Abstract
Objectives
To investigate the association between short-term changes in ambient pollution (particulate matter < 2.5μm in aerodynamic diameter (PM2.5) and ozone (O3)) and the risk of ischemic stroke among individuals living in a bi-ethnic community and whether this association is modified by ethnicity.
Methods
We identified incident ischemic stroke cases from the population-based Brain Attack Surveillance in Corpus Christi (BASIC) project between 2000 and 2012. Associations between PM2.5 (mean 24-hour) and O3 (maximal 8-hour) levels, measured on the same-day and lags of 1-3 days, and odds of ischemic stroke were assessed using a time-stratified case-crossover design and modeled using conditional logistic regression. We explored race/ethnicity (Mexican American versus non-Hispanic white) as a modifier by including interaction terms in the models.
Results
There were 2,948 ischemic strokes with median age 71 years (IQR: 59-80). We observed no overall associations between the air pollutants and odds of ischemic stroke at any lag. When stratified by ethnicity, higher O3 was consistently associated with greater odds of ischemic stroke for non-Hispanic whites, but not for Mexican Americans. Higher PM2.5 was generally associated with lower odds of ischemic stroke for non-Hispanic whites but modestly greater odds for Mexican Americans.
Conclusion
Ethnic differences in the associations between ischemic stroke and short-term exposures to O3 and PM2.5 were suggested indicating that further study in diverse populations may be warranted.
Keywords: Ischemic stroke, ethnicity, air pollution, PM2.5, ozone
1. INTRODUCTION
Acute changes in air pollution have been linked to increased risk of cardiovascular events (Brook et al., 2010; Pope and Dockery, 2006; Simkhovich et al., 2008), but less is known in terms of the association with stroke specifically. Published studies of stroke have examined relationships with particulate matter less than 2.5μm in aerodynamic diameter (PM2.5) and ozone (O3), but inconsistent evidence exists regarding the associations between acute exposures to these pollutants and stroke incidence (Henrotin et al., 2007, 2010; Maheswaran et al., 2012; O’Donnell et al., 2011). One possible explanation for variation in associations across studies could be differing susceptibilities of the populations studied. For example, previous research in cardiovascular disease has suggested there may be differential associations by race/ethnicity, with Hispanics reported to be more susceptible to PM-induced health effects (Allen et al., 2009; Ostro et al., 2008; Sacks et al., 2011). Existing stroke research, however, has been conducted in predominantly non-Hispanic white populations and thus questions remain regarding enhanced susceptibility by race/ethnicity for this endpoint.
Our objective was to investigate associations between daily changes in ambient PM2.5 and O3 levels and the risk of ischemic stroke and to explore effect modification of these associations by ethnicity. Using data from individuals living in the bi-ethnic community of Nueces County, Texas between 2000 and 2012 and a time-stratified case-crossover design, this analysis builds upon past research in this community that documented borderline significant associations between PM2.5 and O3 and stroke (Lisabeth et al., 2008). By more than doubling the follow-up period, we improve our power to detect associations and are able to focus on a more specific endpoint of ischemic stroke using validated data that is not available in many studies. We furthermore add a new hypothesis that associations will be modified by ethnicity. Specifically, we hypothesized that higher levels of PM2.5 and O3 are associated with increased risk of incident ischemic stroke and that ethnicity modifies the associations between PM2.5 and O3 and incident ischemic stroke, such that the associations are greater in Mexican Americans compared with non-Hispanic whites.
2. MATERIAL AND METHODS
2.1 Study Population
Data are from the Brain Attack Surveillance in Corpus Christi (BASIC) project (Morgenstern et al., 2013; Smith et al., 2004). BASIC is an ongoing population-based stroke surveillance study in Nueces County, Texas. Nueces County is located on the Gulf Coast, geographically isolated from the larger cities in southeast Texas, being over 150 miles from Houston and San Antonio making complete case capture for stroke possible. Approximately, 340,000 people live in Nueces County with the majority of the population (95%) residing in the urban city of Corpus Christi. Based on the 2010 Census, 61% of the population is Mexican American and 33% is non-Hispanic white (US Census Bureau, 2012). There were 2,948 ischemic strokes included in the current analysis after 268 strokes were excluded due to missing exposure data.
2.2 Study Design
We used a time-stratified case-crossover study design to assess the associations between ambient air pollution (PM2.5 and O3) and odds of incident ischemic stroke and evaluate whether ethnicity modifies these associations. This study design allowed for the comparison of each subject’s exposure to air pollution prior to an acute stroke event with his or her own exposure during referent control periods where he/she did not have a stroke (Lumley and Levy, 2000). Control periods were selected on the same day of the week, falling in the same calendar month as the stroke event. Such that if an individual had a stroke on July 1st, the control dates would all be post-stroke dates of July 8th, 15th, 22nd, and 29th. Similarly, if an individual had a stroke on July 15th, the control dates would be the two pre-stroke dates (July 1st and 8th) and the two post-stroke dates (July 22nd and 29th). This selection approach avoids overlap bias and bias in time trends while controlling for seasonality and all time-invariant individual level characteristics (Janes et al., 2005).
2.3 Stroke Ascertainment
Methods for case identification in BASIC included active and passive surveillance techniques as has been previously described (Morgenstern et al., 2013; Smith et al., 2004). Briefly, between January 1, 2000 and June 30, 2012, trained abstractors screened ischemic stroke cases from seven hospitals in the county. Out of hospital surveillance was also conducted using other sources at various times in the study as previously described (Morgenstern et al., 2013). Admission and emergency department logs were screened daily for validated cerebrovascular diagnostic terms. Monthly admissions from the hospitals were also checked for cerebrovascular ICD-9 discharge codes for stroke. Study neurologists blinded to age and ethnicity validated strokes according to published international clinical criteria (Asplund et al., 1988) that require a focal neurologic deficit of acute onset specifically attributable to cerebrovascular distribution lasting longer than 24 hours. For the purposes of this study, we focused on first-ever completed ischemic strokes defined as no documented medical history of stroke/transient ischemic attack (TIA) in the medical record. Per the BASIC protocol, patients were excluded if they were younger than 45 years of age, lived outside of Nueces County, or if their strokes were traumatic. The BASIC project was approved by the University of Michigan Institutional Review Board and each of the Nueces County hospital systems.
2.4 Other Covariates Collected (Race/Ethnicity Ascertainment)
We ascertained race/ethnicity from medical records, which have been demonstrated to have a 97% agreement with self-reported race/ethnicity in this study community (kappa=0.94) (Smith et al., 2004). Additional information collected from medical records included date of first presentation for stroke, demographics, traditional stroke risk factors, including diabetes, hypertension, atrial fibrillation, high cholesterol, heart disease, and smoking status. Home addresses were recorded from the medical record and sent to an external company for geocoding (Mapping Analytics, Rochester, New York). Approximately 97% of addresses were able to be geocoded, with 94% at the block-face-level.
2.5 Air Pollutant and Meteorology Data
We obtained ambient air pollutant concentration (PM2.5 and O3) and meteorological data for 2000 to 2012 from the Texas Commission on Environmental Quality’s (TCEQ) Texas Air Monitoring Information System (TAMIS) (TCEQ (Texas Commission on Environmental Quality), 2012). Data for the air pollutants and wind direction were collected from one monitor centrally located within the urban population, Corpus Christi West C4 (483550025). PM2.5 was measured using a tapered element oscillating microbalance (TEOM) and O3 was measured using an ultraviolet absorption analyzer. Relative humidity was calculated using dew point temperature from the National Oceanic and Atmospheric Administration (NOAA) (NOAA (National Oceanographic and Atmospheric Administration), 2013) from the Corpus Christi International airport 6.5 km away from the pollutant monitor. PM2.5, ambient temperature, and relative humidity were averaged daily (midnight to midnight) and the daily maximal 8-hour average was calculated for O3. Of the 4,565 days in the study period, there were 329 days with insufficient data to calculate the mean 24-hour PM2.5, one day with an unusually high average and peak PM2.5 (greater than nine-times median level), and 106 days of missing O3 data resulting in a total of 382 days excluded due to missingness of either air pollutant (8.4%).
2.6 Statistical Methods
We calculated descriptive statistics for the overall study population and by ethnicity. Chi-squared tests were used for categorical variables and Wilcoxon Rank Sum tests for continuous variables. We examined both air pollution and meteorological data with descriptive statistics as well as time-series plots. We used conditional logistic regression, stratifying on each stroke event, to calculate the odds ratios (ORs) and corresponding 95% confidence intervals associated with the air pollutant exposures. We assessed the functional forms of air pollutant and meteorological variables using penalized polynomial splines but found linear functional forms to be appropriate. Our primary analyses utilized single pollutant models with adjustment for ambient temperature and relative humidity at the same lag as the pollutant. We calculated ORs for a 10 μg/m3 or 10 ppb change in PM2.5 and O3, respectively. Associations were examined separately for concentrations measured the same-day (lag 0), 1-day prior (lag 1), 2-days prior (lag 2), and 3-days prior (lag 3) to presentation for stroke. These lags were selected based on associations found in other studies, as well as the belief that this range includes the appropriate pathophysiologic window for triggering a stroke event (Henrotin et al., 2007, 2010; Lisabeth et al., 2008; Wellenius et al., 2012). Day of the week and month were inherently adjusted for by the study design (Lumley and Levy, 2000). We added interaction terms to the models to test effect modification by ethnicity (on the multiplicative scale) and reported ethnic-specific associations and considered p-values < 0.10 to provide evidence of effect modification. We also tested for additive interactions between ethnicity and the pollutants using methods described by Hosmer and Lemeshow (1992).
In secondary analyses, we explored the potential confounding effect of each pollutant with the other by running multi-pollutant models with both pollutants included. We conducted sensitivity analyses on the subset of cases with geocoded address within five kilometers of the ambient monitor to test the robustness of the results to potential exposure measurement error. We similarly examined effect modification of the air pollution-stroke association by season (summer vs. non-summer) as well as a binary indicator for residing downwind of a pollution point source using daily prevailing wind direction. We conducted all analyses using SAS version 9.3 (SAS Institute Inc, Cary, NC) and the R statistical package, version 3.0.1 (R Foundation for Statistical Computing, Vienna, Austria).
3. RESULTS
Median age of the stroke cases was 71 years (interquartile range (IQR): 59-80) with 56% (n=1,652) among Mexican Americans (Table 1). Mexican Americans were more likely than non-Hispanic whites to have their strokes at younger ages, have a history of diabetes, and have a history of hypertension, but less likely to be former smokers and have a history of atrial fibrillation. Most stroke cases (85%) resided within 20 km of the ambient monitoring site with a median distance of 6.9 km (IQR: 3.6-13.3). Median temperature for the study period was 23.3°C (IQR, 18.4-27.5) and median relative humidity was 78.3% (IQR: 70.2-84.0).
Table 1.
Characteristics of 2948 Incident Ischemic Strokes in Nueces County, Texas, 2000-2012
| Characteristic | Overall (N=2948) |
Mexican American (N=1652) |
Non-Hispanic White (N=1296) |
P |
|---|---|---|---|---|
| Age, median (Q1, Q3), y | 71 (59, 80) | 67 (57, 78) | 75 (63, 83) | <0.001 |
| Female | 1511 (51.3) | 835 (50.5) | 676 (52.2) | 0.384 |
| MA | 1652 (56.0) | - | - | |
| Medical History | ||||
| Atrial fibrillation | 390 (13.2) | 152 (9.2) | 238 (18.4) | <0.001 |
| Coronary artery disease | 895 (30.4) | 499 (30.2) | 396 (30.6) | 0.846 |
| Diabetes mellitus | 1204 (40.8) | 882 (53.4) | 322 (24.9) | <0.001 |
| High cholesterol | 956 (32.4) | 551 (33.4) | 405 (31.3) | 0.226 |
| Hypertension | 2204 (74.8) | 1275 (77.2) | 929 (71.7) | <0.001 |
| Smoking History | ||||
| Current | 610 (20.7) | 340 (20.6) | 270 (20.8) | 0.867 |
| Former | 366 (12.4) | 158 (9.6) | 208 (16.1) | <0.001 |
| Distance to monitor, median (Q1, Q3), km |
6.9 (3.6, 13.3) | 2.7 (1.4, 6.3) | 5.9 (3.7, 10.8) | <0.001 |
Q = quartile.
3.1 PM2.5
The median pollutant level of PM2.5 for the study period was 7.7 μg/m3 (IQR: 5.7-10.6). Across all individuals, we found no associations between the odds of incident ischemic stroke and PM2.5 concentrations (Figure 1). Effect modification of the PM2.5 association by ethnicity was, however, borderline significant for same-day PM2.5 levels (p-interaction=0.07). At this exposure time, a 4.9 μg/m3 (IQR) higher same-day PM2.5 was associated with a 6% higher odds of ischemic stroke in Mexican Americans (95% CI: 0.99-1.12), but a 3% lower odds of ischemic stroke in non-Hispanic whites (95% CI: 0.90-1.04). Effect modification PM2.5 by ethnicity was not present for other lag days. Tests for additive interaction were non-significant for all lags (all p-interaction > 0.29).
Figure 1.
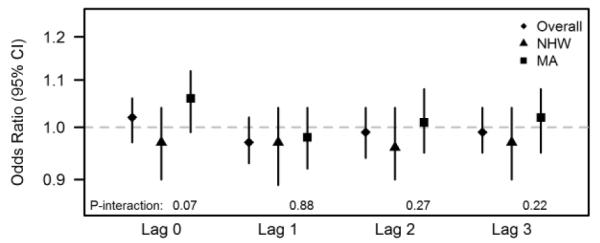
Odds ratios associated with a 10 μg/m3 increase in 24-hour PM2.5 overall and stratified by ethnicity for 2000-2012 incident ischemic stroke cases in Nueces County, Texas. NHW corresponds to non-Hispanic White ethnicity and MA corresponds to Mexican American ethnicity.
3.2 O3
The median pollutant level of O3 for the study period was 35.7 ppb (IQR: 25.5-46.3). Across all individuals, higher O3 levels corresponded with higher odds of incident ischemic stroke with the strongest associations for lags 1 and 2, but not significantly (Figure 2). In models with interaction terms by ethnicity, non-Hispanic whites were consistently found to have stronger associations between O3 concentrations and incident ischemic stroke with strongest differences at the longer lag periods. This modification by ethnicity was strongest at lag 2 (p-interaction=0.06), where a 20.8 ppb (IQR) higher O3 level was associated with a 12% higher odds of ischemic stroke (95% CI: 1.01-1.25) among non-Hispanic whites while Mexican Americans experienced no difference in odds (OR: 0.99, 95% CI: 0.90-1.09). Tests for additive interaction were non-significant for all lags (all p-interaction > 0.29).
Figure 2.
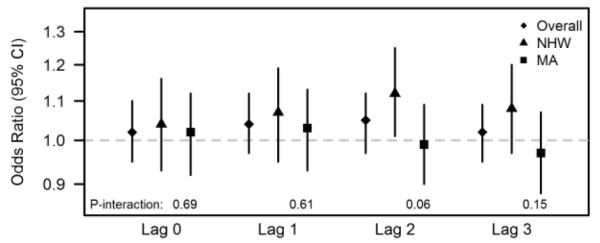
Odds ratios associated with a 10 ppb increase in maximal 8-hour O3 overall and stratified by ethnicity for 2000-2012 incident ischemic stroke cases in Nueces County, Texas. NHW corresponds to non-Hispanic White ethnicity and MA corresponds to Mexican American ethnicity.
3.3 Sensitivity Analysis
Multi-pollutant models yielded similar results as reported for single pollutant models (Supplementary Table 1). Results were similarly robust across season and presence of upwind pollution sources. Restriction to the 1,121 ischemic strokes residing within five km of the air pollution monitor were also consistent with our main results, with slightly stronger associations for PM2.5 and slightly attenuated associations for O3 (Supplementary Table 2).
4. DISCUSSION
In this population-based stroke study that included 13 years of validated ischemic strokes, we documented suggestive associations between higher short-term O3 exposures and higher odds of incident ischemic stroke among non-Hispanic whites but not Mexican Americans. No consistent associations were found for PM2.5. Although we did not find strong associations between incident ischemic stroke and short-term changes in air pollution, the suggestion of ethnic differences indicates that more research in diverse populations may be warranted.
These findings are in line with suggestive associations previously observed in this population over a 5-year follow-up period for O3 and stroke, but not PM2.5 (Lisabeth et al., 2008). In that study, borderline associations were found between risk of ischemic stroke/TIA and same-day and lag 1 PM2.5 concentrations (RR: 1.03, 95% CI: 0.99-1.07 and RR: 1.03, 95% CI: 1.00-1.07 per 5.1 μg/m3) and lag 1 O3 concentrations (RR: 1.04, 95% CI: 0.99-1.09 per 15.7 ppb). This analysis added an additional 7 years of follow-up, restricted to validated incident ischemic stroke, and newly explored effect modification of associations between air pollution and stroke by ethnicity. Although we hypothesized that associations would be stronger when restricted to incident ischemic stroke, it is possible that we did not observe associations in the same area over a longer time period because we excluded recurrent events and TIAs, which could have stronger associations with air pollutants than ischemic stroke (Bedada et al., 2012; Henrotin et al., 2007). Power may also have been an issue even over the longer follow-up period given that the observed levels of ambient air pollution in Nueces County were quite low with relatively little variability.
We hypothesized that both PM2.5 and O3 would be associated with incident stroke risk, however the lack of overall associations found in our study is consistent with some previous studies. Studies from Canada with similar pollution levels also reported no association between ischemic stroke risk and PM2.5 in a case-crossover design (O’Donnell et al., 2011; Villeneuve et al., 2012). Case-crossover studies in Massachusetts (Wellenius et al., 2012), Pennsylvania (Xu et al., 2013), and France (Henrotin et al., 2010) reported no associations between same day or previous day O3 with risk of ischemic stroke; these studies also reported lower average daily concentrations of O3 than we observed. Additionally, recent reviews and meta-analyses have suggested null to small associations between O3 and ischemic stroke, with slightly stronger effects in case-crossover studies (Ljungman and Mittleman, 2014; Shah et al., 2015). Conversely to our results, some studies have found an association between PM2.5 and incident stroke. A study in Boston, Massachusetts found that an IQR increase in PM2.5 (6.4 μg/m3) in the 24 hours preceding stroke was associated with an OR of 1.11 (95% CI: 1.03-1.20) for ischemic stroke (Wellenius et al., 2012). This could be due in part to different chemical components of PM2.5 across these areas (Bell et al., 2009, 2007). Further research is needed to examine the effects of PM species in the context of their association with ischemic stroke.
A unique contribution of our investigation of air pollution and stroke was the consideration of differences by ethnicity. Mexican Americans have an increased stroke risk compared to non-Hispanic whites (Morgenstern et al., 2013), but the modification of relationships between stroke and air pollution have not been investigated. A priori, we hypothesized a stronger association with PM2.5 in Mexican Americans based on previous research that has demonstrated that Hispanics are more susceptible to PM-induced cardiovascular health effects (Sacks et al., 2011). Possible explanations for these differences may be that Mexican Americans have a higher prevalence of living in disadvantaged areas with different housing characteristics (Dvonch et al., 2009; Lisabeth et al., 2007) and hold more blue-collar occupations where they may have increased exposure to outdoor air pollution (Cattan, 1993). Another possibility is that biological impacts of air pollution on stroke risk vary by ethnicity, in part due to increased prevalence of diabetes in Mexican Americans (Lisabeth et al., 2006; Moon et al., 2012), as stronger associations have been found between PM2.5 and ischemic stroke among diabetics as compared to nondiabetics (O’Donnell et al., 2011). A recent meta-analysis of air pollution and stroke data has also suggested that low income, a marker of disadvantaged areas, may modify the association between air pollution and stroke (Shah et al., 2015), which could also partly explain our observed ethnic differences.
Although associations with PM2.5 were not strong in this study, the magnitude of the association we observed between PM2.5 and stroke in Mexican Americans was larger than for non-Hispanic whites for the same-day lag as has been previously reported (Lisabeth et al., 2008; Wellenius et al., 2012). Greater short-term PM2.5 exposure was associated with an increased risk of cardiovascular mortality among Hispanics as compared to non-Hispanic whites in a study of six California counties (Ostro et al., 2008); specifically, Hispanics had a 2.5-6% excess risk of mortality due to PM2.5 compared a 0-2% excess risk of mortality for non-Hispanic whites. Similarly, the Multi-Ethnic Study of Atherosclerosis, with estimated PM2.5 concentrations ranging from 10.6 to 24.7 μg/m3, reported 10 μg/m3 increases in PM2.5 among Hispanics were associated with a 22% elevated risk of coronary calcification (Allen et al., 2009), while no increased risk was found in non-Hispanic whites.
In contrast, among non-Hispanic whites, increases in lag 2 O3 were associated with higher odds of ischemic stroke, but not in Mexican Americans. The 6% higher odds of ischemic stroke that we found for lag 2 exposure in non-Hispanic whites was comparable to the results of Henrotin et al., who reported an OR of 1.04 for lag 2 O3 exposure in a non-Hispanic white European population (Henrotin et al., 2010). The reasons for our contrasting findings for PM2.5 and O3 by ethnicity are not clear though it may represent a complex interplay of biologic susceptibility, infiltration of homes, or activity patterns. Chance is also a possible explanation. Our focus was on the existence of an ethnic disparity and as a result, additional research is needed in diverse populations to investigate ethnic-specific effects and their causes.
Our results have implications in terms of public health. The magnitude of the observed associations between O3 concentrations and incident ischemic stroke may be modest, but the number of strokes that are attributable to O3 may be high given that air pollution exposure affects almost everyone. Assuming that the association between O3 and incident ischemic stroke is causal and a linear function, a 20% reduction in the mean O3 levels (7.4 ppb) during the study period may have averted approximately 6,007 of the 387,000 stroke hospitalizations in the South region of US in 2010 alone (National Center for Health Statistics, 2010).
There are some limitations of this work that warrant discussion. The classification of the exposure for individuals was limited by the fact that we only had one monitor in the study community. The measurements from the single fixed monitor may introduce measurement error into our analysis if the daily fluctuations were not homogeneous across the county. However, another monitor in the county measuring 24-hour PM2.5 every three to six days using the Federal Reference Method showed large correlations (ρ≥80%) with the single monitor used in our study. This is consistent with the topography of Nueces County (flat, with elevation varying from sea level to a maximum elevation of 180 feet (TNRIS (Texas Natural Resources Information System), 2013)) which suggests that air pollution exposures are likely to be highly correlated across space. It is possible, however, that our observed ethnic differences may, in part, be due to differential measurement error if the communities resided in distinct neighborhoods in Nueces County although we did find similar associations when restricted to those that resided within a 5km buffer of the air pollution monitor. We are also assuming that ambient pollutant concentrations are surrogates for personal pollutant exposures, which may be the case for PM2.5 but not O3 (Sarnat et al., 2001). Another issue is that we do not have the exact time of stroke onset, but rather the day of hospital presentation. Although consistent with much of the existing literature on air pollution and stroke, this may have resulted in an underestimation of the strength of the association between air pollution and ischemic stroke (Lokken et al., 2009). Another possibility is that air pollution exposures could have triggered death such that competing risks would reduce the observed association between air pollution and incident stroke. Also, the ethnic distribution and air pollution exposures of Corpus Christi are unique, and therefore generalizability may be limited.
In summary, we observed suggestive associations between higher PM2.5 and O3 levels and incident ischemic stroke, with associations observed only among Mexican Americans for PM2.5 and only among non-Hispanic whites for O3. This study contributes to the literature by being the first study to our knowledge to address a possible ethnic difference in the influence of air pollution on stroke risk, and suggests that further study in diverse populations is warranted.
Supplementary Material
HIGHLIGHTS.
First study to examine possible ethnic differences in air pollution on stroke risk.
Case-crossover design to assess associations between PM2.5/O3 and stroke incidence.
Suggestive association between PM2.5 and ischemic stroke among Mexican Americans.
Suggestive association between O3 and ischemic stroke among non-Hispanic whites.
Further study in diverse populations is warranted.
ACKNOWLEDGEMENTS
None
FUNDING
This study was supported by grants from the American Heart Association (14PRE18360000) and the National Institutes of Health/National Institute of Neurological Disorders and Stroke (R0138916).
ABBREIVIATIONS
- PM2.5
particulate matter less than 2.5μm in aerodynamic diameter
- O3
Ozone
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
HUMAN SUBJECTS
The Brain Attack Surveillance In Corpus Christi (BASIC) project was approved by the University of Michigan Institutional Review Board and each of the Nueces County hospital systems.
COMPETING INTERESTS
None
REFERENCES
- Allen R, Criqui M, Roux A. Fine particulate matter air pollution, proximity to traffic, and aortic atherosclerosis. Epidemiol. 2009;20:254–264. doi: 10.1097/EDE.0b013e31819644cc. doi:10.1097/EDE.0b013e31819644cc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asplund K, Tuomilehto J, Stegmayr B, Wester PO, Tunstall-Pedoe H. Diagnostic criteria and quality control of the registration of stroke events in the MONICA project. Acta Med. Scand. Suppl. 1988;728:26–39. doi: 10.1111/j.0954-6820.1988.tb05550.x. [DOI] [PubMed] [Google Scholar]
- Bedada GB, Smith CJ, Tyrrell PJ, Hirst AA, Agius R. Short-term effects of ambient particulates and gaseous pollutants on the incidence of transient ischaemic attack and minor stroke: a case-crossover study. Environ. Health. 2012;11:77. doi: 10.1186/1476-069X-11-77. doi:10.1186/1476-069X-11-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell ML, Dominici F, Ebisu K, Zeger SL, Samet JM. Spatial and temporal variation in PM(2.5) chemical composition in the United States for health effects studies. Environ. Health Perspect. 2007;115:989–95. doi: 10.1289/ehp.9621. doi:10.1289/ehp.9621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell ML, Ebisu K, Peng RD, Samet JM, Dominici F. Hospital admissions and chemical composition of fine particle air pollution. Am. J. Respir. Crit. Care Med. 2009;179:1115–20. doi: 10.1164/rccm.200808-1240OC. doi:10.1164/rccm.200808-1240OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brook RD, Rajagopalan S, Pope CA, Brook JR, Bhatnagar A, Diez-Roux AV, Holguin F, Hong Y, Luepker RV, Mittleman MA, Peters A, Siscovick D, Smith SC, Whitsel L, Kaufman JD. Particulate matter air pollution and cardiovascular disease: An update to the scientific statement from the American Heart Association. Circulation. 2010;121:2331–78. doi: 10.1161/CIR.0b013e3181dbece1. doi:10.1161/CIR.0b013e3181dbece1. [DOI] [PubMed] [Google Scholar]
- Cattan P. The Diversity of Hispanics in the US Work Force. Mon. Lab. Rev. 1993;116:3–15. [Google Scholar]
- Dvonch JT, Kannan S, Schulz AJ, Keeler GJ, Mentz G, House J, Benjamin A, Max P, Bard RL, Brook RD. Acute effects of ambient particulate matter on blood pressure: differential effects across urban communities. Hypertension. 2009;53:853–9. doi: 10.1161/HYPERTENSIONAHA.108.123877. doi:10.1161/HYPERTENSIONAHA.108.123877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henrotin JB, Besancenot JP, Bejot Y, Giroud M. Short-term effects of ozone air pollution on ischaemic stroke occurrence: a case-crossover analysis from a 10-year population-based study in Dijon, France. Occup. Environ. Med. 2007;64:439–45. doi: 10.1136/oem.2006.029306. doi:10.1136/oem.2006.029306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henrotin J-B, Zeller M, Lorgis L, Cottin Y, Giroud M, Béjot Y. Evidence of the role of short-term exposure to ozone on ischaemic cerebral and cardiac events: the Dijon Vascular Project (DIVA) Heart. 2010;96:1990–6. doi: 10.1136/hrt.2010.200337. doi:10.1136/hrt.2010.200337. [DOI] [PubMed] [Google Scholar]
- Hosmer DW, Lemeshow S. Confidence interval estimation of interaction. Epidemiology. 1992;3:452–456. doi: 10.1097/00001648-199209000-00012. [DOI] [PubMed] [Google Scholar]
- Janes H, Sheppard L, Lumley T. Case-crossover analyses of air pollution exposure data: referent selection strategies and their implications for bias. Epidemiology. 2005;16:717–26. doi: 10.1097/01.ede.0000181315.18836.9d. [DOI] [PubMed] [Google Scholar]
- Lisabeth LD, Diez Roux AV, Escobar JD, Smith MA, Morgenstern LB. Neighborhood environment and risk of ischemic stroke: the brain attack surveillance in Corpus Christi (BASIC) Project. Am. J. Epidemiol. 2007;165:279–87. doi: 10.1093/aje/kwk005. doi:10.1093/aje/kwk005. [DOI] [PubMed] [Google Scholar]
- Lisabeth LD, Escobar JD, Dvonch JT, Sánchez BN, Majersik JJ, Brown DL, Smith MA, Morgenstern LB. Ambient air pollution and risk for ischemic stroke and transient ischemic attack. Ann. Neurol. 2008;64:53–9. doi: 10.1002/ana.21403. doi:10.1002/ana.21403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lisabeth LD, Risser JMH, Brown DL, Al-Senani F, Uchino K, Smith MA, Garcia N, Longwell PJ, McFarling DA, Al-Wabil A, Akuwumi O, Moyé LA, Morgenstern LB. Stroke burden in Mexican Americans: the impact of mortality following stroke. Ann. Epidemiol. 2006;16:33–40. doi: 10.1016/j.annepidem.2005.04.009. doi:10.1016/j.annepidem.2005.04.009. [DOI] [PubMed] [Google Scholar]
- Ljungman PL, Mittleman MA. Ambient Air Pollution and Stroke. Stroke. 2014 doi: 10.1161/STROKEAHA.114.003130. doi:10.1161/STROKEAHA.114.003130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lokken PR, Wellenius GA, Coull BA, Burger MR, Schlaug G, Suh HH, Mittleman MA. Air Pollution and Risk of Stroke. Epidemiology. 2009;20:137–142. doi: 10.1097/ede.0b013e31818ef34a. doi:10.1097/EDE.0b013e31818ef34a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lumley T, Levy D. Bias in the case–crossover design: implications for studies of air pollution. Environmetrics. 2000;11:689–704. [Google Scholar]
- Maheswaran R, Pearson T, Smeeton NC, Beevers SD, Campbell MJ, Wolfe CD. Outdoor air pollution and incidence of ischemic and hemorrhagic stroke: a small-area level ecological study. Stroke. 2012;43:22–7. doi: 10.1161/STROKEAHA.110.610238. doi:10.1161/STROKEAHA.110.610238. [DOI] [PubMed] [Google Scholar]
- Moon JR, Capistrant BD, Kawachi I, Avendaño M, Subramanian SV, Bates LM, Glymour MM. Stroke incidence in older US Hispanics: is foreign birth protective? Stroke. 2012;43:1224–9. doi: 10.1161/STROKEAHA.111.643700. doi:10.1161/STROKEAHA.111.643700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgenstern LB, Smith MA, Sánchez BN, Brown DL, Zahuranec DB, Garcia N, Kerber KA, Skolarus LE, Meurer WJ, Burke JF, Adelman EE, Baek J, Lisabeth LD. Persistent ischemic stroke disparities despite declining incidence in Mexican Americans. Ann. Neurol. 2013;74:778–85. doi: 10.1002/ana.23972. doi:10.1002/ana.23972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for Health Statistics [accessed 12.12.14];Health Data Interactive. 2010 [WWW Document]. URL www.cdc.gov/nchs/hdi.htm.
- NOAA (National Oceanographic and Atmospheric Administration) [accessed 7.18.13];Surface Data, Hourly Global. 2013 [WWW Document]. URL http://www.ncdc.noaa.gov/cdo-web/
- O’Donnell MJ, Fang J, Mittleman MA, Kapral MK, Wellenius GA. Fine particulate air pollution (PM2.5) and the risk of acute ischemic stroke. Epidemiology. 2011;22:422–31. doi: 10.1097/EDE.0b013e3182126580. doi:10.1097/EDE.0b013e3182126580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ostro BD, Feng W-Y, Broadwin R, Malig BJ, Green RS, Lipsett MJ. The impact of components of fine particulate matter on cardiovascular mortality in susceptible subpopulations. Occup. Environ. Med. 2008;65:750–6. doi: 10.1136/oem.2007.036673. doi:10.1136/oem.2007.036673. [DOI] [PubMed] [Google Scholar]
- Pope CA, Dockery DW. Health effects of fine particulate air pollution: lines that connect. J. Air Waste Manag. Assoc. 2006;56:709–42. doi: 10.1080/10473289.2006.10464485. [DOI] [PubMed] [Google Scholar]
- Sacks JD, Stanek LW, Luben TJ, Johns DO, Buckley BJ, Brown JS, Ross M. Particulate matter-induced health effects: who is susceptible? Environ. Health Perspect. 2011;119:446–54. doi: 10.1289/ehp.1002255. doi:10.1289/ehp.1002255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarnat JA, Schwartz J, Catalano PJ, Suh HH. Gaseous pollutants in particulate matter epidemiology: confounders or surrogates? Environ. Health Perspect. 2001;109:1053–61. doi: 10.1289/ehp.011091053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah ASV, Lee KK, McAllister DA, Hunter A, Nair H, Whiteley W, Langrish JP, Newby DE, Mills NL. Short term exposure to air pollution and stroke: systematic review and meta-analysis. BMJ. 2015;350:h1295. doi: 10.1136/bmj.h1295. doi:10.1136/bmj.h1295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simkhovich BZ, Kleinman MT, Kloner RA. Air pollution and cardiovascular injury epidemiology, toxicology, and mechanisms. J. Am. Coll. Cardiol. 2008;52:719–26. doi: 10.1016/j.jacc.2008.05.029. doi:10.1016/j.jacc.2008.05.029. [DOI] [PubMed] [Google Scholar]
- Smith MA, Risser JMH, Moyé LA, Garcia N, Akiwumi O, Uchino K, Morgenstern LB. Designing multi-ethnic stroke studies: the Brain Attack Surveillance in Corpus Christi (BASIC) project. Ethn. Dis. 2004;14:520–6. [PubMed] [Google Scholar]
- TCEQ (Texas Commission on Environmental Quality) [accessed 5.2.13];Texas Air Monitoring Information System (TAMISWeb) 2012 [WWW Document]. URL http://www.tceq.texas.gov/agency/data/download-data.html.
- TNRIS (Texas Natural Resources Information System) Texas Natural Resources Information System; [accessed 6.19.13]. 2013. [WWW Document]. URL www.tnris.org. [Google Scholar]
- US Census Bureau [accessed 10.17.12];Census 2010 summary file 2 (SF2) Population of Nueces County, Texas: 2010. 2012 [WWW Document]. URL www.census.gov.
- Villeneuve PJ, Johnson JYM, Pasichnyk D, Lowes J, Kirkland S, Rowe BH. Short-term effects of ambient air pollution on stroke: Who is most vulnerable? Sci. Total Environ. 2012;430:193–201. doi: 10.1016/j.scitotenv.2012.05.002. doi:10.1016/j.scitotenv.2012.05.002. [DOI] [PubMed] [Google Scholar]
- Wellenius GA, Burger MR, Coull BA, Schwartz J, Suh HH, Koutrakis P, Schlaug G, Gold DR, Mittleman MA. Ambient air pollution and the risk of acute ischemic stroke. Arch. Intern. Med. 2012;172:229–34. doi: 10.1001/archinternmed.2011.732. doi:10.1001/archinternmed.2011.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu X, Sun Y, Ha S, Talbott EO, Lissaker CTK. Association between ozone exposure and onset of stroke in Allegheny County, Pennsylvania, USA, 1994-2000. Neuroepidemiology. 2013;41:2–6. doi: 10.1159/000345138. doi:10.1159/000345138. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


