Abstract
Aim
To compare between soft and hard occlusal splint therapy for the management of myofacial pain dysfunction (MPD) or internal derangement (ID) of the temporomandibular joint (TMJ) with reciprocal clicking.
Patients and methods
This study included 50 patients (age range: 24–47 years) who had been diagnosed with MPD or ID of the TMJ in the form of reciprocal clicking. Patients were divided into two groups. They were treated for 4 months with either a vacuum-formed soft occlusal splint constructed from 2-mm-thick elastic rubber sheets (soft splint group) or a hard flat occlusal splint fabricated from transparent acrylic resin (hard splint group). Monthly follow-up visits were performed during the treatment period. Before treatment and 1, 2, 3 and 4 months after treatment, the dentist measured all parameters of TMJ function (pain visual analog scores, tenderness of masticatory muscles, clicking and tenderness of the TMJ, and range of mouth opening).
Results
All parameters of TMJ function showed significant improvement in both groups during the follow-up period, with a statistically significant difference between the two groups at the 4-month follow-up visit.
Conclusions
Both forms of occlusal splints (soft and hard) improved TMJ symptoms in patients with MPD or ID of the TMJ. However, the soft occlusal splints exhibited superior results after 4 months of use.
Keywords: Soft occlusal splint, Hard occlusal splint, MPD, Internal derangement, TMJ
1. Introduction
The temporomandibular joint (TMJ) is interrelated with other neuromuscular components. Defects of any of these components or factors preventing them from working in harmony could lead to temporomandibular disorders (TMDs). The American Academy of Orofacial Pain classifies TMD broadly into myogenous and arthrogenous types, both of which can be present at the same time, making diagnosis and treatment more difficult (Kafas and Leeson, 2006). TMDs have a multifactorial etiology, with bruxism, psychological illness, and traumatic injuries from mastication, extreme mouth opening, and dental treatments being considered as the main causes (Fearon and Serwatka, 1983, Seligman et al., 1988, Pullinger and Seligman, 1991 Lavigne et al., 2008). TMDs are characterized by clicking and pain, either confined to the TMJ region or radiating to the eyes, shoulder, and neck. Headaches, tinnitus, jaw deviation, locking, and limited mouth opening are common symptoms (Pollmann, 1993, Kafas et al., 2007a). Pain is the most crucial symptom for which patients seek medical care (Dworkin et al., 1990). TMJ locking could progress to complete jaw motion inability. Symptoms range from minor to disabling (Dworkin, 1997).
Management of TMD includes conservative and surgical interventions. Examples of conservative treatments are physical therapy, localized steam application, external muscle massage (Reisine and Weber, 1989), occlusal adjustment (Lundh et al., 1988), analgesia, psychotropic medication (Greene, 1992), splint therapy (Kafas et al., 2007b), alternative therapies such as acupuncture (List et al., 1993), as well as treatment modalities such as ultrasound, soft laser, diathermy, and infrared radiation (Mohl et al., 1990). Surgical treatments include meniscoplasty, meniscectomy, and meisectomy with disk replacement using the Proplast-Teflon interpositional implant (Tolvanen et al., 1988, Peltola et al., 2000).
Occlusal adjustment involves repositioning the mandible to a centric position by using prosthodontic or orthodontic appliances. Intraoral occlusal splints are designed to provide even and balanced occlusal contact without forcefully altering the mandibular rest position or permanently altering the dental occlusion. Usually made of processed hard acrylic, a splint is worn on the teeth like retainer or a removable denture. Types of occlusal splints include the stabilization splint, modified Hawley splint, and repositioning splint (Wright et al., 1995). Nevertheless, the use of occlusal splints to alleviate TMD signs and symptoms is controversial (Mona et al., 2004).
Most comparative studies of different splint designs have relied only on medical history and clinical examination to diagnose disk displacement (Lundh et al., 1985). Soft splints, which are more convenient for patients than hard splints, can be used immediately after provisional diagnosis with TMD (Wright et al., 1995). The rationale for using soft splints is that the soft resilient material may help in distributing the heavy load associated with parafunctional habits (Okeson, 2003). Hard splints are thought to reduce TMD symptoms by altering the occlusal equilibrium, changing the afferent impulses to the central nervous system, improving the vertical dimension, correcting the condylar position, and aiding cognitive awareness (Dylina, 2001).
Littner et al. (2004) reported that hard splints offer more successful outcomes than soft splints for patients with functional disorders of the masticatory system. However, other studies have shown that both soft and hard appliances are equally beneficial in improving masticatory muscle pain in the short term (Pettengill et al., 1998). Given these contradictions, this study aimed to evaluate soft and hard occlusal splint therapies for the management of myofacial pain dysfunction (MPD) or internal derangement (ID) of the TMJ in patients with reciprocal clicking.
2. Patients and methods
2.1. Patient selection
The study sample included 50 patients (21 males and 29 females) who were referred to the Oral and Maxillofacial Surgery outpatient clinic of the Faculty of Oral and Dental Medicine of the Cairo University between January 2010 and November 2012. Inclusion criteria for patient selection were a diagnosis of MPD or ID of the TMJ reciprocal clicking. Patients with a history of previous treatment for TMD were excluded. Diagnostic criteria of MPD included tenderness of the masticatory muscles, restricted or deviated mandibular movement due to muscular restriction, and a myofacial pain duration of at least 3 months. Diagnostic criteria of ID included a history of TMJ noise, anterior disk displacement with reduction, and negative locked jaw. Selected patients were divided into two groups and treated for 4 months with either vacuum-formed soft occlusal splints constructed from 2-mm-thick elastic rubber sheets (soft splint group), or hard flat occlusal splints fabricated from transparent acrylic resin (hard splint group).
2.2. Preoperative examination
At the first visit after study selection, each patient provided a thorough medical history that included a description of the pain (type, frequency, and intensity) and reaction to jaw movements during chewing, speaking, and swallowing. To record pain intensities, patients used the Visual Analog Scale (VAS, 10-cm line), which ranged from 0 (no pain) to 10 (worst possible pain). A clinical evaluation was performed, which included measurement of the maximum comfortable jaw opening using a Boley gauge, as well as assessments of clicking, tenderness at rest and during various jaw movements, and deviation during opening and closing movements. Tenderness of the extraoral masticatory and neck muscles was evaluated by digital palpation. Resistance testing and functional manipulation were used to evaluate the medial and lateral pterygoid muscles. Symptom severity of clicking and tenderness of the TMJ and muscles were graded as 1 (negative), 2 (moderate), or 3 (severe).
2.3. Splint construction
Splints were constructed for the upper arch of each patient. For both splint types, a master cast of the maxilla was fabricated by taking an alginate impression of the maxillary arch. For the soft splint, a vacuum pressure molding device was used for fabrication with 2-mm-thick rubber sheets measuring 13 × 13 cm. The rubber sheet was completely and properly adapted to the cast in the vacuum former. The sheet was removed, and sharp scissors were used to trim the splint edges. The palatal portion of the splint was removed to obtain the final shape (Figure 1, Figure 2). For the hard splint, self-curing transparent acrylic resin was used to fabricate the splint in the form of a flat anterior bite plane with a thickness of 2–3 mm, which separated the posterior teeth while allowing contact between the anterior teeth. The hard splint was retained by Adam’s clasps on the upper first molars (Figure 3, Figure 4).
Figure 1.

The final trimmed night guard & patient cast.
Figure 2.

Night guard inside patient mouth.
Figure 3.

Flat anterior bite plane hard splint inside patient mouth.
Figure 4.
Occlusion with hard splint inside patient mouth.
All splints were disinfected with 2% glutaraldehyde and then tried in the patient’s mouth to check retention. Patients were advised to wear the splint for 4 months. Instructions were given to the patients for progressively increasing the duration of splint use, starting from 2 h on the first day. The time that the splint was used was increased by 2 h each day to reach 14 h per day by the end of the first week. This splinting time was maintained during the second week. At the beginning of the third week, the splinting time was increased by 2 h per day to reach 24 h per day by the end of the week. Subsequently, patients were advised to wear the splint at all times except during meal times and while performing oral hygiene procedures.
2.4. Data and statistical analyses
Patients were recalled weekly during the first month and then monthly after 1, 2, 3, and 4 months of treatment. Monthly follow-up intervals between start of treatment and 1 month, 1–2 months, 2–3 months, and 3–4 months are designated as 1 M, 2 M, 3 M, and 4 M, respectively. TMJ functional parameters, including pain visual analog scale (VAS) scores, tenderness of the masticatory muscles, clicking and tenderness of the TMJ, and range of mouth opening, were recorded before treatment and at each follow-up visit.
TMJ functional parameters were measured and compared between groups and across the follow-up period. Adequate treatment was defined as pain VAS scores less than 2, negative clicking, and a maximum mouth opening of greater than 38 mm. For statistical analysis, the Microsta7 for Windows software package (Microstat Inc.) was used. A one-way ANOVA was used to evaluate the effect of time on parameters in each group, whereas the independent Student t-test was used to compare the two groups at each follow-up interval. The significance level for this study was set at p ⩽ .05.
3. Results
The study comprised of 50 patients (age range: 24–47 years) who had been diagnosed with MPD or ID of the TMJ with reciprocal clicking. Patients in both groups responded well to splint therapy. Pain, maximum jaw opening, TMJ clicking, and muscle tenderness improved in all patients during all follow-up intervals.
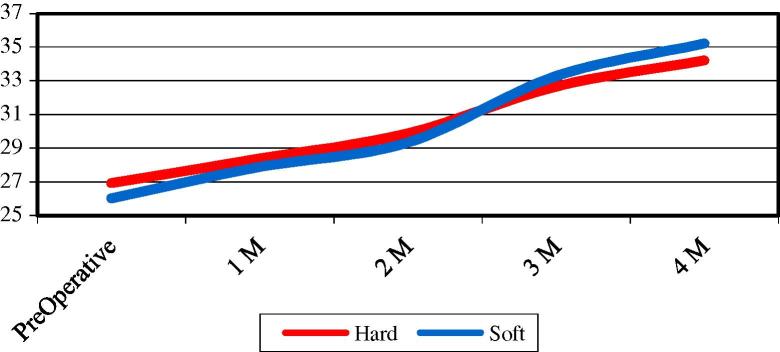
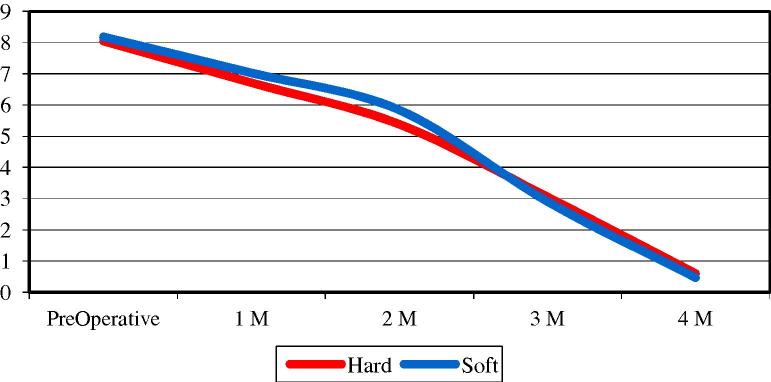
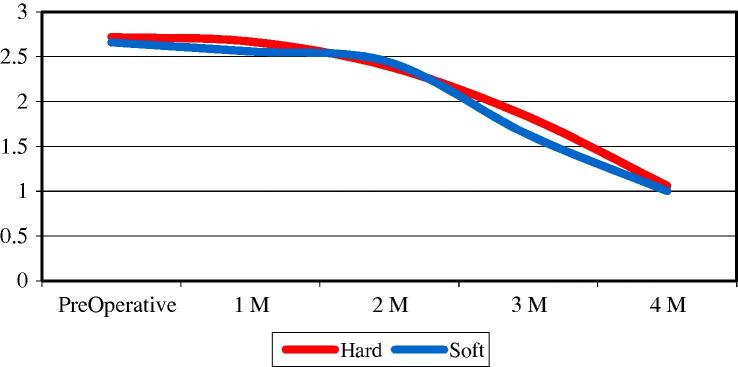
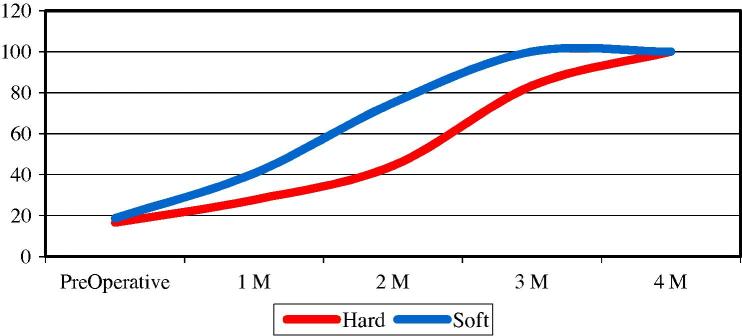
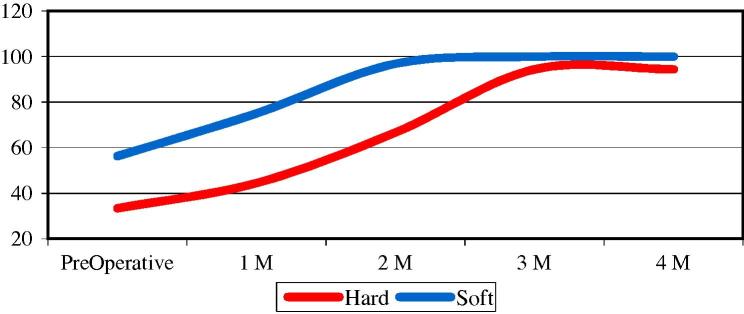
The maximum mouth opening significantly increased over the follow-up period in both groups, with increases starting from 1 M in the soft splint group and 2 M in the hard splint group. At 4 M, but not at any other follow-up interval, the soft splint group showed significantly higher values of mouth opening (Table 1, Fig. 5). VAS scores for pain significantly decreased in both groups throughout the entire follow-up period, with no significant differences between the two groups at any interval (Table 2, Fig. 6). Clicking scores significantly decreased in both groups throughout the follow-up period, starting from 2 M with the hard splint and 3 M with the soft splint. However, there were no statistically significant differences between the two groups at any follow-up interval (Table 3, Fig. 7).
Table 1.
Means of mouth opening during whole follow up intervals.
| Mean ± standard deviation |
“t” | Probability | ||
|---|---|---|---|---|
| Hard | Soft | |||
| Preoperative | 26.94 ± 20.60 | 26.03 ± 3.84 | 0.898 | 0.187 |
| 1 M | 28.39 ± 2.95 | 27.88 ± 3.93 | 0.482 | 0.316 |
| 2 M | 29.89 ± 3.38 | 29.34 ± 4.15 | 0.475 | 0.318 |
| 3 M | 32.67 ± 2.67 | 33.28 ± 3.05 | 0.713 | 0.240 |
| 4 M | 34.22 ± 1.77 | 35.22 ± 2.01 | 1.754 | 0.043 |
| F value | 21.779 | 38.239 | ||
| Probability | 2.14E-12 | 3.09E-22 | ||
| LSD | 1.818 | 1.726 | ||
Figure 5.
Effect of time on mean values of mouth opening in both groups throughout study intervals.
Table 2.
Mean values of pain scores in both groups throughout the study intervals.
| Mean ± standard deviation |
“t” | Probability | ||
|---|---|---|---|---|
| Hard | Soft | |||
| Preoperative | 8.06 ± 1.39 | 8.19 ± 1.60 | 0.293 | 0.385 |
| 1 M | 6.72 ± 1.99 | 7.03 ± 1.99 | 0.526 | 0.301 |
| 2 M | 5.39 ± 2.45 | 5.84 ± 2.26 | 0.663 | 0.255 |
| 3 M | 3.06 ± 1.95 | 2.91 ± 1.78 | 0.274 | 0.392 |
| 4 M | 0.61 ± 0.78 | 0.47 ± 0.76 | 0.630 | 0.266 |
| F value | 48.456 | 103.650 | ||
| Probability | 3.62E-21 | 8.9765E-43 | ||
| LSD | 1.21 | 0.868 | ||
Figure 6.
Effect of time on mean values of pain scores in both groups throughout the study intervals.
Table 3.
Mean values OF CLICKING SCORES IN both groups throughout the study intervals.
| Mean ± standard deviation |
“t” | Probability | ||
|---|---|---|---|---|
| Hard | Soft | |||
| Preoperative | 2.72 ± 0.46 | 2.66 ± 0.48 | 0.471 | 0.320 |
| 1 M | 2.67 ± 0.49 | 2.56 ± 0.50 | 0.711 | 0.240 |
| 2 M | 2.39 ± 0.61 | 2.44 ± 0.62 | 0.268 | 0.395 |
| 3 M | 1.83 ± 0.38 | 1.63 ± 0.49 | 1.549 | 0.064 |
| 4 M | 1.06 ± 0.24 | 100. ± 0.00 | 1.344 | 0.093 |
| F value | 42.990 | 74.226 | ||
| Probability | 1.12E-19 | 5.01E-35 | ||
| LSD | 0.301 | 0.236 | ||
Figure 7.
Effect of time on mean values of clicking in both groups throughout the study intervals. Severe = 3, Moderate = 2, Absent = 1.
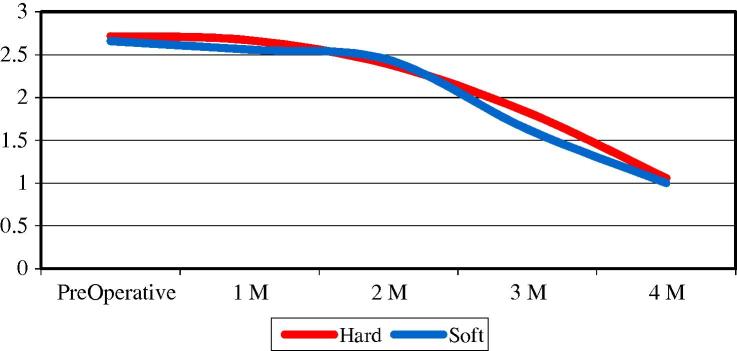
Statistically significant improvements in the tenderness of the TMJ, masticatory muscles, and neck muscles were found in both groups throughout the follow-up period. TMJ tenderness did not differ between the groups at any follow-up interval (Table 4, Fig. 8). However, tenderness of the masticatory muscles showed a significantly greater percentage of improvement in the soft compared to the hard splint group, with complete disappearance of tenderness at 3 M versus 4 M (Table 5, Fig. 9). Similarly, the tenderness of the neck muscles showed a greater percentage of improvement in the soft compared to the hard splint group. Neck tenderness disappeared by 3 M in the soft splint group, but remained at 4 M in the hard splint group (Table 6, Fig. 10).
Table 4.
Mean values of joint tenderness in both groups throughout the study intervals.
| Mean ± standard deviation |
“t” | Probability | ||
|---|---|---|---|---|
| Hard | Soft | |||
| Preoperative | 2.39 ± 0.61 | 2.47 ± 0.57 | 0.466 | 0.322 |
| 1 M | 2.00 ± 0.43 | 2.03 ± 0.54 | 0.222 | 0.413 |
| 2 M | 1.72 ± 0.46 | 1.63 ± 0.66 | 0.553 | 0.292 |
| 3 M | 1.44 ± 0.51 | 1.28 ± 0.46 | 1.162 | 0.126 |
| 4 M | 1.06 ± 0.24 | 1.00 ± 0.00 | 1.344 | 0.093 |
| F value | 23.095 | 43.661 | ||
| Probability | 6.11E-13 | 1.68E-24 | ||
| LSD | 0.301 | 0.251 | ||
Figure 8.
Effect of time on mean values of joint tenderness in both groups throughout the study intervals. Severe = 3, Moderate = 2, Absent = 1.
Table 5.
Percent of negative sings of tenderness of masticatory muscles in both groups throughout the study intervals.
| Percent of negative tenderness |
||
|---|---|---|
| Hard | Soft | |
| Preoperative | 16.67 | 18.75 |
| 1 M | 27.78 | 40.625 |
| 2 M | 44.4 | 75 |
| 3 M | 83.33 | 100 |
| 4 M | 100 | 100 |
Figure 9.
Effect of time on percent of negative signs of tenderness in masticatory muscles in both groups throughout the study intervals.
Table 6.
Percent of negative sings of tenderness of neck muscles in both groups throughout the study intervals.
| Percent of negative tenderness |
||
|---|---|---|
| Hard | Soft | |
| Preoperative | 33.33 | 56.25 |
| 1 M | 44.44 | 75 |
| 2 M | 66.67 | 96.88 |
| 3 M | 94.44 | 100 |
| 4 M | 94.44 | 100 |
Figure 10.
Effect of time on percent of negative signs of tenderness in neck muscles in both groups throughout the study intervals.
4. Discussion
As most TMD symptoms have a high incidence of remission over time, usually within 2–4 weeks (Dworkin, 1997), conservative treatment is considered more appropriate than surgery for these disorders. As a conservative treatment of TMDs, soft splints have some advantages, such as their relative simplicity, reversibility, noninvasiveness, and cost. These splints could be made to fit either the maxillary or mandibular arch and often are inserted immediately (Wright et al., 1995). Owing to their soft and resilient material features, soft splints easily distribute the heavy loads encountered during parafunctional activities, and they have been associated with a high degree of patient tolerance (Okeson, 2003). In contrast, Littner et al. (2004) found that hard splints had successful outcomes in patients complaining of masticatory system disorders. Offering a third opinion, Pettengill et al. (1998) claimed that both soft and hard occlusal appliances are equally useful in improving masticatory muscle pain in the short term. Given these conflicts of opinions, the present study was conducted to compare the efficiency of soft versus hard occlusal splint therapies for the management of TMDs.
In the current study, gradual rehabilitation using occlusal splints was applied to allow patient accommodation to the intraoral bulk and avoid splint rejection. VAS scores for pain showed significant improvement throughout all study intervals. Similarly, Raphael et al. (2003) reported a decrease in VAS scores and the number of painful muscles in patients with myofacial pain after 6 weeks of occlusal splint therapy.
A significant improvement in mouth opening was attained in both groups across the study period. This improvement was significant after 1 or 2 months of treatment in the soft or hard splint group, respectively. These results are comparable to those of Suvinen and Reade (1989), who reported a 7.4-mm increase in jaw opening after splint therapy. The early improvement in mouth opening observed with the soft splint therapy might be due to the material resiliency, which helped to distribute the heavy functional occlusal forces and hastened relief from muscle spasms. This resiliency could also underlie the early relief from masticatory muscle tenderness compared to the hard splint group. Nevertheless, both splint therapies alleviated the pain and tenderness of the TMJ and muscles, leading to an increase in maximal jaw opening. This result is in accordance with Block et al. (1978), who concluded that almost 74% of patients with TMDs had complete remission of symptoms after 6 weeks of occlusal splint therapy.
The early improvement in TMJ clicking observed with hard splint therapy might be due to the wider TMJ space created by the hard occlusal splint. The increased TMJ space allows the meniscus to return to its original position with ease, thus reducing the chance for clicking. The improvement in TMJ clicking and alleviation of tenderness in the TMJ and masticatory muscles observed in this study are in agreement with Kovaleski (1975), who reported improvements in TMJ clicking and tenderness after 2 months of occlusal splint therapy. Another study reported that 87% of patients showed a reduction in pain, 50% showed a reduction in VAS scores, and 70% had no clicking after splint therapy (Tsuga et al., 1989). In another study, soft splint therapy reduced facial myalgia and TMJ clicking by 74% (Harkins et al., 1988). These improvements can be attributed to the even intensity of contacts among all teeth, with disocclusion of the posterior teeth and condylar guidance in all movements. These conditions lead to a relaxation of the elevator and positioning muscles and contribute to reduce the abnormal muscle hyperactivity (Boero, 1989).
Occlusal splint insertion alters the resting position, and adapting to this new position increases the occlusal vertical dimension beyond the free space. The new resting position allows muscles to function more efficiently during contact and reduces muscle activities during postural functions. Meanwhile, the increase in the vertical dimension decreases the muscular effort required, resulting in relaxation of the muscles and TMJ (Mona et al., 2004). The findings of the present study are in agreement with those of Naikmasur et al. (2008). These authors compared the use of a soft occlusal splint with muscle relaxants and analgesics in the management of MPD, and concluded that occlusal splint therapy was superior to pharmacological treatment in terms of improving pain, muscle tenderness, and TMJ clicking. From findings obtained by electromyography of the masticatory muscles, Daif Emad (2012) concluded that occlusal splint therapy for MPD improves the signs and symptoms of TMD. Our findings support their results, revealing that occlusal splint therapy is a conservative treatment modality that is beneficial for reducing pain and muscle tenderness and for improving jaw opening.
5. Conclusions
Both hard and soft occlusal splint therapies are beneficial in the treatment of TMD; however, soft splint therapy results in earlier improvement of some TMD symptoms. Three months is considered to be the minimum period for splint therapy to improve TMD symptoms. Therefore, this study supports the use of splint therapy for managing MPD and TMDs in patients with anterior disk displacement and reduction.
Ethics statement
Patients participated in the current study were consented prior participation after detailed explanation of the treatment steps. Approval for the study proposal was obtained from the dental research center, faculty of oral and dental medicine, Cairo University.
Conflict of interest
The authors reported no conflicts of interest related to this study.
Disclosure of funding
We would like to declare that we did not receive any funding regarding this clinical research. All the work was done at our own expenses.
Footnotes
Peer review under responsibility of King Saud University.
References
- Block S.L., Apfel M., Laskin D.M. The use of a resilient rubber bite appliance in the treatment of MPD syndrome. J. Dent. Res. 1978;57:92. [Google Scholar]
- Boero R.P. The physiology of splint therapy: a literature review. Angle Orthod. 1989;59:165–180. doi: 10.1043/0003-3219(1989)059<0165:TPOSTA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Daif Emad T. Correlation of splint therapy outcome with electromyography of masticatory muscles in temporomandibular disorders with myofascial pain. Acta Odontol. Scand. 2012;70(1):72–77. doi: 10.3109/00016357.2011.597776. (6) [DOI] [PubMed] [Google Scholar]
- Dworkin S.F., Truelove E. In: Conn’s Current Therapy. Rakel R., editor. WB Saunders; Philadelphia: 1997. pp. 1006–1011. [Google Scholar]
- Dworkin S.F., Huggins K.H., LeResche L., Von Korff M., Howard J., Truelove E., Sommers E. Epidemiology of signs and symptoms in temporomandibular disorders: clinical signs in cases and controls. J. Am. Dent. Assoc. 1990;120:273–281. doi: 10.14219/jada.archive.1990.0043. [DOI] [PubMed] [Google Scholar]
- Dylina T.J. A common-sense approach to splint therapy. J. Prosthet. Dent. 2001;86:539–545. doi: 10.1067/mpr.2001.118878. [DOI] [PubMed] [Google Scholar]
- Fearon C.G., Serwatka W.J. A common denominator for nonorganic TMJ pain-dysfunction. J. Prosthet. Dent. 1983;49:805–808. doi: 10.1016/0022-3913(83)90354-2. [DOI] [PubMed] [Google Scholar]
- Greene C.S. Managing TMD patients: initial therapy is the key. J. Am. Dent. Assoc. 1992;123:43–45. doi: 10.14219/jada.archive.1992.0188. [DOI] [PubMed] [Google Scholar]
- Harkins S., Marteney J.L., Cueva O., Cueva L. Application of soft occlusal splints in patients suffering from clicking temperomandibular joints. J. Cranio. Pract. 1988;6:71–75. doi: 10.1080/08869634.1988.11678222. [DOI] [PubMed] [Google Scholar]
- Kafas P., Leeson R. Assessment of pain in temporomandibular disorders: the bio-psychosocial complexity. Int. J. Oral Maxillofac. Surg. 2006;35:145–149. doi: 10.1016/j.ijom.2005.04.023. [DOI] [PubMed] [Google Scholar]
- Kafas P., Chiotaki N., StavrianosCh Stavrianou I. Temporomandibular joint pain: diagnostic characteristics of chronicity. J. Med. Sci. 2007;7:1088–1092. [Google Scholar]
- Kafas P., Kalfas S., Leeson R. Chronic temporomandibular joint dysfunction: a condition for a multidisciplinary approach. J. Med. Sci. 2007;7:492–502. [Google Scholar]
- Kovaleski W.C., Beaver De J. Influence of occlusal splints on jaw position and musculature in patients with temporomandibular joint dysfunction. J. Prosthet. Dent. 1975;33:321–327. doi: 10.1016/s0022-3913(75)80090-4. [DOI] [PubMed] [Google Scholar]
- Lavigne G.J., Khoury S., Abe S., Yamaguchi T., Raphael K. Bruxism physiology and pathology: an overview for clinicians. J. Oral Rehabil. 2008;35(7):476–494. doi: 10.1111/j.1365-2842.2008.01881.x. [DOI] [PubMed] [Google Scholar]
- List T., Helkimo M., Karlsson R. Pressure pain thresholds in patients with craniomandibular disorders before and after treatment with acupuncture and occlusal splint therapy: a controlled clinical study. J. Orofac. Pain. 1993;7:275–282. [PubMed] [Google Scholar]
- Littner D., Perlman-Emodi A., Vinocuor E. Efficacy of treatment with hard and soft occlusal appliance in TMD. Refuat Hapeh Vehashinayim. 2004;21(3):52–58. 94. [PubMed] [Google Scholar]
- Lundh H., Westesson P.-L., Koop S., Tillstrom B. Anterior repositioning splint in the treatment of temporomandibular joints with reciprocal clicking: comparison with flat occlusal splint and an untreated controlled group. Oral Surg. Oral Med. Oral Pathol. 1985;60:131–136. doi: 10.1016/0030-4220(85)90280-4. [DOI] [PubMed] [Google Scholar]
- Lundh H., Westesson P.L., Jisander S., Eriksson L. Disc-repositioning onlays in the treatment of temporomandibular joint disc displacement: comparison with a flat occlusal splint and with no treatment. Oral Surg. Oral Med. Oral Pathol. 1988;66:155–162. doi: 10.1016/0030-4220(88)90084-9. [DOI] [PubMed] [Google Scholar]
- Mohl N.D., Ohrbach R.K., Crow H.C., Gross A.J. Devices for the diagnosis and treatment of temporomandibular disorders. Part III: Thermography, ultrasound, electrical stimulation, and electromyographic biofeedback. J. Prosthet. Dent. 1990;63(4):472–477. doi: 10.1016/0022-3913(90)90240-d. [DOI] [PubMed] [Google Scholar]
- Mona F., Nagwa E., Dalia E., Adel B. Occlusal splint therapy and magnetic resonance imaging. World J. Orthod. 2004;5:133–140. [PubMed] [Google Scholar]
- Naikmasur V., Bhargava P., Guttal K., Burde K. Soft occlusal splint therapy in the management of myofascial pain dysfunction syndrome: follow-up study. Indian J. Dent. Res. 2008;19:196–203. doi: 10.4103/0970-9290.42950. [DOI] [PubMed] [Google Scholar]
- Okeson, J.P., 2003. Management of Temporomandibular Disorders and Occlusion. 5th ed. Mosby, St. Louis. p. 260. Oral Surg. Oral Med. Oral Pathol. 1991, 71:529-534.
- Peltola M.K., Pernu H., Oikarinen K.S., Raustia A.M. The effect of surgical treatment of the temporomandibular joint: a survey of 70 patients. Cranio. 2000;18:120–126. doi: 10.1080/08869634.2000.11746123. [DOI] [PubMed] [Google Scholar]
- Pettengill Craig A., Growney Maurice R., Jr., Schoff Robert, Kenworthy Christian R. A pilot study comparing the efficacy of hard and soft stabilizing appliances in treating patients with temporomandibular disorders. J. Prosthet. Dent. 1998;79:165–168. doi: 10.1016/s0022-3913(98)70211-2. [DOI] [PubMed] [Google Scholar]
- Pollmann L. Sounds produced by the mandibular joint in a sample of healthy workers. J. Orofac. Pain. 1993;7(359):361. [PubMed] [Google Scholar]
- Pullinger A.G., Seligman D.A. Trauma History in Diagnostic Groups of Temporomandibular Disorders. Oral Surg. Oral Med. Oral Pathol. 1991;71(5):529–534. doi: 10.1016/0030-4220(91)90355-g. [DOI] [PubMed] [Google Scholar]
- Raphael K.G., Marbach J.J., Klausner J.J., Teaford M.F., Fischoff D.K. Is bruxism severity a predictor of oral splint efficacy in patients with myofascial face pain? J. Oral Rehabil. 2003;30:17–29. doi: 10.1046/j.1365-2842.2003.01117.x. [DOI] [PubMed] [Google Scholar]
- Reisine S.T., Weber J. The effects of temporomandibular joint disorders on patients’ quality of life. Community Dent. Health. 1989;6:257–270. [PubMed] [Google Scholar]
- Seligman D.A., Pullinger A.G., Solberg W.K. The prevalence of dental attrition and its association with factors of age, gender, occlusion, and TMJ symptomatology. J. Dent. Res. 1988;67:1323–1333. doi: 10.1177/00220345880670101601. [DOI] [PubMed] [Google Scholar]
- Suvinen T., Reade P. Prognostic features of value in the management of temporomandibular joint pain-dysfunction syndrome by occlusal splint therapy. J. Prosthet. Dent. 1989;61:355–361. doi: 10.1016/0022-3913(89)90145-5. [DOI] [PubMed] [Google Scholar]
- Tolvanen M., Oikarinen V.J., Wolf J. A 30-year follow-up study of temporomandibular joint meniscectomies: a report on five patients. Br. J. Oral Maxillofac. Surg. 1988;26(4):311–316. doi: 10.1016/0266-4356(88)90049-6. [DOI] [PubMed] [Google Scholar]
- Tsuga K., Akagawa Y., Sakaguchi R., Tsuru H. A short-term evaluation of the effectiveness of stabilization-type occlusal splint therapy for specific symptoms of temporomandibular joint dysfunction syndrome. J. Prosthet. Dent. 1989;61:610–613. doi: 10.1016/0022-3913(89)90286-2. [DOI] [PubMed] [Google Scholar]
- Wright E., Anderson G., Schulte J. A randomized clinical trial of intraoral soft splints and palliative treatment for masticatory muscle pain. J. Orofac. Pain. 1995;9:192–199. [PubMed] [Google Scholar]