seasons, which translated into approximately 1.5 academic years. The AD expressed hope that first-hand exposure to an AT for student-athletes, parents, and administrators would encourage the school board to hire the AT full time at the end of the grant period. This grant program is of note because it is similar to the pilot athletic training program established in Hawaii in 1993. After an extensive lobbying and media campaign, the state of Hawaii allocated $1.2 million to a 2-year program, placing ATs in its 38 public secondary schools. To convince the state legislature that funding to hire ATs was a primary health and safety concern in the state, a community-based educational platform aimed at parents, coaches, ADs, and school administrators was established. A 2-fold needs-assessment study that consisted of a survey on the current practices of sports health care and a year-long injury-surveillance survey within the 38 public secondary schools was also implemented to support the effort.35 The study provided empirical data for the need to hire ATs for the public secondary schools, and the state of Hawaii is still the only state requiring that ATs be employed in public schools.
Limitations and Directions for Future Research
Our study had several limitations, including sample size, high school type, and perspective. We reached data saturation with the 20 interviews conducted; however, this represents a small sample of public high schools without ATs. Our data mirrored the initial findings of the CATCH-ON project; however, we recognize that this is a very small sample and, whereas relatively equal regional distribution was achieved, participants were from only 15 states. All themes may not be universally applicable based on variations in state athletic association regulations. In addition, we studied only public schools; therefore, our findings may not be applicable to private high schools. Future authors may choose to complete similar studies on a larger scale, possibly using online data-collection procedures to gain more information about barriers to hiring an AT. Additional data are necessary to determine whether similar factors exist for those ADs. Future researchers could also focus on schools that employ ATs to identify the resources and strategies used to hire and retain their ATs.
Our results indicated that the AD in the public high school sector has little control over budgetary concerns and hiring of ATs; therefore, to address this concern, members of the school board must be interviewed to gain a more robust understanding. Examining the understanding of superintendents and school board administrators about the role of ATs, emergency planning, and athletic health care recommendations will provide this information and further clarify the concept of lack of power that ADs described. These efforts may lead to the development of informational programs targeted at administrators at the appropriate level of organizational power within school districts to initiate change.
CONCLUSIONS
Whereas many ADs would prefer to employ ATs at their schools, they are not in a position of power to approve such hires. They are bound by the decisions of their school boards and district administrators, which are largely driven by the available budgets. A major barrier to hiring ATs was public school budget cuts. Several participants noted that their districts are coping with teacher layoffs, and their school boards would not consider the addition of an AT position. Location presents unique challenges to hiring an AT. This challenge can be attributed to financial concerns and to lack of resources (ie, clinics, hospitals) within an appropriate geographic vicinity to schools in rural areas. Misconceptions about the role of the AT, particularly in relation to having other medical care providers (eg, EMTs, physical therapists) supply the medical coverage, interfered with hiring ATs in public schools. Athletic directors also appeared to be satisfied with having coaches with basic emergency care training evaluate and manage injuries and potential medical emergencies.
Although continuing research is needed, we hope that identifying these barriers will lead to the development of strategies to overcome them. To combat misconceptions about the role of ATs, state legislatures could pass more structured guidelines for athletic health care that follow the recommendations of the NATA23 and other organizations9 about appropriate medical coverage at secondary schools. Using the state of Hawaii as a model, other states can make changes to help provide AT services in high schools. One change can focus on removing the misconception that basic CPR, AED, first-aid, and concussion training for coaches is an acceptable substitution for AT services. Creativity in budgeting, such as sponsoring pilot programs similar to those illustrated in the community interference theme, may also help bring ATs into schools. Community outreach programs from clinics, hospitals, and universities may be a way for public schools to acquire AT services, especially in rural or low-budget settings. However, these institutions must be both willing to supply professionals and located within an appropriate distance of the schools. We hope that our findings can serve as a catalyst for change to someday enable all high school student-athletes to have access to ATs.
REFERENCES
- 1.Wier L, Miller A, Steiner C. HCUP. Statistical Brief #75: sports injuries in children requiring hospital emergency care, 2006. Agency for Healthcare Research and Quality Web site. 2015 http://www.hcup-us.ahrq.gov/reports/statbriefs/sb75.pdf. Accessed June 10. [PubMed] [Google Scholar]
- 2.Rechel JA, Yard EE, Comstock D. An epidemiologic comparison of high school sports injuries sustained in practice and competition. J Athl Train. 2008;43(2):197–204. doi: 10.4085/1062-6050-43.2.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shankar PR, Fields SK, Collins CL, Dick RW, Comstock RD. Epidemiology of high school and collegiate football injuries in the United States, 2005–2006. Am J Sports Med. 2007;35(8):1295–1303. doi: 10.1177/0363546507299745. [DOI] [PubMed] [Google Scholar]
- 4.Mueller FO, Casa DJ. Fatal and catastrophic injuries in athletics: epidemiologic data and challenging circumstances. In: Casa DJ, editor. Preventing Sudden Death in Sports and Physical Activity. Sudbury, MA: Jones and Bartlett Learning;; 2012. pp. 1–14. In. ed. [Google Scholar]
- 5.Pagnotta KD, Casa DJ, Cates J, Mazerolle SM. Arkansas' creation and implementation of health and safety legislation utilizing Ambrose's requirements for change. Curr Sports Med Rep. 2013;12(5):285–289. doi: 10.1249/JSR.0b013e3182a4b858. [DOI] [PubMed] [Google Scholar]
- 6.Andersen JC, Courson RW, Kleiner DM, McLoda TA. National Athletic Trainers' Association position statement: emergency planning in athletics. J Athl Train. 2002;37(1):99–104. [PMC free article] [PubMed] [Google Scholar]
- 7.Casa DJ, Guskiewicz KM, Anderson SA, et al. National Athletic Trainers' Association position statement: preventing sudden death in sports. J Athl Train. 2012;47(1):96–118. doi: 10.4085/1062-6050-47.1.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Casa DJ, Almquist J, Anderson SA, et al. The Inter-Association Task Force for Preventing Sudden Death in Secondary School Athletics Programs: best practices recommendations. J Athl Train. 2013 doi: 10.4085/1062-6050-48.4.12. 48(4):546–553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lyznicki JM, Riggs JA, Champion HC. Certified athletic trainers in secondary schools: report of the council on scientific affairs, American Medical Association. J Athl Train. 1999;34(3):272–276. [PMC free article] [PubMed] [Google Scholar]
- 10.Waxenberg R. Athletic trainers fill a necessary niche in secondary schools. National Athletic Trainers' Association Web site. 2015 http://www.nata.org/NR031209. Published 2009. Accessed June 10, [Google Scholar]
- 11.Pryor RR, Case DJ, Vandermark LW, et al. Athletic training services in public secondary schools: a benchmark study. J Athl Train. 2015;50(2):156–162. doi: 10.4085/1062-6050-50.2.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Creswell JW. Qualitative Inquiry & Research Design: Choosing Among Five Traditions. 3rd ed. Thousand Oaks, CA: SAGE Publications, Inc;; 2013. pp. 145–178. [Google Scholar]
- 13.Thomas DR. A general inductive approach for analyzing qualitative evaluation data. Am J Eval. 2006;27(2):237–246. [Google Scholar]
- 14.Pitney WA, Parker J. Qualitative Research in Physical Activity and the Health Professions. Champaign, IL: Human Kinetics;; 2009. [Google Scholar]
- 15.Semelsberger K. A survival kit for the new athletic director. Paper presented at: Michigan Interscholastic Athletic Administrators Association Summer Workshop; 2000 Jul; Mount Pleasant, MO. [Google Scholar]
- 16.2015 Mission statement. National Association of Collegiate Directors of Athletics Web site. http://www.nacda.com/nacda/nacda-missionstatement.html. Accessed June 10, [Google Scholar]
- 17.McCarthy MR, Hiller WD, Yates-McCarthy JL. Sports medicine in Hawaii: care of the high school athlete in Oahu's public schools. Hawaii Med J. 1991;50(11):395–396. [PubMed] [Google Scholar]
- 18.Slack T, Parent MM. Understanding Sport Organizations: The Application of Organization Theory. 2nd ed. Champaign, IL: Human Kinetics;; 2006. [Google Scholar]
- 19.Tinuoye K. DJ Searcy case: mom vows to get justice in football player's heat-related death. The Grio Web site. 2015 http://thegrio.com/2012/08/02/dj-searcy-case-mom-vows-to-get-justice-in-football-players-heat-related-death. Published 2012. Accessed June 10, [Google Scholar]
- 20.DiMaggio PJ, Powell WW. The iron cage revisited: institutional isomorphism and collective rationality in organizational fields. Adv Strategic Manage. 2000;17:143–166. [Google Scholar]
- 21.Hinings CR, Greenwood R. The Dynamics of Strategic Change. New York, NY: Basil Blackwell;; 1988. [Google Scholar]
- 22.Meyer JW, Rowan B. Institutional organizations: formal structure as myth and ceremony. Am J Sociol. 1977;83(2):340–363. [Google Scholar]
- 23.Almquist J. Valovich McLeod TC, Cavanna A, et al., editors. Summary statement: appropriate medical care for the secondary school-aged athlete. J Athl Train. 2008;43(4):416–427. doi: 10.4085/1062-6050-43.4.416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wham GS, Saunders R, Mensch J. Key factors for providing appropriate medical care in secondary school athletics: athletic training services and budget. J Athl Train. 2010;45(1):75–86. doi: 10.4085/1062-6050-45.1.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nass SJ. A survey of athletic medicine outreach programs in Wisconsin. J Athl Train. 1992;27(2):180–183. [PMC free article] [PubMed] [Google Scholar]
- 26.Jarman DW, Boyland LG. The impacts of budget reductions on Indiana's public schools: the impact of budget changes on student achievement, personnel, and class size for public school corporations in the state of Indiana. Curr Issues Educ. 2011;14(2):1–11. [Google Scholar]
- 27.Johnson N, Oliff P, Williams E. An update on state budget cuts: at least 46 states have imposed cuts that hurt vulnerable residents and the economy. Center on Budget and Policy Priorities Web site. 2015 http://www.cbpp.org/cms/?fa=view&id=1214. Updated February 9, 2011. Accessed June 10, [Google Scholar]
- 28.Brown DL, Swanson LE. Rural America enters the new millennium. In: Brown DL, Swanson LE, editors. Challenges for Rural America in the Twenty-First Century. University Park, PA: The Pennsylvania State University Press;; 2003. pp. 1–15. In. eds. [Google Scholar]
- 29.Hardre PL, Sullivan DW, Crowson HM. Student characteristics and motivation in rural high schools. J Res Rural Educ. 2009;24(16):1–19. [Google Scholar]
- 30.2015 Post-professional athletic training program. Ohio University Web site. http://www.ohio.edu/chsp/ahsw/academics/atg.cfm. Accessed June 10, [Google Scholar]
- 31.Mazerolle SM, Pagnotta KD, Applegate KA, Casa DJ, Maresh CM. The athletic trainer's role in providing emergency care in conjunction with the emergency medical services. Int J Athl Ther Train. 2012;17(2):39–44. [Google Scholar]
- 32.Applegate K. Investigation of Emergency Medical Technicians Practice and Beliefs Regarding the Recognition and Treatment of Exertional Heat Stroke [master's thesis] Storrs: University of Connecticut;; 2011. [Google Scholar]
- 33.Decoster LC, Swartz EE, Hootman JM, Cappaert TA. Characteristics of interactions between certified athletic trainers and emergency medical services personnel in secondary school and collegiate settings: a national survey. J Athl Train. 2010;45(suppl 3):S82. [Google Scholar]
- 34.Ransone J, Dunn-Bennett LR. Assessment of first-aid knowledge and decision making of high school athletic coaches. J Athl Train. 1999;34(3):267–271. [PMC free article] [PubMed] [Google Scholar]
- 35.Buxton BP, Okasaki EM, McCarthy MR, Ho KW. Legislative funding of athletic training positions in public secondary schools. J Athl Train. 1995;30(2):115–120. [PMC free article] [PubMed] [Google Scholar]